Anterior Abdominal Wall
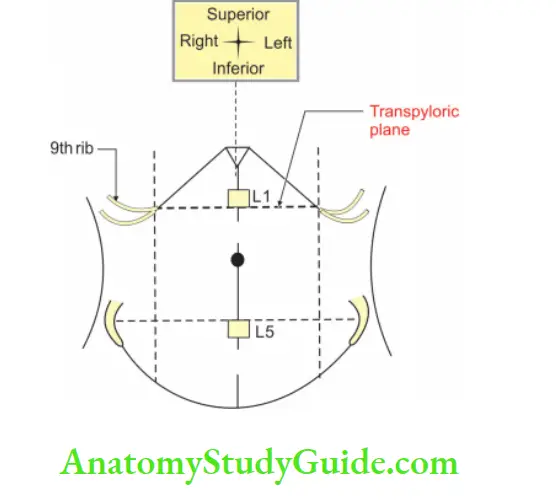
Transpyloric Plane (Addison’s plane)(Trans—across, pyloric—end of the stomach)
Transpyloric Plane Introduction: It is a horizontal plane passing through the pyloric end of the stomach.
Table of Contents
1. Transpyloric Plane Situation:
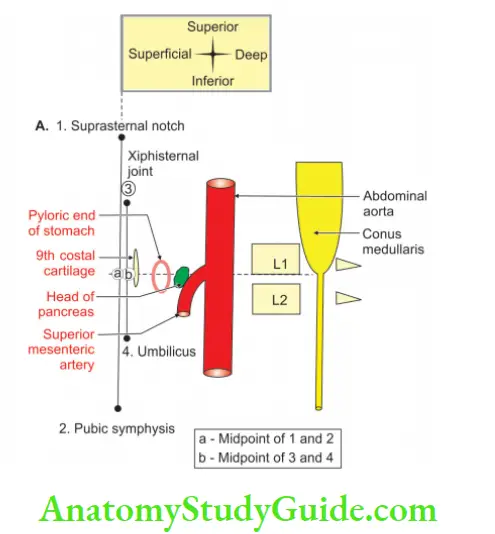
- It lies midway between suprasternal notch and upper end of pubic symphysis.
- It roughly corresponds with midpoint between xiphisternal joint and the umbilicus.
- Anteriorly, it is at tips of 9th costal cartilages.
- Posteriorly, it is at lower border of L1 (lower border of 1st lumbar vertebra) vertebra.
Read And Learn More: General Histology Question And Answers
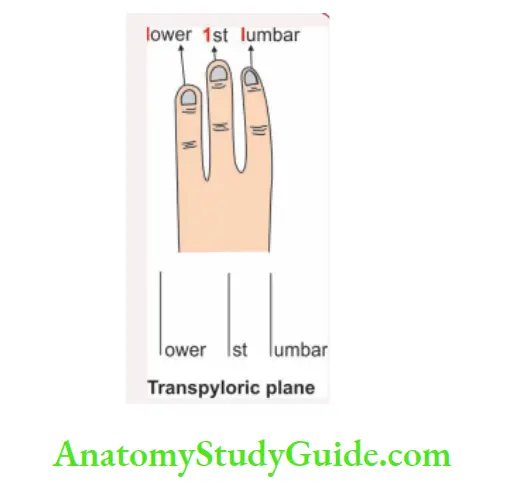
Transpyloric Plane is recollected by:
Transpyloric Plane Association memory:
Three vertical lines indicate “transpyloric plane” which is a horizontal plane
- 1st vertical line indicates “L” of lower.
- 2nd vertical line indicates the 1st.
- 3rd vertical line indicates “L” of lumbar.
2. Structures at the transpyloric plane are:
- Pyloric end of the stomach.
- Lower end of spinal cord.
- Origin of superior mesenteric artery.
- Lateral aortic group of lymph node.
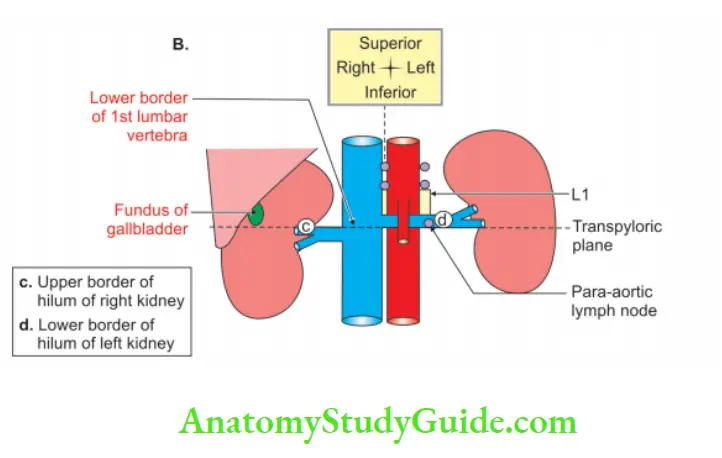
- Hila of both kidneys.
- Fundus of the gallbladder.
Visual memory:
ATM: Above structures can be recollected by visualizing structures from posterior to anterior.
1. First analyze the word “Transpyloric”. The word “transpyloric” indicates a transverse plane present at pyloric end of stomach.
1. Spinal cord passes trough vertebral canal which ends at transpyloric plane.
2. Anterior to vertebra we have abdominal aorta. The artery arising from abdominal aorta at this plane is superior mesenteric artery.
3.. The lymph nodes surrounding the aorta are called para-aortic lymph nodes and they are present at this level.
4. On both sides of vertebrae, we have kidneys.
- We know, right kidney is at lower level because of presence of liver on right side. The upper border of the hilum of right kidney is at this plane.
- The left kidney is at higher level. Hence the lower border of hilum of
left kidney is at this level. - On right side, we have part of the gallbladder below the inferior border of liver. It is the fundus of gallbladder.
Sites of Portocaval Anastomoses
1. Anterior abdominal wall
2. Posterior abdominal wall
3.Lower end of oesophagus
4. Lower end of rectum
5. Falciform ligament
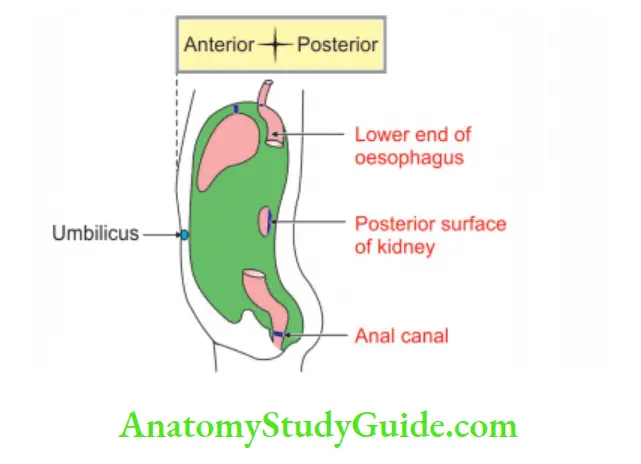
Caput medusae (Caput—head, Medusae—Greek myth, female ^ with snaky hair.)
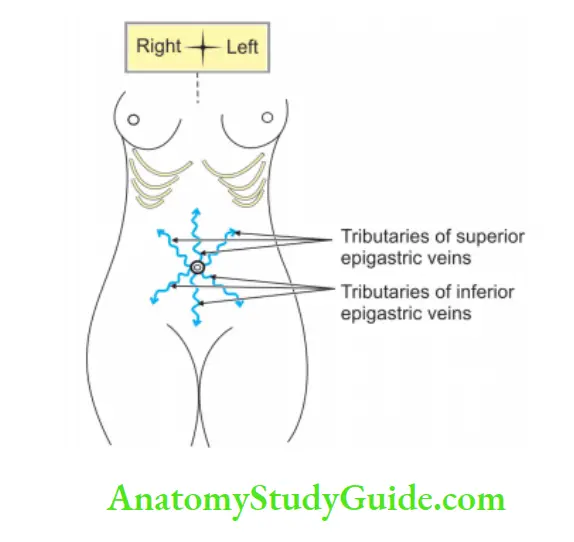
1. The umbilicus is one of the important sites of portocaval anastomosis.
2. There is anastomosis between tributaries of portal and tributaries of systemic veins. The veins are paraumbilical veins in the falciform ligament (tributaries of portal vein) and
Subcutaneous veins in the anterior abdominal wall (tributaries of epigastric veins which are tributaries of inferior vena cava) .
3. In case of portal hypertension, the blood from portal tributaries is directed into the caval tributaries causing their dilatation and tortuosity. This condition is referred to as ‘caput medusae’ because of its resemblance to the serpents on the head of Medusa, a mythical lady in Greek mythology.
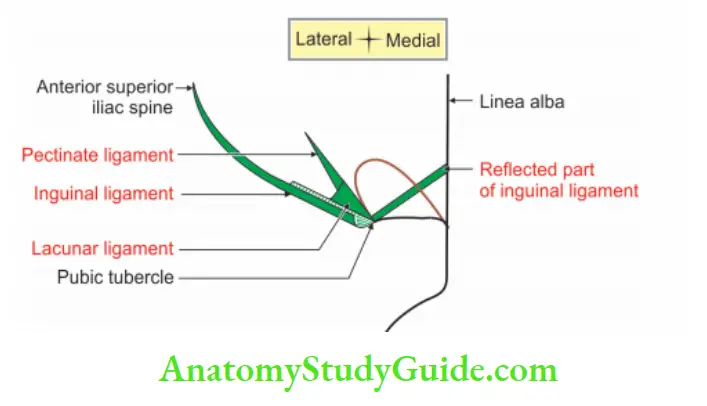
Inguinal ligament
Inguinal ligament Synonymous: Inguinal arch, arcus inguinalis, ligament of Poupart.
Inguinal ligament Introduction: It is a thickening of lower border of external oblique aponeurosis. It separates abdomen from thigh.
1. Inguinal ligament Extent: It extends from anterior superior iliac spine to pubic tubercle.
2. Inguinal ligament Features:
- It is thickening of lower border of external oblique muscle.
- It divides abdomen above and thigh below.
- It extends from anterior superior iliac spine to pubic tubercle.
3. Inguinal ligament Attachments:
1. Upper surface gives attachments to
- Internal oblique in lateral 2/3rd
- Transversus abdominis in lateral 1/3rd
- Cremaster muscle in middle part.
2. Fascia lata to lower border.
4. Inguinal ligament Relations:
1. Upper grooved part forms the floor of inguinal canal.
2. Its lodges
- Spermatic cord in male ♂
- Round ligament of uterus in female ♀
5. Extension:
1.Pectineal part of the inguinal ligament.:It is called lacunar ligament. It is ![]() lar in shape.
lar in shape.
- Anteriorly: It is attached to the medial end of the inguinal ligament.
- Posteriorly: It is attached to the pecten pubis. It is horizontal in position and supports the spermatic cord.
- Apex is attached to the pubic tubercle.
2. Pectineal ligament (ligament of Cooper): It is an extension of the inguinal ligament. It extends from posterior part of base of lacunar ligament. It is attached to the pecten pubis.
3. The reflected part of inguinal ligament: Extends from inguinal ligament to linea alba.
Rectus Abdominis
1. Proximal attachments: It arises by two tendinous heads as follows
- Lateral head from the lateral part of the pubic crest.
- Medial head from the anterior pubic ligament.
- The direction of the fibres is vertically and upwards.
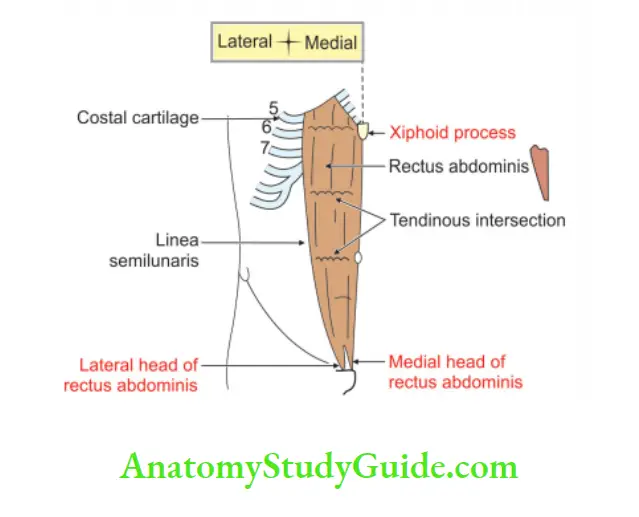
2. Rectus Abdominis Distal attachments: It is inserted along a horizontal line extending from the xiphoid process to the 7th, 6th and 5th costal cartilages.
3. Rectus Abdominis Nerve supply: Intercostal nerves (lower 6 or 7 thoracic spinal nerves).
4. Rectus Abdominis Action: Flexion of the trunk (lumbar spine).
Question – 1: Describe Rectus Sheath under the following heads
1. Rectus Sheath Formation
2. Rectus Sheath Contents, and
3. Rectus Sheath Applied Anatomy.
Answer:
Rectus Sheath Introduction: It is an aponeurotic sheath enclosing the rectus abdominis and pyramidal muscles.
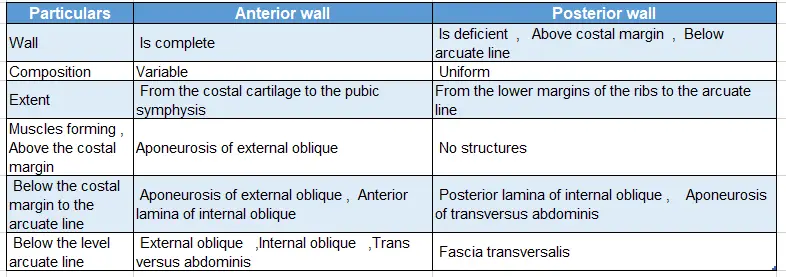
1. Rectus Sheath Formation
- Number: There is one on each side.
- Features: Given in the table
Formation of rectus sheath:
2. Rectus Sheath Contents
1. Muscles:
- Rectus abdominis
- Pyramidalis.
2. Arteries:
- Superior epigastric artery, a branch of the internal thoracic artery.
- Inferior epigastric artery, a branch of the external iliac artery.
3. Veins:
- Superior epigastric vein > internal thoracic vein > subclavian vein > superior vena cava.
- Inferior epigastric vein > external iliac vein > common iliac vein > inferior vena cava.
4. Nerves: Lower 5 intercostal nerves and subcostal nerves.
3. Rectus Sheath Applied anatomy
1. Divarication of recti:
In multiparous women and chronically weak children, the upper part of linea alba becomes stretched and the gap is produced between two recti.
2. Supraumbilical Median Incisions:
Supraumbilical Median Incisions Advantages: It is a bloodless area hence there is less bleeding during the operation.
Supraumbilical Median Incisions Disadvantages:
- It leaves a postoperative big scar.
- There is a delay in the healing of the wound.
3. Infraumbilical median incisions:
Infraumbilical median incisions Advantages: It prevents ventral hernia.
Infraumbilical median incisions Disadvantages:
- There is a delay in the healing of the wounds because of the low blood supply.
- The big scar is formed.
4. Advantage of paramedian incision: There is an early healing of the wound because of the rich blood supply.
5. Incisional hernia: Hernia through the incision taken for the surgery is called incisional hernia. It may be because of injury to spinal nerves.
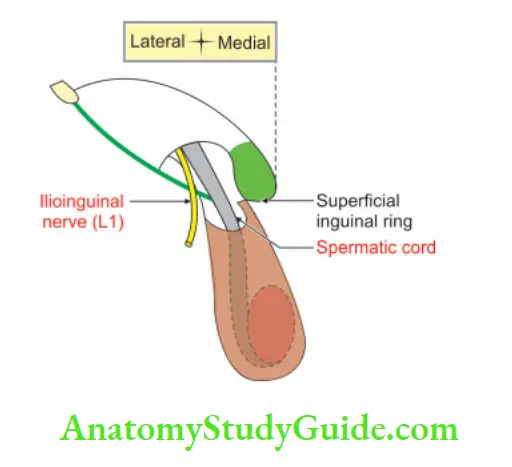
Question – 2: Name the contents of Inguinal Canal in male ♂
Answer:
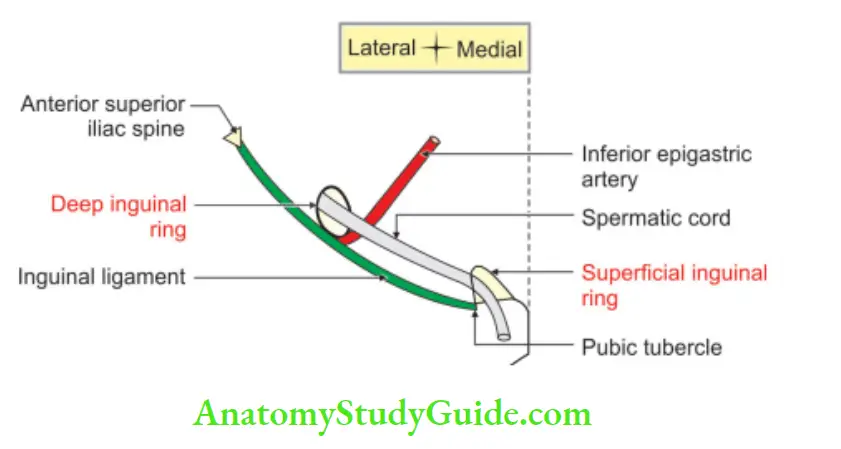
1. Spermatic cord in male ♂: It enters through the deep inguinal ring and comes out through the superficial inguinal ring of the inguinal canal.
2. Ilioinguinal nerve (L1): It lies outside the spermatic cord but inside the inguinal canal.
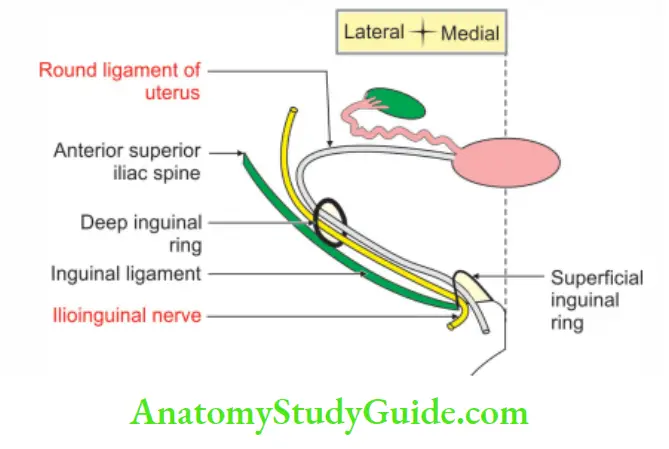
Question – 2: Name the contents of the inguinal canal in female ♀
1. Round ligament of uterus.
2. Ilioinguinal nerve.
Question – 3: Describe Inguinal Canal under the following heads
1. Inguinal Canal Gross anatomy
2. Inguinal Canal Development, and
3. Inguinal Canal Applied Anatomy.
Answer:
Inguinal Canal Introduction: It is an oblique passage or canal present in the lower part of the anterior abdominal wall for the passage of
- Spermatic cord in male ♂ or
- Round ligament of the uterus in female ♀
1. Inguinal Canal Gross anatomy
Situation: It is situated just U” above the midpoint of the inguinal ligament.
Extent: It extends from the deep inguinal ring to the superficial inguinal ring
Length: 1.5″ (4 cm)
Direction: Oblique, downwards, forwards and medially (same as the direction of fibres of external oblique muscle)
Gender variation: The canal is larger in males ♂ than in females ♀. This is because of the larger dimensions of the testis in males ♂.
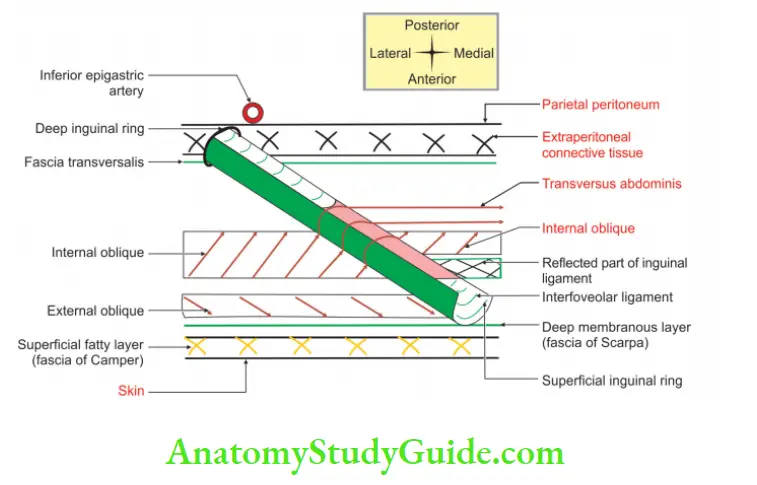
Inguinal Canal Boundaries:
1. Roof: Roof is formed by lower arched fibres of internal oblique and transversus abdominis.
2. Floor:
Laterally: Grooved surface of inguinal ligament.
Medially:
- The grooved surface of the inguinal ligament.
- The upper surface of lacunar ligament.
- Attachment of fascia transversalis with the inguinal ligament.
3. Inguinal Canal Anterior wall:
1. Laterally
- Skin
- Superficial fascia
- External oblique aponeurosis
- Internal oblique
2. Medially
- Skin.
- Superficial fascia
- External oblique aponeurosis
4. Inguinal Canal Posterior wall:
1. Laterally
- Interfoveolar ligament: It is a thickening in the fascia transversalis. It is present on the medial side of the deep inguinal ring. It is connected above to the transversal muscle and below
- Fascia transversalis.
- Extraperitoneal connective tissue.
- Parietal peritoneum.
2. Medially
- Reflected part of inguinal ligament.
- Fascia transversalis.
- Conjoint tendon formed by internal oblique and transversus abdominis.
- Extraperitoneal connective tissue.
- Parietal peritoneum.
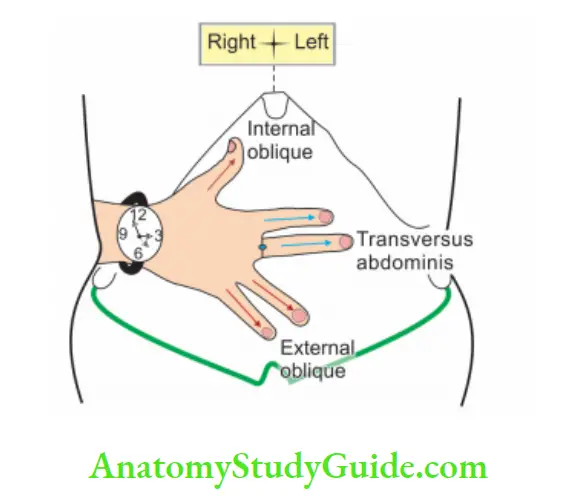 Direction of muscles of the anterior abdominal wall. “The directions are shown by the hands of the clock. 3 o’clock indicates the direction of the transversus abdominis, 4 o’clock indicates the direction of the external oblique, 11 o’clock indicates the direction of the internal oblique
Direction of muscles of the anterior abdominal wall. “The directions are shown by the hands of the clock. 3 o’clock indicates the direction of the transversus abdominis, 4 o’clock indicates the direction of the external oblique, 11 o’clock indicates the direction of the internal oblique
7. Inguinal Canal Contents:
1. Spermatic cord: In male ♂ and round ligament of uterus in female ♀ . It enters
through the deep inguinal ring and passes out through the superficial inguinal ring of the inguinal canal.
2. Ilioinguinal nerve: It is derived from 1st lumbar nerve. In the anterior abdominal wall, it lies in the neurovascular plane between the internal oblique and transversus abdominis muscles.
It is the content of the inguinal canal but it does not enter the canal through the deep inguinal ring. It pierces the internal oblique muscle and enters the inguinal canal.
It passes in front of the spermatic cord and leaves the canal through the superficial inguinal ring. It supplies the skin of the root of the penis and anterior 1/3rd of the scrotum in males ♂ and labium majus in females.
It also supplies a small area of the thigh below the medial end of the inguinal ligament.
8. Defensive mechanism of the inguinal canal: It is the mechanism by which the
abdominal contents normally are prevented from entering the inguinal canal.
These are as follows
1. Flap valve mechanism: The increased intra-abdominal pressure approximates anterior and posterior walls and obliterates the inguinal canal. ![]() .
.
2. Slit valve mechanism: The contraction of the external oblique approximates two cruris of the superficial inguinal ring ![]() .
.
3. Shutter mechanism: The contraction of the internal oblique closes the inguinal
the canal as a shutter ![]() .
.
4. Ball valve mechanism: The cremaster muscle contracts and draws upwards the constituents of the spermatic cord. These constituents aggregate at the superficial inguinal ring and act as a plug for the superficial inguinal ring![]()
5. Superficial: The inguinal ring is guarded by a conjoint tendon and reflected part of the inguinal ligament.
6. Deep: The inguinal ring is guarded by fibres of internal oblique.
7. Hormones: Play an important role in maintaining the tone of inguinal musculature.
2. Inguinal Canal Development
The canal is (developmentally) formed by the descent of the gubernaculum of the testis or ovary. In fetal life, the round ligament of the uterus is accompanied by a process of peritoneum. It usually disappears after birth. In females ♀ , if it persists after birth, it is called a canal of Nuck.
3. Inguinal Canal Applied anatomy
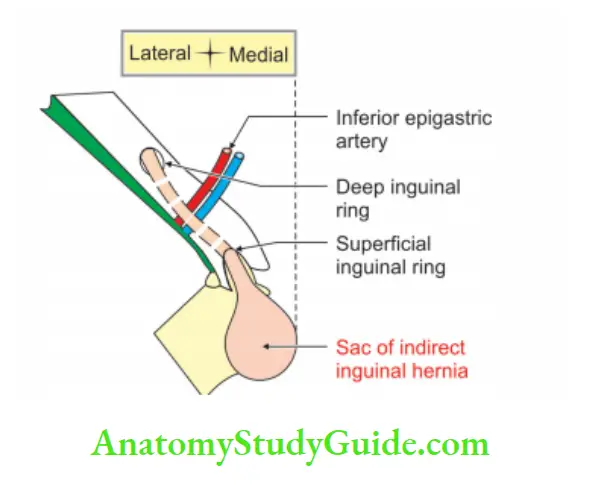
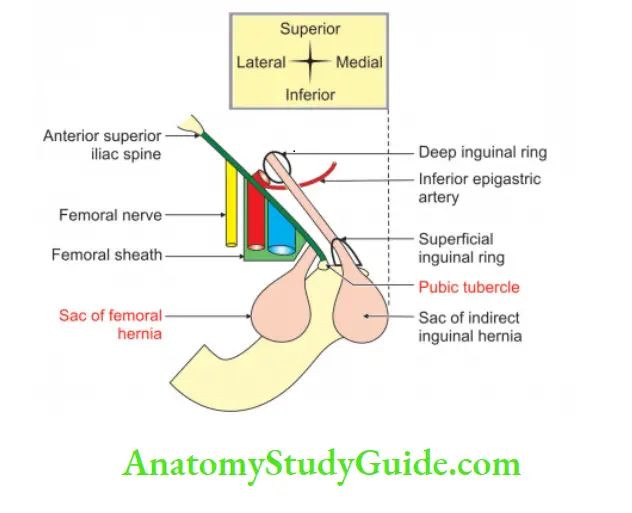
1. The inguinal canal is a region of potential weakness in the lower part of the anterior abdominal wall. Protrusion of abdominal contents through the inguinal canal is called inguinal hernia
2. If contents are pushed out indirectly through deep inguinal ring > inguinal canal.
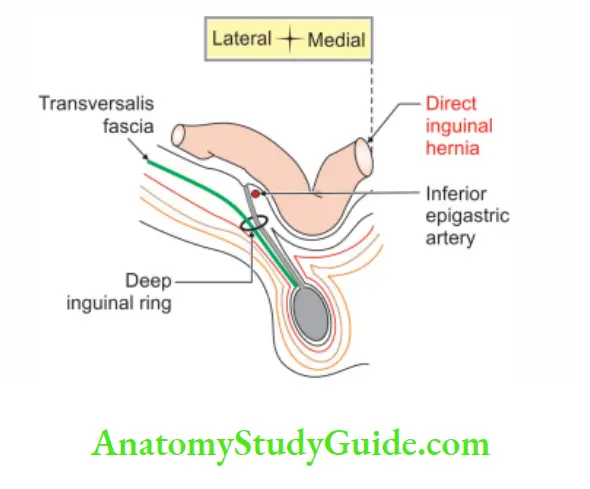
3. Superficial inguinal ring > scrotum, it is called indirect inguinal hernia It enters the inguinal canal through the deep ring lateral to the inferior epigastric artery.
4. If the contents are pushed out directly forward through the posterior wall of the inguinal canal. Superficial inguinal ring > scrotum, it is called ‘direct inguinal hernia’. The direct inguinal hernias pass medial to the inferior epigastric artery and lie medial to the spermatic cord.
- Medial direct inguinal hernia, and
- Lateral indirect inguinal hernia.
5. Inguinal hernias lie superior and medial to the pubic tubercle. This is in contrast to the femoral hernias which lie inferior and lateral to the pubic tubercle
6. Direct inguinal hernias are more frequent in old persons. In old age, muscles become lax due to loss of tone and power. The lax muscles yield easily following a
1. Heavy strain
2. Chronic cough
3. Constipation, and
4. Bladder Outlet Obstruction. It is commonly called BOO are
- Stricture of urethra
- Meatal stenosis
- Cancer of bladder
- Prostatitis, and
- Prostatic abscess.
Lacunar Ligament
Lacunar Ligament Introduction: Lacunar ligament is pectineal part of inguinal ligament.
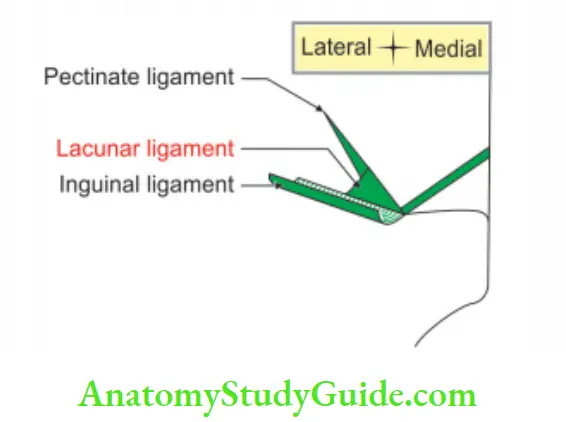
1. Lacunar Ligament Features:
- It is
 lar.
lar. - It forms the medial boundary of the femoral ring.
- It is strengthened by
- Pectineal fascia, and
- Linea alba.
2. Lacunar Ligament Attachments:
- Anteriorly to the medial end of the inguinal ligament.
- Posteriorly to pectin pubis
- Apex is attached to the pubic tubercle.
3. Lacunar Ligament Function: It supports the spermatic cord.
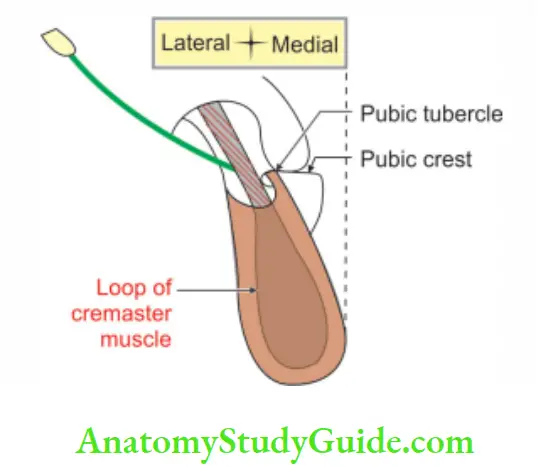
Attachments to Pubic Tubercle
1. Medial end of inguinal ligament
2. Medial ends of the loop of the cremaster
Superficial Inguinal Ring
1. Superficial Inguinal Ring Location: It is situated 1 cm above the pubic tubercle.
2. Superficial Inguinal Ring Formation: It is formed in the external oblique muscle.
3. Superficial Inguinal Ring Shape: It is ![]() lar in shape.
lar in shape.
4. Superficial Inguinal Ring Axis: It is oblique.
5. Superficial Inguinal Ring Dimension:
- Length: 1
- Breadth: ½
6. Superficial Inguinal Ring Relations:
1. Anterior:
- Skin, and
- Superficial fascia.
2. Medial: Pubic tubercle.
3. Lateral: Inferior crus of external oblique muscle which is attached to the pubic tubercle.
4. Posterior:
- Conjoint tendon.
- Reflected part of the inguinal ligament.
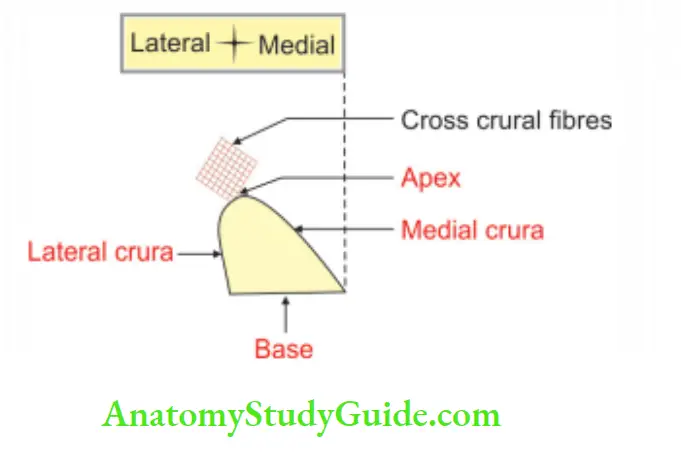
7. Superficial Inguinal Ring Contents:
- Ilioinguinal nerve.
- Spermatic cord or round ligament of uterus.
Deep Inguinal Ring
1. Deep Inguinal Ring Location: It is situated 1 cm above the mid-inguinal point.
2. Deep Inguinal Ring Formation: It is present in the fascia transversalis.
3. Deep Inguinal Ring Shape: It is oval ‘ hi shape.
4. Deep Inguinal Ring Axis: It is vertical.
5. Deep Inguinal Ring Relations:
- Anterior: Arched fibres of transversus abdominis.
- Medial: Inferior epigastric artery.
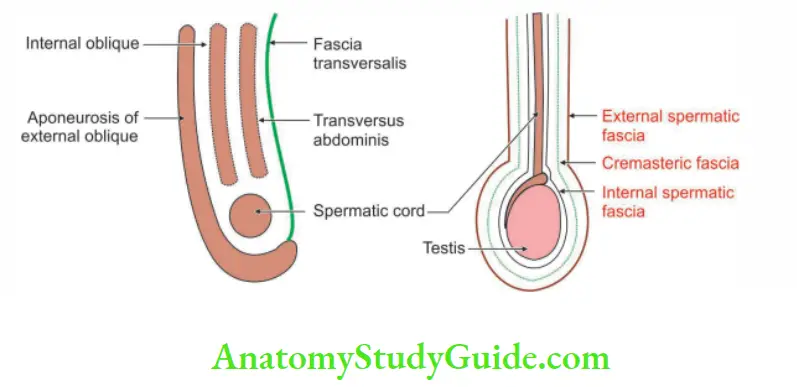
Coverings of Spermatic Cord
Coverings of spermatic cord: These are described from superficial to deep.
1. External spermatic fascia: It is formed by the external oblique. It covers the cord below the superficial inguinal ring.
2. Cremasteric fascia: It is derived from the internal oblique and transversus abdominis muscle. It covers the cord below the level of these muscles.
3. Internal spermatic fascia: It is derived from fascia transversalis. It covers the cord to the whole extent.
Spermatic Cord
Spermatic Cord Introduction: Each testis develops in the lower thoracic and upper lumbar regions. It migrates into the scrotum. During its descent, it carries “vas deferens” with its vessels, nerves, etc. It is one on each side.
1. Spermatic Cord Gross
- Length: 7 cm.
- Extent: It extends from the upper pole of the testis to the deep inguinal ring.
- Course: It ascends in the scrotum and enters the inguinal canal to the superficial inguinal ring. It passes through the inguinal canal and ends at the deep inguinal ring.
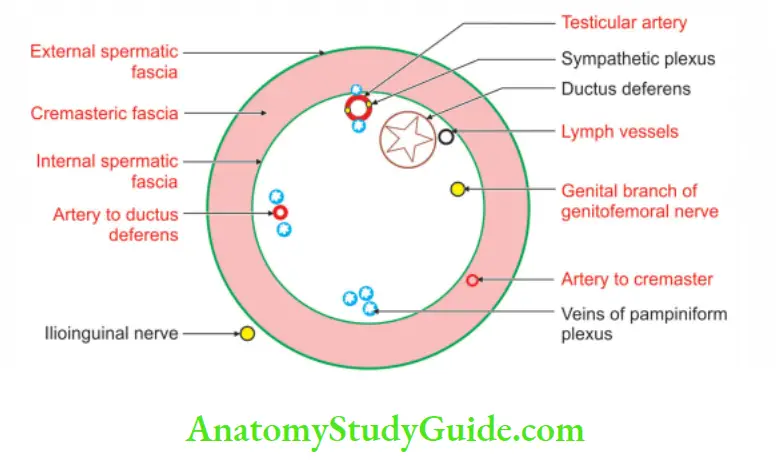
2. Spermatic Cord Constituents are grouped as
1. Deep to internal spermatic fascia
“Vas deferens”: It starts at the tail of epididymis. At the upper pole of the testis, it is accompanied by other constituents of the spermatic cord. At the deep inguinal ring, it leaves all the structures and enters the abdomen.
Artery to vas: It is a branch of the inferior or superior vesical artery, which is a branch of the anterior division of the internal iliac artery.
Structures in relation to testis:
- Testicular artery: It is a branch of the abdominal aorta.
- Testicular sympathetic plexus: It is formed by renal and aortic plexus.
- Testicular lymph vessels: They drain into the lateral aortic group of lymph nodes.
- Pampiniform plexus
Genital: Branch of genitofemoral nerve supplies cremaster muscle.
2. Between external and internal spermatic fascia: Artery to cremaster, a branch of the inferior epigastric artery.
3. Outside spermatic cord: Ilioinguinal nerve
3. Spermatic Cord Applied anatomy
- Vasectomy: It is the surgical removal of the “vas deferens” or a portion of it. It is one of the most common operations done for family planning.
- Varicocele: The dilatation and tortuosity of pampiniform plexus in the spermatic cord is called varicocele. It mainly occurs on the left side.
- Torsion of the spermatic cord: Torsion (twisting) of the spermatic cord results in the death of the testis. Hence, it is a surgical emergency.
Hesselbach’s (Trigonum inguinale—Inguinal trigone)
Hesselbach’s Introduction: It is a ![]() lar area present on the anteroinferior wall of the abdomen.
lar area present on the anteroinferior wall of the abdomen.
1. Hesselbach’s Boundaries: It is bounded.
- Medially by the lateral border of the rectus abdominis muscle.
- Laterally by the inferior epigastric artery.
- Base by the inguinal ligament.
- Floor by the posterior wall of the inguinal canal.
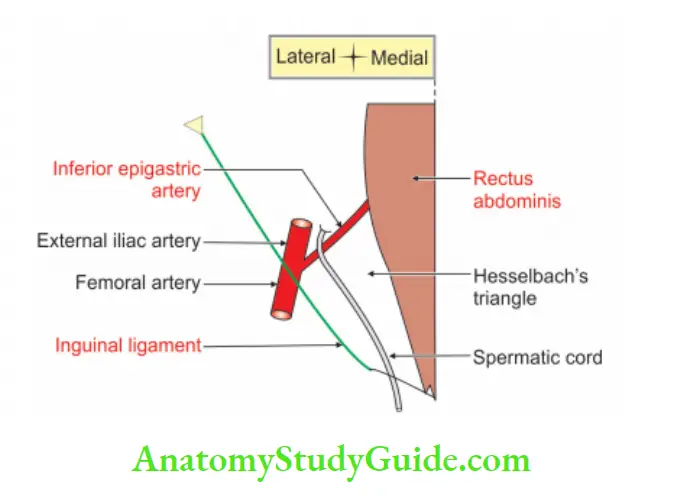
2. Hesselbach’s Distribution: Inguinal hernia is divided into two types depending upon the relation in the Hesselbach’s
![]()
1. If the hernia is passing laterally to the Hesselbach’s hernia.![]() , it is called an indirect inguinal hernia.
, it is called an indirect inguinal hernia.
2. If a hernia passes through the Hesselbach’s ![]() , it is called a direct inguinal hernia (i.e. medial to the inferior epigastric artery). Direct inguinal hernia is again subdivided into.
, it is called a direct inguinal hernia (i.e. medial to the inferior epigastric artery). Direct inguinal hernia is again subdivided into.
- Lateral direct inguinal hernia: It lies lateral to the obliterated umbilical artery. The contents of the direct hernia enter through the medial inguinal fossa.
- Medial direct inguinal hernia: It lies medial to the obliterated umbilical artery. The contents of the hernia enter through the supravesical fossa.
3. Hesselbach’s Characters:
Inguinal hernia passing through Hesselbach’s ![]()
- It is acquired.
- It is usually bilateral and occurs in old age.
4. Hesselbach’s Applied Anatomy:
1. In a long-standing hernia, the inferior epigastric artery helps to differentiate between direct and indirect inguinal hernias.
2. It is an anatomical landmark to
- Differentiate between direct and indirect hernias, and
- Recognize the neck of the hernial sac.
Question – 4 : What is inguinal hernia?
The inguinal canal is a region of potential weakness in the lower part of the anterior abdominal wall. Therefore, following an increased intra-abdominal pressure, the abdominal contents are pushed out through an inguinal canal called an inguinal hernia.
Inguinal Hernia
Inguinal Hernia Introduction: It is an abnormal protrusion of abdominal contents through the weak point of the abdominal wall.
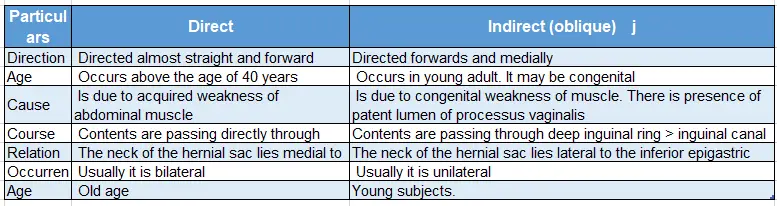
1. Inguinal Hernia Classification:
1. Based on the situation of the contents of the hernia.
Inguinal Hernia Direct (old age): If the contents are pushed out directly forward through the posterior wall of the inguinal canal > superficial inguinal ring > scrotum, it is called a ‘direct inguinal hernia’.
If the hernia is medial to the inferior epigastric artery, it is diagnosed as a direct inguinal hernia. These are subdivided depending upon the relation to the obliterated umbilical artery.
- Medial: Contents of hernia are medial to obliterated umbilical artery.
- Lateral: Contents of hernia are lateral to obliterated umbilical artery.
Inguinal Hernia Indirect (oblique): If contents are pushed out indirectly through deep inguinal ring> inguinal canal > superficial inguinal ring into the scrotum, it is called
indirect inguinal hernia. Indirect inguinal hernias enter the inguinal canal through the deep ring.
It is lateral to the inferior epigastric artery and lies within the spermatic cord.
- Congenital.
- Acquired.
2. Inguinal Hernia Features:
1. Inguinal hernia lies superior and medial to the pubic tubercle. This is in contrast to the femoral hernias.
2. Direct inguinal hernias are more frequent in old persons. In old age, muscles become lax due to loss of tone and power. The lax muscles yield easily following a heavy strain, as in chronic cough and constipation.
3. Difference between direct and indirect hernias.
External Oblique Muscle of Anterior Abdominal Wall
1. Proximal attachments:
- The middle part of the shaft of the lower 8 ribs.
- The upper 4 slips get merged with the lower 4 digitations of the serratus anterior.
- Lower fibres get merged with the upper fibres of the latissimus dorsi.
- Direction of fibres: Downwards, medially and forwards.
2. Distal attachments: Fibres of the muscles are fleshy in proximal attachments and end in aponeurosis. The aponeurosis ends in
- Xiphisternum
- Linea alba
- Pubic symphysis
- Pubic crest, and
- Pectinate line of pubis
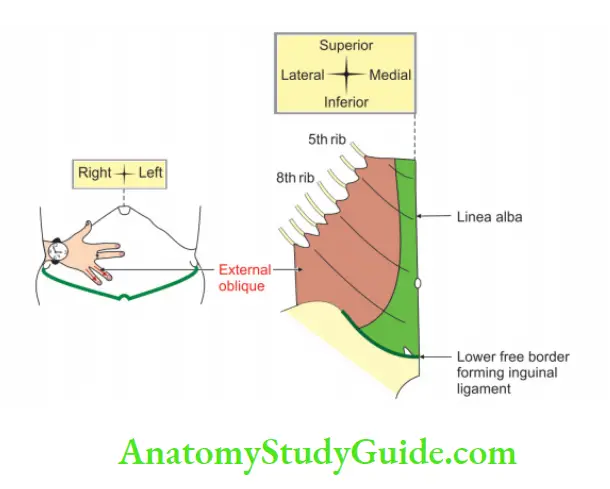
3. Actions:
- Lateral bending of the back
- With the opposite internal oblique, it brings rotation.
4. Nerve supply: Lower 6 thoracic spinal nerves
Transversus Abdominis Muscle:
1. Proximal attachments: Fibres of the muscles are fleshy in proximal attachments and end in aponeurosis. The fleshy part arises from
- Lateral 1/3rd of inguinal ligament
- Anterior 2/ 3rd of the outer lip of the ventral segment of the iliac crest.
- Thoracolumbar fascia, and
- The inner surface of lower 6 costal cartilages.
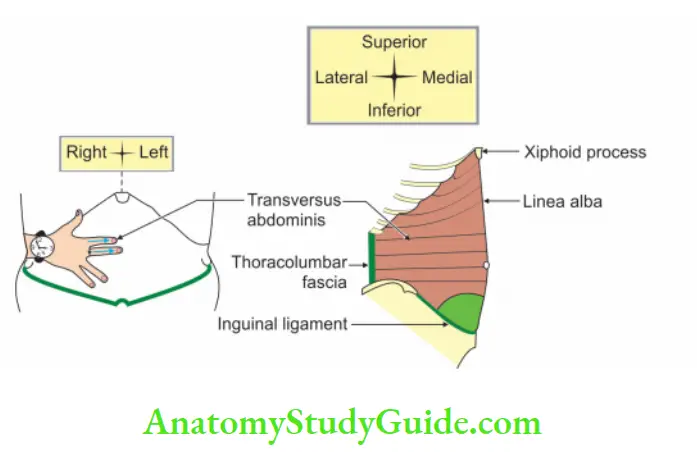
2. Direction of fibres: Runs horizontally
3. Distal attachments: Along a line of
- Xiphoid process
- Linea alba
- Pubic crest, and
- The pectineal line of the pubis
4. Nerve supply: Lower 6 thoracic nerves and first lumbar nerve.
Leave a Reply