Cervicofacial Lymphadenopathy Essay Questions
Question 1. Outline the various causes of cervicofacial lymphadenopathy.
Answer:
Table of Contents
Cervicofacial lymphadenopathy Infection:
- Bacterial
- Streptococcus and Staphylococcus infection.
- Cat-scratch disease
- Tuberculosis
- Atypical mycobacterial infection
- Primary and secondary syphilis
- Diphtheria
- Leprosy
Read And Learn More: Oral Medicine and Radiology Question And Answers
- Viral
- Herpes simplex infection
- Herpes zoster infection
- Rubella
- Measles
- Infectious mononucleosis
- Adenovirus infection
- Acquired immune deficiency syndrome
- Fungal
- Rhinocerebral mucormycosis
- Histoplasmosis
- Parasitic
- Toxoplasmosis
- Leishmaniasis
Cervicofacial lymphadenopathy Immunologic Diseases:
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Sjogren’s syndrome
- Mikulicz’s disease
- Serum sickness
- Drug hypersensitivity
- Graft-versus-host disease
Cervicofacial lymphadenopathy Malignant Diseases:
- Leukemia
- Hodgkin’s lymphoma
- Non-Hodgkin’s lymphoma
- T-cell lymphoma
- Multiple myeloma
- Metastatic tumors of the head and neck
Cervicofacial lymphadenopathy Lipid Storage Disease:
- Gaucher’s disease
- Niemann-Pick disease
Cervicofacial lymphadenopathy Other Disorders:
- Castleman’s disease (giant lymph node hyperplasia)
- Sarcoidosis
- Lymphomatoid granulomatosis
- Kawasaki’s disease (mucocutaneous lymph node syndrome)
- Histiocytosis X
- Severe hypertriglyceridemia
Read And Learn More: Oral Medicine and Radiology Question And Answers
Cervicofacial lymphadenopathy Drugs:
- Allopurinol
- Atenolol
- Captopril
- Carbamazepine
- Gold
- Hydralazine
- Phenytoin
- Primidone
- Quinidine.
Question 2. Clinical evaluation of cervical lymphadenopathy.
Answer: The following features need to be checked:
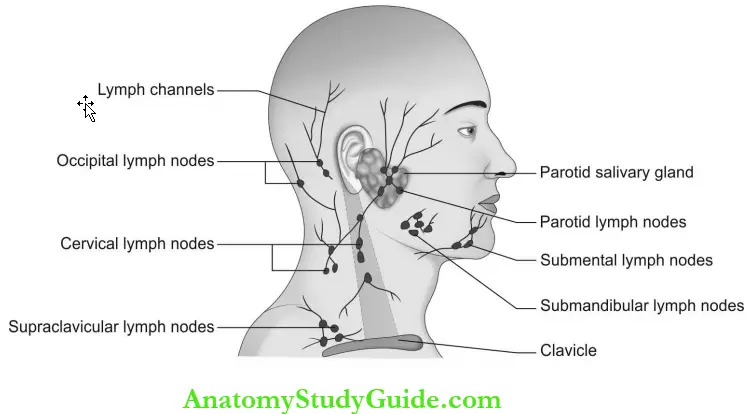
- Location: Anatomical site of involvement. (cervical, submandibular, submental, supraclavicular, occipital, preauricular, auricular, axial inguinal).
- A number of nodes—Single or multiple.
- Enlargement of nodes—Localized or generalized.
- Involvement—Unilateral or bilateral, if bilateral nodes are present, the symmetry should be checked.
- Consistency—Firm, soft, rubbery, rock hard, and bone hard.
- Nature—Movable or fixed.
- Size: <1 cm, or >1 cm
- Symptoms: Tenderness and associated systemic symptoms.
Cervical lymph-adenopathy Diagnosis:
- Complete blood count
- Lymph node biopsy and fine needle aspiration cytology
- Ultrasonography
- Computed tomography
- Magnetic resonance imaging
- Positron emission tomography.
Cervicofacial Lymphadenopathy Short Notes
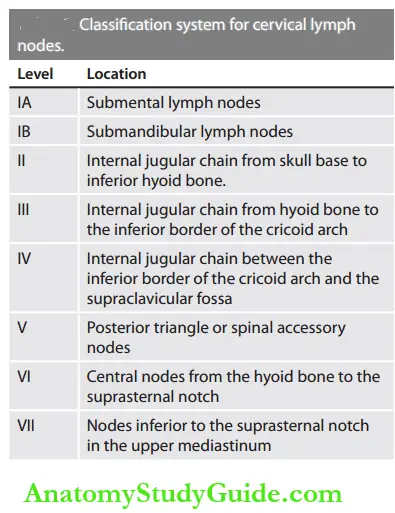
Question 1. Write a simplified numerical classification system for cervical lymph nodes.
Answer:
Question 2. Enumerate the conditions that cause generalized lymphadenopathy.
Answer:
- Generalized lymphadenopathy occurs in systemic conditions where the symptoms are widespread.
- AIDS-related complex due to severe immune deficiency by HIV infection results in unexplained, generalized lymphadenopathy.
- Disseminated carcinomatosis and lymphomas can cause generalized adenopathy.
- Inherited metabolic disorders (Gaucher disease) and endocrine disorders (Graves’ disease—hyperthyroidism, and Addison’s disease hypocortisolism).
- Immunological disorders like serum sickness and sarcoidosis also produce widespread adenopathy.
- Connective tissue disorders like rheumatoid arthritis and systemic lupus erythematosus also tend to cause generalized lymphadenopathy.
- Infectious diseases like tuberculosis, hepatitis, toxoplasmosis, and infectious mononucleosis lead to generalized lymph node enlargement.
Cervicofacial Lymphadenopathy Multiple Choice Questions
Question 1. A lymph node of <1cm size denotes
- Anatomical nodes
- Inflammatory response nodes
- Nonspecific reactive nodes
- Granulomatous disease
Answer: 3. Nonspecific reactive nodes
Question 2. A lymph node of >2 cm2 size is probably due to
- Malignancy
- Tuberculosis
- Parasite infection
- Reactive lesions
(Note: Lymph node of >2 cm2 size is probably due to malignant or granulomatous disorders).
Answer: 1. Malignancy
Question 3. Metastatic nodes are
- Soft and tender
- Tender and mobile
- Mobile and hard
- Hard and non-tender
Answer: 4. Hard and non-tender
Question 4. The approximate total number of lymph nodes in a body is 600.
- 300
- 1200
- 600
- 80
Answer: 3. 600
Question 5. The organ devoid of lymphatic supply is
- Brain
- Liver
- Kidney
- Limbs
(Note: Bone, cartilage, brain, spinal cord, and retina are the organs that do not have lymphatic vessels).
Answer: 1. Brain
Question 6. During development, the lymphatic system is the derivative of
- Endoderm
- Mesoderm
- Bone marrow
- Spleen
(Note: During development, the lymphatic system is the derivative of mesoderm but the adult progenitor cells are derived from bone marrow).
Answer: 2. Mesoderm
Question 7. Stone hard consistency of lymph nodes suggests
- Tuberculosis
- Lymphoma
- Metastasis
- Syphilis
Answer: 3. Metastasis
Question 8. Firm and rubbery nodes are characteristic for
- Tuberculosis
- Lymphoma
- Metastasis
- Syphilis
Answer: 2. Lymphoma
Question 9. Buckshot nodes are the cervical nodes in children with
- Primary complex
- Malnutrition
- Congenital syphilis
- Viral infection
Answer: 4. Viral infection
Question 10. The cartilage-like consistency of lymph nodes denotes
- Tuberculosis
- Lymphoma
- Metastasis
- Syphilis
Answer: 4. Syphilis
Question 11. Inflammatory lymph nodes are
- Soft and mobile
- Hard and mobile
- Soft and fixed
- Hard and fixed
Answer: 1. Soft and mobile
Question 12. A group of coalesced nodes that move as a single unit is denoted as
- Buckshot nodes
- Matted nodes
- Caseous nodes
- Granulomatous nodes
Answer: 2. Matted nodes
Question 13. Matted nodes are seen in
- Tuberculosis
- Syphilis
- Hodgkin’s disease
- Non-Hodgkin’s disease
(Note: Matted nodes are seen in tuberculosis, sarcoidosis, and lymphomas).
Answer: 1. Tuberculosis
Question 14. A positive mono spot test confirms
- Hodgkin’s lymphoma
- kaposi’s sarcoma
- Sarcoidosis
- Infectious mononucleosis
(Note: Monospot test is a positive heterophilic antibody test that confirms infectious mononucleosis).
Answer: 4. Infectious mononucleosis
Question 15. Localized lymphadenopathy with constitutional symptoms should be advised for biopsy when persisting more than
- 6 days
- 3-4 weeks
- 6 months
- 2-3 weeks
Answer: 2. 3-4 weeks
Question 16. In benign lymphadenopathy, the nodes are
- Freely mobile
- Fixed
- Nonpalpable
- Nonenlarged
Answer: 1. Freely mobile
Question 17. Left-side supraclavicular nodes are known as
- Virchow’s nodes
- Sentinel nodes
- Waldeyer’s ring
- Castleman’s nodes
Answer: 1. Virchow’s nodes
Question 18. Lymphadenopathy that indicates dangerous signs is
- Sacral lymphadenopathy
- Subclavian lymphadenopathy
- Supraclavicular lymphadenopathy
- Inguinal lymphadenopathy
(Note: Supraclavicular lymphadenopathy is an alarming sign for the clinician).
Answer: 3. Supraclavicular lymphadenopathy
Cervicofacial Lymphadenopathy Viva Voce
Question 1. What are Virchow’s nodes?
Answer:
- Left supraclavicular lymph nodes are called as Virchow’s nodes, by the name of a German pathologist “Rudolf Virchow, and enlargement of these nodes is called as Troisier’s sign.
- The enlargement of these nodes denotes malignant metastasis from distant organs like the stomach, esophagus, testis, and breasts; hence they are also called as signal nodes.
Question 2. What is lymph?
Answer: Lymph is an interstitial fluid composed of cellular fluids, extravasated leukocytes, extracellular substances, protein, and fat.
Question 3. What are the functions of the lymphatic system?
Answer: The lymphatic system delivers the lymphocytes and antigen-presenting cells to regional nodes and encounters the pathogens, maintaining the homeostasis of tissue fluid, and transport of cell debris and extracellular substances.
Cervicofacial Lymphadenopathy Highlights
- Lymphadenopathy is the term used to denote the enlargement of lymph nodes. It may be a primary or secondary manifestation of various disorders and may be a presenting sign or symptom of a patient’s illness. The involvement of nodes may be localized or generalized.
- Lymphadenitis is an acute infectious condition where lymph nodes are swollen, tender, soft, and isolated, while chronic infection gives firm, non-tender, and freely mobile nodes.
- Lymph nodes that are gradually enlarging, hard in consistency, and fixed to the underlying or adjacent tissues are malignant.
Soft, flat palpable submandibular nodes which are smaller than 1 cm size are normal in children. - This chapter highlights the reasons for cervicofacial lymphadinopathy and diagnostic clues for various diseases based on lymph node examination.
Leave a Reply