Anterior Compartment Of The Leg And Dorsum Of The Foot
Question 1. Enumerate the muscles of the anterior compartment of the leg.
Answer:
Anterior Compartment:
Anterior Compartment They are:
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
- Peroneus Tertius
Question 2. Give the origin, insertion, nerve supply, and actions of the tibialis anterior muscle.
Answer:
Anterior muscle:
Anterior Muscle Origin:
Upper 2/3rd of the lateral surface of the tibia and adjacent interosseous membrane.
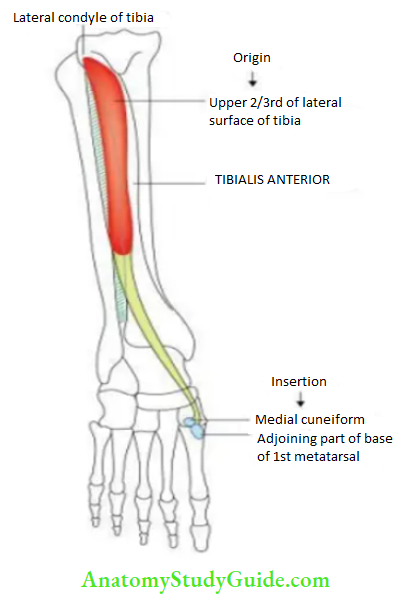
Anterior Muscle Insertion
- The medial side of the medial cuneiform
- Adjoining part of the base of the first metatarsal.
Anterior Muscle Nerve Supply
Deep peroneal nerve (anterior tibial nerve).
Anterior Muscle Actions
- It is the dorsiflexor of the foot at the ankle joint.
- It is an inverter of the foot at the subtalar and midtarsal joints.
Question 3. Write a short note on dorsalis pedis artery.
Answer:
Pedis Artery:
It is the chief artery of the dorsum of the foot.
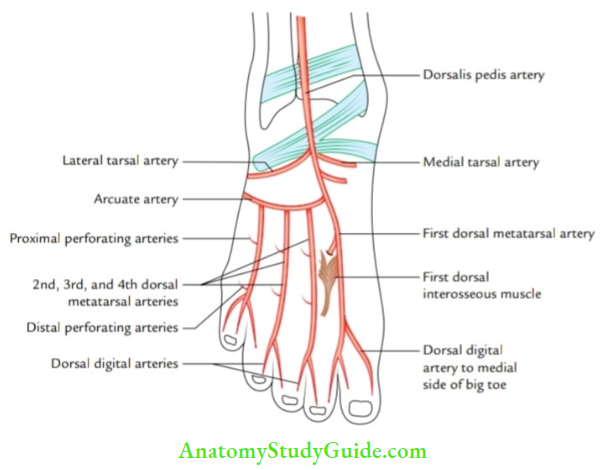
Pedis Artery Origin:
It is a continuation of an anterior tibial artery in front of the ankle joint between the medial and lateral malleoli.
Pedis Artery Course:
- It passes forward between the tendon of the extensor hallucis longus on the medial side, and deep peroneal nerve, and tendons of the extensor digitorum longus on the lateral side to reach the proximal end of 1st intermetatarsal space.
- Here, it dips downwards between the two heads of 1st dorsal interosseous muscle to reach the sole where it anastomoses with the lateral plantar artery to complete the lateral plantar arch.
Pedis Artery Branches:
- Medial and lateral tarsal arteries
- Arcuate artery
- First dorsal metatarsal artery
Pedis Artery Applied Anatomy:
Pedis Artery Dorsalis Pedis Pulse:
The pulsations of dorsalis pedis artery can be felt on the dorsum of the foot distal to the ankle joint between the tendons of the extensor hallucis longus (medially) and the extensor digitorum longus (latterly).
Pedis Artery Lateral Compartment Of The Leg
Question 4. Enumerate muscles of the lateral compartment of the leg.
Answer:
Lateral Compartment Of The Leg:
Lateral Compartment Of The leg They Are:
- Peroneus longus
- Peroneus Brevis
Question 5. Give the origin, insertion, nerve supply, and actions of the peroneus longus muscle.
Answer:
Longus Muscle:
Longus Muscle Origin:
Head and upper 2/3rd of the lateral surface of the fibula.
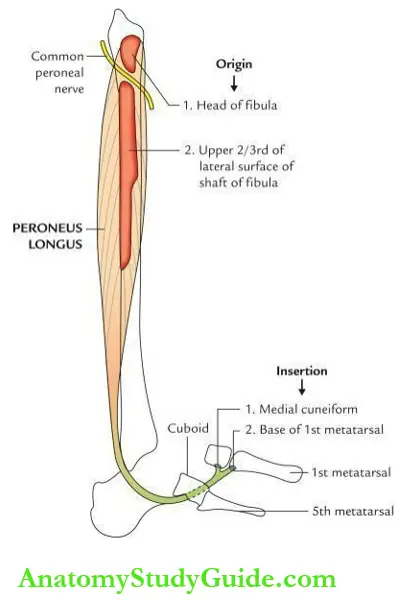
Longus Muscle Insertion: The tendon enters the sole through the groove on the plantar surface of the cuboid and crosses it from the lateral to the medial side to be inserted on the base of the first metatarsal and adjoining part of the medial cuneiform.
Longus Muscle Nerve Supply: The superficial peroneal nerve.
Longus Muscle Actions:
- It is evertor of the foot at the subtalar and midtarsal joints.
- Its tendon acts as a pulley and supports the arches of the foot from above.
Question 6. Give a brief description of the deep peroneal nerve.
Answer:
Peroneal Nerve:
Peroneal Nerve Origin:
It is one of the terminal branches of the common peroneal nerve.
Peroneal Nerve Course:
- It begins at the lateral side of the neck of the fibula and enters the anterior compartment of the leg by piercing the anterior intermuscular septum.
- In the anterior compartment, it courses downward first lateral to the anterior tibial artery, then in front of the artery, and then again lateral to the artery as if the nerve hesitates to cross the artery.
- For this region, it is also called nervus hesitant. It enters the dorsum of the foot by passing deep to the superior extensor retinaculum midway between the medial and lateral malleoli and terminates by dividing into medial and lateral terminal branches.
Peroneal Nerve Branches:
Peroneal Nerve In the Leg:
Muscular branches supply all four muscles of the anterior compartment of the leg.
Peroneal Nerve On the Dorsum Of The Foot:
- Medial Terminal Branch:
- Muscular branch to 1st dorsal interosseous muscle.
- Dorsal digital nerves provide sensory innervation to the skin of 1st interdigital cleft.
- Lateral Terminal Branch: Ends By Forming a nodule called pseudoganglion.
- Muscular branches to extensor digitorum brevis.
- Muscular branch to 2nd dorsal interosseous muscle.
Peroneal Nerve Applied Anatomy: Effects of injury to the deep peroneal nerve are:
Peroneal Nerve Motor loss: Paralyzes of the muscles of the anterior compartment of the leg (i.e., dorsiflexion of the ankle joint), leading to foot drop.
Peroneal Nerve Sensory loss: On the dorsum of the foot in the first interdigital cleft.
Question 7. Describe the superficial peroneal nerve in brief.
Answer:
Brief:
Brief Origin:
It is one of the terminal branches of the common peroneal nerve.
Brief Course:
- It begins at the lateral aspect of the neck of the fibula and travels downward between peroneus longus and peroneus brevis:
- At the junction of the upper 2/3rd and lower 1/3rd of the leg, it pierces deep fascia to enter the superficial fascia.
- In the lower part of the leg, it divides into medial and lateral branches that cross in front of the extensor retinaculum to reach the dorsum of the foot.
Brief Branches:
Brief In the leg:
- Muscular branches to peroneus longus (PL) and peroneus brevis (PB).
- Cutaneous branches to:
- Lower 1/3rd of the lateral side of the leg
- The medial side of the great toe
- Interdigital clefts between 2nd, 3rd, 4th, and 5th toes
- Most of the dorsum of the foot
Brief Applied Anatomy:
Brief Injury To The Superficial Peroneal Nerve Leads to:
- Weakness of eversion of foot, due to paralysis of peroneus longus and peroneus brevis.
- Sensory loss on the lateral aspect of the leg.
- Sensory loss on the dorsum of the foot and toes except for the first interdigital cleft and lateral side of the 5th toe.
Question 8. Write a short note on an anserine bursa.
Answer:
Aanserine Bursa:
- It is a large complex synovial bursa located on the upper medial aspect of the tibia.
- It separates tendons of sartorius, gracilis, and semitendinosus from each other. It also separates the tendon of the semitendinosus from the medial (tibial) collateral ligament.
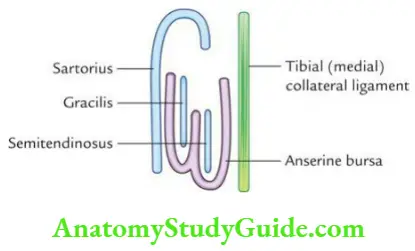
Anserine Bursa Applied Anatomy:
Anserine Bursaries:
Repeated trauma on the upper medial aspect of the leg leads to inflammation of the anserine bursa called anserine bursitis. Clinically it presents as pain and swelling on the upper part of the medial aspect of the leg.
Posterior Compartment Of The Leg
Question 9. Enumerate the muscles of the posterior compartment of the leg.
Answer:
Posterior Compartment Of The Leg:
They are divided into superficial and deep groups:
Posterior Compartment Of The Leg Superficial Muscles:
- Gastrocnemius
- Soleus
- Plantaris
Posterior Compartment of the leg Deep Muscles:
- Popliteus
- Flexor digitorum longus
- Flexor hallucis longus
- Tibialis posterior
Question 10. Give the origin, insertion, nerve supply, and actions of the gastrocnemius muscle.
Answer:
Gastrocnemius Muscle:
The gastrocnemius forms the bulk of the calf.
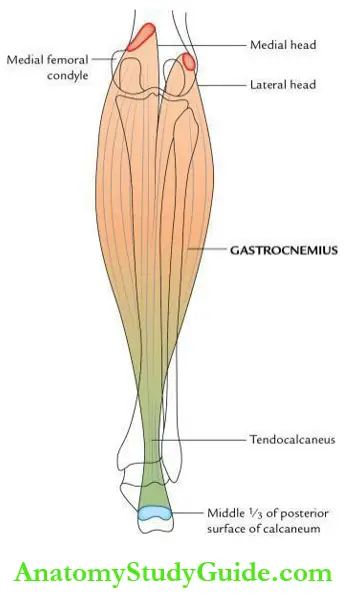
Gastrocnemius Muscle Origin:
Gastrocnemius Muscle Medial Head: From the upper and posterior part of the medial condyle of the femur behind the adductor tubercle and adjacent part of the popliteal surface of the femur.
Gastrocnemius Muscle Lateral Head: From the lateral aspect of the lateral condyle of the femur and the adjoining part of the lateral supracondylar line.
Gastrocnemius Muscle Insertion: The gastrocnemius joins the tendon of the soleus to form a conjoint tendon – the tendocalcaneus that is inserted into the middle 1/3rd of the posterior surface of the calcaneus.
Gastrocnemius Muscle Nerve Supply: Tibial nerve.
Gastrocnemius Muscle Actions: Flexion of the knee joint.
Question 11. Give the origin, insertion, nerve supply, and actions of the soleus muscle.
Answer:
Soleus Muscle:
It is a powerful muscle situated deep in the gastrocnemius. It is a multipennate muscle and shaped like a fish/sole of the foot.
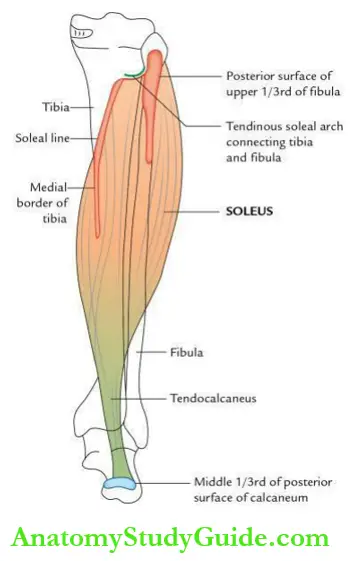
Soleus Muscle : Origin
- Upper 1/3rd of the posterior surface of the fibula
- Tendinous solely arch
- Soleal line
- Middle 1/3rd of the medial border of the tibia
Soleus Muscle Insertion:
The tendon of soleus fuses with the tendon of gastrocnemius to form tendocalcaneus that is inserted into the middle 1/3rd of the posterior surface of the calcaneus.
Soleus Muscle Actions:
- Plantar flexion of the foot at the ankle
- Provides main propulsive force during running and walking
Question 12. Write a short note on the ‘calf muscle pump’ and ‘peripheral heart’.
Answer:
Peripheral Heart:
Peripheral Heart Calf Muscle Pump/Calf Pump:
It is formed by the gastrocnemius and soleus muscles together. During an upright position, contraction of these muscles facilitates the venous return from the lower limb.
Peripheral heart Peripheral heart:
- The soleus muscle is regarded as the peripheral heart because it houses large valveless venous sinuses (solely sinuses), which are connected to both superficial veins (by perforating veins) and deep veins (directly).
- Therefore, the contraction of the soleus muscle helps in sucking the blood from superficial veins via perforating veins and propelling it to the deep veins of the posterior compartment of the leg, which subsequently drain into the heart.
Question 13. Give the origin, insertion, nerve supply, and actions of the popliteus muscle.
Answer:
Popliteus Muscle:
It is the only short muscle on the back of the leg and forms the lower part of the floor of the popliteal fossa.
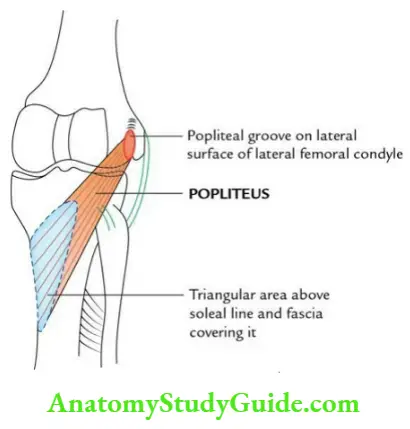
Popliteus Muscle Origin:
Popliteal groove (anterior part) on the lateral surface of the lateral condyle of the femur.
Popliteus Muscle Insertion:
The triangular area on the posterior surface of the tibia above the seal line and fascia covering it.
Popliteus Muscle Nerve supply:
Nerve to popliteus, a branch of the tibial nerve.
Popliteus Muscle Actions:
- It unlocks the knee in the initial phase of flexion by causing:
- Medial rotation of the tibia on the femur when the foot is off the ground or
- Lateral rotation of the femur on the tibia when the foot is on the ground.
- It pulls the lateral meniscus posteriorly and prevents it from being trapped at the beginning of the knee flexion, thus preventing it from tearing.
Popliteus Muscle Note:
- The nerve to the popliteus winds around the lower margin of the popliteus to supply it from its anterior surface.
- The Popliteus muscle is important in unlocking the locked knee; hence, it is referred to as the key muscle of the knee joint.
Question 14. Describe the tibial nerve (medial popliteal nerve) in brief and give the effects of its injury.
Answer:
Tibial Nerve: It is the larger terminal branch of the sciatic nerve (root value: L4, L5, S1, S2, and S3).
Tibial Nerve Origin And Course:
- It arises from the sciatic nerve at the junction of the upper 2/3rd and lower 1/3rd of the back of the thigh.
- It enters the popliteal fossa where it crosses popliteal vessels superficially from lateral to medial side.
- From the popliteal fossa, it enters the posterior compartment of the leg at the level of the inferior border of the popliteus undercover the tendinous arch of the soleus.
- In the leg, it crosses the tibial artery from the medial to the lateral side just below the tendinous arch.
- At the ankle, it lies lateral to the posterior tibial artery.
- It terminates deep into the flexor retinaculum by dividing into lateral and medial plantar nerves.
Tibial Nerve Branches:
Tibial Nerve In the Popliteal Fossa:
- Muscular branches to gastrocnemius (both heads), planters, and popliteus
- Cutaneous branch, sural nerve
- Articular, middle genicular to the knee joint
Tibial Nerve In the leg, Below the popliteal fossa:
- Muscular branches to soleus, flexor digitorum longus (FDL), flexor hallucis longus (FHL), and tibialis posterior.
- Cutaneous branch
- Medial calcaneal branch.
- Articular branches to knee and ankle joints.
- Terminal branches
- The medial plantar nerve.
- The lateral plantar nerve.
Tibial Nerve Applied Anatomy:
Effects of injury of the tibial nerve in the popliteal fossa
Tibial Nerve Motor Loss:
- Inability to flex the knee, due to paralysis of gastrocnemius and soleus.
- Inability to invert foot, due to paralysis of tibialis posterior.
- Foot assumes the position of calcaneovalgus, due to the unopposed action of extensors and investors. As a result, the patient cannot stand on the tips of her toes and feels difficulty in ‘taking off’.
- Inability to flex the toes, due to paralysis of long and short flexors of the toes.
Tibial Nerve Sensory Loss: Loss of sensation in the sole of the foot.
Question 15. Describe the common peroneal nerve in brief and give the effects of its injury.
Answer:
Common Peroneal Nerve In Brief: It is the smaller terminal branch of the sciatic nerve (root value: L4, L5, S1, and S2).
Common Peroneal Nerve In Brief Origin And Course:
It begins at the junction of the upper 2/3rd and lower 1/3rd of the back of the thigh. It enters the popliteal fossa through its upper angle and then follows the tendon of the biceps to reach the back of the head of the fibula, where it curves forward on the lateral side of the neck of the fibula and terminates by dividing into superficial and deep peroneal nerves.
A Common Peroneal Merve In Brief Branches:
A Common Peroneal Nerve in Brief In Popliteal Fossa:
- Superior and inferior lateral genicular nerves
- The lateral cutaneous nerve of the calf
- Communicating branch to the sural nerve
A Common Peroneal nerve in brief In the leg below:
- Recurrent genicular
- Deep peroneal nerve
- Superficial peroneal nerve
A Common Peroneal Nerve in brief Applied anatomy:
Common peroneal nerve in brief Effects of injury to common peroneal nerve:
- It is the most commonly injured peripheral nerve in the lower limb. It gets injured either due to a fractured neck of the fibula or due to the direct pressure of the tightly applied plaster cast. Clinically, it presents as (due to the involvement of both deep and superficial peroneal nerves)
- Foot drop (foot is inverted and plantar flexed) due to the paralysis of dorsiflexion of the ankle and evertors of the foot. As a result, the patient walks on her toes.
- Sensory loss on the dorsum of the foot and toes except medial and lateral margins of the foot and lateral side of the little toe.
Question 16. Write a short note on the flexor retinaculum of the ankle.
Answer:
Flexor Retinaculum Of The Ankle:
It is a thickened band (about 2.5 cm broad) of deep fascia on the medial aspect of the ankle.
Flexor Retinaculum Of The Ankle Attachments:
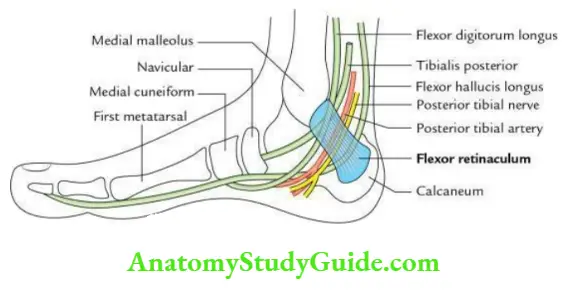
Flexor Retinaculum Of The Ankle Anteriorly: Posterior border and tip of the medial malleolus.
Flexor Retinaculum Of The Ankle Posteriorly: Medial tubercle of the calcaneum.
Flexor retinaculum of the ankle Structures passing deep to the retinaculum:
Flexor retinaculum of the ankle From medial to lateral:
- Tendon of the tibialis posterior
- Tendon of the flexor digitorum longus
- Posterior tibial artery and its terminal branches
- Tibial nerve and its terminal branches
- Tendon of the flexor halluces longus
Flexor retinaculum of the ankle Mnemonic: The Doctors Are Not Here.
Flexor retinaculum of the ankle Functions: It holds the tendons in place (i.e., prevents their bowstring) as they curve to pass forward from the back of the leg to the sole of the foot.
Question 17. Write a short note on the extensor retinacula of the ankle.
Answer:
Extensor retinacula of the ankle:
These are two thickened bands of deep fascia, viz. superior and inferior called superior and inferior retinacula.
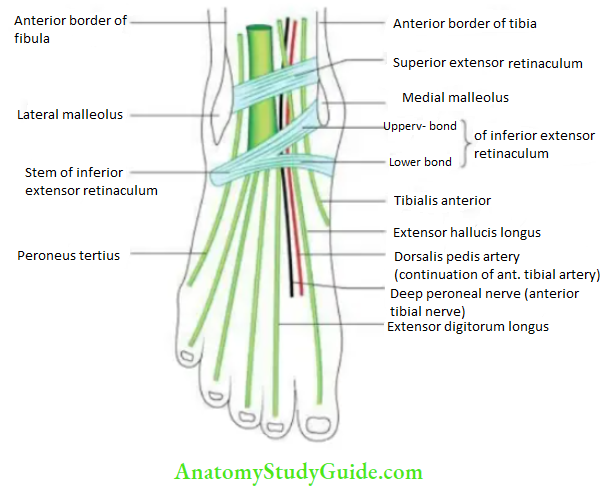
Extensor retinacula of the ankle Attachments of the superior extensor retinaculum:
Extensor retinacula of the ankle Medially: Anterior border of the tibia.
Extensor retinacula of the ankle Laterally: Anterior aspect of the fibula.
Extensor retinacula of the ankle Attachments of inferior extensor retinaculum (Y-shaped):
Extensor retinacula of the ankle Medially:
- The upper band of ‘Y’ to the medial malleolus.
- The lower band of ‘Y’ to the deep fascia of the sole.
Extensor retinacula of the ankle Laterally: Stem of ‘Y’ to the anterior part of the calcaneum (upper surface).
Structures passing deep to the extensor retinacula of the ankle:
Extensor retinacula of the ankle From medial to lateral, these are:
- Tibialis anterior
- Extensor hallucis longus
- Anterior tibial artery
- Deep peroneal nerve
- Extensor digitorum longus
- Peroneus Tertius
Extensor retinacula of the ankle Mnemonic: The Himalayas Are Not Dry Places.
Foot
Question 18. Write a short note on cutaneous innervation of the dorsum of the foot.
Answer:
Foot:
The cutaneous innervation of the dorsum of the foot is provided by the following nerves (given in the box below).
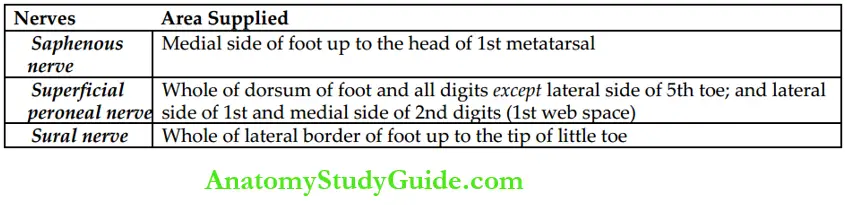
Foot Note:
Nail beds of medial 3½ digits are supplied by the medial plantar nerve and those of lateral 1½ digits by the lateral plantar nerve.
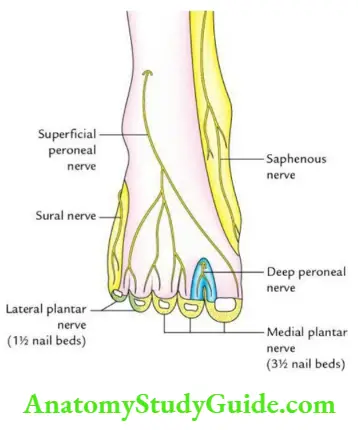
Question 19. Draw a labeled diagram to show the sensory innervation of the sole.
Answer:
Sensory innervation of the sole:
Question 20. Write a short note on plantar aponeurosis.
Answer:
Plantar aponeurosis:
- It is a central thickened part of the deep fascia of the sole.
- It is triangular in shape, having an apex and base.
Plantar aponeurosis Attachments:
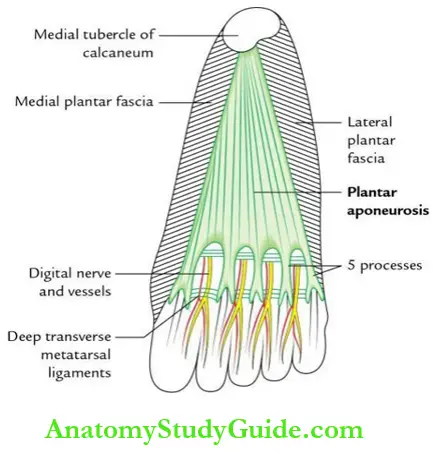
Plantar Aponeurosis Apex:
It is directed proximally and attached to the medial tubercle of the calcaneum.
Plantar Aponeurosis Base:
- It is a broad distal part that divides into five processes, opposite to the heads of the metatarsal bones. These processes are connected by the transverse fibers.
- The digital nerves and vessels pass through the intervals between the processes. Each process splits into a superficial and a deep slip.
- The superficial slip is attached to the skin, and the deep slip divides into two parts that embrace the flexor tendons and blend with the fibrous flexor sheaths and also with the deep transverse metatarsal ligaments.
Plantar Aponeurosis Note:
Morphologically, plantar aponeurosis is the detached tendon of the plantar muscle.
Plantar Aponeurosis Functions:
- It fixes the skin of the sole and protects the deeper structures of the sole.
- It helps in maintaining the longitudinal arches of the foot by acting as a tie beam.
Plantar Aponeurosis Applied Anatomy:
Plantar Aponeurosis Plantar Fasciitis:
- It is the inflammation or tear of the apical part of the plantar fascia and causes pain in the heel during walking especially on a hard surface.
- It commonly affects the individuals who are supposed to stand for a long period of time, viz. traffic police personnel, hence also called Policeman’s heel: neglected may lead to the formation of the calcaneal spur.
Question 21. Enumerate muscle layers of the sole.
Answer:
Enumerate Muscle:
The muscles and tendons of the sole are arranged into the following 4 layers:
Enumerate Muscle First Layer:
Enumerate Muscle It Consists Of 3 Muscles:
- Abductor hallucis
- Flexor digitorum brevis
- Abductor digiti minimi
Enumerate Muscle Second Layer:
Enumerate Muscle It Consists Of 2 Tendons And 2 Muscles:
- Tendon of flexor hallucis longus
- Tendon of flexor digitorum longus
- Flexor digitorum accessorius
- Lumbrical muscles.
Enumerate Muscle Third layer:
Enumerate Muscle It Consists Of 3 Muscles:
- Flexor hallucis brevis
- Adductor hallucis
- Flexor digiti minimi brevis.
Enumerate Muscle Fourth Layer:
Enumerate Muscle It Consists Of 2 Tendons And 2 Muscles:
- Tendon of peroneus longus
- Tendon of the tibialis posterior
- Plantar interossei
- Dorsal interossei
Enumerate Muscle Note:
The 1st neurovascular plane lies between the first and second layers of the sole, while the 2nd neurovascular plane lies between the third and fourth layers of the sole.
Question 22. Write a short note on the plantar arch.
Answer:
Plantar Arch:
- It is the name given to the continuation of the distal part of the lateral plantar artery.
- It courses across the sole from the lateral to the medial side between the third and fourth layers of the sole.
- It presents as a concavity proximally and convexity distally.
- It begins at the base of the 5th metatarsal bone and extends to the first intermetatarsal space where it ends by joining the dorsalis pedis artery.
- The deep branch of the lateral plantar nerve lies in its concavity.
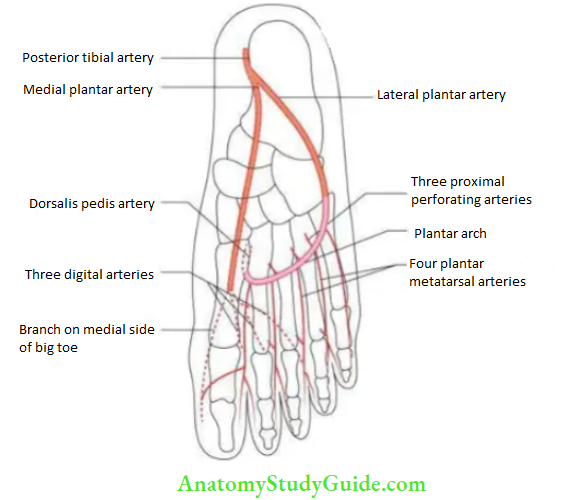
Plantar arch Branches:
- Three proximal perforating arteries enter the 2nd, 3rd, and 4th intermetatarsal spaces.
- Four plantar metatarsal arteries run forward in corresponding intermetatarsal spaces.
Plantar Arch Applied Anatomy:
If the plantar arch is cut, it is difficult to control the bleeding by direct pressure/ligature due to its deep location. To stop it effectively, one needs to compress the femoral artery.
Question 23. Describe the arches of the foot under the following headings:
- Definition,
- Classification,
- Formation and features,
- Factors responsible for the maintenance of the arches,
- Functions and
- Applied anatomy.
Answer:
Headings:
Headings Definition:
The human foot is designed to form segmented arches not only to support the body weight but also to propel the body forward during walking and running. The arches of the foot are distinguished features of a human.
Headings Classification:
When looked at from below, the foot appears arched not only longitudinally, but also transversely. Thus, there are two types of arches.
Headings Longitudinal Arches:
- Medial
- Lateral
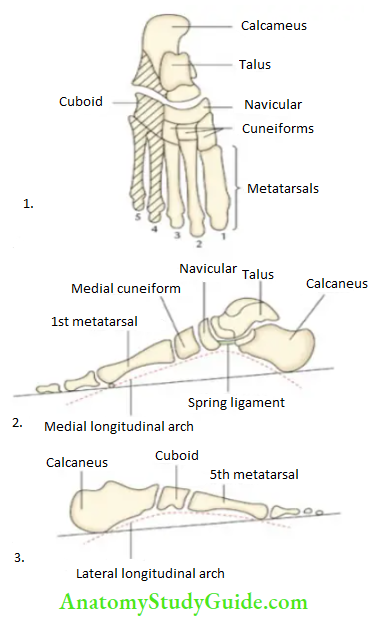
Headings Transverse Arches:
- Anterior
- Posterior
Headings Formation of the medial longitudinal arch:
It is considerably higher mobile and resilient.
From behind forward, it is formed by:
- Calcaneus
- Talus
- Navicular.
- Three cuneiforms
- Three medial metatarsals
Headings Features of the medial longitudinal arch:
Headings Ends:
- The anterior end is formed by the heads of the 1st, 2nd, and 3rd metatarsals.
- The posterior end is formed by the medial tubercle of the calcaneum.
- Summit is formed by the superior articular surface of the body of the talus.
Headings Pillars:
- The anterior pillar is long and weak. It is formed by talus, navicular, 3 cuneiforms, and 1st three metatarsals.
- The posterior pillar is short and strong. It is formed by the medial part of the calcaneum.
- Join The important joint is the talocalcaneonavicular joint.
Headings Formation of the lateral longitudinal arch:
It is low with limited mobility. It is built to transmit weight and thrust to the ground. It acts as a shock absorber. From behind forward, it is formed by: calcaneum, cuboid, and two lateral metatarsals.
Headings Joint:
The important joint of the arch is the talocalcaneonavicular joint.
Headings Features of the lateral longitudinal arch:
Headings Ends:
- The anterior end is formed by the heads of the fourth and fifth metatarsals.
- The posterior end is formed by the lateral tubercle of the calcaneus.
Headings Summit:
It is formed by the cuboid.
Headings Pillars
- The anterior pillar is formed by the cuboid and fourth and fifth metatarsals. It is long and weak.
- The posterior pillar is formed by the lateral half of the calcaneum. It is strong and short.
Headings Joint:
The important joint of the arch is the calcaneocuboid joint.
Headings Formation Of The Anterior Transverse Arch
It is formed by the heads of all the metatarsals.
Headings Formation Of The Posterior Transverse Arch
It is formed by calcaneum, cuboid, cuneiforms, and metatarsals except their heads. It is like a half dome because only its lateral end comes in contact with the ground.
Headings Factors Responsible For The maintenance of the arches of the foot
Headings Shapes Of The Bones: They are very important for maintaining the posterior transverse arch where many tarsal bones are involved and interlocked.
Headings Intersegmental Ties Or Ligaments:
They hold different segments of arches together like the spring ligaments for the medial longitudinal arch and the long and short plantar ligaments for the lateral longitudinal arch.
Headings Tie Beams Or Bowstrings:
They connect the two ends of the arch, which prevents the arches from flattening. It is done by plantar aponeurosis and muscles of the first layer of the sole in the case of longitudinal arches and adductor hallucis in the case of transverse arches.
Headings Slings:
- They keep the summit pulled up.
- Medial longitudinal arch, by tendons passing from the posterior segment of the leg into the sole.
- Lateral longitudinal arch, tendons of peroneus longus and brevis.
- Transverse arches, peroneus longus, and tibialis posterior.
Headings Functions of the arches
- Provide rigid support and distribute the body weight to the weight-bearing areas of the sole in a standing position.
- Act as a mobile springboard during walking and running.
- Act as a shock absorber during jumping.
- Protect the nerves and vessels of the sole from rubbing against the ground.
Headings Applied anatomy
Headings Flatfoot (pes planus):
It occurs either due to the absence or due to the collapse of the longitudinal arches, especially the medial longitudinal arch. Clinically, it presents as:
- Clumsy and shuffling gait due to the loss of spring action of the foot.
- Foot trauma and osteoarthritis due to the loss of shock absorption.
- Compression of nerves and vessels of the sole due to the loss of concavity.
Headings High-Arched Foot (Pes Cavus):
It occurs when longitudinal arches become unduly elevated (i.e., exaggeration of longitudinal arches) due to the shortening of plantar aponeurosis or contracture of the intrinsic muscles of the sole.
Leave a Reply