Anterior Abdominal Wall
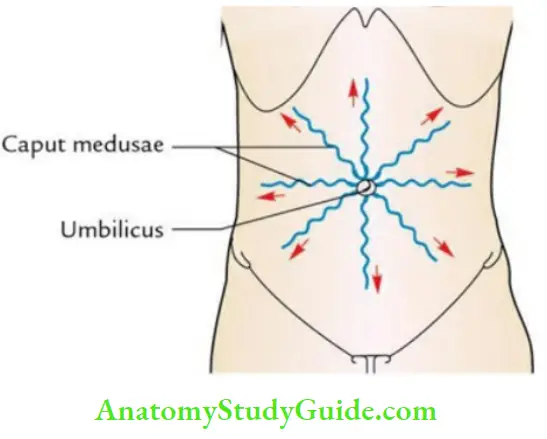
Question 1. Write a short note on the caput medusae.
Answer:
Caput Medusae Definition:
The caput medusae is a clinical sign characterized by the radiation of dilated and tortuous veins from the umbilicus like the spokes of a wheel.
Read And Learn More: Anatomy Question And Answers
Caput Medusae Anatomical basis
The umbilicus is one of the important sites of portocaval anastomosis.
- This anastomosis takes place between the paraumbilical veins in the falciform ligament (tributaries of the portal vein) and subcutaneous veins of anterior abdominal wall (tributaries of superior and inferior epigastric veins, which in turn are tributaries of inferior vena cava).
- In portal hypertension, the blood from portal tributaries is shunted into the caval tributaries, leading to dilatation and tortuosity.
- Such veins radiate from the umbilicus like the spokes of a wheel. This condition is termed caput medusae because of its resemblance to the head of Medusa, a mythical lady in Greek mythology who had serpents on her head instead of hair.
Anterior Abdominal Wall Layers
Question 2. Describe the umbilicus in brief and discuss its anatomical, embryological, and clinical importance.
Answer:
Umbilicus:
The umbilicus is a puckered scar made up of cicatricial tissue on the anterior abdominal in the midline and represents the site of attachment of the umbilical cord in fetal life. It lies at the level of the intervertebral disc between the L3 and L4 vertebrae.
Umbilical Cord
Umbilicus Anatomical importance:
- The skin around the umbilicus is supplied by T10 spinal segment.
- It is one of the important sites of portocaval anastomosis.
- With reference to the lymphatic and venous drainage of the anterior abdominal wall, the horizontal plane at the level of the umbilicus acts as a watershed line.
- Lymph from the skin above the umbilicus is drained into axillary lymph nodes, and from skin below the umbilicus into superficial inguinal lymph nodes.
- Venous blood from the skin above the plane of the umbilicus drains into axillary veins and from the skin below the plane of the umbilicus into great saphenous veins.
Umbilical Cord or Umbilicus Clinical importance:
- It is the most important soft tissue landmark on the anterior abdominal wall.
- It is of great cosmetic value; hence, surgical incision should not be given across the umbilicus.
- It is the site of referred pain of viscera supplied by the T10 spinal segment.
- It may be the site of the urinary fistula due to nonobliteration of the urachus.
- It is the site of exomphalos and congenital umbilical hernias.
- It may be the site of a fecal fistula.
- The umbilicus is therefore considered the hotbed of embryology by clinicians.
Question 3. Enumerate the muscles of the Anterior Adominal Wall.
Answer:
The anterior abdominal consists of 5 pairs of muscles: 3 pairs of flat muscles placed anterolaterally and 2 pairs of vertical muscles placed anteriorly on either side of the median plane.
Anterior Adominal Wall – Flat muscles:
- External oblique
- Internal oblique
- Transversus abdominis
Anterior Adominal Wall – Vertical muscles:
- Rectus abdominis
- Pyramidalis
Question 4. Give the origin, insertion, and nerve supply of the External Oblique Muscle.
Answer:
External Oblique Muscle Origin:
By 8 fleshy slips from the middle of the lower 8 ribs, interdigitating with serratus anterior and latissimus dorsi. The fibers run downward, forward, and medially.
External Oblique Muscle Insertion:
- By aponeurosis into the xiphoid process, linea alba, symphysis pubis, and pubic crest.
- By inguinal ligament into the anterior superior iliac spine and the pubic tubercle.
- By fleshy fibers into the anterior 2/3rds of the outer lip of the iliac crest.
External Oblique Muscle Nerve supply: By ventral rami of lower 6 thoracic spinal nerves (T7- T12).
Question 5. Give the origin, insertion, and nerve supply of the internal oblique muscle.
Answer:
Internal oblique muscle Origin: From before backward:
- Lateral 2/3rd of the inguinal ligament.
- Anterior 2/3rd of the intermediate area of the iliac crest.
- Thoracolumbar fascia.
The fibers run upward, forward, and medially, crossing the fibers of the external oblique the right angle.
Internal oblique muscle Insertion:
- Posterior part by fleshy fibers into the lower three or four ribs and their cartilages.
- The remaining muscle is inserted by aponeurosis into the 9th, 8th, and 7th costal cartilages, xiphoid process, linea alba, pubic crest, and pectineal line of the pubis.
Internal oblique muscle Nerve supply: By ventral rami of lower 6 thoracic spinal nerves and first lumbar nerve (T7–L1).
Question 6. Give the origin, insertion, and nerve supply of the transversus abdominis muscle.
Answer:
Transversus Abdominis muscle Origin: From before backward
- Lateral 1/3rd of the inguinal ligament.
- Anterior 2/3rd of the inner lip of the iliac crest.
- Thoracolumbar fascia.
- Inner surfaces of lower 6 costal cartilages interdigitating with the diaphragm.
Transversus Abdominis muscle Insertion:
- By broad aponeurosis into the xiphoid process and linea alba.
- By the conjoint tendon into the pubic crest and pectineal line of pubis.
Transversus Abdominis muscle Nerve supply: By ventral rami of lower 6 thoracic spinal nerves and first lumbar nerve (T7–L1).
Anterior Abdominal Wall Layers
Question 7. Write a short note on the Inguinal Ligament.
Answer:
Inguinal ligament:
The inguinal ligament is formed by the lower border of the aponeurosis of the external oblique muscle that has folded backward upon itself. It extends from the anterior superior iliac spine to the pubic tubercle in the inguinal region.
The inguinal ligament is convex downward (i.e. toward the thigh) where it gives attachment to fascia lata (the deep fascia of the thigh) and concaves toward the abdomen where it gives attachment to internal oblique and transverses abdominal muscles.
Note: The inguinal ligament is convex downward due to the downward pull exerted by the fascia lata.
Direct And Indirect Inguinal Hernia
Inguinal Ligament Extensions
- The extensions of the inguinal ligament are:
- Lacunar (Gimbernat) ligament
- Pectineal ligament (ligament of Cooper)
- Reflected part of the inguinal ligament
- Ilioinguinal ligament
Question 8. Give a brief account of the cremasteric muscle and add a note on the cremasteric reflex.
Answer:
1. Cremasteric muscle:
- The cremasteric muscle consists of muscle fasciculi that spring from the middle of the inguinal ligament.
- They form loops around the spermatic cord and testis; and get attached to the pubic tubercle, pubic crest, and conjoint tendon.
- The gaps between the loops are filled by cremasteric fascia.
- The cremaster muscle and cremasteric fascia together form the musculofascial sac to suspend the testis.
Cremasteric muscle Nerve supply:
- By the genital branch of the genitofemoral nerve (L1).
- Actions
- It suspends the testis and can be elevated by its contraction.
- It helps to close the superficial inguinal ring when intra-abdominal pressure is raised.
2. Cremasteric reflex:
- Upon stroking the skin of the upper part of the medial aspect of the thigh, there is a reflex contraction of the cremasteric muscle, leading to an elevation of the testis.
- The cremasteric reflex is brisk in children.
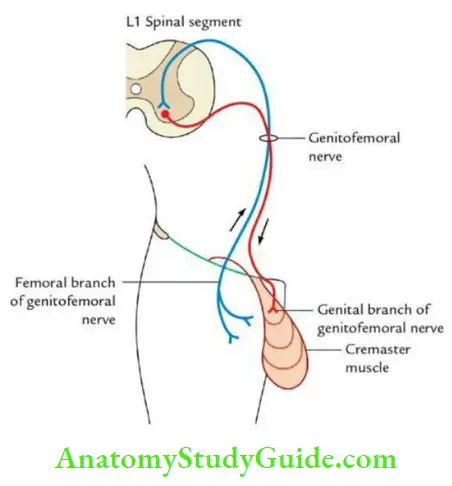
Note: This reflex is mediated by the L1 spinal segment. The afferent limb is formed by the femoral branch of the genitofemoral nerve and the efferent limb by the genital branch of the genitofemoral nerve. This reflex is lost in upper motor neuron lesions.
Question 9. Write a short note on conjoint tendon/falx inguinal.
Answer:
Conjoint Tendon/Falx Inguinalis:-
The conjoint tendon is formed by the fusion of the lower aponeurotic arching fibers of the internal oblique and transverses abdominal muscles. It is attached to the public crest and pectineal line. It lies in front of the rectus muscle. It strengthens the posterior wall of the inguinal canal in its medial 1/3rd opposite the superficial inguinal ring.
Anterior Abdominal Wall Layers
Question 10. Give the origin, insertion, and nerve supply of the rectus abdominis muscle.
Answer:
Rectus abdominis muscle Origin:
By two tendinous heads.
- Lateral head: From the lateral part of the pubic crest.
- Medial head: From the anterior pubic ligament.
Rectus abdominis muscle Insertion:
The fibers run vertically upward towards the costal margin and get inserted on the thoracic cage, along a horizontal line extending laterally from the xiphoid process and cutting in order the 7th, 6th, and 5th costal cartilages.
Rectus abdominis muscle Nerve supply: By the lower 6 or 7 thoracic spinal nerves (T5–T12/T6–T12).
Question 11. Enumerate the main actions of the muscles of the anterior abdominal wall.
Answer:
Direct And Indirect Inguinal Hernia
Main Actions Of The Muscles Of The Anterior Abdominal Wall:-
- Provide support and protection to abdominal viscera.
- Provide force for explosive acts, viz, defecation, micturition, and parturition.
- Play an important role in forceful expiratory acts such as coughing, sneezing, and nose blowing.
- Produce movements of the trunk, viz.
- Flexion, mainly by rectus abdominis muscles.
- Lateral flexion, by unilateral contraction of oblique muscles.
- Rotation, by a combined action of the external oblique muscle of one side and the internal oblique muscle of the opposite side.
Anterior Abdominal Wall Layers
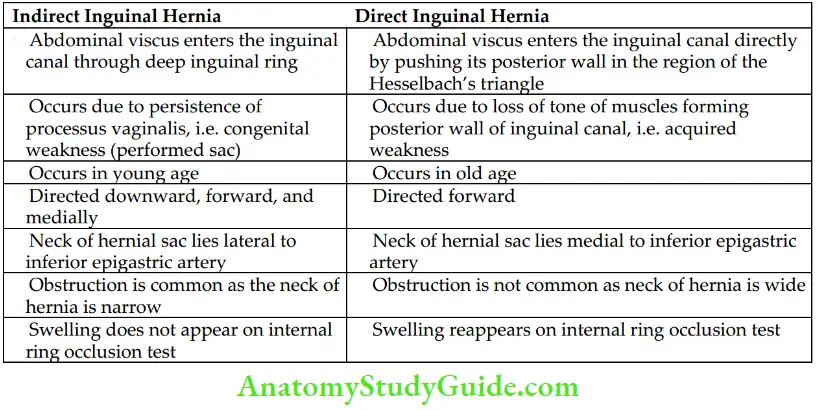
Question 14 . Give the differences between indirect and direct inguinal hernias.
Answer:
The differences between the direct and indirect inguinal hernias are given in Table
Differences between the Indirect and Direct Inguinal Hernias:’
Question 15. Enumerate the coverings of indirect inguinal hernia.
Answer:
Direct And Indirect Inguinal Hernia
From deep to superficial, these are:
- Peritoneal sac
- Extraperitoneal tissue
- Internal spermatic fascia
- Cremasteric muscle and fascia
- External spermatic fascia
- Dartos muscle
- Skin
Question 16. Enumerate the coverings of the Direct Inguinal Hernia.
Answer:
The coverings of the lateral and medial direct hernias from deep to superficial are given in Table.
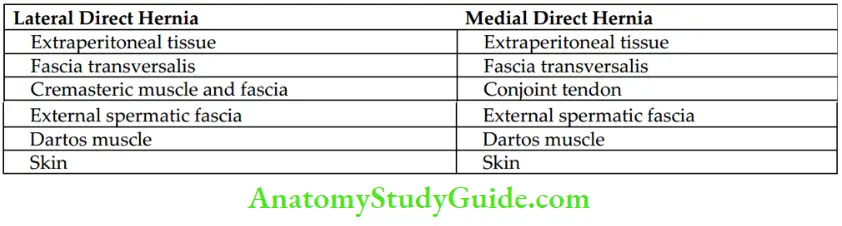
Coverings of the Lateral and Medial Direct Inguinal Hernia:
Question 17. Write a short note on Hesselbach’s triangle/inguinal triangle.
Answer:
Hesselbach’s Triangle:-
The Hesselbach’s triangle is a triangular area on the posterior aspect of the anteroinferior wall of the abdomen, above the medial half of the inguinal ligament.
Hesselbach’s triangle Boundaries:
- Lateral: Inferior epigastric artery.
- Medial: Lateral border of rectus abdominis muscle.
- Base: Medial half of the inguinal ligament.
- Floor: Conjoint tendon and fascia transversalis (posterior wall of the inguinal canal).
- Apex: Meeting point of the inferior epigastric artery and lateral border of the rectus abdominis muscle.
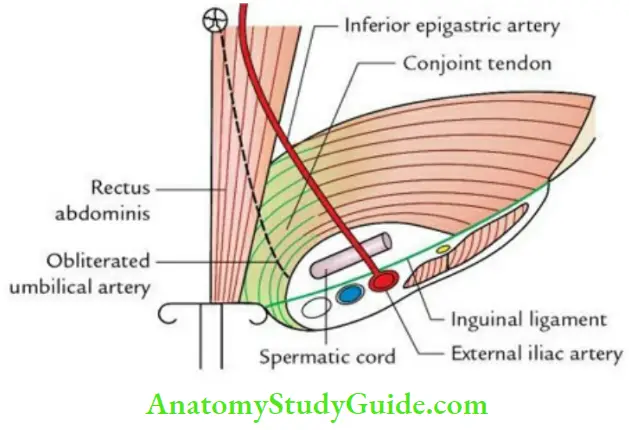
Note: Hesselbach’s triangle is divided into medial and lateral halves by the obliterated umbilical artery (lateral umbilical ligament).
Hesselbach’s triangle Applied anatomy: Hesselbach’s triangle is the site of a direct inguinal hernia.
Anterior Abdominal Wall Layers
Question 18. Write a short note on vas deferens/ductus deferens.
Answer:
Deferens/Ductus Deferens:-
The vas deferens is a thick-walled muscular tube measuring about 45 cm in length. It transports the spermatozoa from the epididymis to the ejaculatory duct.
Course and relations:
During its course, it traverses through 3 regions, viz. scrotum, spermatic cord, and lesser pelvis in successions. Accordingly, it is divided into 3 parts: 1st, 2nd, and 3rd.
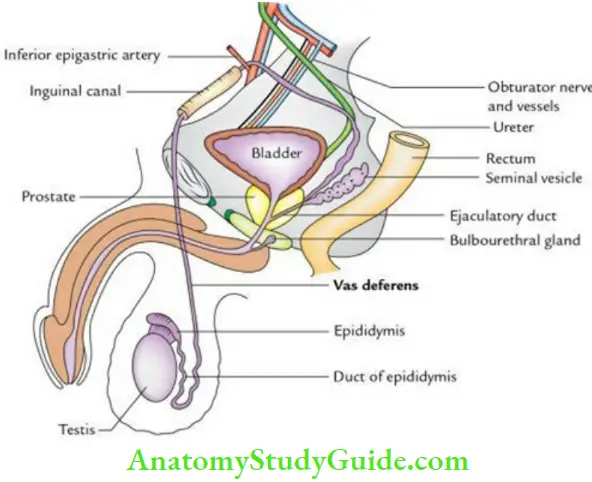
- In the Scrotum: The 1st part of vas deferens begins at the tail of the epididymis and is tortuous, but gradually it becomes straight and ascends along the posterior border of the testis, medial to the epididymis.
- In the Spermatic Cord: The 2nd part of the vas deferens runs vertically upwards in the posterior part of spermatic cord and passes successively through the superficial inguinal ring, inguinal canal, and deep inguinal ring. In spermatic cord, it is felt like a cord with a consistency like a plastic tube.
- In the Pelvis: The 3rd part of vas deferens begins at the deep inguinal ring; it leaves the spermatic cord and hooks around the lateral side of the inferior epigastric artery. It then passes backward and medially, across the external iliac vessels, and enters the lesser pelvis.
Direct And Indirect Inguinal Hernia
In the Lesser Pelvis:
- It first lies along its lateral wall and then runs downward and backward deep to the peritoneum. Here, it crosses the obliterated umbilical artery, the obturator nerve and vessels, and the vesical vessels.
- It then crosses the ureter, to reach the base of the urinary bladder where it runs downward and forward medial to the seminal vesicle. Here, it approaches the opposite vas deferens and reaches the base of the prostate.
- At the base of the prostate, the ductus deferens ends by joining the duct of the seminal vesicle at an acute angle to form the ejaculatory duct.
- The terminal dilated end of vas deferens that lies behind the urinary bladder is called the ampulla.
Applied anatomy
Vasectomy:
- For family planning, a small incision is placed in the upper part of the scrotum on both sides. The position of vas deferens is identified by palpating it in the spermatic cord.
- The spermatic cord is pulled out and its coverings are cut open. A small segment of each ductus deferens is cut and the cut ends are ligated on both sides.
Question 19. Give the histological features of the vas deferens.
Answer:
Histological Features Of The Vas Deferens:-
A histological section of the ductus deferens presents a small lumen and a thick wall surrounding it.
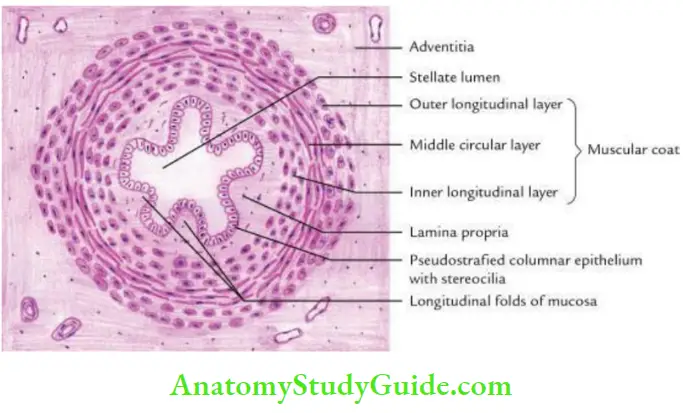
Lumen: Narrow and stellate-shaped.
Wall: From within outward it consists of 3 layers: mucosa, muscular coat, and adventitia (fibrous coat).
- Mucosa:
- Epithelial lining: Epithelial lining is made up of columnar or pseudostratified columnar, cells with stereocilia.
- Lamina propria: Lamina propria is the thin layer of connective tissue containing an extensive network of elastic fibers. It is thrown into 4–6 longitudinal folds.
- Muscular coat: Consists of 3 layers of smooth muscle fibers – inner and outer longitudinal layers and a thick powerful intermediate circular layer.
- Adventitia: Thin layer of connective tissues, containing blood vessels and nerves
Leave a Reply