Response To Cell Injury And Causes
Cell injury is defined as the functional and morphologic effects of a variety of stresses on the cell from various etiologic agents which result in changes in its internal and external environment.
Table of Contents
However, when body cells are exposed to injurious agents, they have inbuilt mechanism te deal with changes in environment (or adapt) to a limited extent without undergoing cellular injury.
Read And Learn More: General Pathology Notes
Thus, the cellular response to stress may vary depending upon following two types of factors:
- Host factors i.e. the type of cell, nutritional status of cell etc.
- Factors pertaining to injurious agent i.e. its type, dose etc.
Read And Learn More: General Pathology Notes
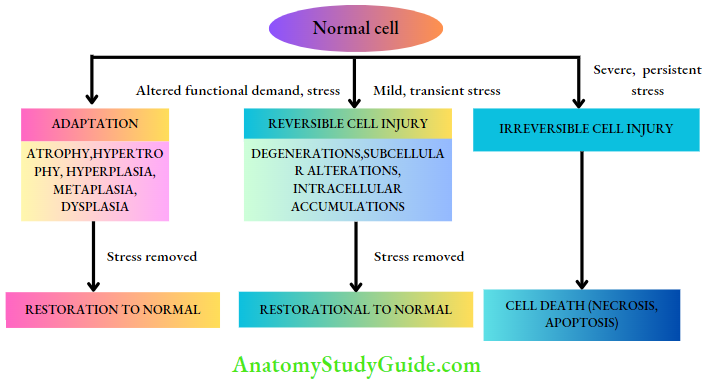
Accordingly, various forms of cellular responses to injurious agents may be as follows:
- When there is altered functional demand (increased or decreased), cells may adapt to changes that are expressed morphologically, which then revert back to normal after the stress is removed; these are termed cellular adaptations.
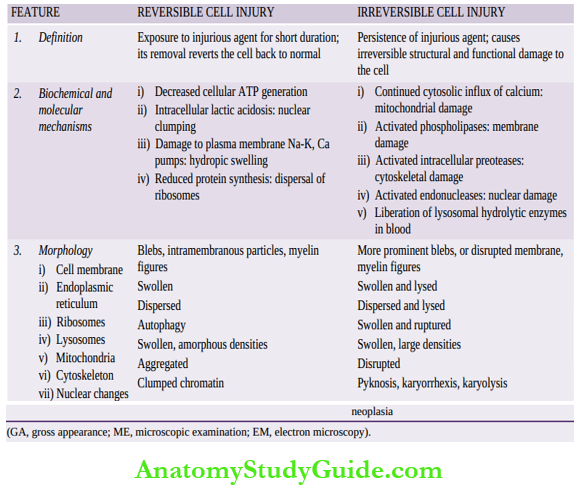
- When the stress is mild to moderate, the injured cell may recover (reversible cell injury), while persistent and severe form of cell injury may cause cell death (irreversible cell injury).
- The residual effects of reversible cell injury may persist in the cell as evidence of cell injury at subcellular level (subcellular changes), or metabolites may accumulate within the cell (intracellular accumulations).
Etiology Of Cell Injury:
Diverse diseases affecting human beings at different ages can be broadly classified into 4 groups: developmental, inflammatory, neoplastic, and degenerative. In general, cell injury underlies all these diseases.
Cell injury may occur from one of the two broad groups of causes: genetic and acquired (or environmental). Genetic causes of various diseases are discussed in Chapter 10. Acquired causes of disease comprise vast majority of common diseases afflicting mankind.
Common acquired causes of cell injury, which may be acting singly or in combination, are as under:
1. Hypoxia And Ischaemia:
- Cells of different tissues essentially require oxygen to generate energy and perform metabolic functions.
- Deficiency of oxygen or hypoxia results in failure to carry out these activities by the cells. Hypoxia is the most common cause of cell injury.
Hypoxia may result from the following 2 pathways:
- The most common mechanism of hypoxic cell injury is by reduced blood supply to the cells due to interruption i.e. ischaemia.
- Hypoxia may also result from impaired blood supply from causes other than interruption for example, Disorders of oxygen-carrying RBCs (for example,Anaemia, carbon monoxide poisoning), heart diseases, lung diseases and increased demand of tissues.
2. Physical Agents:
- Physical agents in causation of disease are as under:
- Mechanical trauma (for example,Road accidents)
- Thermal trauma (for example,By heat and cold)
- Electricity
- Radiation (for example,Ultraviolet and ionising); and rapid changes in atmospheric pressure.
3. Chemicals And Drugs:
An ever-increasing list of chemical agents and drugs may cause cell injury.
Important examples include the following:
- Chemical poisons such as cyanide, arsenic, mercury
- Strong acids and alkalis
- Environmental pollutants
- Insecticides and pesticides
- Oxygen at high concentrations
- Hypertonic glucose and salt social agents such as alcohol and narcotic drugs; and therapeutic administration of drugs.
4. Microbial Agents:
Injuries by microbes include infections caused by:
- Bacteria
- Rickettsiae
- Viruses
- Fungi
- Protozoa
- Metazoa, and other parasites.
5. Immunologic Causes:
Immunity is a ‘double-edged sword’—it protects the host against various injurious agents but it may also turn lethal and cause cell injury for example,
- Hypersensitivity reactions
- Anaphylactic reactions and
- Autoimmune diseases.
- Immunologic tissue injury.
6. Nutritional Derangements:
A deficiency or an excess of nutrients may result in nutritional imbalances.
- Nutritional deficiency diseases may be due to overall deficiency of nutrients (for example, Starvation) of protein calorie (for example, Marasmus, kwashiorkor), of minerals (for example, Anaemia), or of trace elements.
- Nutritional excess is a problem of affluent societies resulting in obesity, atherosclerosis, heart disease and hypertension.
7. Ageing Cellular:
- Ageing or senescence leads to impaired ability of the cells to undergo replication and repair, and ultimately leads to cell death culminating in death of the individual.
8. Psychogenic Causes:
- There are no specific biochemical or morphologic changes in common acquired mental diseases due to mental stress, strain, anxiety, overwork and frustration for example, Depression, Schizophrenia.
- However, Problems of drug addiction, Alcoholism, and smoking result in various organic diseases such as liver damage, chronic bronchitis, lung cancer, peptic ulcer, hypertension, ischaemic heart disease etc.
9. Latrogenic Causes:
- Although as per the Hippocratic oath, every physician is bound not to do or administer anything that causes harm to the patient, there are some diseases as well as deaths attributed to iatrogenic causes (owing to physician).
- Examples include the occurrence of disease or death due to error in judgment by the physician and untoward effects of administered therapy (drugs, radiation).
10. Idiopathic Diseases:
- Idiopathic means “of unknown cause”. Finally, although so much is known about the etiology of diseases, there still remain many diseases for which exact cause is undetermined.
- For example, a most common form of hypertension (90%) is idiopathic (or essential) hypertension. Similarly, exact etiology of many cancers is still incompletely known.’
Response to Cell injury and Etiologic Agents:
- Cell injury is the functional and morphologic effects of a variety of stresses on the cell from various etiologic agents which result in changes in its internal and external environment.
- Cellular response to stress depends upon the type of cell and tissue involved, and the type and dose of injurious agent.
- When exposed to mild stress or due to altered functional demand, the cells adjust and adapt to a limit (cellular adaptation) and revert back to normal.
- Mild to moderate stress for shorter duration may cause reversible cell injury; severe and persistent stress causes cell death.
- Among various etiologic factors, hypoxia-ischaemia is the most important; others are chemical and physical agents, microbes, immunity, ageing etc
Cellular Adaptations
As outlined already, cellular adaptations are the adjustments which the cells make in response to stresses which may be for physiologic needs (physiologic adaptation) or a response to non-lethal pathologic injury (pathologic adaptation).
Broadly speaking, such physiologic and pathologic adaptations occur by following processes:
- Decreasing or increasing their size i.e. atrophy and hypertrophy respectively, or by increasing their number i.e. hyperplasia (postfix word -trophy means nourishment; -plasia means growth of new cells).
- Changing the pathway of phenotypic differentiation of cells i.e. metaplasia and dysplasia (prefix word meta- means transformation; dys- means bad development).
In general, adaptive responses are reversible on the withdrawal of stimulus. However, if the irritant stimulus persists for longer duration or is more lethal, the cells may not be able to survive and may either die or progress further for example, Cell death may occur in sustained atrophy; dysplasia may progress into carcinoma in situ.
Thus, the concept of evolution ‘survival of the fittest’ holds true for adaptation as ‘survival of the adaptable’. Common forms of cellular adaptive responses, their mechanisms and examples of physiologic and pathologic adaptations are briefly discussed here.
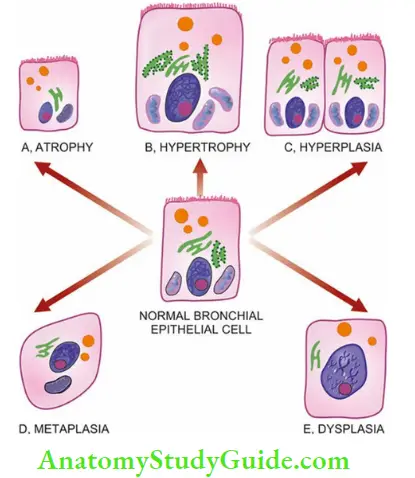
Atrophy:
Reduction of the number and size of parenchymal cells of an organ or its parts which were once normal is called atrophy (compared to hypoplasia which is the term used for developmentally small size, and aplasia for extreme failure of development with the presence of only rudimentary tissue).
Causes Of Atrophy:
Atrophy may occur from physiologic or pathologic causes:
1. Physiologic atrophy:
Atrophy is a normal process of ageing in some tissues, which could be due to loss of endocrine stimulation or from senile arteriolosclerosis.
For example:
- Atrophy of lymphoid tissue with age.
- Atrophy of thymus in adult life.
- Atrophy of gonads after menopause.
- Atrophy of the brain with ageing.
- Osteoporosis with reduction in the size of bony trabeculae due to ageing.
2. Pathologic atrophy The causes are as under:
- Starvation atrophy In starvation, there is first depletion of carbohydrate and fat stores followed by protein catabolism. There is general weakness, emaciation and anaemia referred to as cachexia seen in cancer and severely ill patients.
- Ischaemic atrophy Gradual diminution of blood supply due to atherosclerosis may result in shrinkage of the affected organ for example:
- Small atrophic kidney in atherosclerosis of renal artery.
- Atrophy of the brain in cerebral atherosclerosis.
- Disuse atrophy Prolonged diminished functional activity is associated with disuse atrophy of the organ for example:
- Wasting of muscles of limb immobilised in a plaster cast.
- Atrophy of the pancreas in obstruction of pancreatic duct.
- Neuropathic atrophy Interruption in nerve supply leads to wasting of muscles for example
- Poliomyelitis
- Motor neuron disease
- Nerve section.
- Endocrine atrophy Loss of endocrine regulatory mechanism results in reduced metabolic activity of tissues and hence atrophy for example,
- Hypopituitarism may lead to atrophy of the thyroid, adrenal and gonads.
- Hypothyroidism may cause atrophy of the skin and its adnexal structures.
- Pressure atrophy Prolonged pressure from benign tumours or cyst or aneurysms may cause compression and atrophy of the tissues for example,
- Erosion of the spine by tumour in nerve root.
- Erosion of the skull by meningioma arising from pia-arachnoid.
- Erosion of the sternum by aneurysm of arch of the aorta.
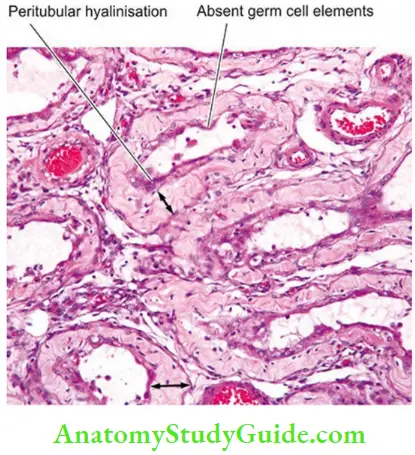
- Developmental disorders for example, cryptorchid testis due to incomplete descent of testis into normal scrotal position causing testicular atrophy.
- Idiopathic atrophy There are certain examples of atrophy where no obvious cause is present for example, Myopathies.
Morphologic Features Of Atrophy:
Irrespective of the underlying cause for atrophy, the pathologic changes are similar. The organ is small, often shrunken. The cells become smaller in size but are not dead cells.
Shrinkage in cell size is due to reduction in cell organelles, chiefly mitochondria, myofilaments and endoplasmic reticulum. There is often increase in the number of autophagic vacuoles containing cell debris.
These autophagic vacuoles may persist to form ‘residual bodies’ in the cell cytoplasm for example,Lipofuscin pigment granules in interstitial (Leydig) cells in testicular atrophy, thickened basement membrane and hyalinisation.
Molecular Pathogenesis Of Atrophy:
Atrophy from any of the above causes leads to an imbalance in cellular protein pathway: reduced synthesis and increased degradation:
- Reduced cellular protein synthesis is due to a deficient supply of nourishment to the cell.
- Increased cellular degradation of proteins occurs from activation of ubiquitin ligases which attach to cellular proteins and direct them to undergo degradation in proteasomes.
Hypertrophy:
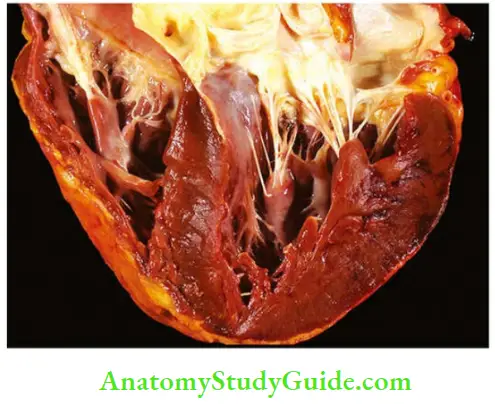
Hypertrophy is an increase in the size of parenchymal cells resulting in enlargement of the affected organ or tissue. Hypertrophy affects mainly all types of muscles.
Dividing cells may respond to stress by undergoing both hypertrophy and hyperplasia (for example, Uterine smooth muscle), while non-dividing cells undergo hypertrophy only (for example, Cardiac muscle).
Causes of Hypertrophy:
Hypertrophy may be physiologic or pathologic. In either case, it is caused by increased functional demand or by hormonal stimulation.
1. Physiologic hypertrophy:
Enlarged size of the uterus in pregnancy under oestrogenic stimulation is an example of physiologic hypertrophy (as well as hyperplasia).
2. Pathologic hypertrophy: Examples of certain diseases associated with hypertrophy are as
under:
- Hypertrophy of cardiac muscle may occur from chronic haemodynamic overload in a number of cardiovascular diseases for example,
- Systemic hypertension
- Aortic valve disease (stenosis and insufficiency)
- Mitral insufficiency
- Hypertrophy of smooth muscle for example,
- Cardiac achalasia (in oesophagus)
- Pyloric stenosis (in stomach)
- Intestinal strictures
- Muscular arteries in hypertension.
- Hypertrophy of skeletal muscle for example: Hypertrophied muscles in athletes and manual labourers.
- Compensatory hypertrophy of an organ may occur when the contralateral organ is removed for example:
- Following nephrectomy on one side in a young patient, there is compensatory hypertrophy as well as hyperplasia of the nephrons of the other kidney.
- Adrenal hyperplasia following removal of one adrenal gland.
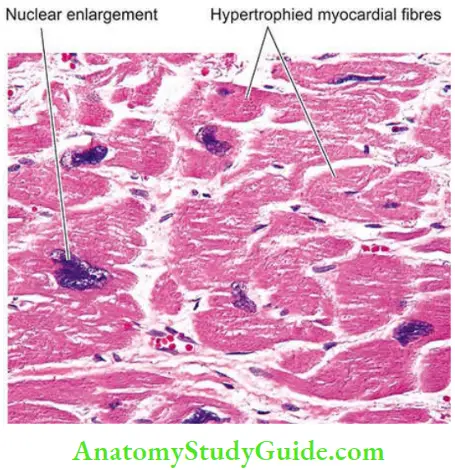
Morphologic Features of Hypertrophy:
Grossly, the affected organ is enlarged and heavy. For example, a hypertrophied heart of a patient with systemic hypertension may weigh 700-800 g as compared to average normal adult weight of 350 g
Microscopically, there is enlargement of muscle fibres as well as of nuclei. At the ultrastructural level, there is increased protein synthesis, increased number of myofilaments, and an increased number of organelles such as mitochondria, endoplasmic reticulum and myofibrils.
Molecular Pathogenesis of Hypertrophy:
Just as atrophy occurs from reduced cellular protein synthesis, hypertrophy results from increased synthesis of cellular proteins.
For example, in cardiac hypertrophy, increased protein synthesis is stimulated by the following pathway:
- Increased workload on the myocardial cell causes increased production of growth factors atthe cell membrane for example,TGF-β, fibroblast growth factor, insulin-like growth factor.
- This leads to activation of signal transduction pathways which activate transcription factors for example, GATA4, nuclear factor of activated T cells (NFAT) and myocyte enhancing factor 2 (MEF2).
- These, in turn, lead to increased myofibril contractile protein synthesis, production of growth factors and induction of embryonic or foetal genes (for example,Cardiac α-actin, atrial natriuretic factor ANF). The reappearance of the foetal genes in hypertrophy has a role in coping up cellular response to stress.
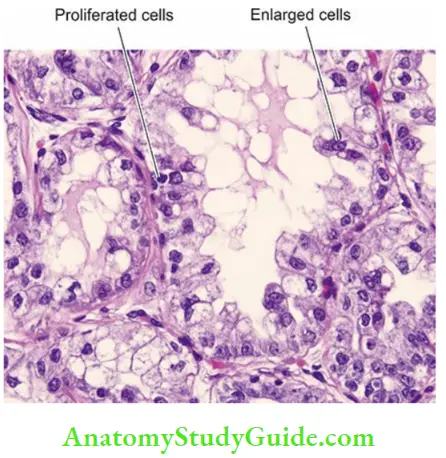
Hyperplasia:
Hyperplasia is an increase in the number of parenchymal cells resulting in enlargement of the organ or tissue. Quite often, both hyperplasia and hypertrophy occur together.
Hyperplasia occurs due to increased recruitment of cells from G0 (resting) phase of the cell cycle to undergo mitosis when stimulated. All body cells do not possess hyperplastic growth potential.
Labile cells (for example,Epithelial cells of the skin and mucous membranes, cells of the bone marrow and lymph nodes) and stable cells (for example, Parenchymal cells of the liver, pancreas, kidney, adrenal, and thyroid) can undergo hyperplasia, while permanent cells (for example, Neurons, cardiac and skeletal muscle) have little or no capacity for regenerative hyperplastic growth.
Neoplasia differs from hyperplasia in having hyperplastic growth with loss of growth-regulatory mechanism due to change in the genetic composition of the cell, while hyperplasia persists so long as stimulus is present
Difference between Hypetrophy and Hyperplasia:
Causes of Hyperplasia:
Hyperplasia may also be physiologic and pathologic.
1. Physiologic hyperplasia:
The two most common types are hormonal and compensatory:
- Hormonal hyperplasia i.e. hyperplasia occurring under the influence of hormonal stimulation for example:
- Hyperplasia (as well as hypertrophy) of female breast during pregnancy and lactation
- Hyperplasia (as well as hypertrophy) of the pregnant uterus.
- Compensatory hyperplasia i.e. hyperplasia occurring following removal of part of an organ or in the contralateral organ in paired organ for example:
- Restoration to normal size of the donor liver following lobectomy done for liver transplantation.
- Marrow hyperplasia following rapid loss of blood in haemolysis or blood donation.
2. Pathologic hyperplasia: Most examples of pathologic hyperplasia are due to excessive stimulation by hormones or growth factors on target cells for example:
- Endometrial hyperplasia following oestrogen excess.
- Usual ductal hyperplasia in fibrocystic changes of the breast.
- Benign prostatic hyperplasia in old age.
- Hyperplasia of the skin in non-healing ulcers, viral warts.
Morphologic Features of Hyperplasia:
There is enlargement of the affected organ or tissue and increase in the number of cells, often accompanied with hypertrophy. This is due to increased rate of DNA synthesis and hence increased mitoses of the cells
Molicular Mechanism of Hyperplasia:
Hyperplasia occurs from the proliferation of cells under the influence of growth factors. These growth factors act on receptors located on the neighbouring cells and activate their signalling pathways causing the proliferation of cells.
Salient distinguishing features between hypertrophy and hyperplasia are given in below
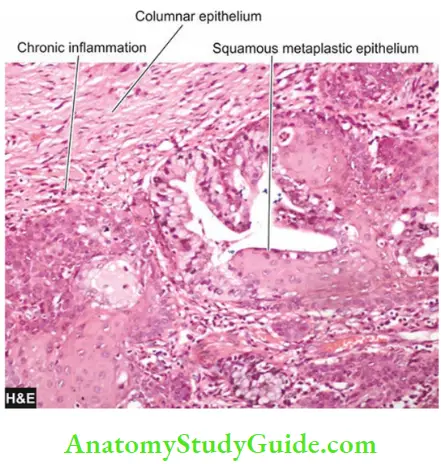
Metaplasia:
Metaplasia is defined as a reversible change of one type of mature differentiated epithelial or mesenchymal cells to another type of mature epithelial or mesenchymal cells, usually in response to abnormal stimuli, and the transformed cells are able to withstand the adverse effects of the irritant better.
Metaplasia often reverts back to normal on removal of stimulus but if the stimulus persists for a long time, epithelial metaplasia may progress to dysplasia and further into cancer.
Metaplasia is broadly divided into 2 types: epithelial and mesenchymal.
1. Epithelial Metaplasia:
Epithelial metaplasia is more common. Depending upon the type of epithelium transformed, it is of two types: squamous (more common) and columnar metaplasia.
The metaplastic change may be patchy or diffuse and usually results in replacement by stronger but less well-specialised epithelium. However, the metaplastic epithelium being less well-specialised such as squamous type, results in deprivation of protective mucus secretion and
hence more prone to infection.
- Squamous metaplasia: Various types of specialised epithelium are capable of undergoing squamous metaplastic change due to chronic irritants as stimuli which may be mechanical, chemical or infective in origin. Some common examples of squamous metaplasia are seen at following sites:
- In bronchus (normally lined by pseudostratified columnar ciliated epithelium) in heavy smokers.
- In uterine endocervix (normally lined by simple columnar epithelium) in prolapse of the uterus and in old age.
- In stones in ducts at different locations such as bile duct, pancreas, salivary glands, and prostate (normally lined by simple columnar epithelium).
- In renal pelvis and urinary bladder (normally lined by urothelium) in chronic infection and stones.
- In vitamin A deficiency, squamous metaplasia seen in xerophthalmia and in the respiratory tract.
- Columnar metaplasia: There are some conditions in which there is transformation to columnar epithelium. For example:
- Columnar metaplasia in Barrett’s oesophagus, in which there is change of normal squamous epithelium in the lower oesophagus to columnar epithelium and is a precancerous condition.
- Intestinal metaplasia in healed chronic gastric ulcer.
- Change of pseudostratified ciliated columnar epithelium in chronic bronchitis and bronchiectasis to columnar type.
2. Mesenchymal of Metaplasia:
Less often, there is transformation of one mature differentiated type of mesenchymal tissue to another. Often, it is osseous metaplasia i.e. formation of bone in fibrous tissue, cartilage and myxoid tissue. Examples of osseous metaplasia are as under:
- In arterial wall in old age (Mönckeberg’s medial calcific sclerosis)
- In myositis ossificans occurring following haematoma in soft tissues
- In cartilage of larynx and bronchi in elderly people
- In old scar of chronic inflammation of prolonged duration
- In the fibrous stroma of tumour e.g. in leiomyoma.
Molecular Pathogenesis of Metaplasi:
Metaplasia results from reprogramming of stem cells of one type of differentiated lineage of cells to another type of differentiated cell lineage.
Reprogramming of precursor stem cells to another pathway is possibly triggered by exogenous inciting stimuli and involves the generation of signals for dysregulation of transcription factors, cytokines and extracellular matrix components.
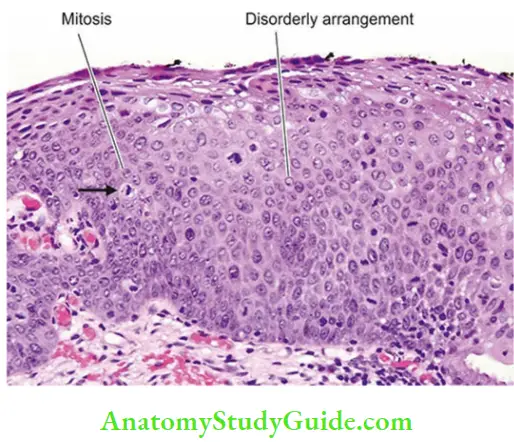
Dysplasia:
Dysplasia means ‘disordered cellular development’ often preceded or accompanied with metaplasia and hyperplasia; it is therefore also referred to as atypical hyperplasia.
Dysplasia occurs most often in epithelial cells. Epithelial dysplasia may be of varying grades (mild, moderate and severe).
Accordingly, it is characterised by cellular proliferation and cytologic changes of varying degree as under:
- Increased number of layers of epithelial cells
- Disorderly arrangement of cells from basal layer to the surface layerLoss of basal polarity i.e. nuclei
- Lying away from basement membrane
- Cellular and nuclear pleomorphism
- Increased nucleocytoplasmic ratio
- Nuclear hyperchromatism
- Increased mitotic activity due to accelerated cell proliferation.
The two most common examples of dysplastic changes are the uterine cervix and respiratory tract; other sites are oral cavity, oesophagus etc. In cervix, dysplasia of mild, moderate and severe grades is also termed as cervical intraepithelial neoplasia (CIN) of three grades (CIN, I, II, III)
Dysplastic changes often occur due to chronic irritation or prolonged inflammation. On removal of the inciting stimulus, mild and moderate dysplastic changes may disappear. However, if inciting stimulus persists for a long time, lower grades of dysplasia may progress to severe grade, to carcinoma in situ (cancer confined to layers superficial to basement membrane), or to invasive cancer.
Thus, dysplasia may be a precursor of carcinoma, but not always. As in cancer, dysplastic changes of varying grades involve mutations in genes of the affected cells.
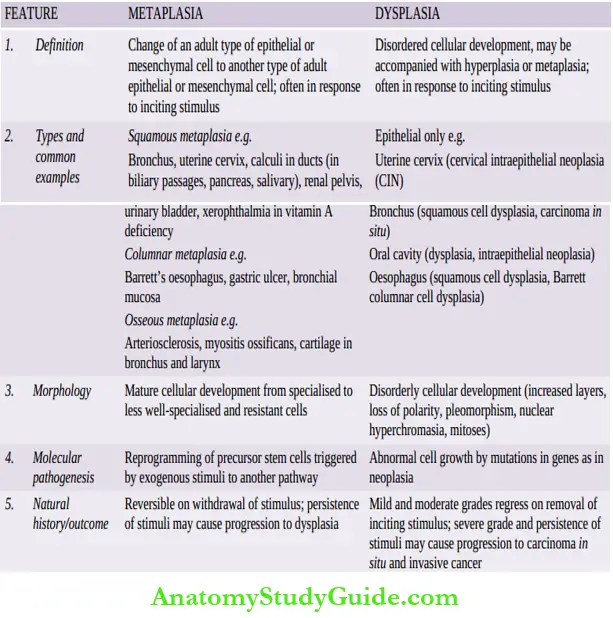
Current concept of dysplasia, newer terminologies and criteria for grading are further. The contrasting features of dysplasia and metaplasia are tabulated in
Difference between metaplasia and dysplasia:
Cellular Adaptations:
- These are adjustments which cells make in response to exogenous inciting stimuli. Atrophy is reduction of the number and size of parenchymal cells of an organ or its parts which was once normal.
- Hypertrophy is an increase in the size of parenchymal cells resulting in enlargement of the organ or tissue. It affects both dividing and non-dividing cells
- Hyperplasia is an increase in the number of parenchymal cells resulting in enlargement of the organ or tissue. It involves dividing cells only.
- Hypertrophy and hyperplasia may coexist for example, Uterus in pregnancy, lactating breast.
- Metaplasia is defined as a reversible change of one type of mature epithelial or mesenchymal cells to another type of mature epithelial or mesenchymal cells, usually in response to abnormal stimuli, and often reverts back to normal on removal of stimulus.
- Dysplasia is ‘disordered cellular development’, often preceded or accompanied with metaplasia and hyperplasia; most common sites being uterine cervix and bronchus.
- Mild and moderate grades may be reversible on withdrawal of inciting stimuli. Persistence of stimuli may cause progression to higher grades or to carcinoma in situ.
Leave a Reply