History, Taxonomy, Morphology and Physiology of Bacteria and Microbial Pathogenicity
History
Louis Pasteur
Table of Contents
Louis Pasteur is also known as father of microbiology. He has many contributions to microbiology:
- He has proposed the principles of fermentation preservation of food.
- He introduced sterilization techniques and developed steam sterilizers, hot air over autoclave
- He described the method of pasteurization milk
- He had also contributed for designing the vaccines against several diseases such as anthrax, fowl cholera and rabies
- He disproved the theory of spontaneous generation of disease and postulated the ‘germ theory of disease’. He stated that disease cannot be caused by bad air or vapor, but it is produced by the microorganisms present in
- Liquid media concept- He used nutrient broth to grow microorganisms
- He was the founder of the Pasteur Institute, Paris.
Robert Koch
Read And Learn More: Micro Biology And Immunology Notes
Robert Koch provided remarkable contributions to the field of microbiology:
- He used of solid media for culture of bacteria-Eilshemius Hesse, the wife of Walther Hesse, one of Koch’s assistants had suggested the use of agar as solidifying agent.
- He also introduced methods for isolatio of bacteria ipure culture.
- Described hanging drop method for testing motility.
- Discovered bacteria such as the anthrax bacilli, tubercle bacilli, and cholera bacilli.
- Introduced staining techniques by using aniline dye.
- Koch’s phenomenon: Robert Koch observed that guinea pigs already infected with tubercle bacillus developed a hypersensitivity reaction whe injected with tubercle bacilli or its protein. This reaction is called Koch’s phenomenon.
- Koch’s Postulates:
According to Koch’s postulates, a microorganism cabe accepted as the causative agent of a infectious disease only if the following conditions are fulfilled:
- The microorganism should be constantly associated with the lesions of the disease.
- It should be possible to isolate the organism ipure culture from the lesions of the disease.
- The same disease must result whethe isolated microorganism is inoculated into a suitable laboratory animal.
- It should be possible to re-isolate the organism ipure culture from the lesions produced ithe experimental
animals.
An additional fifth criterion was introduced subsequently which states that antibodies to the causative organism should be demonstrable in the patient’s serum.
Exceptions to Koch’s postulates: It is observed that it is not always possible to apply these postulates to study all the human diseases. There are some bacteria that do not satisfy all the four criteria of Koch’s postulates. Those organisms are:
4/3 Mycobacterium leprae and Treponema pallidum: They cannot be growivitro; however cabe maintained in
experimental animals.
4/3 Neisseria gonorrhoeae: There is no animal model; however, it cabe growivitro.
Molecular Koch’s postulates: It was a modification of Koch’s postulates (by Stanley Falkow). He stated that gene (coding for virulence) of a microorganism should satisfy all the criteria of Koch’s postulates rather than microorganism itself.
Paul Ehrlich
- He was the first to report the acid-fast nature of tubercle bacillus.
- He developed techniques to start issues and blood cells.
- He proposed a toxiantitoxiinteractio called as Ehrlich phenomenoand also introduced methods of standardising toxiand antitoxin.
- He proposed the ‘side chaitheory for antibody production’.
- He discovered ‘salvarsan’, aarsenical compound (magic bullet) for treatment of syphilis, hence knowas father of chemotherapy.
- The bacteria ‘Ehrlichia’was named after him.

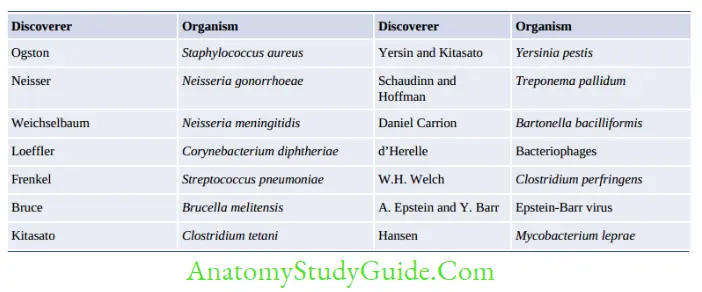
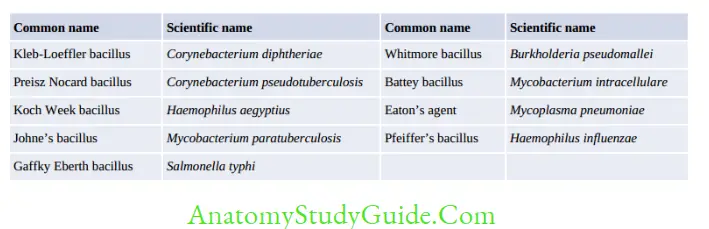
Other Important Contributors Microbiology
- Antonie Philips van Leeuwenhoek: Discovered single-lens microscope and named organisms as ‘Little animalcules’.
- Edward Jenner: Developed the first vaccine of the world, the smallpox vaccine by using cowpox virus.
- Joseph Lister: He is considered to be the father of antiseptic surgery. He used carbolic acid during surgery.
- Hans ChristiaGram: He developed ‘Gram stain’.
- Ernst Ruska: He was the founder of electro microscope.
- Alexander Fleming: He discovered the antibiotic penicillin.
- Elie Metchnikoff: He described phagocytosis and termed phagocytes.
- Kleinberger: He described the existence of L forms of bacteria.
- Barbara McClintock: She described transposons.
- Walter Gilbert and Frederick Sanger: were the first to develop (1977) the method of DNA sequencing.
- Karry B Mullis: Discovered polymerase chair action (PCR).
Bacterial Taxonomy
Cavalier-Smith’s six kingdoms classification (1998) is the most recent and widely used taxonomic classification. It divides organisms into 6 kingdoms Bacteria, Protozoa, Chromista, Plantae, Fungi, and Animalia.
Principle used for Bacterial Classification
- Phylogenetic classification: This is a hierarchical classification representing a branching tree-like arrangement; one characteristic (or trait) is being employed for divisioat each node of the tree.
- Adansonia(or phonetic) classification: To avoid the use of weighted characteristics,Michel Adansoproposed a scheme that classifies organisms based ogiving equal weight to every character of the organism. This principle is used inumeric taxonomy.
- Molecular classification: Based ogenetic relatedness (guanine + cytosine content) of different organisms.
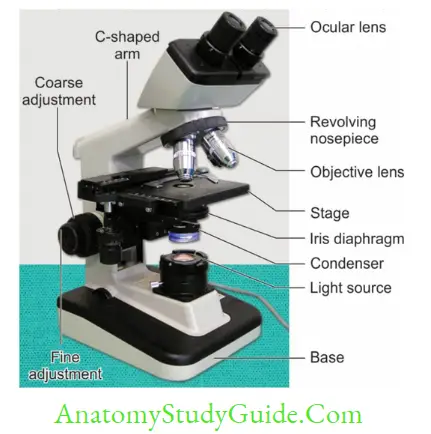
Microscopy
A good microscope should have three properties:
- Good resolution: Resolutiopower refers to the ability to produce separate images of closely placed objects so that they cabe distinguished as two separate entities. The resolution power of:
- Unaided human eye is about 0.2 mm (200 µm)
- Light microscope is about 0.2 µm
- Electron microscope is about 0.5 nm
Resolutiodepends or refractive index. Oil has a higher refractive index than.
- Good contrast: This cabe further improved by staining the specimen.
- Good magnification: This is achieved by use of concave lenses.
Bright-Field or Light Microscope
The bright-field or light microscope forms a dark image against a brighter background.
Dark Field Microscope
- Principle: Idark field microscope, the object appears bright against a dark background.
This is made possible by use of a special dark field condenser. - Applications: It is used to identify the living, unstained cells and the bacteria like spirochetes which cannot be visualized by light microscopy.
Phase Contrast Microscope
It is used to visualize the living cells by creating difference icontrast between the cells and water. It converts slight differences in refractive index and cell density into easily detectable variations in light intensity. It is useful for studying:
- Microbial motility
- Determining the shape of living cells
- Detecting bacterial components such as endospores and inclusion bodies.
Fluorescence Microscope
Principle: Whefluorescent dyes are exposed to ultraviolet (UV) rays, they become excited and are said to fluoresce, i.e. they convert this invisible, short wavelength rays into light of longer wavelengths (visible light).
Applications: Epifluorescence microscope has the following applications:
- Autofluorescence, wheplaced under UV lamp, e.g. Cyclospora
- Microbes coated with fluorescent dye, e.g. Acridine orange for malaria parasites (QBC) and Auramine phenol for M. tuberculosis.
- Immunofluorescence: It uses fluorescent dye tagged antibody to detect cell surface antigens or antibodies bound to cell surface antigens. There are two types: Direct IF and indirect IF.
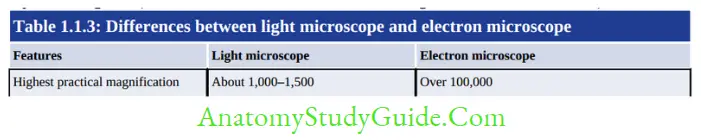
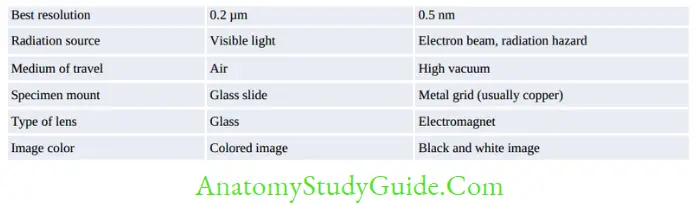
- electron microscope
It was invented by Ernst Ruska i1931. It differs from light microscope by various ways (table givebelow). There are two types of EM: - TransmissioEM (MC type, examine the internal structure, resolutio0.5 nm, gives 2-dimensional view)
- Scanning EM (examine the surfaces, resolutio7 nm, gives 3 dimensional view)
Principle of Transmission Electron Microscope
Specimen preparation: Cells are subjected to the following steps to prepare very thin specimens (20 to 100 nm thick)
- Fixation: Cells are fixed by using glutaraldehyde or osmium tetroxide for stabilization.
- Dehydration: Specifies the dehydrated with organic solvents (e.g. acetone or ethanol).
- Embedding: Specimeis embedded plastic polymer and then, is hardened to form a solid block. Most plastic polymers are water insoluble; hence complete dehydratioof specimen is must before embedding.
- Slicing: Specimeis thecut into thin slices by ultramicrotome knife, and slices are mounted oa metal slide (copper).
Freeze-etching technique: It is alternative method for specime preparatioto visualize the internal organelles with in the cells. Cells are rapidly frozen the warmed → fractured by a knife exposing the internal organelles → subjected to sublimatio→ shadowed by coating with platinum and carbon.
Measures to increase the contrast of EM include:
- Staining by using solutions of heavy metal salts like lead citrate and uranyl acetate
- Negative staining with heavy metals like phosphotungstic acid or uranyl acetate.
- Shadowing: Specimeis coated with a thin film of platinum or other heavy metal at 45° angle so that the metal strikes the microorganism oonly one side
Staining Techniques
Staining is necessary to produce color contrast and thereby increase the visibility of the object.
Before staining, the fixation of the smear to the slide is done:
- Heat fixation is usually done for bacterial smears by gently flame heating air-dried film of bacteria
- Chemical fixation such as ethanol, acetic acid, mercuric chloride, formaldehyde, methanol, and glutaraldehyde. This is useful for examination of blood smears.
Staining Techniques Used in Microbiology
- Simple stain: Basic dyes such as methylene blue or basic fuchsia used as simple stains.
They provide the color contrast, but impart the same color to all the bacteria ia smear. - Negative staining, e.g. India ink or nigrosin. The background gets stained black whereas unstained bacteria stand out icontrast. This is very useful ithe demonstration of bacterial capsules which do not take up simple stains.
- Impregnatiomethods (e.g. silver): Used for demonstration of the structures like bacterial flagella and spirochetes
- Differential stain: Two stains are used which impart different colors which help in differentiating bacteria, e.g.
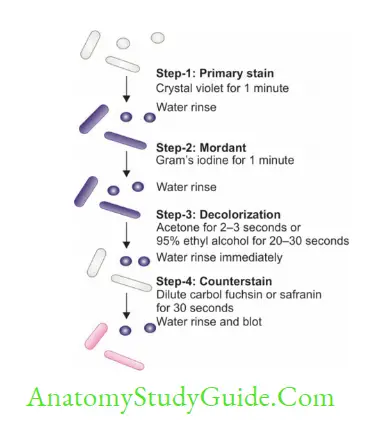
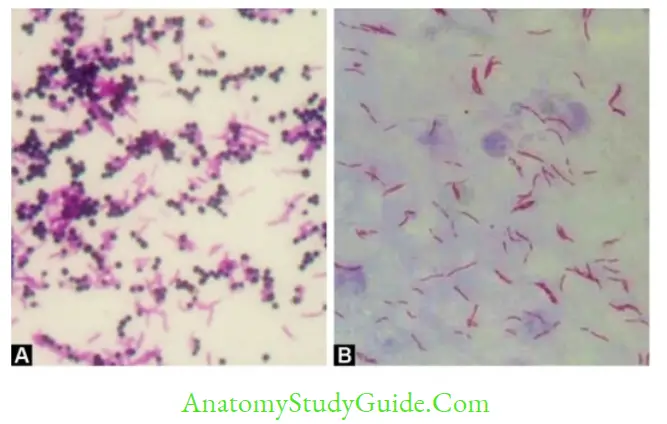
- Gram stain: Differentiates bacteria into Gram-positive (appear violet) and Gram-negative (appear pink) groups
- Primary staiby crystal violet (or gentian violet or methyl violet) for one minute.
- Mordant by Gram’s iodine for one minute.
- Decolorizatioby acetone (for 1–2 sec) or ethanol (20–30 sec) with immediate wash. Decolorizer removes the primary staifrom Gram-negative bacteria while the Gram-positive bacteria retaithe primary stain.
- Counterstaior Secondary stains by safranior dilute carbol fuchsin; is added for 30 sec.
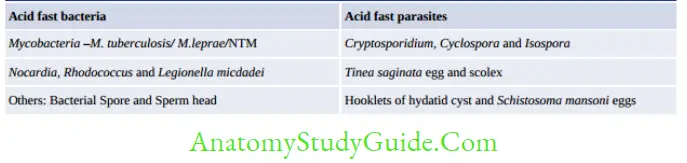
- Acid-fast stain: Acid-fast organisms (Table 1.1.4) resist decolorization mineral acids.
This is due to presence of mycolic acids itheir cell wall.. - Albert stain: Differentiates bacteria having metachromatic granules (e.g.
Corynebacterium diphtheriae) from other bacteria that do not have.
- Gram stain: Differentiates bacteria into Gram-positive (appear violet) and Gram-negative (appear pink) groups
- Other Special Staining Methods:
-
- Spore staining: Acid-fast stai(using 0.25% sulfuric acid) and Malachite green stain (Schaeffer and Fultomethod modified by Ashby) methods are used; however, phase contrast microscope of unstained wet film is the best method.
- Lipids stained by: SudaBlack stain.
- Carbohydrate (Glycogen) stained by Iodine stain.
- Flagellar stain: Tannic acid staining (Leifsomethod).
- Microscopy of Bacteria living State
- Unstained (wet) preparations: Used for:
- Checking bacterial motility (e.g. ihanging drop and wet mount preparations)
- For demonstration of spirochetes (e.g. idark field or phase contrast microscopy).
- Vital stains: Differentiate the living cells from dead cells:
- Isupravital staining, living cells that have beeremoved from a organism are stained; whereas intravital staining is done by injecting staiinto the body.
- Examples of vital stains are eosin, propidium iodide, trypablue, erythrosine and neutral red.
- Unstained (wet) preparations: Used for:
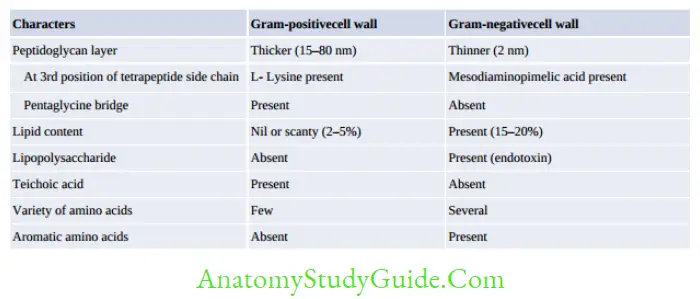
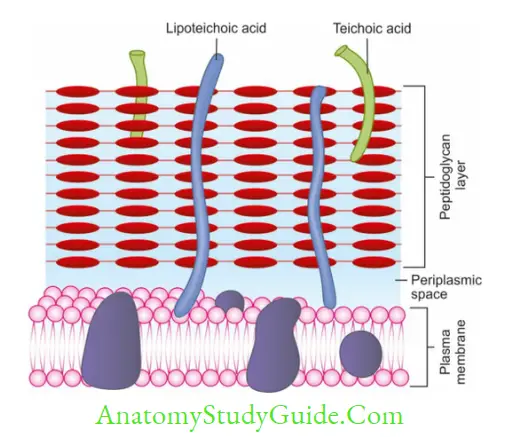
Bacterial Cell Wall
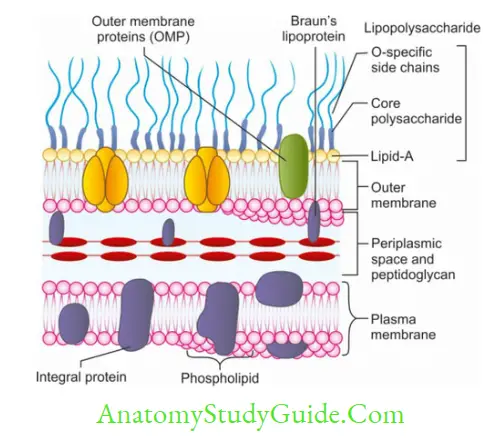
The cell wall is a tough and rigid structure, surrounding the bacterium. Apart from providing protection conferring rigidity, certain parts of cell wall (e.g. LPS) are immunogenic and act as virulence factor.
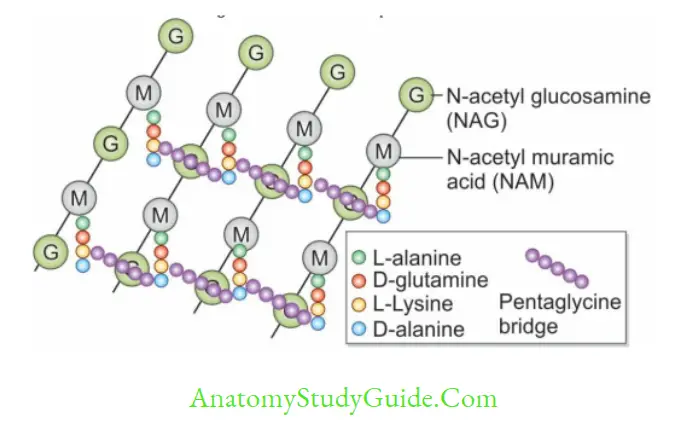
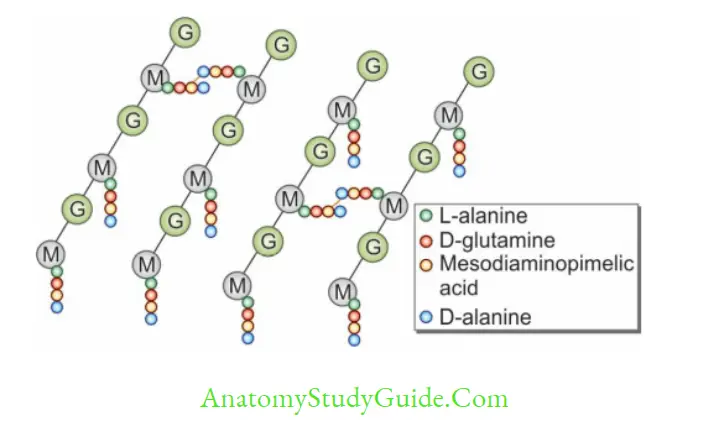
- Peptidoglycais the main component of the cell wall which makes it rigid. It is composed of alternate units of N-acetyl muramic acid (NAM) and N-acetyl glucosamine (NAG) molecules; cross linked to each other via tetrapeptide side chains and pentaglycine bridges.
- Gram-positive bacteria has a thicker peptidoglycaand contains teichoic acid.
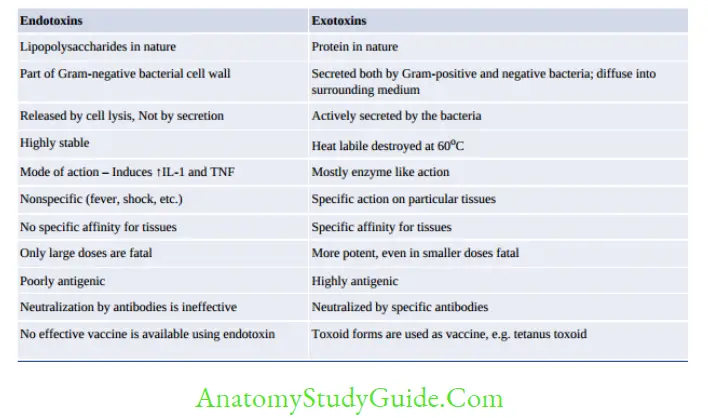
- Gram-negative bacteria-peptidoglycan layer is thin, and it contains additional parts such as (1) Outer membrane, (2) Lipopolysaccharide (LPS) which iturconsists of 1. Lipid A or endotoxin, 2. Core polysaccharide, the 3. O side chain.
Other Parts of Bacterial Cell
Intracytoplasmic Inclusions
They are the storage sites of nutrients/energy, formed inutritional deficiency conditions:
- Organic inclusion bodies, examples include glycogen granules and poly-hydroxyl butyrate granules.
- Inorganic inclusion bodies, examples include:
- Polymetaphosphate or volutior metachromatic granules iC. diphtheria.
- Sulfur granules found actinomyces.
Nucleoid
Bacteria do not have a true nucleus; but the genetic material is located iairregularly shaped regiocalled the nucleoid.
- There is no nuclear membrane or nucleolus and lacks basic proteins.
- Possess a single haploid chromosome, comprising of super coiled circular ds DNA (except two chromosomes iVibrio).
- Bacterial DNA divides by simple binary fission.
- The nucleoid can be seen electron microscopy or obtaining with the Feulgestain
- Bacteria also possess extra-chromosomal DNA called plasmids.
Capsule and Slime Layer
Some bacteria possess a layer of amorphous viscid material lying outside the cell wall called glycocalyx; which may be well-organized (capsule) or unorganized loose material (slime layer).
Some bacteria may possess both capsule and slime layer as streptococcus salivarius.
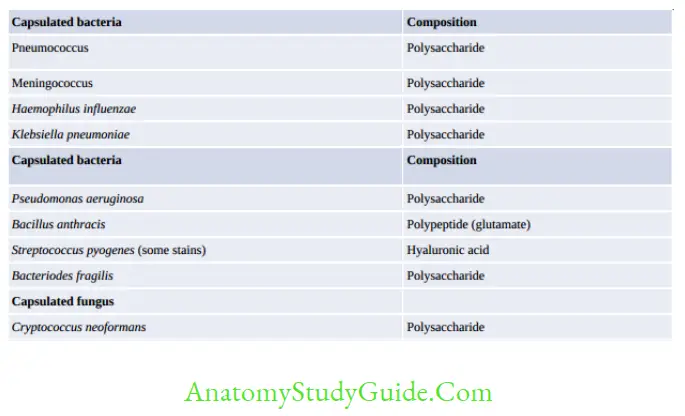
The capsule has various functions
- Acts by inhibiting phagocytosis and complement-mediated lysis
- Biofilm formation and thereby helps iadherence to damaged tissues and plastic surfaces (e.g. medical devices)
- Source of nutrients and energy for the bacteria
- Capsules as vaccine, e.g. Pneumococcus, Meningococcus and Haemophilus influenzae serotype-b and S. typhi Vi vaccine.
Demonstration of capsule by
- Negative staining by India ink and nigrosistain: Capsule appears as a clear refractile halo around the bacteria; whereas both the bacteria and the background appear black.
- M’Faydeacapsule stair Bacillus anthracis by using polychrome methylene blue stain.
- Serological test: Capsular material is antigenic and cabe demonstrated by mixing it with a specific anticapsular serum:
- Quellung reactiofor Streptococcus pneumoniae
- Latex agglutination test by using specific anticapsular antibodies coated olatex.
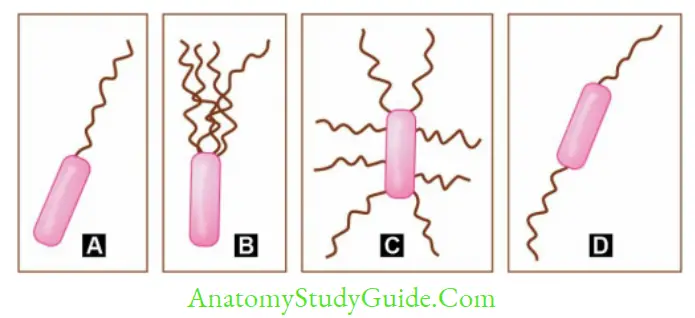
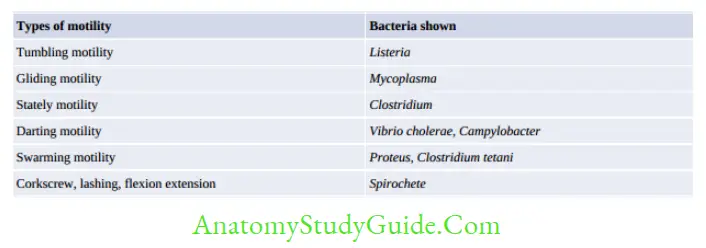
- Flagella
Flagella are thread-like appendages, protruding from the cell wall, composed of protein subunits called flagellin. It has three parts: filament, hook and basal body.
- Size-They measure 5–20 µm ilength and 0.01–0.02 µm thickness.
- They are organs of locomotion, confer motility to the bacteria.
- Arrangement of flagella
- Monotrichous (single polar flagellum) e.g. Vibrio cholerae,
- Pseuodmonas and Campylobacter
- Lophotrichous (multiple polar flagella) e.g. Spirillum.
- Peritrichous (over the entire cell surface) e.g. Salmonella Typhi, Escherichia coli.
- Amphitrichous (single flagellum at both the ends) e.g.
- Alcaligenes faecalis, Spirillum
- (Note: Spirillum has tuft of flagella at one or both the ends (Amphi>lophotrichous)
Flagella cabe demonstrated by
Direct demonstration of flagella
-
- Tannic acid staining (Leifson’s method and Ryu’s method)
- Electron microscopy
- Indirect means by demonstrating the motility:
- Cragie tube method and Hanging drop method
- Semisolid medium, e.g. mannitol motility medium.
- Dark ground or phase contrast microscopy
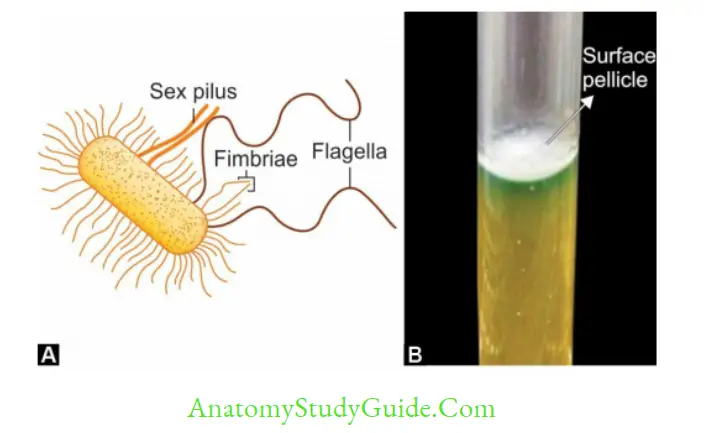
Fimbriae or Pili
Many Gram-negative and some Gram-positive bacteria possess short, fine, hair-like appendages that are thinner thaflagella and not involved imotility, called fimbriae or pili. They measure 0.5 µm long and 10 nm ithickness:
- Pili are made-up of proteicalled pilin.
- They are antigenic; however, the antibodies against fimbrial antigens are not protective.
- Functions: Fimbriae are called the orgaof adhesion. This property enhances the virulence of bacteria.
- Certaifimbriae called sex pili also help ibacterial gene transfer.
- Fimbriae are not related to motility, cabe found both imotile as well as inonmotile organisms.
- Types
- Commopili: These are of six types
- Sex or F (fertility) pili: Help ibacterial conjugation, they are found iGram-negative bacteria. e.g. as found in Gonococcus
- Col I (colicin) pili.
- Detection of fimbriae
- Direct demonstration of fimbriae by Electron microscopy
- Indirect methods to know the presence of fimbriae are:
- Hemagglutination: Many fimbriated bacteria (e.g. Escherichia coli, Klebsiella) strongly agglutinate RBCs. The hemagglutination can be is specifically inhibited by D-mannose.
- Surface pellicles, e.g. some aerobic fimbriated bacteria form a thin layer at the
Atypical Forms of Bacteria
- Involutioforms: Swolleand aberrant forms of bacteria (e.g. Gonococci and Yersinia pestis) eating cultures
- Pleomorphic bacteria: Different shape and size of individual cells, e.g. Proteus and Yersinia pestis
- L form or Cell wall deficient forms: Whebacteria loose cell wall, they become spherical called L form.
- Discovered by E. Klieneberger, while studying Streptobacillus moniliformis
- It is named after its place of discovery, i.e. Lister Institute, London
- L forms mediates persistence of pyelonephritis and other chronic infections.
- L forms iGram-positive bacteria are called Protoplasts and iGram-negative bacteria are called Spheroplasts.
- Mycoplasma do not have a true cell wall; the peptidoglycan layer is replaced by sterol.
It is postulated that Mycoplasma may represent stable L forms of yet-to-be-unidentified parent bacteria.
Bacterial Spores
Spores are highly resistant resting (or dormant) stage of the bacteria formed in unfavorable environmental conditions as a result of the depletion of exogenous nutrients.
- Structure of a spore: From innermost towards the outermost, the layers are core→ cortex→coat→ exosporium
- Sporicidal agents: Spores are highly resistant. Only limited sterilization methods are available to kill the spores
- Used as indicator for proper sterilization.
- Spores of Geobacillus stearothermophilus are used as sterilization control for autoclave.
- Spores of non-toxigenic strains of Clostridium tetani are used as sterilizatiocontrol for hot air oven.
- Used as agents of bioterrorism; e.g. Spores of Bacillus anthracis ithe 2001 USA attack.
Physiology Of Bacteria (Bacterialgrowth And Nutrition)
GenerationTime
Time required for a bacterium to give rise to two daughter cells under optimum condition.
Bacterial Count
Total count: Indicates total number of bacteria (live or dead) ithe specimen.
This is done by counting the bacteria under microscope using counting chamber.
- Viable count: Measures the number of living (viable) cells ithe givespecimen. Viable count may be obtained by:
- Pour plate method (best method)
- Surface viable count by spreading method
- Surface viable count by Miles and Misra method.
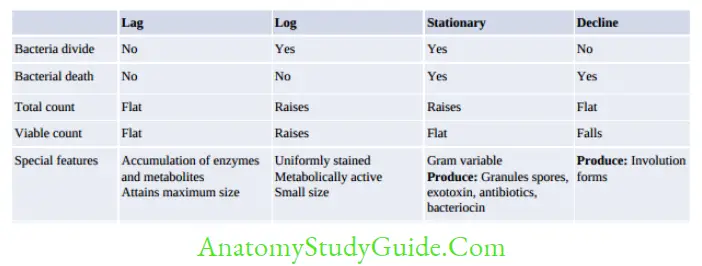
Bacterial Growth Curve
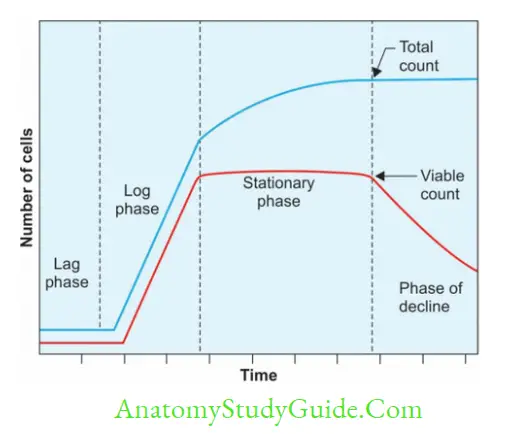
Whea bacterium is inoculated into a suitable liquid culture medium and incubated, its growth follows a definite course. When bacterial count of such culture is determined at different intervals and plotted relations time, a bacterial growth curve is obtained comprising of four phases.
Factors Affecting Growth of Bacteria
- Oxygen: Obasis of their oxygerequirements bacteria are classified as:
- Obligate aerobes: Grow only ithe presence of oxyge(e.g.
- Pseudomonas, M.tuberculosis, Bacillus, Brucella and Nocardia)
- Facultative anaerobes: They are aerobes that can also grow anaerobically (e.g. most of the Facultative aerobes: They are anaerobes that can also grow aerobically (e.g.Lactobacillus)
- Microaerophilic bacteria: Cagrow in the presence of 5–10% of oxygen (For Example. Campylobacter, Helicobacter, Mycobacterium bovis).
- Obligate anaerobes: Grow only in the absence of oxygen.
- Oxygeis lethal to these bacteria (e.g. Clostridium)
- Aerotolerant anaerobe: They tolerate oxygen for some time, but do not use it (Clostridium histolyticum).
- Carbon dioxide: Capnophilic bacteria need 5–10% of CO2. For Example. Brucella abortus, Streptococcus pneumoniae, etc.
- Temperature: Based optimal temperature needed for growth, bacteria can be grouped into:
- Psychrophiles: Grow below 20°C, e.g. saprophytes.
- Mesophiles: Grow betwee25°C and 40°C, e.g. most of the pathogenic bacteria
- Thermophiles: Grow above of 55°C – 80°C, e.g. Bacillus stearothermophilus.
- pH: Most pathogenic bacteria grow between 7.2 pH 7.6. Very few bacteria (lactobacilli) can grow at acidic pH below pH 4, while bacteria such as Vibrio cholerae are capable of growing at alkaline pH (8.2–8.9).
- Light: Bacteria (except phototrophs) grow well dark. They are sensitive to ultraviolet rays and other radiations in light. Photochromogenic mycobacteria produce pigments only on exposure to light.
- Other factors: Osmotic Effect, Mechanical and sonic Stresses, Moisture, and desiccation.
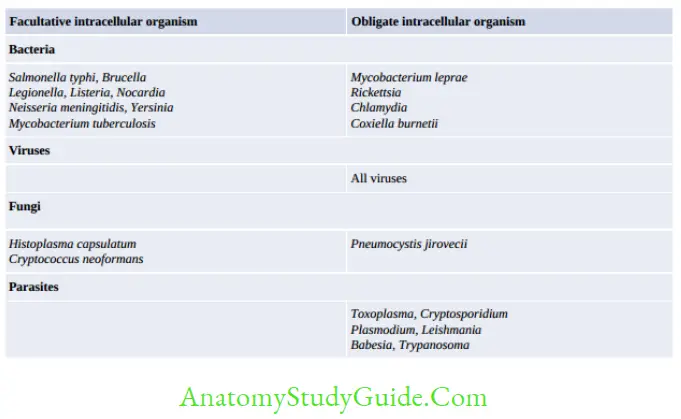
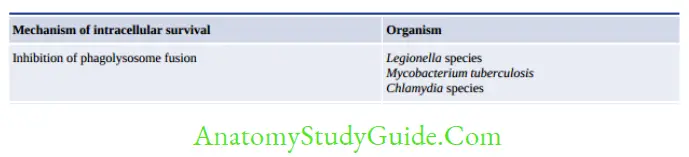
Microbial Pathogenicity
Microbial pathogenicity depends up on the sum total of several factors as described below.
- 1. Route of transmission of infection
- Infective dose of the organism: Minimum inoculum size that is capable of initiating a infection.
- Evasioof the local defenses
- Adhesion: By Fimbriae or pili, other adhesins, biofilm formation
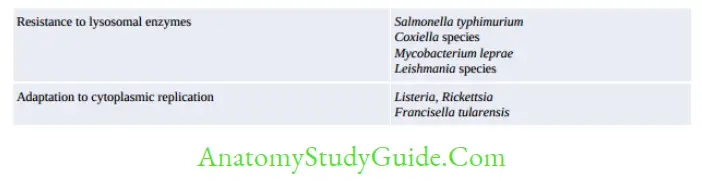
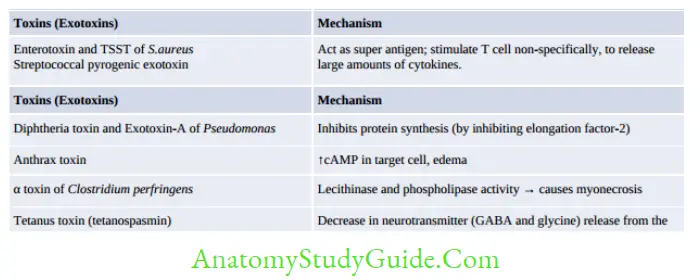
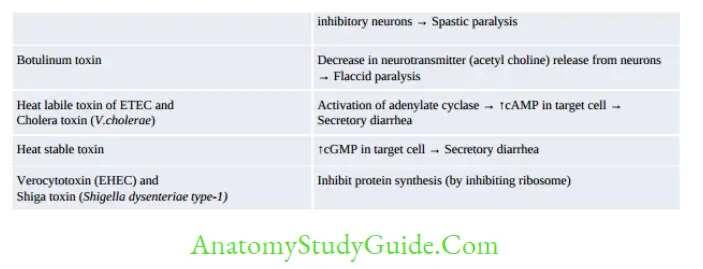
- Invasion: Virulence factors that help in vasio include:
- Virulence marker antigen invasion plasmid antigens shigella
- Enzymes: Invasion of bacteria is enhanced by many enzymes:
- Hyaluronidase, Collagenase, Streptokinase (fibrinolysin), and IgA proteases
- Antiphagocytic factors: Capsule
- Cell wall proteins such as: ProteiA of Staphylococcus aureus and M protein of Streptococcus pyogenes
- Cytotoxins: Interfere with chemotaxis or killing of phagocytes. For example, S. aureus produces hemolysins and leukocidins that lyse and damage RBCs and WBCs.
Leave a Reply