Actinomycosis
Actinomycosis is a chronic suppurative disease caused by anaerobic bacteria of the genus, Actinomycetes (most commonly A. israelii). The disease is conventionally included in mycology though it is caused by filamentous bacteria and not true fungus although its name sounds like one.
Table of Contents
- The disease is worldwide in distribution. The organisms are commensals in the oral cavity, alimentary tract and vagina. The infection is always endogenous in origin and not by person-toperson contact.
- The organisms invade, proliferate and disseminate in favourable conditions like breaks in mucocutaneous continuity, some underlying disease etc.
Read And Learn More: General Pathology Notes
The main Topics
- Chronic inflammation—types and general feature
- Common examples of granulomatous inflammation
- Tissue repair—general aspects, and
- Selected examples of tissue repair.
Morphologic Features:
Depending upon the anatomic location of lesions, actinomycosis may have different forms but the most common locations are oral-cervicofacial, thoracic, abdominal and pelvic.
- Oral-cervicofacial actinomycosis: This is the commonest form (60%) and has the best prognosis. The infection enters from tonsils, carious teeth, periodontal disease or trauma following tooth extraction. Initially, a firm swelling develops in the lower jaw (‘lumpy jaw’).
- In time, the mass breaks down and abscesses and sinuses are formed. The discharging pus contains typical tiny yellow sulphur granules. The infection may extend into adjoining soft tissues and may destroy the bone.
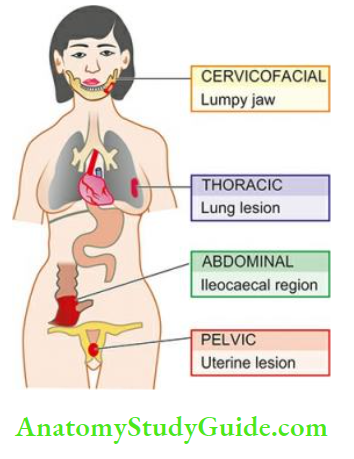
- Thoracic actinomycosis:The infection in the lungs is due to aspiration of the organism from oral cavity or extension of infection from abdominal or hepatic lesions. Initially, the disease resembles pneumonia but subsequently, the infection spreads to the whole of lung, pleura, ribs and vertebrae.
- Abdominal actinomycosis: This type presents as an abscess, commonly in the appendix, caecum and liver. The abdominal infection results from swallowing of organisms from oral cavity or extension from thoracic cavity.
- Pelvic actinomycosis: Infection in the pelvis occurs most often as a complication of intrauterine contraceptive devices (IUCDs) and begins as endometritis.
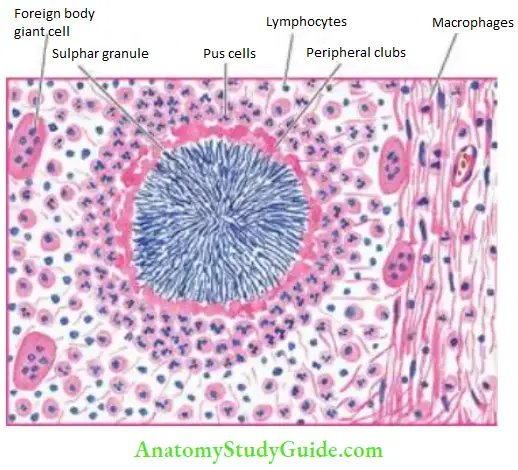
Microscopically: Irrespective of the location of actinomycosis, the following features are seen
- The inflammatory reaction is a granuloma with central suppuration. There is a formation of abscesses in the centre of lesions and at the periphery chronic inflammatory cells, giant cells and fibroblasts are seen.
- The centre of each abscess contains the bacterial colony, ‘sulphur granule’, characterised by radiating filaments (hence previously known as ray fungus) with hyaline, eosinophilic, club-like ends representing secreted immunoglobulins.
- Bacterial stains reveal the organisms as gram-positive filaments, nonacid-fast, which stain positively with Masson’s trichrome and Gomori’s methenamine silver (GMS) stains.
Clinically: Actinomycosis is characterised by a classic triad of features:
- Progression across mucous membranes, chronicity and mass-like lesion.
- Development of a sinus tract which may resolve and relapse spontaneously.
- Relapse of infection after short course of therapy since it requires long-term treatment.
Actinomycosis:
- Actinomycosis is a chr onic suppurative disease caused by anaerobic bacteria
- Actinomycetes israelii, though the name of disease sounds like a fungus.
- Depending upon the anatomic location, actinomycosis is of 4 main types:
- Oral cervicofacial (commonest, appearing as the lumpy jaw),
- Thoracic
- Abdominal and
- Pelvic.
- Microscopically, the lesions have an abscess containing the bacterial colony as sulphur granule and surrounded by granulation tissue.
- Clinically, actinomycosis presents as a chronic inflammatory mass developing in mucosal locations, developing sinus tract in due course of time, and relapses after short course of therapy since it requires prolonged treatment.
Sarcoidosis (Boeck’S Sarcoid):
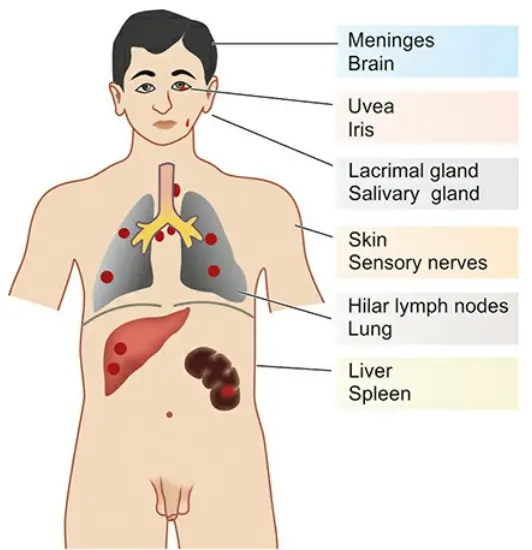
Sarcoidosis is a multisystem inflammatory disease of unknown etiology. It is worldwide in distribution and affects adults from 20-40 years of age. The disease is characterised by the presence of non-caseating epithelioid cell granulomas (‘sarcoid granuloma’) in the affected tissues and organs, notably in the lungs, lymph nodes, liver, skin and eye.
Other involved sites are the uvea of the eyes, spleen, salivary glands, liver and bones of hands and feet.
Etiology and Pathogenesis:
The cause of sarcoidosis remains unknown. Currently, the aetiology is explained on the basis of three interlinked factors:
- Genetic predisposition
- Exposure to an environmental agent
- Cellular immune response
1. Genetic predisposition:
Although no consistent genetic loci have been found, there is development of sarcoidosis in certain HLA class II haplotype, HLA-DRB1, HLA-A1, and HLA-B8.
2. Exposure to environmental agent:
Infectious and noninfectious environmental agents acting that initiates the immunologic inflammatory response have long been suspected.
Possible infectious agents are mycobacteria or their antigenic proteins, atypical mycobacteria, Propionibacterium acnes, or certain moulds. Noninfectious agents include exposure to insecticides. It is also likely that more than one agent may be involved.
3. Cellular immune response:
The disease is characterised by granulomatous tissue reaction, indicative of expression of cell-mediated immune mechanism:
- Antigen-presenting cells (i.e. dendritic cells or macrophage) present an unknown antigen to
helper T cells. - Clusters of macrophages and helper T cells on activation release several cytokines—IL-2, IFN-γ, IL-8, IL-10, IL-12, IL-18 and TNF.
- These multiple cytokines form the granuloma in which macrophages predominate but T cells have a necessary role in initial inflammatory reaction.
Thus, interlinking these three factors, it can be summed up that lesions of sarcoidosis in the target organ occur in a Genetically predisposed host After exposure to infectious or noninfectious environmental agent
That triggers granulomatous inflammatory response by initiating immune response involving antigen-presenting cells, helper T cells and by release of multiple cytokines
Kveim’S Test:
It is a useful intradermal diagnostic test based on the immune pathogenesis of the disease. The antigen prepared from involved lymph node or spleen is injected intradermally.
In a positive test, nodular lesion appears in 3-6 weeks at the inoculation site which on microscopic examination shows the presence of non-caseating granulomas.
Morphologic Features:
The lesions in sarcoidosis are generalised and may affect various organs and tissues at some point of time in the course of disease. However, brunt of the disease is borne by the lungs;
other commonly affected organs are lymph nodes, skin, liver and eye .
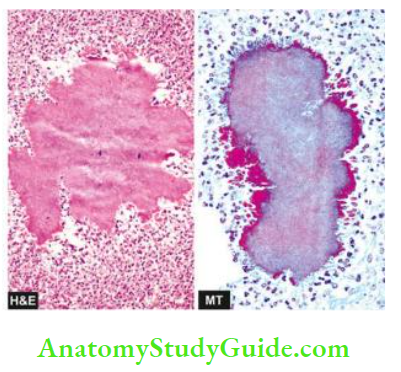
Microscopically: The diagnosis is generally made by exclusion of other causes of granulomatous inflammation. However, following features favour sarcoidosis over other causes of granulomatous inflammation :
- Presence of non-caseating sarcoid granulomas, which are composed of epithelioid cells, Langhans’ and foreign body giant cells and surrounded peripherally by fibroblasts.
- However,at times fibrinoid necrosis, identified by brightly eospinophilic and fibrillary appearance, may
be seen in the centre of the granuloma. - Typically, granulomas of sarcoidosis are ‘naked’ i.e. devoid of peripheral rim of lymphocytes or there is paucity of lymphocytes.
- In late stage, the granuloma is either enclosed by hyalinised fibrous tissue or is replaced by hyalinised fibrous mass.
The giant cells in sarcoid granulomas may contain certain cytoplasmic inclusions as follows:
- Asteroid bodies which are eosinophilic and stellate-shaped structures.
- Schaumann’s bodies or conchoid (conch-like) bodies which are concentric laminations of calcium and of iron salts, complexed with proteins.
- Birefringent cytoplasmic crystals which are colourless. However, similar types of inclusions may be observed in chronic berylliosis.

Clinical Features And Diagnosis:
Clinical manifestations in sarcoidosis may range from asymptomatic to major organ dysfunction.
Since it is a multisystem disease, presenting features depend upon the site of predominant involvement.
However, main features are as under:
- Referable to lungs: Since lungs are involved in >90% cases, respiratory complaints such as dry hacking cough (due to tracheal compression by mediastinal lymphadenopathy) and dyspnoea are common.
- Other organ involvements: Some of the commonly affected sites are as under:
- Skin lesions are readily visible and appear as shiny maculopapular and nodular lesions.
- Ocular lesions as anterior uveitis
- Extrathoracic lymph node involvement
- Constitutional features: A few nonspecific systemic features are generally present. These are fatigue, low-grade fever, night sweats and weight loss.
- Clinically and pathologically, sarcoidosis mimics tuberculosis and its diagnosis is made by exclusion but treatment of the two conditions is quite different. Unlike tuberculosis, definite etiology of sarcoidosis is not known. In general, the following investigations favour diagnosis of sarcoidosis:
- Imaging studies, e.g. X-ray chest and CT scan indicating nodular infiltrate of the interstitial lung (ILD) and paratracheal lymphadenopathy
- Serum level of angiotensin-converting enzyme (ACE) is elevated, more often in acute disease (60%) than in chronic disease (20%).
- Tissue diagnosis by bronchoalveolar lavage (BAL), or endobronchial ultrasound-guided transbronchial needle aspirate (EBUS-NA), or biopsy from the lesion.
- AFB negative in sputum and cytologic material or tissue biopsy. Features distinguishing sarcoidosis from tuberculosis, which is a closely mimicking condition both clinically and histologically, are summed up in Table.
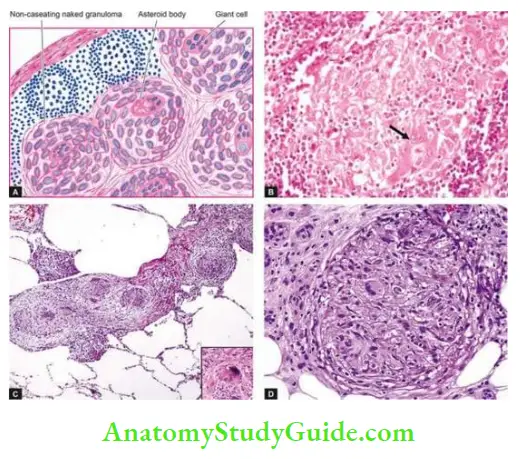
- (A) ,(B) – Sarcoidosis Lymph Nodes
- (C) – Sarcoidosis of the lung
- (D) – Sarcoidosis of the skin
Sarcoidosis:
- Sarcoidosis is a multisystem inflammatory disease of unknown etiology. It is worldwide in distribution and affects adults from 20 to 40 years of age.
- The disease is characterised by the presence of non-caseating epithelioid cell granulomas (‘sarcoid granuloma’) in the affected tissues and organs, notably lymph nodes, lungs, skin and eyes, which are naked granulomas i.e. devoid of lymphocytic infiltrate.
- The cause of sarcoidosis remains unknown. However, the disease has immune pathogenesis and involves interplay of 3 factors: genetic predisposition, exposure to an unknown infectious or non-infectious environmental agent, and cellular immune events causing granulomatous inflammation.
- Main presenting features pertain to the respiratory system, lymph nodes, skin or eye. The diagnosis is made by exclusion of other granulomatous conditions, notably tuberculosis, on clinical and pathologic findings.
Leave a Reply