Autonomic Nervous System
Introduction To Autonomic Pharmacology
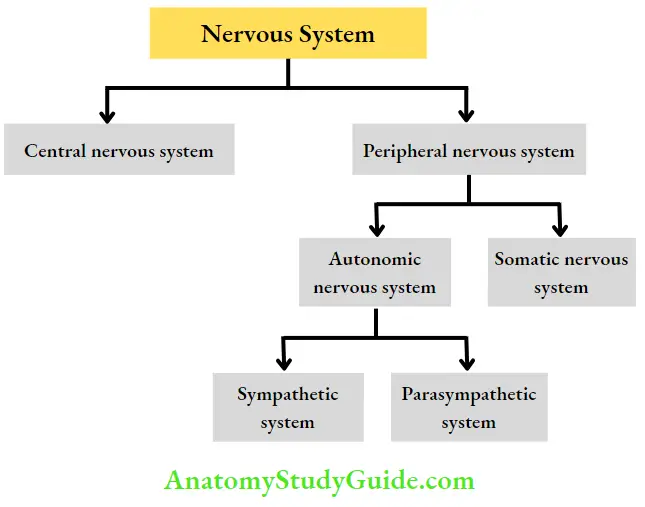
The nervous system is divided into central and peripheral nervous systems. The peripheral nervous system consists of autonomic and somatic nervous systems.
The autonomic nervous system (ANS) is not under voluntary control and therefore was so named by Langley (Autos = self, nomos = governing in Greek). The ANS innervates the heart, the smooth muscles, the glands, and the viscera and controls the functions of these organs.
Read And Learn More: Pharmacology Question And Answers
- The centers for autonomic reflexes are present in the hypothalamus, medulla, and spinal cord. Hypothalamus coordinates the autonomic activity.
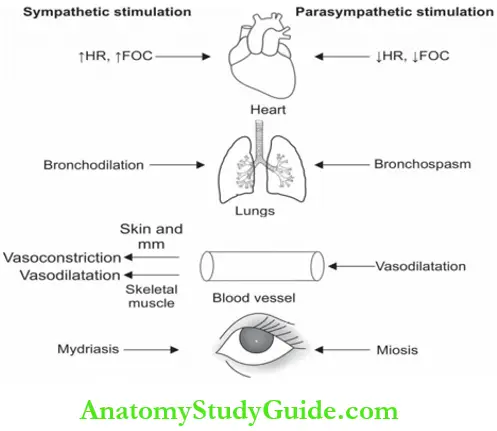
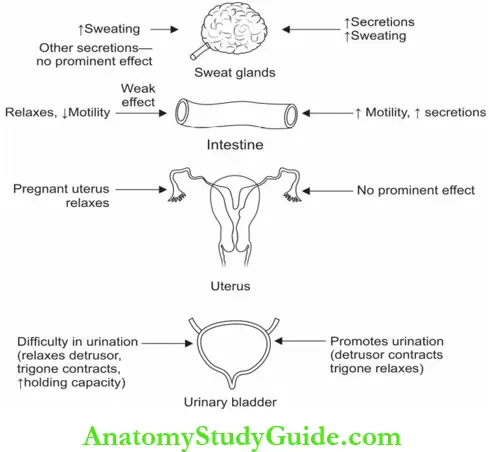
- Two major divisions of ANS—sympathetic and parasympathetic. The two divisions have opposing effects and normally their effects are in a state of equilibrium. Most of the viscera have both sympathetic and parasympathetic innervation.
- The prime function of the sympathetic system is to help a person to adjust to stress and
prepare the body for fight or flight reactions, while the parasympathetic mainly participates in tissue-building reactions.
Man can survive and remain alive without a sympathetic system (if maintained stress-free) but not without a parasympathetic.
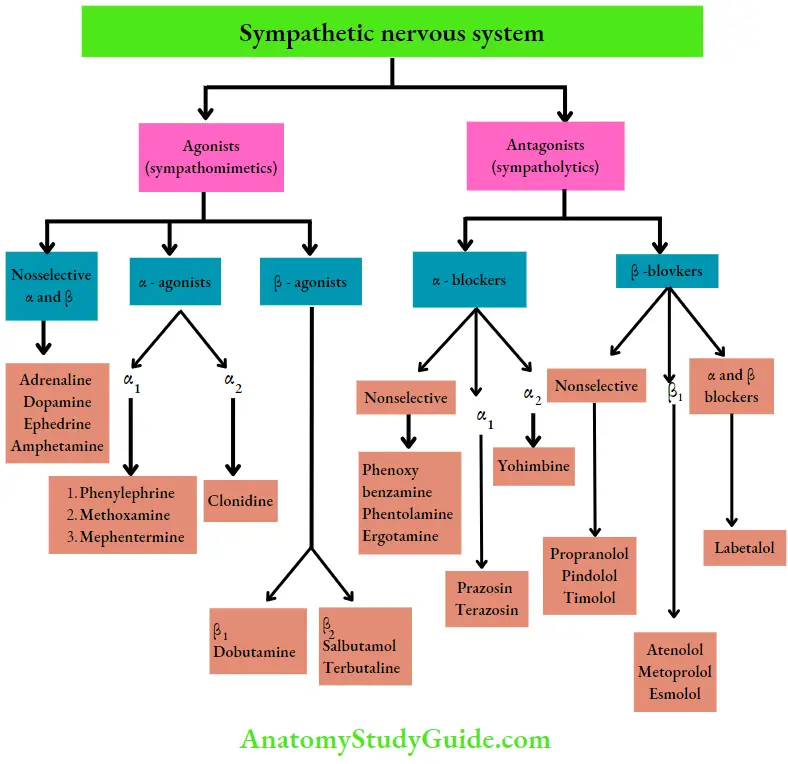
Drugs acting on the sympathetic and parasympathetic nervous system:
Sympathetic nervous system:
Parasympathetic nervous system:

Autonomic Innervation
Like the somatic nervous system, autonomic innervation also has an afferent, a center, and an efferent
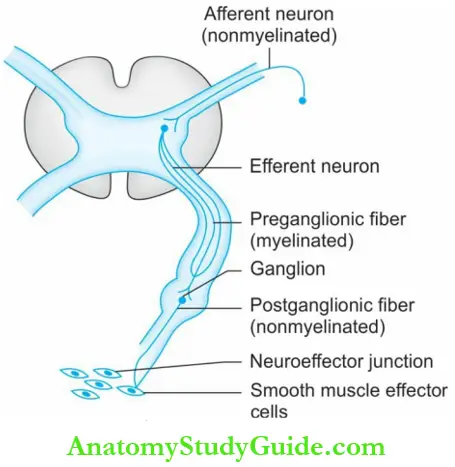
Autonomic Innervation Neurotransmitters:
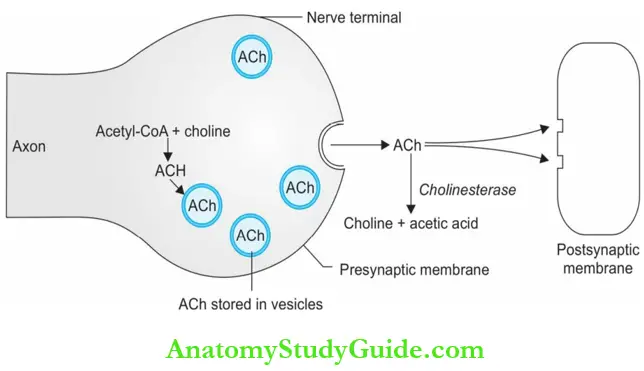
- For the transmission of an impulse across a synapse, a neurohumoral transmitter substance is released into the synaptic cleft.
- In the ANS, the neurotransmitters released are acetylcholine, noradrenaline, and dopamine, and in the adrenal medulla, it is adrenaline and noradrenaline.

Autonomic Innervation Enteric nervous system:
- The enteric nervous system (ENS) of nerve plexuses in the wall of the intestines includes the myenteric plexus and submucosal plexus.
- The ENS receives inputs from the ANS—from both parasympathetic and sympathetic systems. Parasympathetic stimulation in ENS is excitatory.
- Parasympathetic stimulation increases gut motility and relaxes the sphincters, while sympathetic activity has the opposite effect.
Cholinergic System
Cholinesterases are enzymes that hydrolyze acetylcholine. Acetylcholine (ACh) an ester of choline, is the neurotransmitter of the parasympathetic system. The nerves that synthesize, store, and release ACh are called cholinergic.
Question 1. List the sites of the release of acetylcholine.
Answer:
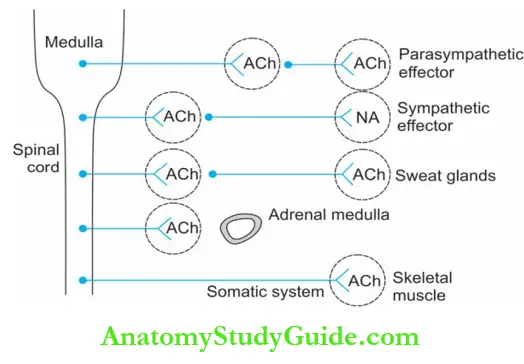
The sites of release of acetylcholine are:
- Ganglia—all the preganglionic fibers of ANS, i.e. at both the sympathetic and parasympathetic ganglia.
- The postganglionic parasympathetic nerve endings.
- Sweat glands are the sympathetic postganglionic nerve endings supplying the sweat glands.
- Skeletal muscles somatic nerve endings supplying skeletal muscles.
- Adrenal medulla.
- CNS brain and spinal cord.
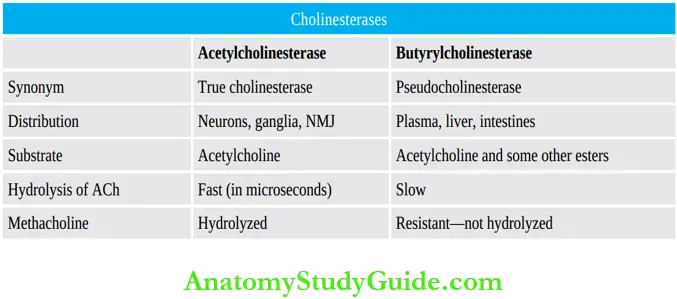
Cholinergic System Cholinesterases
Two types of cholinesterases are:
- True cholinesterase (acetylcholinesterase).
- Pseudocholinesterase (butyrylcholinesterase)
Types of cholinesterases:
Cholinergic Receptors
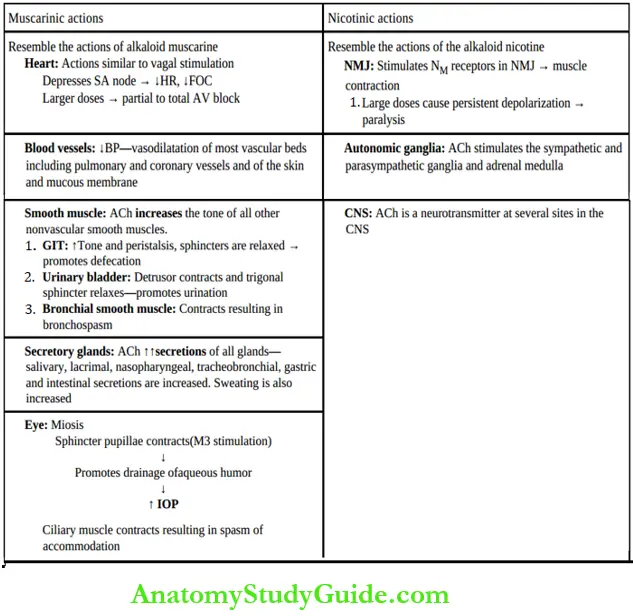
There are two classes of cholinergic receptors—muscarinic and nicotinic:
1. Muscarinic receptors are present in the heart, smooth muscles, glands, eyes, and CNS. Muscarinic receptors are all G-protein coupled receptors. There are five subtypes of muscarinic receptors, M1–M5
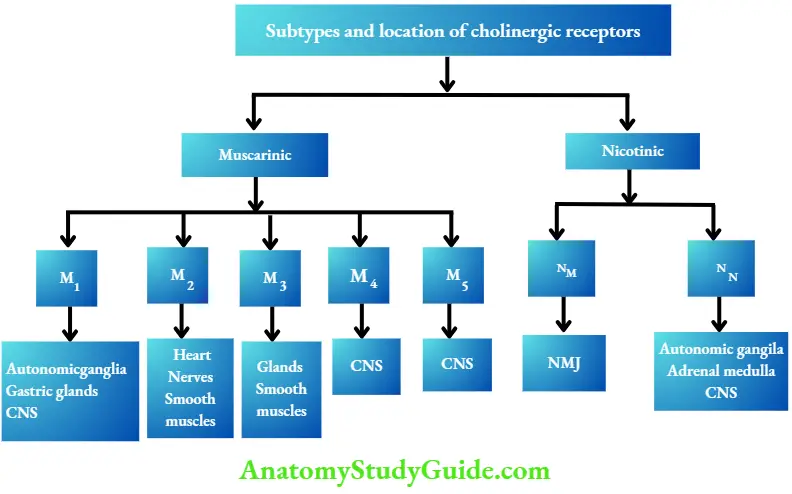
2. Nicotinic receptors are present in the neuromuscular junction (NMJ), autonomic ganglia, and adrenal medulla.
- Nicotinic receptors are ion channels—five subunits (2a, 1b, 1g, and 1d) enclose the channel
- Binding of acetylcholine to subunits opens the channel allowing the entry of Na+ into the cell.
- Two subtypes of nicotinic receptors are NM receptors present at the skeletal
muscle end plate and NN receptors at the autonomic ganglia and adrenal medulla.

Cholinergic Drugs
Cholinergic Drugs Classification:
1. Directly acting:
- Esters of choline: Acetylcholine, methacholine, carbachol, bethanechol
- Cholinomimetic alkaloids: Pilocarpine, muscarine, arecoline
2. Indirectly acting (anticholinesterases):
- Reversible (carbamates): Neostigmine, physostigmine, pyridostigmine, ambenonium, edrophonium, galantamine
- Irreversible
Organophosphorus compounds:
- Echothiophate, malathion, parathion, submission
- Toxic nerve gases: Sarin, tabun
Carbamate insecticides:
- Carbaryl propoxure (Baygon), aldicarb
Actions Of Acetylcholine:
Uses of acetylcholine: Acetylcholine is not used therapeutically because:
- It is rapidly destroyed in the gut when given orally.
- On intravenous administration, it is rapidly metabolized by pseudocholinesterases in the plasma and by true cholinesterase at the site of action.
- Only used as 1% eye drops to rapidly produce miosis during some eye surgeries.
Esters Of Choline
Esters of choline: Carbachol, bethanechol, and methacholine.
- Unlike acetylcholine, they are effective orally.
- Carbachol and bethanechol are resistant to both cholinesterases and have a longer duration of action.
- Their muscarinic actions are prominent with a sustained effect on GI smooth muscles and urinary bladder.
- Carbachol eye drops are used in glaucoma.
- Methacholine is resistant to pseudoChE but is not in use.
Bethanechol uses:
- Hypotonia of the bladder.
- Hypotonia of the gastrointestinal smooth muscles and in congenital megacolon.
- Postoperative paralytic ileus.
- Urinary retention and neurogenic bladder.
- Xerostomia (alternative to pilocarpine).
Choline Adverse effects:
Diarrhea, flushing, salivation, sweating, bradycardia, hypotension, syncope, and bronchospasm.
Cholinomimetic Alkaloids: Pilocarpine is a cholinomimetic alkaloid obtained from the Pilocarpus microphyllus plant.
Cholinomimetic Alkaloids Actions:
- Muscarinic actions are prominent.
- It is a tertiary amine, crosses BBB, and can cause CNS effects.
- When applied to the eye it causes miosis (contracts sphincter pupillae), contraction of the ciliary muscle, spasm of accommodation, and a fall in intraocular tension.
- It increases sweat (diaphoretic) and salivary secretions (sialogogue).

Cholinomimetic Alkaloids Adverse Effects:
- Topical: Eye drops cause a burning sensation, painful spasms of accommodation, brow ache, and corneal edema. Long-term use can cause retinal detachment.
- Systemic use: Salivation, sweating, bradycardia, diarrhea, and bronchospasm can occur.
Cholinomimetic Alkaloids Uses:
- Glaucoma: Pilocarpine 0.5–4% eye drops cause miosis and facilitates drainage of aqueous humor to reduce IOP. Pilocarpine focused acts for 7 days.
- To break the adhesions between the iris and lens: Pilocarpine used alternately with
mydriatics. - To counter the dryness of mouth seen following radiation of the head and neck.
- Sjögren’s syndrome is characterized by dryness of mouth and lack of tears. Pilocarpine being a sialogogue is useful.
Anticholinesterases/Cholinesterase Inhibitors
Question 2. Write short notes on anticholinesterases.
Answer:
Anticholinesterases (AChE) are drugs that inhibit the enzyme cholinesterase. They are either esters of carbamic acid (carbamates) or derivatives of phosphoric acid (organophosphates).
They may be:

Anticholinesterases Mechanism of action:
Anticholinesterases inhibit the enzyme cholinesterase and thereby increase ACh levels.
Anticholinesterases Physostigmine:
- An alkaloid from the plant Physostigma venenosum (Calabar bean)
- . It is a lipid-soluble, tertiary ammonium compound, hence has better penetration into tissues and also crosses the BBB.
Actions: Actions are like acetylcholine.
Anticholinesterases Uses:
- Glaucoma: Physostigmine eye drops are used in glaucoma but can cause brow aches and on longterm use, retinal detachment and cataract.
- Poisoning: Physostigmine IV in atropine and tricyclic antidepressant poisoning.
Anticholinesterases Neostigmine:
Synthetic quaternary ammonium compound—poorly absorbed from the gut and does not cross the BBB.
Physostigmine and Neostigmine:

Anticholinesterases Skeletal muscle:
Neostigmine increases the skeletal muscle strength and force of contraction in myasthenia gravis by anticholinesterase activity, by direct stimulation of nicotinic NM receptors, and by enhancing the amount of ACh released during each action potential.
Dose: 15–30 mg TDS-QID.
Uses of Reversible Anticholinesterases:
1. As a miotic: Physostigmine causes miosis, spasm of accommodation, and a decrease in IOP.
It is used:
- In glaucoma physostigmine (0.1%) can be used with pilocarpine for better effect.
- Alternately with a mydriatic to break the adhesions between the iris and lens.
- To reverse the effect of mydriatics as they cause blurring of vision and photophobia.
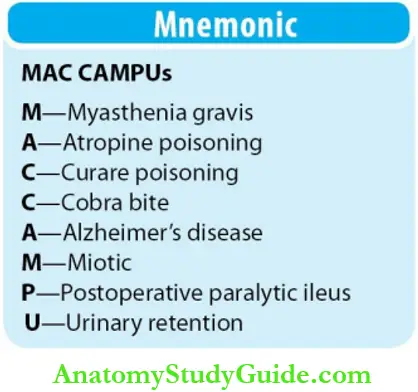
2. Myasthenia gravis: Neostigmine, ambenonium and pyridostigmine are used (see below).
3. Atropine poisoning:
- Physostigmine is the antidote in poisoning due to atropine and other drugs with anticholinergic activity like phenothiazines, tricyclic antidepressants, and antihistamines.
- Since physostigmine crosses the BBB, it reverses all the symptoms of atropine poisoning including CNS effects.
4. Curare poisoning:
- Skeletal muscle paralysis by curare can be reversed by AntiChEs.
- Neuromuscular paralysis due to neuromuscular blockers used along with anesthesia may be reversed using reversible anti-ChEs.
- Neostigmine and pyridostigmine can be used. Though edrophonium is faster acting, it is less effective than nesting
- Acetylcholine and reversible anticholinesterases bind to both anionic and static sites of
- AChE enzyme. Edrophonium binds only to the anionic site and is short-acting because the binding is rapidly reversible.
- OP compounds bind only the esteratic site but the exception is echothiophate which binds both anionic and esteratic sites.
5. Postoperative paralytic ileus and urinary retention: Neostigmine given 0.5–1 mg SC.
6. Cobra bite: Cobra venom, a neurotoxin causes skeletal muscle paralysis. The specific treatment is antivenom. Intravenous edrophonium prevents respiratory paralysis.
7. Alzheimer’s disease: To overcome the deficient cholinergic neurotransmission, rivastigmine, donepezil, and galantamine are tried.

Treatment of myasthenia gravis:
Myasthenia gravis (MG) is a chronic autoimmune disease characterized by progressive weakness with rapid and easy fatigability of the skeletal muscles. Antibodies to nicotinic receptors destroy the nicotinic receptors.
Symptoms resemble that of neuromuscular paralysis produced by tubocurarine—ptosis, diplopia, dysphagia and difficulty in speaking (dysarthria) with weakness of the extremities. In later stages, the disease involves all skeletal muscles.

- Drugs used are antiChE like neostigmine, pyridostigmine, ambenonium and edrophonium.
- Anticholinesterases increase ACh levels by preventing its destruction. They increase muscle power and provide symptomatic relief.
- Factors like infection, surgery, and stress can result in severe muscle weakness →
Myasthenic crisis.
- Severe weakness can also be due to an excess dose of anti-ChE → Cholinergic crisis.
- They can be differentiated by 2 mg IV edrophonium.

Organophosphorus Poisoning
Question 3. Outline the treatment of OP poisoning.
Answer:
As organophosphates (OP) are used as agricultural and household insecticides, poisoning by them is common and may be occupational, accidental or suicidal.
Symptoms: Result from muscarinic, nicotinic, and central effects.

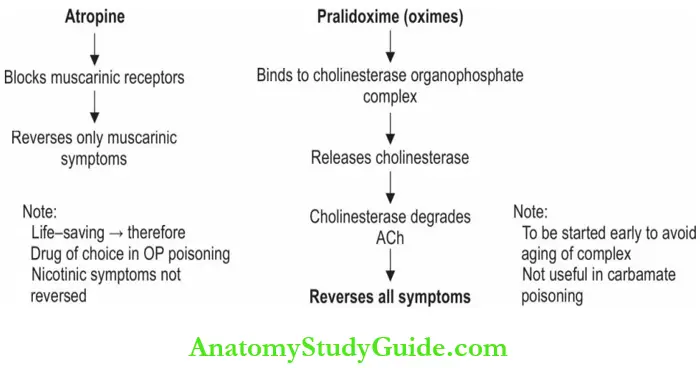
OP poisoning Treatment:
- If poisoning is through skin → remove clothing and wash the skin with soap and water; if consumed by oral route → thorough gastric lavage must be given.
- The patient should be put in a prone position to avoid aspiration of secretions.
- Maintain BP and patent airway.
- Drug of choice—atropine IV 2 mg every 10 minutes till pupil dilates.
- Treatment should be carefully monitored because of the risk of reappearance of symptoms due to delayed absorption of the OP compounds.
- Atropine may be needed for 3–4 weeks.
- Cholinesterase reactivators: Oximes viz pralidoxime, obidoxime, diacetylmonoxime combine with cholinesterase organophosphate complex, release the binding and set free AChE enzyme.
Anticholinergic Drugs
Anticholinergics are drugs that block the muscarinic receptors.
Anticholinergics are drugs Classification:

Anticholinergics Atropine
Question 4. Classify anticholinergics. Discuss the uses of atropine and its derivatives. Mention the adverse effects of atropine.
Or
Write/discuss briefly the actions, uses, and adverse effects of atropine.
Answer:
Atropine is a nonselective, competitive antagonist, that binds to muscarinic receptors and blocks the effects of acetylcholine on these receptors.
Actions of atropine:
Atropine is a CNS stimulant, while scopolamine is a CNS depressant and causes sedation.
1. CVS: Atropine increases heart rate and BP (blockade of M2 receptors in SA node). In large doses → vasodilation and hypotension particularly in cutaneous vessels (atropine flush).
2. Secretions: ↓ ↓ all secretions except milk. Lacrimal, salivary, nasopharyngeal and tracheobronchial secretions as well as sweating are decreased. Decreased salivation results in dry mouth and dysphagia. Atropine also reduces gastric secretions.
3. Smooth muscle:
- GIT: Atropine completely blocks the effects of ACh on the gut, reduces the tone and motility and relieves spasm; these effects together with decreased secretions results in constipation.
- Biliary tract: Smooth muscles are relaxed and biliary spasm is relieved.
- Bronchi: Atropine causes bronchodilatation. As the secretions are also reduced and
mucociliary clearance is interrupted and mucus plugs may be formed. - Genitourinary tract: Atropine relaxes ureters and urinary bladder leading to urinary retention particularly in the elderly men since they may already have prostatic
hypertrophy.
4. Eye: On local instillation, atropine produces passive mydriasis by blocking the muscarinic receptors in the sphincter pupillae (relaxes). It also causes cycloplegia and increased IOP.
5. CNS: In higher doses, atropine stimulates the CNS resulting in restlessness, disorientation,
hallucinations, and delirium. In contrast, scopolamine produces sedation and drowsiness. It can also cause euphoria.
Anticholinergics Adverse effects: Diplopia (blurring of vision), Dry mouth, Dysphagia, Dermal Dryness (dry skin), fever, (skin rashes), Difficulty in Defecation, and Difficulty in urination.
Question 5. Outline the treatment of Belladonna/atropine poisoning.
Answer:
Belladonna poisoning: Overdose of atropine or Belladonna alkaloids or Datura stramonium can be fatal.
- Symptoms: Hyperthermia, palpitation, flushing, restlessness, delirium, hallucinations, psychosis, convulsions, circulatory collapse, respiratory failure, and coma.
- Treatment is symptomatic.
- If the poison is taken orally → gastric lavage.
- Cold water sponging for hyperthermia.
- Respiratory support if needed.
- Physostigmine (1–3 mg slow IV, after 2 hr) can reverse both central and peripheral effects.
- Diazepam may be used to control seizures.
- Children are more susceptible to the toxic effects of atropine which can be rapidly fatal.
Symptoms of atropine poisoning as described by Cohen:
- Hot as a hare: Body temperature is increased because of the inhibition of sweating.
- Red as a beet: Skin is hot and red like a beetroot because of cutaneous vasodilation (atropine flush).
- Blind as a bat: Blurring of vision and photophobia due to mydriasis and cycloplegia.
- Dry as a bone: As atropine inhibits sweating, the skin and mucous membrane get dry.
- Mad as a wet hen: Atropine delirium, confusion, excitement, disorientation, and restlessness resemble that of a wet hen.
Atropine Substitutes/Derivatives
Question 6. Write briefly on atropine derivatives. Discuss the uses of atropine derivatives.
Answer:
Atropine produces a wide range of effects and these can result in various side effects since they lack selectivity. Hence, several semisynthetic and synthetic derivatives have been introduced some of which have selective action and are clinically useful
Question 8. Write a short note on the actions of adrenaline.
Answer:
1. Cardiovascular system:
- Heart: Adrenaline is a powerful cardiac stimulant. Acting through β1 receptors, it increases the heart rate, the force of contraction, cardiac output, and conduction velocity. The work done by the heart and the resultant O2 consumption are increased
2. Blood vessels and BP:
- Small doses—fall in BP because of vasodilation in the skeletal muscles (βreceptors sensitive even to these small doses).
- Moderate doses (IV)—produce a biphasic response. Rise in BP due to vasoconstriction (α1) and ↑ HR, the force of contraction (β1), and CO.
- As the action on a receptor wears off, the action on b2 receptors which is more persistent gets unmasked resulting in decreased BP. Noradrenaline is mainly an alpha agonist and therefore brings about a rise in BP.
- Other vascular beds: Adrenaline causes renal, pulmonary and mesenteric vasoconstriction. Cerebral and coronary blood flow is increased.
This is associated with bradycardia due to baroreceptor stimulation:

3. Smooth muscles:
Bronchi: Adrenaline is a powerful bronchodilator (activation of b2 receptors) and a weak respiratory stimulant. Pulmonary vasoconstriction (a1) relieves bronchial congestion. All these result in an increase in vital capacity.
- Uterus:
- Nonpregnant uterus—contracts
- Last month of pregnancy—relaxes.
- Gut: Smooth muscle is relaxed, but weak action.
- Splenic capsule: Contracts resulting in the release of RBCs into circulation.
- Pilomotor: Pilomotor muscles of the hair follicle contract.
- Bladder: The detrusor is relaxed (b3 receptors) and trigone is contracted → increasing the holding capacity of the bladder.
4. Eye:
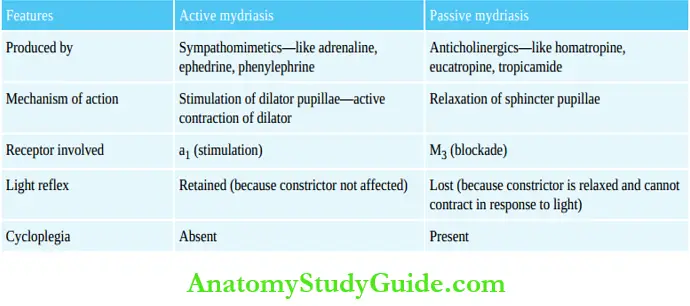
- Causes mydriasis by active contraction of the radial muscles (α1) of the iris—active mydriasis
- Also reduces intraocular pressure—reduces both the production of aqueous humor (b) and improves its drainage (a receptor) (see Compare and Contrast)

Active mydriasis and Passive mydriasis:
5. Metabolic effects:
- Adrenaline increases the blood sugar level by increasing hepatic glycogenolysis. It also inhibits insulin release.
- By increasing the breakdown of triglycerides in the adipose tissue, more free fatty acids are made available in the plasma by action on b3 receptors in adipocytes.

6. Skeletal muscles:
Catecholamines facilitate neuromuscular transmission by action on both α and β receptors and they increase the amount of ACh released.
Adrenaline Pharmacokinetics:
Because catecholamines are rapidly inactivated in the gut and the liver, they are not given orally. Adrenaline and NA are metabolized by COMT and MAO
Adrenaline Adverse reactions:
- Anxiety, palpitation, weakness, tremors, pallor, dizziness, restlessness, and throbbing headache may follow adrenaline/NA administration.
- In patients with ischemic heart disease, both adrenaline and NA can precipitate anginal pain.
- Rapid IV injection can cause a sudden sharp rise in BP which may precipitate arrhythmias, subarachnoid hemorrhage or hemiplegia.
Uses Of Adrenaline
Question 7 . Write a short note on the uses of adrenaline.
Answer:
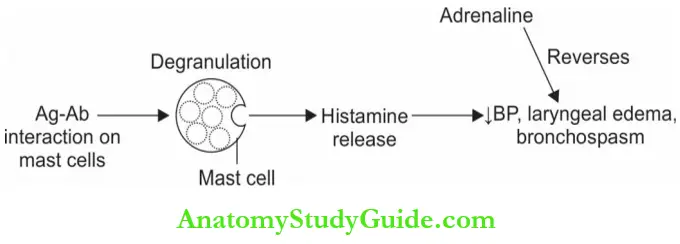
1. Anaphylactic shock:
- Adrenaline—drug of choice (0.3–0.5 mL of 1:1,000 solution) promptly reverses hypotension, laryngeal edema and bronchospasm and is life-saving in anaphylactic shock.
- Adrenaline is also life-saving in angioneurotic edema of the larynx.
- Absorption by SC route is not reliable in shock → IM route is preferred.’
2. Bronchial asthma: Though adrenaline is a bronchodilator, it is not preferred as more selective (b2) drugs are available.
3. Cardiac arrest: Sudden cardiac arrest due to drowning, electrocution, etc. are treated with cardiopulmonary resuscitation (CPR) and IV or intracardiac adrenaline 1 mg into 4th or 5th intercostal space, 2–3 inches from the sternum; before injecting, ensure that the tip of the needle is in the heart. If the piston of the syringe is withdrawn, blood should enter the
syringe.
4. Control of hemorrhage: Adrenaline (1: 10,000 to 1:20,000) topical hemostatic to control bleeding as it causes vasoconstriction. Adrenaline packs are used for bleeding after tooth extraction and in epistaxis.
5. With local anesthetics: Injected with LA, adrenaline causes vasoconstriction and reduces the rate of absorption of LA. This, it prolongs the action and reduces systemic toxicity of LA. 1:10,000 to 1:2,00,000 adrenaline is used.
6. Glaucoma: Adrenaline decreases IOP and can be used in glaucoma, but it has the disadvantages of being:
- Poorly absorbed.
- Short-acting as it is quickly metabolized in the eye.
Hence dipivefrine—a prodrug of adrenaline is used
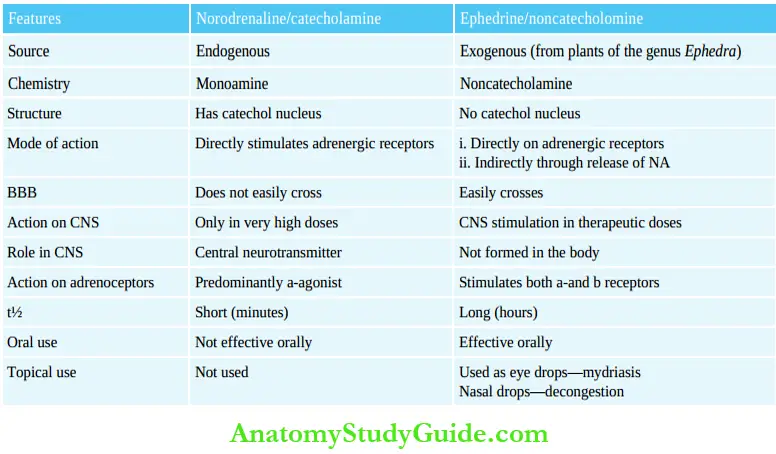
Noradrenaline and Ephedrine:
Adrenaline and Noradrenaline:

Question 8. Write a short note on dopamine or discuss briefly the actions and uses of dopamine.
Answer:
Dopamine a precursor of NA acts on dopaminergic and adrenergic receptors. There are 5 subtypes of dopamine receptors: D1–D5.
- Dopamine is a central neurotransmitter. Low doses stimulate vascular D1 receptors in renal, mesenteric, and coronary beds causing vasodilatation in these vessels.
- D2 receptor stimulation in the sympathetic nerve terminals and in cardiovascular centers also results in renal vasodilation.
- Hence, renal blood flow and GFR increase.
- Higher doses cause cardiac stimulation through b1 receptors resulting in an increase in the force of contraction with a minor increase in the heart rate.
- In high doses a1 receptors are activated causing vasoconstriction and ↑ BP.
- Dopamine does not cross the BBB, hence it has no CNS effects. DA is given IV, short-acting and the infusion rate can be adjusted to get the appropriate effect by monitoring BP.
- Dopamine is metabolized by COMT and MAO. Epinine (ibopamine) is an ester of methyl dopamine which acts like dopamine.

Dopamine Adverse effects:
Nausea, vomiting, palpitation, headache, angina, and sudden rise in BP may occur.
Question 11. Give the rationale for the use of dopamine in shock.
Answer:
Dopamine Uses: Dopamine is used in the treatment of shock—cardiogenic, hypovolemic, and septic.
It is especially useful when there is renal dysfunction and low cardiac output because:
- DA ↑ renal blood flow and thereby GFR
- DA stimulates the heart—↑ FOC, ↑ cardiac output, and BP.
- DA is short-acting and therefore the response can be easily controlled by modifying the infusion rate.
- Dose: 2–5 mg/kg/min.
Question 9. What is dobutamine? Write its uses.
Answer:
Dobutamine a derivative of dopamine is a relatively selective b1-agonist.
- Though it stimulates a1, b1, and b2 receptors, in therapeutic doses the only dominant action is an increase in the force of contraction of the heart without much increase in the heart rate.
- Hence, the increase in myocardial O2 demand is milder when compared to dopamine and is therefore more useful than dopamine in cardiogenic shock.
Dose: 2–15 mg/kg/min
Uses: In pump failure as in CCF or acute myocardial infarction or following cardiac surgery

Question 10. Write a short note on ephedrine.
Answer:
- Ephedrine is an alkaloid from the plants of the genus Ephedra
- Ephedrine acts by direct stimulation of a and b-receptors and indirectly through the release of NA.
- Actions—raises BP by peripheral vasoconstriction and by increasing the cardiac output.
- Repeated frequent administration results in tachyphylaxis.
- Like adrenaline, it is a bronchodilator (b2).
- CNS stimulant → produces insomnia, restlessness, anxiety, tremors, and increased mental activity.
- Ephedrine has good oral bioavailability and a t½ of 4–6 hours.

Ephedrine Adverse effects:
Gastric upset, insomnia, tremors, difficulty in micturition, anxiety, and restlessness.
Ephedrine Uses: Ephedrine is not preferred now as safer drugs are available.
- Hypotension: Used for prevention and treatment of hypotension (IM/IV) during spinal
anesthesia. - Mydriasis: Ephedrine eye drops are used to produce mydriasis without cycloplegia.
- Narcolepsy: It is an irresistible desire and tendency to sleep. As ephedrine is a CNS
stimulant, it is useful in narcolepsy. - Bronchial asthma: Was used in mild bronchial asthma but is not preferred now.
- Nasal decongestion: Pseudoephedrine—an isomer of ephedrine is preferred over ephedrine because its effects on the CNS and the heart are milder.
- Nocturnal enuresis (bed-wetting) in children: It increases the holding capacity of the bladder but drugs should be avoided. Also useful in urinary incontinence in adults.
Question 11. Write a short note on amphetamine.
Answer:
Amphetamine is an indirectly acting sympathomimetic with actions similar to ephedrine. It promotes the release of NA from central nerve terminals.
Amphetamine Actions:
- CNS: Amphetamine is a potent CNS stimulant On repeated use tachyphylaxis develops.
- Respiration: Stimulates respiratory center (analeptic).
- Suppression of appetite: Acting on the feeding center in the hypothalamus, amphetamine suppresses appetite and reduces hunger.

Amphetamine Adverse effects:
Including restlessness, tremors, insomnia, palpitation, anxiety, confusion and hallucinations.
- Dependence: Amphetamine causes addiction and dependence. Long-term use results in psychosis and other behavioral abnormalities.
- Toxicity: High doses cause headache, nausea, vomiting, abdominal cramps, flushing, angina, delirium, arrhythmias, hypertension, restlessness, suicidal or homicidal tendencies, acute psychosis, followed by coma and death due to convulsions.
- Treatment: Acidification of urine with ammonium chloride to increase urinary excretion of amphetamine; sedatives, α blockers/sodium nitroprusside to control the BP and chlorpromazine to control the psychosis. Peritoneal dialysis may be needed.
Amphetamine Uses:
- Attention deficit hyperactivity disorder (ADHD) in children is characterized by decreased ability to concentrate and hold attention, aggressive behavior, and hyperactivity;
- Though amphetamine increases attention span in such children, due to the risk of addiction it is not preferred for this purpose. Modafinil—a CNS stimulant is useful in such patients.
- Narcolepsy: Though amphetamine is effective, dependence liability makes it less used.
- Obesity: Though appetite is suppressed, due to the risk of dependence and the side effects, amphetamine should not be used for this purpose.
Vasopressors:
Question 15. Write a short note on vasopressors.
Answer:
Vasopressors are a1-agonists and they are:
- Noradrenaline, dopamine, metaraminol, mephentermine, midodrine, phenylephrine, and methoxamine.
- They cause the contraction of vascular smooth muscles by activating the a1 receptors in them.
- They increase the BP by increasing total peripheral resistance (TPR) or cardiac output (CO) or both. The rise in BP is associated with reflex bradycardia.
- Vasopressors are given parenterally with constant monitoring of BP. Hypovolemia if any should be corrected before administration of vasopressors. Tachyphylaxis may develop.

Vasopressors Uses
- To raise the BP in hypotension as seen in cardiogenic or neurogenic shock and during spinal anesthesia.
- Some of them are also nasal decongestants.
- Phenylephrine: Is used as a vasopressor, nasal decongestant and mydriatic.
- Midodrine: Midodrine is an orally effective prodrug converted to the active metabolite which contracts both arterial and venular smooth muscles and is useful in controlling orthostatic hypotension, particularly in autonomic imbalance.
Nasal Decongestants
Question 12. Write a short note on nasal decongestants.
Answer:
Nasal decongestants are a1-agonists. They are:
- Oral ephedrine, pseudoephedrine, phenylephrine
- Topical (nasal drops) oxymetazoline, xylometazoline, naphazoline Phenylephrine, mephentermine, and metaraminol.
Ephedrine hydrochloride relieves congestion and the effect lasts up to 6 hours. Pseudoephedrine is a component of several cold remedies given orally. Topically acting agents should be used carefully and patients should be warned against overuse.
Nasal Decongestants Mechanism of action:
- Nasal decongestants act by stimulating the a1 receptors present in the blood vessels of the nasal mucosa. They relieve nasal congestion also reduce nasal secretion.
- The nasal decongestants thus provide only symptomatic relief in rhinitis due to allergy and upper respiratory infections.

Nasal Decongestants Adverse effects:
- Oral ephedrine and pseudoephedrine—can cause insomnia, tremors, and irritability.
- Topical agents can cause nasal irritation.
- Prolonged use can cause:
- Atrophy of the nasal mucosa due to intense vasoconstriction.
- Recongestion or ‘after congestion’ when the drug is stopped (due to vasodilatation).
- Loss of efficacy or tolerance due to desensitization of the receptors.
- Nasal decongestants should be used carefully in patients with hypertension.
- Phenylpropanolamine was widely used in cold remedies but its use can increase the risk of hemorrhagic stroke and is therefore banned.
Nasal Decongestants Uses:
- Rhinitis in upper respiratory infections.
- Allergic and vasomotor rhinitis and sinusitis.
- Blocked eustachian tubes.
Leave a Reply