Ventilation
Pulmonary Ventilation
Pulmonary Ventilation Definition:
Table of Contents
- Pulmonary ventilation is a cyclic process, by which fresh air enters the lungs and an equal volume of air leaves the lungs.
- It is the volume of air moving in and out of the lungs per minute in quiet breathing. It is also called respiratory minute volume (RMV).
Normal Value And Calculation:
Normal Value: Normal value of pulmonary ventilation is 6000 mL (6 liters)/minute.
Read And Learn More: Medical Physiology Notes
Calculation:
Pulmonary ventilation is the product of tidal volume (TV) and the rate of respiration (RR). It is calculated by the formula:
Pulmonary Ventilation
= Tidal volume × Respiratory rate
= 500 mL x 12/minute
= 6,000 mL/minute
Alveolar Ventilation
Alveolar Ventilation Definition:
The alveolar ventilation is the amount of air utilized for gaseous exchange every minute.
- Alveolar ventilation is different from pulmonary ventilation.
- In pulmonary ventilation, 6 L of air moves in and out of the lungs in every minute. But the whole volume of air is not utilized for the exchange of gases.
- The volume of air subjected to the exchange of gases is alveolar ventilation.
- The air trapped in the respiratory passage (dead space) does not take part in gaseous exchange.
Normal Value And Calculation:
Normal Value: Normal value of alveolar ventilation is 4,200 mL (4.2 liters)/ minute.
Calculation:
It is calculated by the formula given below. Alveolar ventilation
= (Tidal volume – Dead space volume) × Respiratory rate
= (500- 150) x 12 = 4,200 mL (4.2 liters)/minute
Dead Space
Dead Space Definition:
Dead space is defined as the part of the respiratory tract, where gaseous exchange does not take place.
- The air present in the dead space is called dead space air.
- The parts of the respiratory tract, which form the dead space are the nose, pharynx, trachea, bronchi, and branches of bronchi up to terminal bronchioles.
- These structures serve only as the passage for air movement. Gaseous exchange does not take place in these structures.
Types Of Dead Space:
Dead space is of two types:
- Anatomical dead space
- Physiological dead space.
Anatomical Dead Space:
It is the volume of respiratory tract from the nose up to the terminal bronchiole.
Physiological Dead Space:
Physiological dead space includes the anatomical dead space plus two additional volumes.
- These two additional volumes are generally considered as wasted ventilation.
- The additional volumes included in physiological dead space are:
- The air in the alveoli, which are non-functioning.
- In some of respiratory diseases, alveoli do not function because of dysfunction or destruction of the alveolar membrane
- The air in the alveoli, which do not receive adequate blood flow. Gaseous exchange does not take place during inadequate blood supply.
Wasted air:
- The dead space air is generally considered wasted air.
- Wasted air refers to air that is not utilized for gaseous exchange.
Normal Value Of Dead Space:
Under normal conditions, the physiological dead space is equal to the anatomical dead space.
- It is because all the alveoli are functioning and all alveoli receive adequate blood flow in normal conditions.
- The volume of normal dead space is 150 mL.
In respiratory disorders, which affect the pulmonary blood flow or the alveoli, the dead space increases. - It is associated with a reduction in alveolar ventilation.
Measurement Of Dead Space- Nitrogen Washout Method:
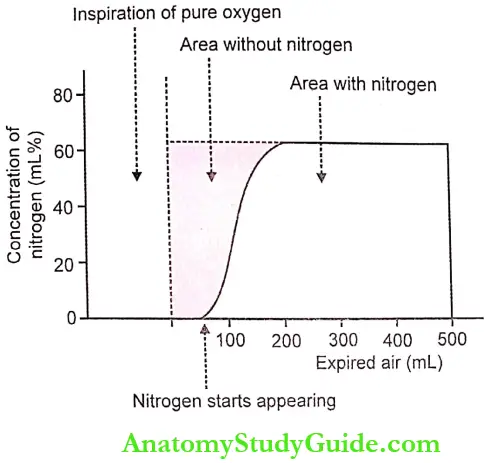
The dead space is determined by the single breath nitrogen washout method.
- The subject respires normally for a few minutes. Then, he takes a sudden inhalation of pure oxygen.
- The oxygen replaces the air in dead space (air passage), i.e. the dead space air contains only oxygen, * pushes the other gases into alveoli.
- Now. the subject exhales through a nitrogen meter. TTogsrr meter shows the concentration of nitrogen in Ine expired air continuously.
- The first portion of expired air comes from the upper part of the respiratory tract or air passage which only oxygen.
- The next portion of expired air comes from the alveoli, which contain nitrogen.
- Now, the nitrogen meter shows the nitrogen concentration, which rises sharply and reaches the plateau soon.
- By using data obtained from the nitrogen meter, a graph is plotted. From this graph, the dead space is calculated.
- The graph has two areas, the area without nitrogen and the area with nitrogen. The area of the graph is measured by a planimeter.
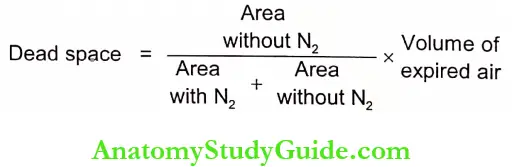
The area without nitrogen indicates dead space air. It is calculated by the formula:
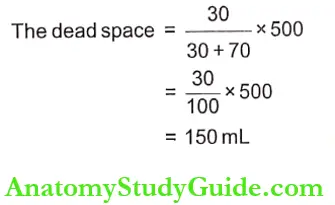
For example, in a subject:
- Area with nitrogen = 70sq.cm.
- Area without nitrogen = 30sq.cm.
- The volume of air expired =500mL
Ventilation – Perfusion Ratio
Ventilation – Perfusion Ratio Definition:
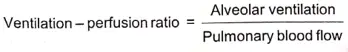
The ventilation-perfusion ratio is the ratio of alveolar ventilation and the amount of blood that perfuses the alveoli.
It is expressed as VA/Q:
- VA is alveolar ventilation
- Q is the blood flow (perfusion)
Normal Value And Calculation:
Normal Value: The normal value of the ventilation-perfusion ratio is about 0.84.
Calculation: Alveolar ventilation is calculated by the formula:
Alveolar ventilation
Alveolar ventilation = (Tidial volume – Dead space) x Respiratory rate
= (500-150) x 12
= 4,200 mL/minute
Blood flow through alveoli (Pulmonary blood flow)
= 5,000 mL/minute
Therefore, the Ventilation-perfusion ratio
= 4,200/5,000
= 0.84
Significance Of Ventilation – Perfusion Ratio:
The ventilation-perfusion ratio signifies the gaseous exchange. It is affected if there is any change in alveolar ventilation or in blood flow.
Wasted Air And Wasted Blood:
- The ventilation-perfusion ratio is not perfect because of the existence of two factors on either side of the alveolar membrane.
- The two factors are physiological dead space and physiological shunt.
- Physiological dead includes wasted air (see above) and physiological c birr includes wasted blood.
Variations In Ventilation – Perfusion Ratio:
Physiological Variation:
- The ratio increases, if ventilation increases without any change in blood flow
- The ratio decreases if blood flow increases without any change in ventilation
- In a sitting position, there is a reduction in blood flow in the upper part of the lungs (zone 1) than in the lower part (zone 3).
- Therefore, in zone 1 of the lungs ventilation-perfusion ratio increases three times.
- At the same time, in zone 3 of the lungs, because of increased blood flow.
- The ventilation-perfusion decreases.
Pathological Variation:
In chronic obstructive pulmonary disease (COPD), ventilation is affected because of obstruction and destruction of the alveolar membrane. So, the ventilation-perfusion ratio reduces greatly.
Leave a Reply