Drugs Acting On Cell Membrane
Question 6. Short note: Amphotericin B, azoles, pneumon.
Or
Classify antifungal drugs. Write the pharmacology of azoles.
Answer:
Polyene Antibiotics:
Amphotericin B: Obtained from Streptomyces nodosus is a polyene antibiotic containing many double bonds.

Read And Learn More: Pharmacology Question And Answers
Polyene Antibiotics Antifungal spectrum:
- A wide antifungal spectrum—Candida albicans, Histoplasma capsulatum, Cryptococcus neoformans, Coccidioides, Aspergillus and
- Blastomyces dermatitidis and leishmania. It is fungistatic at low and fungicidal at high concentrations.
Polyene Antibiotics Mechanism of action:
- Amphotericin B binds to ergosterol present in fungal cell membrane and forms pores in the cell membrane.
- Through these pores, cell contents leak out resulting in cell death.
- Because amphotericin has greater affinity for the fungal membrane sterol, i.e. ergosterol the main sterol in human cells, the action of amphotericin is selective for the fungi.
Polyene Antibiotics Pharmacokinetics:
- Amphotericin is not absorbed orally → Given IV, >90% bound to plasma proteins, widely distributed in the body and has a long t½ of 15 days. Dose: 0.5 mg/kg infusion.
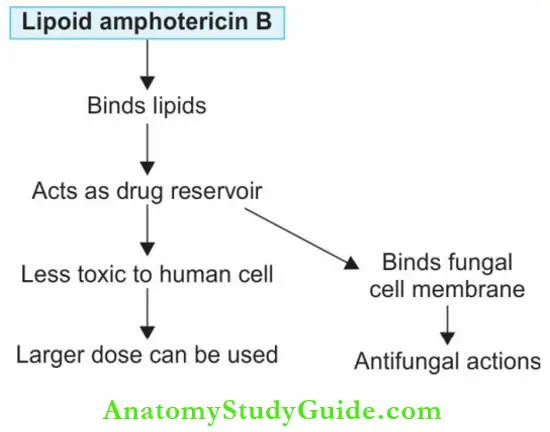
- Lipid formulation of amphotericin B is less likely to bind the human cell membrane and is thereby less toxic; used only in patients who do not respond to conventional preparations as it is expensive.
Polyene Antibiotics Adverse effects:
- Fever, chills, muscle spasms, vomiting, dyspnea, headache and hypotension can be seen on IV infusion. The fever and chills subside in about 30 minutes.
- Amphotericin should be injected slow IV, cautiously—to avoid arrhythmias; anaphylaxis is rare. Allergic reactions are less common with lipid formulation.
- Paracetamol (oral) + hydrocortisone (IV) before amphotericin avoid this.

Nephrotoxicity:
- Renal impairment with renal tubular acidosis and loss of potassium and magnesium are common. Infusion of normal saline before each dose of amphotericin can reduce these toxic effects. Prolonged use can cause irreversible nephrotoxicity.
- Use of other nephrotoxic drugs should be avoided. Anemia and bone marrow depression can also occur.
Neurotoxicity: Neurotoxicity and abnormal liver function tests have also been reported. Topical use can cause skin rashes.
Neurotoxicity Uses:
- Drug of choice for all life-threatening mycotic infections:
- Because it is fungicidal and has a broad antifungal spectrum—mucormycosis, invasive aspergillosis, cryptococcosis, sporotrichosis, trichosporanosis, blastomycosis, histoplasmosis, coccidioidomycosis, and paracoccidioidomycosis all respond.
- Candiasis: Useful in esophageal candidiasis. In cystitis due to Candida, amphotericin B is used to irrigate the bladder. Also used topically in candidiasis (3% lotion, cream, ointment).
- To prevent relapse of cryptococcosis and histoplasmosis in patients with AIDS.
- Given orally in fungal infections of the gut.
- Leishmaniasis: An alternative in kala-azar and mucocutaneous leishmaniasis.
Nystatin:
- Obtained from Streptomyces noursei is similar to amphotericin B. Because it is too toxic for systemic use, it is used topically candidal infections like oral thrush and vaginal candidiasis.
- 5 mL oral nystatin suspension should be swished in the mouth and then swallowed 4 times a day to treat the candida in the esophagus.
Hamycin: Hamycin is similar to nystatin—used topically for cutaneous candidiasis and otomycosis.
Azoles
Azoles are newer synthetic antifungals that are effective orally and are less toxic. Azoles include imidazoles and triazoles.

The triazoles have more selective effect on fungal sterol synthesis and are longer-acting than imidazoles. Ketoconazole, miconazole, and clotrimazole are the commonly used imidazoles out of them clotrimazole and miconazole are used only topically.
Azoles Antifungal spectrum:
- Broad-spectrum antifungal activity—inhibit dermatophytes, Blastomyces dermatitidis, Candida,
- Cryptococcus neoformans, H. capsulatum, coccidioides, some paracoccidioides and other deep mycoses.
Azoles Mechanism of action:
- Azoles inhibit the fungal enzyme lanosine 14α-demethylase which is required for conversion of lanosterol to ergosterol.
- Thus it results in ergosterol deficiency which causes weak fungal cell membrane and inhibits fungal replication.
- Azoles have higher affinity to fungal than human enzymes → selective activity.

Ketoconazole (KTZ)
- First oral azole to be available
- Well-absorbed from the gut
- Food and low gastric pH increase absorption
Ketoconazole Adverse reactions:
- Gastric irritation, nausea, vomiting, headache, allergic reactions, and hepatotoxicity.
- Higher doses → ↓ Synthesis of adrenal and gonadal steroids → Gynecomastia
- This steroid suppression effect of KTZ limits its use.
Ketoconazole Drug Interactions:
- Antacids, H2 blockers, and proton pump inhibitors reduce the bioavailability of KTZ because acidic medium is necessary for KTZ dissolution.
- Rifampicin and phenytoin induce KTZ metabolism and decrease its efficacy.
- Ketoconazole is microsomal enzyme inhibitor.

Ketoconazole Uses:
- Mucocutaneous candidiasis and dermatophytosis.
- Cushing’s syndrome.
- Cutaneous leishmaniasis.
- Deep mycoses but not preferred because of slow response, toxicity and long duration of treatment (6–12 months) required.
Drugs used in systemic fungal infections:

Fluconazole: Fluconazole A flourinated triazole is water-soluble, well absorbed from the gut, reaches all body fluids and attains good CSF concentration.
- Hence it is useful even in fungal meningitis.
- Fluconazole is eliminated by the kidneys, t½—25 hours, available for oral and IV use.
- Dose: 200–800 mg/day.
Fluconazole Adverse effects:
- Mild gastrointestinal disturbances, headache, and rashes.
- No effect on hepatic microsomal enzymes, drug interactions are less common.
Fluconazole Uses:
- Cryptococcal meningitis: Fluconazole given after initial treatment with amphotericin B. Fluconazole can also be used for prophylaxis.
- Coccidioidal meningitis: Drug of choice—higher doses (400–800 mg/day) used.
- Candidiasis: Oropharyngeal, esophageal and other mucocutaneous candidal infections for 2 weeks. Given IV to treat candidaemia in ICU patients.
- Other fungal infections: Useful in infections like tinea infections.
- Leishmaniasis (off label use): 200 mg/day for 6 weeks

Itraconazole:
- Most potent azole—given orally, its absorption is increased by food and gastric acid. It is a weak hepatic microsomal enzyme inhibitor, does not affect steroid synthesis → preferred over ketoconazole.
- Itraconazole is >99% bound to plasma proteins and does not reach the CSF. It has a t½ of 30–36 hours and is available both for oral and IV use.
- Dose: 100 mg BD with food.
A carrier molecule cyclodextrin has been used in new formulations of itraconazole.
Itraconazole Adverse effects:
- Include headache, dizziness, GI disturbances, allergic reactions, hepatitis and hypokalemia.
- Avoid in pregnant women
Ketoconazole And Fluconazole:

Itraconazole Uses:
- Drug of choice in most systemic mycoses (without meningitis)—given IV in severe infections.
- Itraconazole oral solution is used in oropharyngeal and esophageal candidiasis—10 mL (100 mg) to be swished vigorously in the mouth before swallowing on an empty stomach—twice a day for 2–4 weeks.
- Can be used in onychomycosis, candidiasis and dermatophytoses.
Voriconazole
- Wider spectrum and better efficacy than fluconazole.
- Microsomal enzyme inhibitor (inhibits CYP3A4) → drug interactions can occur.
Voriconazole Adverse effects:
- Skin rashes, visual disturbances, hepatotoxicity, and QTc prolongation.
- IV formulation can rarely cause anaphylaxis.
- It is contraindicated in pregnancy.
Voriconazole Uses:
- Drug of choice in invasive aspergillosis (has better efficacy and less toxicity than amphotericin B).
- Voriconazole can also be used in esophageal candidiasis.
Posaconazole:
- Posaconazole is similar to itraconazole but with the broadest spectrum of antifungal activity among azoles including zygomycosis and mucormycosis.
- It is available as a liquid only for oral use. Fatty food increases absorption and attains high levels in the tissues.
Posaconazole Uses:
- Refractory invasive aspergillosis, chromoblastomycosis, fusariosis, and coccidioidomycosis.
- Prophylaxis of fungal infection in immunosuppressed patients.
- Ravuconazole and isavuconazole are newer triazoles with longer action and broader spectrum.
Topical Azoles
Clotrimazole, miconazole and econazole:
- These are poorly absorbed from the skin (<1%).
- Absorption from the vaginal mucous membrane is not significant—used topically in dermatophytic infections (ringworm) and mucocutaneous candidiasis.
- Miconazole penetrates the cutaneous layer—stratum corneum and remains at this site for 3–4 days. It has better efficacy.
Clotrimazole troche is available for oral thrush:
- They can cause mild irritation at the site of application—particularly on mucous membranes. Skin preparations can rarely cause rashes, oedema and pruritus.
- Econazole cream may also cause burning or stinging sensation.
Drugs used in superficial mycosis:

Fenticonazole, terconazole, tioconazole, butaconazole, oxiconazole, sulconazole and sertaconazole all azoles available for topical use as creams and lotions for use in dermatophytoses and mucocutaneous candidiasis.
Allylamines:
Terbinafine: A synthetic antifungal that is effective against dermatophytes and candida:
- It gets concentrated in the keratin-like griseofulvin. Terbinafine inhibits an enzyme (squalene epoxidase) needed for the biosynthesis of ergosterol by fungi and is fungicidal.
- Well absorbed, orally effective undergoes extensive first-pass metabolism and >99% bound to plasma proteins. On attaining a steady state, the t½ increases to 200–400 hours.
Allylamines Adverse effects:
Are rare—gastrointestinal disturbances, rashes, and headaches can occur.
Allylamines Uses:
- Dermatophytosis, pityriasis, onychomycosis, and candidiasis—are particularly preferred in onychomycosis.
- Dose: 250 mg OD for 3 months—superior to azoles and griseofulvin.
Drugs Acting On Cell Wall
Echinocandins or pneumocandins:
- Caspofungin, micafungin, and anidulafungin—the echinocandins are a newly introduced group of fungicidal drugs that are effective against candidiasis and Aspergillus species including those resistant to azoles.
- Caspofungin also has activity against Pneumocystis jiroveci infections.
- Echinocandins inhibit the formation of the fungal cell wall. They inhibit the synthesis of an important component of the fungal cell wall—a glucose polymer β-glucan as a result of which the fungal cell lysis occurs.
- Echinocandins are given IV—not absorbed on oral use, anidulafungin is long-acting with t½ 24–48 hours.

Echinocandins Adverse effects:
Minor and echinocandins are well-tolerated—can cause histamine release on rapid infusion and thrombophlebitis.
Echinocandins Uses:
- Candida infections: For treatment and antifungal prophylaxis in febrile neutropenia.
- Invasive aspergillosis: In patients who have not responded to amphotericin.
Drugs Acting On Nucleus
Griseofulvin:
- Griseofulvin is a fungistatic derived from Penicillium griseofulvum.
- It is the antifungal given orally in superficial dermatophytosis (caused by Trichophyton, Microsporum, and Epidermophyton).
Griseofulvin Mechanism of action:
Griseofulvin binds to microtubular protein in the nucleus, disrupts the mitotic spindle, and inhibits mitosis in the fungus.
Griseofulvin Pharmacokinetics:
- Griseofulvin is poorly water-soluble with poor bioavailability.
- Absorption can be enhanced by using microfine drug particles and by giving it fatty food.

Griseofulvin Adverse effects: Include allergic reactions, hepatitis, and neurotoxicity.
Griseofulvin Drug Interactions:
- Phenobarbitone → ↓ Absorption of griseofulvin → Therapeutic failure
- Griseofulvin → Microsomal enzyme induction → ↑ Warfarin metabolism
- Griseofulvin + alcohol → Disulfiram-like reaction → Intolerance to alcohol
Griseofulvin Uses:
- Superficial dermatophytosis given orally it gets concentrated in the tinea-infected cells and therefore, suitable for ringworm infection of skin and nail.
- Dose: 1 g daily. It is preferred when a larger area is involved and topical antifungals are not suitable. Duration of treatment —3 weeks–1 year.
- Nail infections require 6–12 months treatment.
Flucytosine:
- Flucytosine is a fluorinated pyrimidine effective against Cryptococcus neoformans and some strains of Candida.
- It is a prodrug taken up by the fungal cells and converted to 5-fluorouracil which inhibits DNA synthesis.
- Because the drug cannot be converted by human cells to active metabolites, flucytosine is toxic only to the fungal cells.
- Flucytosine has synergistic activity with amphotericin B and azole antifungals. It is well absorbed, reaches all body fluids including CSF, and is excreted by the kidneys.
- Bone marrow depression and gastrointestinal disturbances are the most common adverse effects.
Amphotericin damages fungal cell membrane → ↑ Flucytosine penetration → Synergistic combination
Flucytosine Uses:
- Flucytosine is used with amphotericin B in cryptococcal meningitis and systemic candidiasis because:
- It is synergistic with amphotericin
- Used alone, resistance develops rapidly
- Flucytosine is also used with itraconazole in chromoblastomycosis.
Other Topical Antifungal Agents
Apart from nystatin, clotrimazole, miconazole, and terbinafine, some drugs like salicylic acid, benzoic acid, tolnaftate, naftifine, haloprogine, and ciclopirox olamine are used topically for dermatophytosis and pityriasis versicolor.
Ciclopirox olamine:
- Ciclopirox olamine is effective against Candida, dermatophytes, and Malassezia furfur.
- When applied to the skin (cream, lotion) it does not get absorbed systemically but penetrates the skin to reach the dermis, and no adverse effects are reported.
Selenium sulfide:
- It is useful in tinea versicolor caused by Malassezia furfur, and also in dandruff. It is an irritant to the eyes and the odor is unpleasant.
- Selsun 2.5% suspension of selenium sulfide in a shampoo base.
Newer Drugs
Nikkomycins:
Nikkomycins are a class of antifungals that inhibit chitin synthesis which is another important component of fungal cell wall and is under development.
Sordarins:
Sordarins selectively inhibit fungal protein synthesis and have shown good activity against a variety of Candida species, some filamentous fungi and also against Pneumocystis jiroveci.
Antiviral Drugs
- Viruses are intracellular parasites and depend on the host cells for their food, growth and multiplication.
- The virus attaches itself to the host cell membrane and penetrates it (entry), DNA/RNA is released in the host cell (uncoating) where it is duplicated.
- The viral components are assembled (assembly) and the mature viral particle is then released from the host cell (budding and release).
- Chemotherapy can interfere with any of these steps. Drugs that interfere with viral replication may also interfere with host cell function causing toxicity.

Antiviral Drugs Classification:
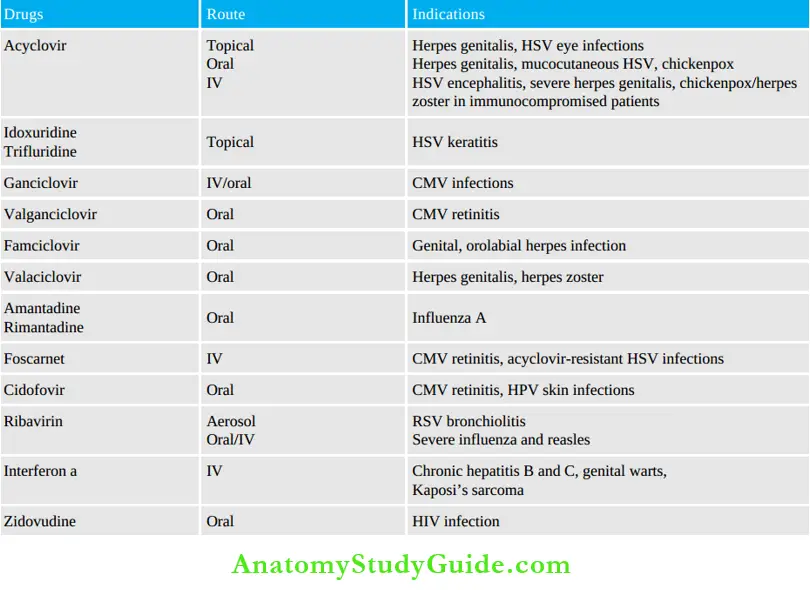
- Antiherpes drugs: Acyclovir, ganciclovir, famciclovir, penciclovir, valaciclovir, idoxuridine, trifluridine, foscarnet, fomivirsen, cidofovir
- Anti-CMV drugs: Ganciclovir, valganciclovir, foscarnet, cidofovir
- Anti-influenza drugs: Amantadine, rimantadine, oseltamivir, zanamivir
- Antihepatitis agents:
- Antihepatitis B agents: Adefovir, entecavir, interferons, telbivudine, lamivudine, tenofovir
- Antihepatitis C agents: Ribavirin, interferons, sofosbuvir, protease inhibitors—boceprevir, simeprevir, telaprevir.
- Antirhinovirus/antienterovirus agent: Pleconaril
- Antiretroviral drugs:
- Nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs): Zidovudine, didanosine, stavudine, emtricitabine, zalcitabine, lamivudine, abacavir, tenofovir
- Non-nucleoside reverse transcriptase inhibitors (NNRTIs): Nevirapine, efavirenz, delavirdine, etravirine, rilpivirine.
- Protease inhibitors (PIs): Saquinavir, indinavir, ritonavir, nelfinavir, amprenavir, lopinavir, atazanavir, darunavir, fosamprenavir, tipranavir
- Entry inhibitors: Enfuvirtide, maraviroc
- Integrase strand transfer inhibitors (INSTIs): Raltegravir, elvitegravir, dolutegravir.
Antiherpes Virus Agents
Acyclovir: Acyclovir is effective against herpes simplex virus (HSV) type 1 and type 2, varicella zoster virus (VZV) and Epstein-Barr virus (EBV).
Acyclovir Mechanism of action:
- Acyclovir is taken up by the virus-infected cell, and converted to acyclovir triphosphate (by viral kinase) and this inhibits viral DNA synthesis by inhibiting viral
- DNA polymerases and causing DNA chain termination.
Acyclovir Pharmacokinetics:
- Acyclovir has poor bioavailability (15–20%); widely distributed—attains good concentration in the CSF and aqueous humor.
- It is eliminated by the kidneys and the t½ is prolonged in renal failure.
Acyclovir Adverse effects:
- Acyclovir is well-tolerated; nausea, diarrhea, headache, and rashes may occur occasionally. Topical acyclovir can cause burning and irritation.
- Given IV, it may cause renal and neurotoxicity but are uncommon.

Acyclovir Uses:
1. HSV infections: Infection with HSV-1 causes diseases of the mouth, face, skin, esophagus, or brain. HSV-2 usually causes infections of the genitals, rectum, skin, hands or meninges.
- Primary and recurrent genital and labial herpes: Acyclovir (400 mg TDS for 10 days).
- In mild cases, topical acyclovir (5% ointment) can be tried. In recurring genital herpes, parenteral acyclovir is needed—IV 5 mg/kg every 8 hours for 10 days.
- For long-term suppression, oral acyclovir is given for (400 mg BD) 1 year.
- HSV encephalitis: HSV encephalitis and other severe HSV infections—IV acyclovir
- HSV keratoconjunctivitis: Acyclovir eye drops (3–5%).
2. Herpes zoster: Acyclovir shortens the duration of illness.
3. Chickenpox: In adults and in immunodeficient patients (15 mg/kg/day IV for 7 days), acyclovir reduces the duration and severity of illness. In children, routine use is not recommended. In close contact, acyclovir (400 mg QID for 7 days) given during the incubation period may prevent chickenpox.
The congeners valacyclavir, penciclovir, and famciclavir are converted to their triphosphate derivatives which inhibit viral DNA/RNA polymerases and inhibit viral replication.
Drugs Used In Cytomegalovirus Infections
Ganciclovir and Valganciclovir:
- Ganciclovir is a guanosine analog and valganciclovir is the prodrug of ganciclovir and is orally effective.
- The active drug remains in the cytomegalovirus (CMV) infected cells for a longer time and inhibits viral synthesis.
- Toxicity includes myelosuppression and gonadal toxicity.
Indications of some antiviral drugs:
Ganciclovir and Valganciclovir Uses:
- Intravenous ganciclovir and oral valganciclovir are used in the treatment and chronic suppression of CMV retinitis in immunocompromised patients.
- To prevent CMV disease in organ transplant patients.
- Topical ganciclovir may be used for herpetic keratitis.
Foscarnet:
Foscarnet directly inhibits viral DNA and RNA polymerase, CMV colitis, and esophagitis, as well as acyclovir-resistant herpes infections.
Foscarnet Adverse effects:
Foscarnet chelates divalent cations resulting in hypocalcemia, hypokalemia and hypomagnesemia.
Anti-Influenza Virus Agents
Question. Short note:
- Drugs used in influenza
- Amantadine
- Drugs used in the treatment of H1N1.
Answer:
Amantadine and rimantadine:
- Inhibit the replication of influenza A viruses. Given orally, both of them are well absorbed and attain good concentrations in the nasal secretions and CSF.
- They are generally well-tolerated; nausea, vomiting, diarrhea, anorexia, dizziness, insomnia, difficulty in concentrating, and ankle edema are reported, but are seen with only higher doses.
- Both are teratogenic. Rimantadine is longer-acting and has fewer adverse effects.

Amantadine and rimantadine Uses:
- Treatment of influenza A: Started at the onset of symptoms—reduce the fever, duration, and severity of influenza by 1–2 days. 200 mg/day OD for 5 days of amantadine/rimantadine.
- Prophylaxis of influenza A: During an epidemic especially in high-risk patients.
- Parkinsonism: Amantadine increases the release of dopamine and is useful in Parkinsonism.

Oseltamivir and zanamivir:
- Inhibit viral replication by inhibiting the neuraminidase activity which is essential for the release of daughter virions.
- Oseltamivir and zanamivir are effective against both influenza A and influenza B. These drugs should be administered within a few hours after the onset of symptoms (in 36–48 hours). They reduce both the duration and severity of illness.
- Oseltamivir is well-tolerated—can cause nausea, vomiting, headache, diarrhea and abdominal discomfort. It should not be given in children <1 year of age. Zanamivir is given by inhalation which can rarely cause respiratory distress.
Oseltamivir Uses:
- Prevention and treatment of influenza including H1N1.
- Dose: Oseltamivir 75 mg BD for 5 days. Zanamivir 10 mg inhalation twice daily for 5 days.
Ribavirin:
- Has broad-spectrum antiviral activity. Its active metabolite ribavirin triphosphate is effective against many DNA and RNA viruses including influenza A and B, respiratory syncytial virus (RSV), HCV and HIV. It is used as an aerosol in RSV bronchiolitis in children.
- Ribavirin is also used in severe influenza and measles in immunocompromised patients and in HCV. Adverse effects include hemolytic anemia, fatigue, nausea and allergic reactions. Dose: 200 mg QID.
Antihepatitis Drugs
Antihepatitis Drugs Include:
Antihepatitis B Agents
Question 7. Short note: Interferons.
Answer:
Adefovir:
- Adefoviris phosphorylated by viral kinase to adefovir diphosphate which inhibits viral DNA polymerase.
- It is incorporated into viral DNA and causes DNA chain termination.
- Adefovir is well-tolerated—can cause headache, diarrhea, weakness and abdominal pain.
- Nephrotoxicity has been reported. It is used orally (10 mg OD) in chronic HBV infection and is particularly useful in lamivudine-resistant HBV patients.
Entecavir:
- Entecavir is a guanosine nucleoside analog that inhibits DNA polymerase.
- It is completely absorbed on oral administration but should be given on an empty stomach. It is well-tolerated.
- Entecavir is useful in chronic HBV infection.
Interferons (IFN):
- Interferons are cytokines produced by host cells in response to viral infections. They also have immunomodulating and antiproliferative properties.
- There are three types—α, β, and γ interferons in man. They inhibit the multiplication of many DNA and RNA viruses. Interferons are given parenterally (SC/IM).
Interferons Mechanism of action:
- Interferons bind to specific receptors and thereby stimulate the synthesis of certain proteins which inhibit viral protein synthesis.
- Interferon α acts on multiple stages of viral replication including inhibition of viral penetration, protein synthesis, maturation and release.

Interferons Adverse effects:
- Flu-like syndrome starts in about 6 hours but may resolve in 12–24 hours.
- Pretreatment with antipyretics reduces the febrile response.
- Other adverse effects including myelosuppression, hypotension, arrhythmias, depression, transient elevation of enzymes, hepatotoxicity, weight loss, alopecia, pneumonitis, ototoxicity, retinopathy, thyroiditis, headache, and arthralgia are reported on long-term use. They can also cause neurotoxicity resulting in confusion, sedation, and rarely seizures.
Interferons Uses:
- Chronic hepatitis B: Interferons administered for 4–6 months for an overall improvement.
- Chronic hepatitis C infection: Interferons + ribavirin → response is better and longer lasting.
- Kaposi’s sarcoma in AIDS patients.
- Genital warts caused by papilloma—interferons are injected into the lesion.
- Some leukemias and lymphomas, mutiple myeloma, and CML
- Multiple sclerosis: Interferon β reduces severity.
- Rhinovirus cold: Interferon α is given intranasally for prophylaxis.
Lamivudine:
- Remains in HBV-infected cells for long periods and is well-tolerated.
- It may also be useful in the prevention of vertical transmission from mother to fetus.
Telbivudine:
Telbivudine inhibits DNA polymerase in the hepatitis B virus and tenofovir has activity against lamivudine-resistant strains of chronic hepatitis.
Antihepatitis C Agents
- Hepatitis C can vary in severity from mild infection of few weeks to serious lifelong disease.
- Hepatitis C-related liver diseases include cirrhosis and liver cancer.
Drugs used to treat HCV infection include:
- Interferons
- Ribavirin
- Sofosbuvir
- Protease inhibitors—boceprevir, simeprevir, and telaprevir.
HCV is treated with a combination of interferon-alpha and ribavirin or newer drugs.
Sofosbuvir:
Inhibits RNA-dependent RNA polymerase. Sofosbuvir is used in combination with interferon and ribavirin to attain high cure rates. It is given orally and is well-tolerated; fatigue and headache are reported.
Protease inhibitors:
Boceprevir, simeprevir, and telaprevir inhibit HCV protease and are used in combination with IFNs and ribavirin.
Antiretroviral Drug
Pleconaril:
Pleconaril binds to viral capsid and prevents attachment and/or viral uncoating. It is found to be effective in rhinovirus and enterovirus and is indicated in enteroviral meningitis and rhinoviral cold.
Antiretroviral Agents
Acquired immunodeficiency syndrome (AIDS) results from infection with the human immunodeficiency virus (HIV)—a retrovirus. Two types of HIV have been identified as HIV-1 and HIV-2.
Drugs used in the treatment of AIDS are of five groups:
- Nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs)
- Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
- Protease inhibitors (PIs)
- Entry inhibitors (including fusion inhibitors and CCR5 receptor antagonists)
- Integrase strand transfer inhibitors (INSTIs).
HIV has a high mutation rate and, therefore, easily develops resistance to the drugs. National
AIDS Control Organisation (NACO) is working towards controlling the spread of AIDS in India.

Nucleoside And Nucleotide Reverse Transcriptase Inhibitors (NRTIs)
Zidovudine didanosine, stavudine, zalcitabine, lamivudine, emtricitabine, abacavir, tenofovir.
NRTIs Mechanism of action:
- NRT inhibitors enter the cells and are converted to their corresponding triphosphate derivatives.
- These have a high affinity for reverse transcriptase, an enzyme required for DNA synthesis in HIV.
- The NRT inhibitors are nucleoside analogs. They competitively inhibit reverse transcriptase, are taken up into viral DNA chain, and terminate DNA chain elongation. Thus inhibiting viral replication.
 .
.
NRTIs Pharmacokinetics:
The NRT inhibitors are well absorbed when given orally, t½ varies from 1–4 hours. Stavudine attains good CSF levels. Most NRT inhibitors are excreted by the kidneys.
Common adverse effects to NRTIs include:
- Bone marrow suppresion with anemia, granulocytopenia, myopathy, peripheral neuropathy and pancreatitis.
- Lactic acidosis and hepatic steatosis are rare but can be fatal. Toxicity is due to inhibition of DNA polymerase in human cells to a small extent .
Adverse effects of nucleoside reverse transcip:

Zidovudine (Azidothymidine, AZT):
Zidovudine is a thymidine analog, active against HIV infections and other retroviruses.
Zidovudine Adverse effects:
- Bone marrow suppression is the most prominent adverse effect of zidovudine. Anemia can be treated with erythropoietin, while neutropenia needs G-CSF or GMCSF.
- Headache, nausea, anorexia, myalgia, fatigue, and insomnia can occur. High doses cause myopathy, dyslipidemia, and neurotoxicity.
Zidovudine Uses:
- All are used in combination.
- AZT is a component of the anti-HIV regimen—also used for post-exposure prophylaxis.
- Lamivudine apart from HIV is also effective against hepatitis B virus.
Emtricitabine: Emtricitabine has the advantages of good bioavailability (93%) and long intracellular, t½ of >24 hours—once a day administration.
Tenofovir:
Tenofovir used in HIV infections in combination with other drugs.
Abacavir:
Abacavir advantages are good oral bioavailability and slow development of resistance. Drug interaction with alcohol should be noted.
Drug Interactions of NRT Inhibitors:
- Avoid other myelosuppressants
- Avoid AZT + stavudine → they compete for activation
- Avoid zalcitabine + didanosine → overlapping toxicity
- Avoid zalcitabine + lamivudine → antagonise each others action
- Avoid alcohol with abacavir → both metabolized by alcohol dehydrogenase → compete for matabolism
- Avoid AZT + paracetamol → compete for metabolism → toxicity

Non-Nucleoside Reverse Transcriptase Inhibitors:
The NNRT inhibitors are nevirapine, delavirdine, efavirenz and etravirine.
NNRT Mechanism of action:
NNRT inhibitors bind to reverse transcriptase and inactivate the enzyme.
NNRTIs Adverse effects:
- NNRTIs can cause GI disturbances, headache,s, and allergic reactions. These drugs are metabolized by cytochrome P450 enzymes and can result in related drug interactions.
- Nevirapine attains high levels in CSF and has a long t½. Fatty food increases absorption and also toxicity—hence, it should be taken on empty stomach. Allergic reactions ranging from skin rashes, pruritus to Stevens-Johnson syndrome and toxic epidermal necrolysis can occur.
- It should be started with a low dose and gradually increased. If allergic reactions are severe, nevirapine should be withdrawn. Occasionally, fulminant hepatitis can occur.
Uses of NNRTIs:
- Nevirapine: Nevirapine treatment of HIV-1 infections with other drugs and to prevent vertical transmission from the mother to the newborn.
- Delavirdine: HIV-1 infection with other antiretroviral drugs.
- Efavirenz: Efavirenz is long-acting—given once daily in HIV-1 infection.
- Etravirine and rilpivirine are effective in HIV-1 that is resistant to other NNRTIs.
Drug Interactions Of Nnrt Inhibitors:
NNRT inhibitors induce or inhibit some microsomal enzymes resulting in drug interactions leading to therapeutic failure or toxicity of some drugs given with them.
Protease Inhibitors
Question 8. Short note: Protease inhibitors.
Answer:
Saquinavir/ritonavir, indinavir nelfinavir, amprenavir, lopinavir, atazanavir, and darunavir are protease inhibitors.
Protease inhibitors Mechanism of action:
- HIV protease activity is essential for the activation of viral enzymes, maturation and HIV replication.
- It is needed for the production of mature virions and for viral infectivity.
- The protease inhibitors bind competitively to HIV protease and block viral maturation.

Protease Inhibitors Pharmacokinetics:
- Protease inhibitors are well absorbed except saquinavir.
- All PIs are extensively bound to plasma proteins and metabolized by hepatic microsomal enzymes (cytochrome P450)—also microsomal enzyme inhibitors → hence many drug interactions possible.
Protease inhibitors Adverse effects:
Gastrointestinal disturbances, allergic reactions, paraesthesias, and some of them can increase serum lipids.
Protease inhibitors Uses:
- PIs are used with other antiretroviral drugs in the treatment of HIV infections.
- Ritonavir inhibits microsomal enzymes and thereby prolongs the plasma half-life of other protease inhibitors
- . This beneficial drug interaction permits use of lower doses of other PIs with ritonavir and is used to boost their drug levels.
Entry Inhibitors
Fusion Inhibitor:
Question 9. Short note: Entry inhibitors.
Answer:
Enfuvirtide:
- Enfuvirtide binds to a glycoprotein on the virus → inhibits the binding of the virus to the host cell membrane, and thereby blocks the entry of the virus into human cells (fusion inhibitor) → thus preventing transmission of HIV.
- Metabolism is by hydrolysis and NOT by microsomal enzymes.
- It can cause local injection site reactions (common), pneumonia, and lymphadenopathy.
- Enfuvirtide requires parenteral (SC) administration—therefore, used only as an add-on drug in patients not responding to other antiretroviral drugs in HIV-1 infected patients.
CCR5 Receptor Antagonist:
Maraviroc:
- CCR5 is a coreceptor involved in fusion and entry of the virus into the CD4 cells.
- Maraviroc blocks entry of HIV. It is effective orally, metabolized by hepatic microsomal enzymes CYP3A4 and excreted through the gut.
- Microsomal enzyme inducers and inhibitors can alter the plasma levels of maraviroc.
- It can cause diarrhea, sleep disturbances, cough, myalgia, arthralgia, respiratory infections, and raised liver enzymes.
- Maraviroc is indicated in HIV-1 infection not responding to other drugs.

Integrase Strand Transfer Inhibitors (Instis)
Raltegravir, elvitegravir, dolutegravir:
- Integrase is a viral enzyme necessary for viral replication in both HIV-1 and HIV-2 viruses. Raltegravir, elvitegravir, and dolutegravir bind to integrase and prevent the integration of HIV DNA into the chromosomes of host cells.
- Raltegravir is not metabolized by CYP450 system. It can cause nausea, diarrhea, headache and dizziness.
Treatment Of Hiv Infection
- With appropriate medication, it is possible to control the disease and prolong the life to a large extent.
- Combination of drugs is used to improve efficacy, delay the development of resistance and to improve compliance.
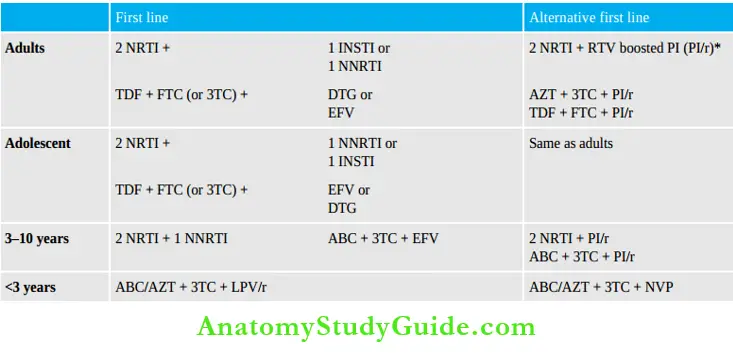
- Two NRTIs form the backbone drugs and a third drug added may be an INSTI or efavirenz and these form the first-line drugs. If first-line therapy fails, alternative first-line drugs are given.
First-line antiretroviral drug regimen updated WHO guidelines 2016:
Cobicistat:
- Cobicistat is a microsomal enzyme inhibitor—it inhibits cytochrome P450 enzymes like CYP 3A4 and thereby increases the plasma levels of drugs metabolized by these enzymes.
- It also inhibits intestinal transport protein resulting in better absorption of drugs like atazanavir and darunavir.
- Cobicistat is used in anti-HIV combination regimens to enhance the plasma levels of drugs like elvitegravir, atazanavir, darunavir, and tenofovir alafenamide.
- However creatinine levels should be monitored as cobicistat increases renal secretion of creatinine.
Postexposure prophylaxis (PEP):
- Accidental exposure to potential blood-borne infections including HIV, HBV, and HCV among healthcare workers including doctors needs immediate attention.
- Postexposure prophylaxis should be initiated at the earliest possible.
- The risk assessment is done based on the severity of the source of infection. Counseling, risk assessment, first aid, and short-term (4 weeks) antiretroviral drugs with appropriate follow-up would help to prevent the disease.
- The first dose of PEP should be given at the earliest, preferably within 2 hours but at least before 72 hours and the complete course is 28 days.
PEP regimen:
Three-drug regimen (WHO recommendation) WHO and other guidelines recommend a three-drug regimen.
- For children <10 years:
- Zidovudine (AZT) and lamivudine (3TC) are backbone drugs.
- Ritonavir boosted lopinavir (LPVr) or atazanavir (ATV/r) is the third drug.
Postexposure prophylaxis WHO guidelines updated 2016:

Chemotherapy Of Malaria
Malaria was so named because it was thought to be due to bad air (‘mala’–bad ‘aria’–air inItalian).
- Malaria caused by protozoa of the genus Plasmodium is most commonly transmitted through the bite of a female Anopheles mosquito, though malaria can also be transmitted by blood transfusion and vertically from the mother to the fetus across the placenta.
- It is a major public health problem in most of the developing countries including India.
- There are primarily 5 species of the malarial parasite—P. faciparum, P. vivax, P. ovale, P. malariae and P. knowlesi. P. falciparum causes the most severe form of malaria (malignant tertian) which can be fatal.
- Infected erythrocytes clog or block the capillaries of various tissues resulting in anoxia. Cerebral anoxia can lead to death.
- P vivax and P. ovale malaria can relapse because of the hypnozoites (sleeping forms) in their life cycle. Stages in the life cycle of the malaria parasite.
Malaria Clinical features:
- Signs and symptoms of malaria include fever with chills, myalgia, arthralgia, headache, vomiting, and fatigue—these symptoms mimic viral fever and by the time it is diagnosed it could be a more severe form.
- Diarrhea, abdominal pain, dizziness, hypotension and convulsions may occur. Mild anemia and splenomegaly and in some of them mild hepatomegaly are the expected findings.

Therapeutic Classification:
- Causal prophylactics:
- Causal prophylactics (primary tissue schizonticides—destroy parasites in liver cells and prevent invasion of erythrocytes)
- Chloroquine, amodiaquine Primaquine, pyrimethamine Chloroquine, quinine, artemisinins, mefloquine, halofantrine, pyrimethamine, atovaquone, chloroguanide Primaquine, tafenoquine.
- Blood schizonticides:
- Blood schizonticides (suppressive) destroy parasites in RBCs and terminate clinical attacks
- Blood schizonticides + hypnozoitocidal drugs
- Tissue schizonticides: Tissue schizonticides used to prevent relapse (hypnozoitocidal drugs destroy hypnozoites of P. vivax and P. ovale that cause relapses)
- Radical curatives (eradicate all forms of P. vivax and P. ovale that cause relapses)
- Gametocidal drugs: Gametocidal drugs (destroy gametocytes, prevent transmission)
Chemical Classification:
- 4-aminoquinolines: Chloroquine, amodiaquine,Primaquine ,Quinine
- 8-aminoquinolines: Primaquine, bulaquine, tafenoquine
- Quinoline methanols: Quinine, quinidine, mefloquine
- Sesquiterpene lactones/artemisinins: Artemisinin, artesunate, artemether, arteether
- Folate antagonists: Proguanil, sulfadoxine, pyrimethamine
- Phenanthrene methanol: Halofantrine, lumefantrine
- Naphthaquinone: Atovaquone
- Antibiotics: Tetracycline, doxycycline, ciprofloxacin, clindamycin, azithromycin
Chloroquine
Chloroquine (CQ) a synthetic 4-aminoquinoline is primary drug in the treatment and prevention of malaria since 1940.
Antimalarial actions:
Chloroquine is a highly effective blood schizonticide with activity against all 5 species of the plasmodia. It completely cures sensitive falciparum malaria. It is rapidlyacting—patients become afebrile in 24–48 hours. Chloroquine also destroys gametocytes of P. vivax, P. ovale, and P. malaria, but has no effect on the hypnozoites in the liver. Chloroquine is safe in pregnancy.
Chloroquine Mechanism of Action:
Chloroquine is specifically taken up by the parasite in the erythrocytes by a specific uptake mechanism. Because chloroquine is a base, it concentrates in the acidic food vacuoles of the parasite. In the malaria parasite, the enzyme heme polymerase detoxifies heme to hemazoin.


Chloroquine inhibits heme polymerase leading to the death of the parasite.
Chloroquine Other Actions:
- Chloroquine has activity against Giardia lamblia and Entamoeba histolytica.
- Attains high concentration in the liver → useful in hepatic amoebiasis.
- Has local anesthetic properties.
- Has anti-inflammatory properties → used in rheumatoid arthritis as a disease-modifying antirheumatic drug.
Chloroquine Pharmacokinetics: Chloroquine may be given both orally and parenterally.

Chloroquine Adverse Effects:
- Nausea and vomiting may be quite severe in some patients—an antiemetic 30 minutes before chloroquine is generally given.
- Anorexia, pruritus, headache, dizziness, visual disturbances, insomnia and skin rashes.
- IV chloroquine may cause hypotension, widening of QRS complex, arrhythmias, respiratory and cardiac arrest— hence parenteral chloroquine should be avoided.
- High doses → cardiomyopathy, peripheral neuropathy, ototoxicity, convulsions and psychiatric disturbances.
- Long-term use can cause blurring of vision, confusion, bleaching of hair, myopathy and rarely blood dyscrasias.
- Prolonged treatment with high doses can cause irreversible retinopathy—as chloroquine accumulates in retina and can result in blindness. Corneal deposits are also known but are reversible.
Chloroquine Uses:
- Malaria:
- Chloroquine is highly effective in the treatment of malaria due to sensitive strains of all 5 species. WHO chloroquine regimen—1 g (600 mg base) at 0, 24 hours and 0.5 g at 48 hours. It is also used for prophylaxis—300 mg base per week.
- Extraintestinal amoebiasis—alternative to metronidazole
- Rheumatoid arthritis
- Infectious mononucleosis
- Rationale → Anti-inflammatory
- Discoid lupus erythematosus
- Photogenic reactions activity.
- Lepra reactions
- Giardiasis.

Precautions And Contraindications
- Avoid in patients with myopathy and hepatic, gastrointestinal or neurological disorders, psoriasis and porphyria.
- Avoid parenteral chloroquine; when required → given as a slow infusion.
- Gold/penicillamine + chloroquine → severe dermatitis.
Avoid chloroquine, quinine, and mefloquine (MFQ) together because:

- Chloroquine + halofantrine (minimum gap of 12 hours needed) → ↑ Risk of arrhythmias
- Avoid chloroquine in patients with retinal diseases. When chloroquine is given in high doses for a long time, regular neurological and eye examination should be done.
- Magnesium containing antacids and kaolin
- Antacids with Magnesium, kaolin → ↓ Absorption of chloroquine → Avoid
Amodiaquine:
- Amodiaquine is similar to chloroquine in actions and adverse effects but is somewhat better tolerated.
- It may be used in uncomplicated falciparum malaria.
Quinine
Question 10. What is the status of quinine in treatment of malaria?
Or
Short note on:
Answer:
Quinine.
- Quinine (QN) is an alkaloid obtained from the bark of the cinchona tree.
- The name cinchona probably comes from the name of a Countess ‘Chinchon’— the wife of the Viceroy of Peru who was cured of her fever by quinine in 1638.
Quinine Actions:
- Quinine destroys erythrocytic forms of the parasite similar to chloroquine and is useful as a suppressive. It is rapidly acting and is often effective even in chloroquine-resistant strains of P. falciparum.
- It is also gametocytocidal for three species of the malarial parasite except for P. falciparum. Quinidine, the d-isomer of quinine, can be used in place of quinine.
Quinine Mechanism of action:
- Quinine may act like chloroquine by inhibiting the enzyme heme polymerase.
- Resistance to quinine is now known in some parts of the world.
Quinine Other actions: Quinine also has
- Mild analgesic and antipyretic activity.
- Myocardiac depressant like quinidine.
- Local anesthetic properties (sodium channel blocker).
- Is a skeletal muscle relaxant.
- Quinine stimulates the uterus (ecbolic) and is an abortifacient.

Quinine Pharmacokinetics:
- Quinine is rapidly and well absorbed, widely distributed in the body tissues.
- The half-life of quinine is longer in patients with malaria because of increased protein binding (↑ an acid glycoprotein) in malaria. It is metabolized in the liver and excreted in the urine. Dose: 600
mg TDS 3–7 days.
Quinine Adverse effects: These are many and some are serious.
- GIT: Quinine is highly bitter and is a gastric irritant—causes nausea, vomiting and epigastric pain—hence poorly tolerated.
- Hypoglycemia: Can be quite severe and result in coma. Hypoglycemic coma should be distinguished from cerebral malaria. Hypoglycemia may be because:
- Quinine stimulates the pancreatic beta cells to release insulin.
- Parasite consumes glucose.
- Decrease in food intake due to malaria.
- Cinchonism: With ringing in the ears, high tone deafness, headache, nausea, visual disturbances and vertigo may be encountered.

- Neurotoxicity in higher doses can cause convulsions.
- CVS: Quinine can cause hypotension (this can be profound, if injected rapidly), widening of QRS complex, AV block and arrhythmias. Hence constant monitoring of cardiovascular functions is a must while on IV quinine.
- Allergic reactions:
- Black water fever—quinine can precipitate acute hemolytic anemia with renal failure, hemoglobinuria and fever which can be fatal. Fortunately, this complication is uncommon and is thought to be a hypersensitivity reaction.
- Skin rashes, urticaria and angioedema. Idiosyncratic reactions with cinchonism from a single dose of quinine is not very common.
- Poisoning: Hypoglycemia, fever, delirium, confusion, hypotension, cardiac arrhythmias, and coma may develop. Fatal dose of quinine is 2–8 g. Death is due to respiratory arrest.
Precautions And Contraindications
- IV quinine → as slow infusion with cardiac function monitoring oral preferable.
- Watch for hypoglycemia → adequate glucose supplementation should be given.
- Quinine + Mefloquine → cardiotoxicity.
Quinine Uses:
- Malaria:
- Uncomplicated falciparum malaria: Quinine 600 mg TDS oral for 3 days + Doxycycline 100 mg BD for 7 days. (to reduce the duration of quinine use). Not preferred now.
- Complicated falciparum malaria and cerebral malaria: As an alternative to artemisinin.
- Quinidine can be used in place of quinine.
- Babesiosis: A combination of quinine and clindamycin—first line treatment.
- Nocturnal muscle cramps: Low dose quinine—200–300 mg at night relieves nocturnal muscle cramps. However, safer muscle relaxants are now available.
- Myotonia congenita: Quinine is useful in relieving the muscle spasms.
Artemisinin And Derivatives
Artemisinin:
- ArtemisininA sesquiterpene lactone is a highly bitter compound obtained from the plant
- Artemisia annua which has been used in the Chinese traditional medicine as ‘Quinghaosu’ for almost 2000 years.
- Several semisynthetic derivatives have been obtained with better efficacy and improved pharmacokinetic profile including—artesunate, dihydroartemisinin, artemether
and arteether. - Artemisinin derivatives are now the first-line drugs in the treatment of falciparum malaria.
Artemisinin Mechanism of action:
- Artemisinin → interacts with heme → generation of free radicals → damage the macromolecules and the parasite membrane
- Monotherapy with these drugs should be avoided to prevent development of resistance.
Artemisinin Actions:
- Artemisinin is a potent, rapidly acting, antimalarial targeting the parasite in the RBCs (erythrocytic schizonticide)—effective against all the 5 plasmodial species including MDR P. falciparum.
- It is also effective against gametocytes (but not the liver stages). It is useful in cerebral malaria.
Artemisinin Disadvantage:
- Recrudescence is common due to its short t½—combining with drugs like mefloquine avoids this.
- Artemisinin has activity against other organisms like T. gondii, Leishmania major and schistosomes.
Artemisinin Pharmacokinetics:
Artemisinin is poorly soluble in water and oil. The derivatives are given by different routes:
- Artesunate—water-soluble—oral, IM, IV, rectal.
- Artemether—lipid soluble—oral, IM and rectal.
- Dihydroartemisinin—water soluble—oral.
- Arteether—longer—IM.
They are rapidly absorbed. Artemisinin and artemether are prodrugs; they are microsomal enzyme inducers and both increase their own metabolism when multiple doses are used.
Artemisinin Adverse effects:
- Artemisinin and its derivatives are the best tolerated antimalarials—mild gastrointestinal symptoms, fever, and bradycardia are reported—these could be due to malaria itself.
- They can also cause itching, rashes, other allergic reactions and rarely raised serum transaminases.
- Bone marrow toxicity with anemia, hemolysis, neutropenia and decrease in reticulocyte count are rare and reversible. Artemisinin can be used in pregnant women only during the 2nd and 3rd trimesters.
Artemisinin-Based Combination Therapy
Artemisinin-based combination therapy (ACT) is the WHO recommended treatment for all confirmed cases of falciparum malaria.
Artemisinin Advantages of the combination therapy are:
- Rapid action and rapid clinical response
- Better efficacy
- High cure rates
- Fast parasite clearance
- Reduced risk of development of resistance
- Fewer toxic effects → hence better tolerated
- In some cases, shorter duration of treatment.
Artemisinins have a short t½ and this is compensated by adding a second drug like mefloquine, lumefantrine or sulfadoxine-pyrimethamine. WHO has particularly listed some ACT regimens to be used in falciparum malaria.
For uncomplicated MDR falciparum malaria—ACT is given orally. For complicated and severe infections—parenteral regimens of ACT are recommended. Intravenous artesunate is highly effective and reduces mortality in severe falciparum malaria and is, therefore, preferred over quinine in such patients.
Some of the ACT are:
- Artesunate + sulfadoxine – pyrimethamine (AS–SP)
- Artemether + lumefantrine (AL)
- Artesunate + mefloquine (AS-MQ)
- Artesunate + amodiaquine (AS-AQ)
- Dihydroartemisinin + piperaquine (DHA-PPQ)
Pyronaridine: Pyronaridine is effective against erythrocytic forms of the malaria parasite.
Mefloquine
- A quinoline methanol
- Single oral dose is effective against erythrocytic forms of the malaria parasite including the
- MDR P. falciparum.
- Mechanism of action—may be like chloroquine—inhibiting heme polymerase.
Well absorbed when given orally and has a long t½ of 20–30 days—as it undergoes extensive enterohepatic circulation; since it causes severe local irritation at the site, it is not given parenterally. It is excreted through the gut.
Dose: 20 mg/kg single dose or in 2 divided doses.
Mefloquine Adverse effects:
- Nausea, vomiting, dizziness, confusion, headache, abdominal pain, sleep disturbances are common.
- CNS effects like ataxia, disorientation, visual and auditory disturbances, seizures, encephalopathy and psychotic manifestations are rare and reversible.
- Mefloquine can depress cardiac conduction resulting in bradycardia and arrhythmias.
Mefloquine Contraindications:
- Avoid in—arrhythmias, conduction defects of the heart, epileptics, and in psychiatric patients.
- Mefloquine should not be combined with quinine and halofantrine.
- Avoid in the first trimester of pregnancy.
Mefloquine Uses:
- Uncomplicated MDR falciparum malaria with artesunate.
- Prophylaxis of MDR malaria in travelers.
Halofantrine And Lumefantrine
Schizonticidal against erythrocytic forms of all Plasmodium species including MDR strains of P. falciparum. Actions are similar to mefloquine.
Halofantrine Disadvantages:
- Response to oral dosage is unpredictable due to variable absorption → Toxicity due to good absorption or therapeutic failure due to poor absorption (Absorption increased by fatty food).
- Halofantrine cannot be given parenterally—a disadvantage in emergencies.
Halofantrine Adverse effects:
- Gastrointestinal disturbances, headache, rashes, pruritus, and cardiotoxicity including prolongation of QT interval and arrhythmias.
- It is also contraindicated in pregnancy.
- Lumefantrine is less toxic and better tolerated.
Halofantrine Uses:
- Halofantrine was used in MDR falciparum malaria—but not preferred now.
- Lumefantrine + artemisinin (ACT-AL) in MDR falciparum malaria with fatty food for good bioavailability.
Primaquine
Primaquine is effective against all forms of the malarial parasite except erythrocytic forms.
- Causal prophylactic → Destroys the parasite in the liver cells and prevents the invasion of erythrocytes—generally not used for this purpose.
- Hypnozoitocidal → Destroys the hypnozoites (exoerythrocytic forms) in the liver and prevents relapse of P. vivax and P. ovale malaria.
- Gametocidal: Destroys the gametocytes of all species of the malarial parasite.
- Has weak activity against the erythrocytic forms.
The mechanism of action of primaquine is not known.
Primaquine Pharmacokinetics:
Primaquine is completely absorbed when given orally and is widely distributed.
Primaquine Adverse effects:
- Primaquine is well-tolerated in therapeutic doses. Epigastric distress can occur.
- In G6PD deficiency, primaquine can induce hemolysis. normal erythrocytes need G6PD to protect their membrane from damage due to chemicals and drugs.
- In G6PD deficient erythrocytes primaquine can induce the generation of free radicals leading to hemolysis.
Primaquine Uses:
Radical cure of P. vivax and P. ovale malaria: Primaquine with a blood schizonticide— destroys hypnozoites and gametocytes. 15 mg/day for 14 days.
- Gametocidal effects: In P. falciparum malaria—45 mg single dose.
- Terminal prophylaxis: After a visit to an endemic area—along with regular chloroquine prophylaxis → primaquine (15–30 mg for 14 days) to destroy hypnozoites and gametocytes.
- Chemoprophylaxis of malaria: As an alternative to mefloquine/doxycycline, primaquine 30 mg daily is effective but routine use is not recommended.
- Pneumocystis jiroveci: As an alternative to cotrimoxazole—clindamycin + primaquine
Tafenoquine: Tafenoquine is longer acting (t½ 4 day) → hence a single dose for prevention of relapse.
Folate Antagonists
Question 11.Short note: Folate antagonists.
Answer:
Pyrimethamine:
- Effective against the erythrocytic forms of all 4 species of plasmodia but is slow acting.
- The pyrimethamine + sulfadoxine combination acts faster.
- Has a long t ½ of 3.5–4 days thereby permitting once a week administration for prophylaxis.

Pyrimethamine Mechanism of Action:
- Pyrimethamine is a dihydrofolate reductase inhibitor.
- It binds plasmodial dihydrofolate reductase with about 2,000 times higher affinity than mammalian enzymes Given with sulfadoxine they produce sequential blockade resulting in inhibition of nuclear division.
- This mode of action makes them slow acting.
- The combination is synergistic and the development of resistance is slower. Pyrimethamine (25 mg) can also be combined with dapsone (100 mg) instead of sulfonamides.
- The combination may cause nausea, rashes, and in high doses megaloblastic anemia.
- Sulfadoxine may cause serious allergic reactions including Stevens-Johnson syndrome.
Pyrimethamine Uses:
- Malaria: Sulfadoxine 500 mg pyrimethamine 25 mg(SP) combination is used with artemisinine (ACT) and with quinine for the treatment of malaria.
- Toxoplasmosis: Sulfadoxine-pyrimethamine treatment of choice for Toxoplasma gondii infection.
- Pneumocystosis: Caused by P. Jiroveci, SP—alternative to cotrimoxazole.
Proguanil (Chloroguanide)
- Proguanil is a biguanide. It is an erythrocytic schizonticide and also has causal prophylactic activity against the pre-erythrocytic forms of the malaria parasite.
- The onset of action is slow and when used as monotherapy resistance develops rapidly → hence used with atovaquone.
Proguanil Mechanism of action:
- Proguanil, a prodrug, is converted to cycloguanil in the body.
- This metabolite is an inhibitor of dihydrofolate reductase in the Plasmodium.
Proguanil Adverse effects: Nausea, vomiting, diarrhea, abdominal pain, and rarely hematuria.
Proguanil Uses: With atovaquone in MDR falciparum malaria
Atovaquone
- Atovaquone is a naphthaquinone, effective against the erythrocytic forms of plasmodia.
- When combined with proguanil, the activity is synergistic and resistance is less common. Atovaquone is also effective against T. gondii and P. jiroveci infections.
Atovaquone Mechanism of action:
- Atovaquone inhibits mitochondrial electron transport leading to the collapse of the mitochondrial membrane potential in the malarial parasite. Proguanil potentiates this action.
- Atovaquone also inhibits ATP synthesis in the parasite.
- Atovaquone is effective orally, fatty food increases its absorption and has a long t½ of 2–3 days.
Atovaquone Adverse effects:
- Vomiting, headache, abdominal pain, diarrhea, skin rashes, and insomnia.
- Atovaquone is contraindicated in pregnancy.
Atovaquone Uses:
- Chloroquine-resistant and MDR falciparum malaria. Atovaquone 250 mg + proguanil 100 mg tablets 4 tabs daily for 3 days.
- Chemoprophylaxis of falciparum malaria—1 tablet daily.
- P. jiroveci infection—alternative to cotrimoxazole given for 3 weeks.
- The preferred antimalarials in the treatment and prophylaxis are given in the Table
Preferred antimalarials in the treatment and prophylaxis of malaria:



Antibiotics In Malaria
- Tetracycline: Tetracycline has weak activity against erythrocytic forms of malaria parasites.
- Doxycycline: Doxycycline with quinine or artesunate for treatment and chemoprophylaxis.
- Clindamycin: Clindamycin alternative to doxycycline with quinine/artemisinin.
- Fluoroquinolones: Fluoroquinolones and azithromycin also have antimalarial activity.
Immunity in malaria:
- People living in an endemic area can develop antibodies to erythrocytic forms of the malaria parasite.
- Immunity can be both humoral and cell-mediated. Immunity is specific to the species and strain prevalent in that particular area and lasts for 6–12 months.
- Maternal antibodies protect infants up to a few months of life.
Malaria vaccine:
- Vaccines against the different stages of the parasite, viz sporozoite vaccine, merozoite vaccine, and gametocyte vaccine are studied.
- The presence of multiple strains of the malaria parasite has been a major problem in the development of an effective vaccine for malaria.
Malaria in Pregnancy:
- P. vivax malaria—chloroquine
- P. falciparum malaria—
- Uncomplicated:
- 1st trimester: quinine + clindamycin (7 days)
- 2nd and 3rd trimesters: ACT (artemether + lumefantrine)
- Alternatives:
- ACT with mefloquine
- Quinine
- Complicated: ACT
Antiamoebic Drugs
Question 12. Name the drugs used in amoebiasis. Write the pharmacology of metronidazole.
Answer:
Amoebiasis:
- Amoebiasis caused by the protozoan Entamoeba histolytica spreads by fecal contamination of food and water.
- Though it primarily affects the colon, other organs like the liver, lungs, and brain are the secondary sites.
- Acute amoebiasis is characterized by bloody mucoid stools and abdominal pain.
- Chronic amoebiasis manifests as anorexia, abdominal pain, intermittent diarrhea, and constipation. Cyst passers or carriers are usually symptom-free—they are asymptomatic carriers.
Metronidazole Classification:

Metronidazole:
Metronidazole is a powerful amoebicide—kills the trophozoites and is effective in both intestinal and extraintestinal amoebiasis. Apart from this, it also inhibits Trichomonas vaginalis, Giardia lamblia, and Balantidium coli. Anaerobic bacteria are also sensitive to metronidazole.

Metronidazole Mechanism of action:
- Metronidazole is a prodrug. Several microorganisms including anaerobic bacteria and certain protozoa reduce the nitro group of metronidazole by a nitroreductase and convert it to a cytotoxic derivative which inhibits protein synthesis
- Aerobic bacteria lack this nitroreductase and are, therefore, not susceptible to metronidazole.
Metronidazole Pharmacokinetics:
- Metronidazole is well absorbed, widely distributed, penetrates all tissues, and reaches adequate concentrations in the CSF.
- It has a plasma t½ of 8 hours. It is metabolized in the liver.
Metronidazole Adverse effects:
- Gastrointestinal effects like nausea, anorexia, stomatitis, glossitis, furry tongue; abdominal pain, and a metallic taste in the mouth are common.
- Headache, dizziness, insomnia, ataxia, vertigo and rarely, on IV use, peripheral neuropathy can occur.
- Pruritus, urticaria, and skin rashes can also occur. IV injection can cause thrombophlebitis—adequate dilution of the drug solution is needed
- High doses given IV can cause convulsions—use cautiously in patients with neurological diseases and severe hepatic dysfunction. It is contraindicated in pregnancy.
Metronidazole Drug Interactions:
- Metronidazole + alcohol → Disulfiram-like reaction → Avoid alcohol.
- Cimetidine → Microsomal enzyme inhibitor → ↑ Metronidazole plasma levels → Toxicity.
Metronidazole Uses:
- Amoebiasis: Drug of choice in all forms of amoebiasis—but does not eradicate the cysts.
- Trichomonas vaginitis: Metronidazole is the drug of choice.
- Giardiasis: Metronidazole is the drug of choice Table 19.
- Anaerobic infections: Drug of choice—given IV for serious infections, particularly C. difficile enteritis. Also useful for surgical prophylaxis of abdominal and pelvic infections.
- H. pylori infections: In peptic ulcer patients, metronidazole + clarithromycin + omeprazole.
- Pseudomembranous colitis: Due to Clostridium difficile responds.
- Acute ulcerative gingivitis: Metronidazole an alternative to penicillin G.
- Dracunculosis: Facilitates extraction of the guinea worm.
- Topical preparations: 1% gel is used in skin infections and acne.

- Tinidazole: Tinidazole is longer acting and is better tolerated than metronidazole—can be used in place of metronidazole.
- Secnidazole: Secnidazole is longer acting → single 2 g dose for most indications of metronidazole.
- Ornidazole: Ornidazole is similar to tinidazole.
- Satranidazole: Satranidazole does not cause a disulfiram-like antabuse reaction and is better tolerated.
- Nimorazole: Nimorazole is similar to metronidazole.
Emetine and dehydroemetine:
- Emetine is an alkaloid, derived from ipecac (Brazil root) and dehydroemetine is a semisynthetic analog. They directly affect the trophozoites but not the cysts.
- As oral absorption is not reliable, they are given parenterally (SC or IM but not IV).
- Used only in severe amoebiasis when metronidazole cannot be used but is generally not preferred due to toxicity. Adverse effects include pain at the injection site, thrombophlebitis, nausea, vomiting, and diarrhea.
- Cardiotoxicity including arrhythmias, hypotension, and cardiac failure.
- Dehydroemetine is preferred over emetine as adverse effects are milder.
- Diloxanide furoate: Is directly amoebicidal. Given orally, it is split in the intestines to diloxanide and furoic acid and acts on the parasite in the intestines but not in the tissues.
- Flatulence, nausea, and occasionally abdominal cramps and rashes can occur.
Emetine Uses:
- Eradication of cysts:
- Diloxanide + nitroimidazole for the cure of amoebiasis, as diloxanide eradicates cysts.
- It can be used alone in asymptomatic cyst passers and mild intestinal amoebiasis.
Nitazoxanide
- Congener of niclosamide.
- Effective against E. histolytica, T. vaginalis, Giardia, H. pylori, and also some intestinal helminths like Ascaris and H. nana.
- Nitazoxanide and its active metabolite nitazoxanide inhibit the PFOR pathway which is needed in the anaerobic metabolism of both protozoa and some bacteria.
- Well-tolerated as adverse effects are rare. It causes a greenish tint to the urine; should be avoided in pregnancy.
- Dose: 500 mg BD for 3 days.
Nitazoxanide Uses:
Giardiasis, amoebiasis, cryptosporidia, C. parvum, Ascaris, T. trichura E. vermicularis and some tapeworms.
Iodoquinol and quiniodochlor
- These 8-hydroxyquinolines are directly acting luminal amoebicides effective orally.
- The exact mechanism of action is not known.
Iodoquinol Adverse effects:
- Include headache, nausea, vomiting, abdominal pain, and diarrhea.
- Iodine present in these compounds may result in thyroid enlargement, pruritus, and skin rashes.
Prolonged use → neurotoxicity including subacute myeloid optic neuropathy → there may be an irreversible loss of vision.
Iodoquinol Uses:
Were used for asymptomatic amoebiasis but diloxanide which is safer is now preferred.
Paromomycin:
- Paromomycin is an aminoglycoside antibiotic given orally. It is poorly absorbed from the gut and acts as an intestinal amoebicide.
- Adverse effects are mild and include diarrhea and abdominal discomfort.
Tetracyclines:
- The older tetracyclines, like chlortetracycline, are not well absorbed and large amounts reach the colon where they inhibit the intestinal flora and break the symbiosis between them and the amoebae.
- Tetracyclines are used as adjuvants in chronic intestinal amoebiasis.
Chloroquine:
- Chloroquine attains high concentration in the liver, is directly toxic against trophozoites, and is, therefore, useful in hepatic amoebiasis.
- As chloroquine is completely absorbed from the small intestines, it is not effective against amoebae in the colon. It is used (500 mg/day for 21 days) as an alternative to metronidazole in hepatic amoebiasis.
- A luminal amoebicide should also be given.
Treatment Of Different Forms Of Amoebiasis
Acute intestinal amoebiasis: One of the following can be given.
- Metronidazole 400–800 mg TDS for 5–7 days or 2.4 g OD for 3 days
- Tinidazole 2 g OD for 3 days or
- Secnidazole 2 g single dose
Alternatively, ornidazole/satranidazole/ benznidazole may be used followed by diloxanide furoate 500 mg TDS for 10 days to eradicate the cysts
- Chronic amoebiasis and asymptomatic cyst passers:
- Diloxanide furoate 500 mg TDS for 10 days or tetracycline 250 mg QID for 10 days.
- The alternatives are iodoquinol (650 mg TDS for 21 days) or paromomycin (10 mg/kg TDS for 7 days).
- Hepatic amoebiasis:
- Requires intensive treatment for the complete eradication of the parasite from the liver to avoid relapses. Metronidazole 600–800 mg TDS for 10 days or tinidazole are the first-line drugs.
- In addition, chloroquine may be given to ensure complete destruction of the liver forms. A course of diloxanide for 10 days should follow to eradicate the cysts.
Drugs used in giardiasis and trichomoniasis:

Treatment Of Pneumocystosis
Pneumocystis jiroveci is a microorganism having features of both protozoa and fungi though now considered to be a fungus. It causes opportunistic infections particularly pneumonia in patients with AIDS which can be fatal.
Drugs used in the treatment of pneumocystosis are:
- Cotrimoxazole: High oral dose of trimethoprim 20 mg/kg + sulfamethoxazole 75 mg/kg daily in 3–4 divided doses to be continued for 21 days. Folinic acid should be added to prevent toxicity.
- Pentamidine: 4 mg/kg daily for 14 days parenterally.
- Atovaquone: As an alternative to cotrimoxazole.
- Pyrimethamine-sulfadoxine: As an alternative for treatment and for chemoprophylaxis in immunocompromised patients—one double-strength tab/day.
Treatment Of Leishmaniasis
Leishmaniasis is caused by protozoa of the genus Leishmania. Kala-azar or visceral leishmaniasis is caused by Leishmania donovani; oriental sore by L. tropica and mucocutaneous leishmaniasis by L. braziliensis. The infection is transmitted by the bite of the female sandfly
Phlebotomus. It is endemic in Bihar.
Drugs used in Leishmaniasis are:
- Antimony compounds: Sodium stibogluconate, meglumine antimonate.
- Other drugs: Pentamidine, amphotericin B, ketoconazole, miltefosine, allopurinol, paromomycin.
- Sodium stibogluconate:
- Sodium stibogluconate a pentavalent antimonial is the most effective drug in kala-azar.
- It is also effective in mucocutaneous and cutaneous leishmaniasis. The mechanism of action is unknown.
Leishmaniasis Adverse effects:
- Include a metallic taste in the mouth, nausea, vomiting, diarrhea, headache, myalgia, arthralgia, pain at the injection site, bradycardia, skin rashes, hematuria and jaundice.
- Some cases of sudden death due to shock have occurred. ECG should be monitored as arrhythmias can occur during the later days of therapy.
- Meglumine antimonate and ethylstibamine can also be used in all forms of leishmaniasis.
Pentamidine:
- Pentamidine is effective against Leishmania donovani, trypanosomes, Pneumocystis jiroveci, and some fungi.
- Given intramuscularly the drug is rapidly absorbed but very little reaches the CNS.
Pentamidine Adverse effects:
- Pentamidine liberates histamine which is responsible for vomiting, diarrhea, flushing, pruritis, rashes, tachycardia and hypotension apart from pain at the injection site.
- Other effects include hepatotoxicity, renal impairment, ECG changes, and in some patients diabetes mellitus may be precipitated.
Pentamidine Uses:
- Leishmaniasis: In visceral leishmaniasis as an alternative to sodium stibogluconate.
- Trypanosomiasis (sleeping sickness): As an alternative to suramin or along with suramin. It can also be used for chemoprophylaxis of African trypanosomiasis.
- Pneumocystosis: An alternative in Pneumocystis jiroveci infections.
Miltefosine:
- It is the first drug that can be used orally in leishmaniasis. It has high efficacy against both visceral and cutaneous leishmaniasis. It is effective also in leishmania resistant to stibogluconate.
- Miltefosine is safe—vomiting and diarrhea are common, while raised liver enzymes and creatinine are reversible. It is contraindicated in pregnancy.
Other Drugs:
- Amphotericin: Amphotericin B has been tried in endemic areas where antimonials may be ineffective.
- Ketoconazole: Ketoconazole inhibits ergosterol synthesis in Leishmania → Effective in cutaneous leishmaniasis.
- Allopurinol: Allopurinol in Leishmania, allopurinol is converted to a metabolite which inhibits protein synthesis. It may be used along with antimonials.
- Paromomycin: Paromomycin (aminosidine) is an amoebicidal aminoglycoside, also effective in all forms of leishmaniasis. Used alone or with antimonials.
Drugs for oriental sore (dermal leishmaniasis):
- Drugs for oriental sore—sodium stibogluconate 200 mg in 2 mL is injected around the sore.
- Paromomycin ointment may be applied topically on the sore.
Treatment Of Trypanosomiasis
- Trypanosomiasis is caused by protozoa of the genus Trypanosoma. African trypanosomiasis or sleeping sickness is caused by T. gambiense and T. rhodesiense, while South
- American trypanosomiasis is caused by T. cruzi. Drugs used in trypanosomiasis are suramin, pentamidine, melarsoprol, eflornithine, nifurtimox and benznidazole.
Suramin sodium:
- It is the drug of choice for early stages of trypanosomiasis. It does not cross the BBB and, therefore, cannot be used in the later stages of the disease.
- It is also useful for prophylaxis but pentamidine is preferable. It may be traced for nearly 3 months in the plasma.
- Suramin is also effective in eradicating adult forms of Onchocerca volvulus.
- Toxicity is high; vomiting, shock, and loss of consciousness may follow IV injections.
- Rash, neuropathies, hemolytic anemia, and agranulocytosis may also occur.
Melarsoprol:
- Melarsoprol is the preferred drug in later stages of trypanosomiasis associated with encephalitis and meningitis. Eflornithine an alternative in CNS trypanosomiasis.
- Nifurtimox and benznidazole are useful in Chaga’s disease (American trypanosomiasis).
Antihelmintics
Question 13 .Write short note on
- Albendazole/mebendazole
- Pyrantel pamoate
- Piperazine citrate
- Praziquantel
- Diethylcarbamazine
- Ivermectin.
Or
Uses of albendazole.
Answer:
Worm infestations are more common in developing countries. It is seen in people with poor hygiene. Antihelmintics are deworming agents. A vermicidal kills, while a vermifuge promotes the expulsion of worms.
Preferred drugs for helminthiasis infections:

Anthelmintics include:
- Mebendazole
- Albendazole
- Pyrantel pamote
- Piperazine citrate
- Levamisole
- Praziquantel
- Diethylcarbamazine
- Ivermectin
Benzimidazoles:
Benzimidazoles include thiabendazole, mebendazole and albendazole.
Thiabendazole:
Thiabendazole is the first agent of this but now mebendazole and albendazole are more commonly used due to milder toxicity and better antihelmintic effect.
Mebendazole
- Mebendazole a broad-spectrum antihelmintic cures roundworm, hookworm, pinworm, and Strongyloides infestations.
- The eggs and larvae are also destroyed.
- The dead parasites are slowly expelled from the gut over several days.
Mebendazole Mechanism of action:
- Benzimidazoles bind to the β-tubulin of the parasite with high affinity (~400 times more than for humans) and inhibit the synthesis of microtubules.
- These microtubules are essential for several metabolic processes in the parasite. Benzimidazoles also inhibit glucose uptake in the parasite.
Mebendazole Pharmacokinetics:
- Mebendazole is poorly absorbed from the gut and also undergoes first-pass metabolism.
- Fatty food enhances absorption. Dose: 100 mg BD for 3 days or 500 mg single dose.
Mebendazole Adverse effects:
- Mebendazole is well-tolerated; nausea, abdominal pain, and diarrhea may be seen in heavy infestations.
- Large doses may cause headaches, dizziness, loss of hair, and granulocytopenia.
- Rarely, it may provoke abnormal migration of the roundworms which may come out through the mouth or nose.
- It should be avoided in pregnancy and in children <2 years.
Mebendazole Uses:
- Treatment of roundworm, hookworm, pinworm, tapeworm, trichuriasis, and hydatid disease.
- It is of special value in multiple worm infestations.
Albendazole
- Albendazole a congener of mebendazole is a broad-spectrum antihelmintic.
- It is a prodrug and the active metabolite has good efficacy against roundworm, hookworm, pinworm, threadworm, tapeworm, and trichuriasis. It is also useful in hydatic disease as the active metabolite penetrates the hydatic cyst.
- Albendazole has actions and mechanisms of action similar to mebendazole but it has several advantages over mebendazole because of which it is the preferred benzimidazole.
Advantages Over Albendazole
- The active metabolite of albendazole achieves a higher concentration (100 times more) than mebendazole.
- Albendazole is better tolerated.
- Effective in a single dose in most infections.
- Superior to mebendazole in hookworm and threadworm infections, hydatid disease, and neurocysticercosis.
- Also has some activity against Trichomonas vaginalis, Giardia lamblia, and W. bancrofti.

Albendazole Pharmacokinetics:
- Albendazole is rapidly absorbed from the gut and fatty food increases its absorption.
- Hence it should be given on an empty stomach for treating intestinal worms while for parasites in the tissues, albendazole is given with a fatty meal.
- It penetrates well into tissues including CSF and hydatid cysts.
- It is rapidly metabolized in the liver and excreted in urine.400 mg chewable tab, 200 mg/5 mL suspension.
Albendazole Adverse effects:
- Are minor and similar to mebendazole. Nausea, diarrhea, abdominal pain, headache, dizziness, and allergic reactions can occur.
- High doses used over a long time can cause jaundice, fever, weakness, alopecia, and granulocytopenia. Albendazole should be avoided in pregnancy.
Albendazole Uses:
- Roundworm, pinworm: Albendazole drug of choice—single dose—400 mg; should be repeated after 2 weeks in pinworm infestation to prevent reinfection from ova that mature later. Trichinosis, hookworm, tapeworms, and strongyloidosis—400 mg daily for 3 days.
- Neurocysticercosis: Albendazole is the drug of choice (400 mg twice daily) but the duration depends on the number of cysts and may vary from 8 to 30 days. Glucocorticoids should be given before starting albendazole to prevent immunological reactions to the dead parasite.
- Hydatid disease: Albendazole drug of choice—400 mg BD for 4 weeks. If needed, the course may be repeated after 2 weeks. When the cysts are removed by surgery, albendazole is more effective in providing a cure.
- Filariasis: Albendaszole (400 ma) with DEC (6 mg/ kg) Or ivermectin (0.3 ma/ka) given as a single dose is found to be effective in W.bancrofti in suppressing microfilariae for l year This also prevents the spread of filariasis and may be continued once a year for 5 – 6 years.
Pyrantel Pamoate
Pyrantel pamoate is effective against roundworms, hookworm, and pinworms. It is poorly absorbed from the gut and acts on the worms in the gut. It stimulates the release of acetylcholine which activates the nicotinic cholinergic receptor in the worm leading to persistent depolarization and spastic paralysis (depolarizing neuromuscular blocker). It also inhibits the cholinesterase enzyme. The paralyzed worms are expelled.

It is well-tolerated; occasional abdominal pain, headache, rashes, weakness, and dizziness may occur.
Pyrantel Pamoate Uses:
- Single oral dose (11 mg/kg) in the roundworm, hookworm, and pinworm infestations. For pinworm, the dose is repeated after 2 weeks.
- Oxantel pamoate: It is effective in trichuriasis infection.
- Piperazine citrate: Piperazine citrate is effective in roundworm and pinworm infestations.
- Competitively blocks the action of acetylcholine → ↓ ↓ Contractions in the worms → Flaccid paralysis → Worms are expelled through the gut by peristalsis.It is also a GABA receptor agonist.
- Adverse effects are mild—gastrointestinal symptoms, headache, and dizziness.
- Uses: Roundworm infestation—also safe in pregnancy.
- Dose: 4 g OD for 2 days.
Levamisole:
- Levamisole is effective against roundworms and hookworms → Causes paralysis of the worms which are expelled live.
- It is well-tolerated and is effective in a single dose of 150 mg in a roundworm and 2 doses of 150 mg at an interval of 12 hours in hookworm infection.
- It is also an immunomodulator.
Niclosamide:
- Niclosamide is effective against most tapeworms. The segments of the dead tapeworms are partly digested and in the case of T. solium, the ova released from these segments may develop into larvae and reach various organs resulting in visceral cysticercosis.
- The purge may be given 2 hours after niclosamide to wash off the worms and avoid cysticercosis. The scolex detected in the stool ensures eradication.
- It is well-tolerated with occurrence of abdominal discomfort, pruritus, and rashes.
Niclosamide Uses:
- Alternative to praziquantel in tapeworms infestation like T. solium, T. saginata, H. nana and D. latum and in intestinal fluke infestations.
- Dose: 2 g in the morning on an empty stomach, to be chewed and swallowed.
Praziquantel
Praziquantel is effective against all schistosomes and most other trematodes and cestodes including in cysticercosis. It is effective as a single oral dose in most infestations.
Praziquantel Mechanism of action:
- It increases cell membrane permeability to calcium → Contraction, followed by → Paralysis → Worms are expelled.
- Adverse effects are mild and include GI disturbances, headache, dizziness, drowsiness, rashes, myalgia, and arthralgia.
- Praziquantel is contraindicated in ocular cysticercosis because the host response can cause repairable damage.
- Dose: 10–20 mg/kg.
Praziquantel Uses:
- Schistosomiasis: Praziquantel is the drug of choice in all forms of schistosomiasis.
- Tapeworms: Single dose (10 mg/kg) is effective in all tapeworm infestations. In T. solium, it has the advantage that it kills the larvae, and therefore, visceral cysticercosis is avoided.
- Neurocysticercosis: Praziquantel is an alternative to albendazole. Inflammatory reactions to the dying parasite may result in worsening of neurological symptoms. Glucocorticoids may be added but unfortunately, the bioavailability of praziquantel is reduced when taken with glucocorticoids.
- Other flukes: Effective in cestodes like H. nana, D. latum, C. sinensis and P. westermani.
Diethylcarbamazine
- Diethylcarbamazine (DEC) is effective in filariasis—W. bancrofti, B. malayi and B. timori.
- It immobilizes the microfilariae (MF) resulting in their displacement in the tissues and also alters their surface structure making them more susceptible to the host defense mechanisms.
- Microfilariae rapidly disappear from the blood except those present in hydroceles and nodules.
- It also kills the adult worms of Loa loa and prolonged treatment can kill the adult B. malayi and probably W. bancrofti.

DEC is rapidly absorbed in oral administration and is also rapidly metabolized. Alkalinizing the urine increases the plasma levels and prolongs the action of DEC. Dose should be reduced in renal dysfunction.
DEC Adverse effects:
- Are mild; anorexia, nausea, vomiting, dizziness, and headache.
- Allergic reactions with itching, rashes, and fever due to the release of proteins and antigens from the dying worms may occur. Antihistamines are given with DEC to minimize these reactions.
- DEC is contraindicated in onchocerciasis as it can cause severe reactions to products of destroyed microfilaria.
Pregnancy: ↑ ↑ PG production → Abortion → Avoid in pregnancy
DEC Uses
- Filariasis: DEC drug of choice (100 mg TDS for 21 days)—in 7 days, patients become noninfective to mosquitoes as microfilariae rapidly disappear. Adult worms may need repeated courses.
- Antihistamines should be started to reduce allergic reactions. If severe reactions are noted, glucocorticoids may be given.
- Mass treatment with DEC in endemic areas reduces filaria transmission. DEC (0.2–0.4%) incorporated into table salt or given as a single annual dose (6 mg/kg) with albendazole (400 mg) reduces microfilaria in the blood.
- Tropical eosinophilia (2 mg/kg TDS for 7 days)—symptoms rapidly disappear.
- Loa loa: The test dose of DEC should be given 50 mg/day for 3 days followed by 150 mg TDS for 2–3 weeks.
Ivermectin
- Ivermectin obtained from Streptomyces avermitilis is effective against many nematodes, arthropods, and filariae.
- It is very effective against the microfilaria of Onchocerca volvulus. It is microfilaricidal and also blocks the release of microfilariae from the uterus of adult worms.
- There is a rapid decrease in the microfilariae count in the skin and eyes.
- Ivermectin is as effective as DEC against W. bancrofti and B. malayi. It is also effective against Strongyloidis stercoralis, Ascaris lumbricoides, cutaneous larva migrans, Sarcoptis scabii, and lice.
- Dose: 10–15 mg single dose.
Ivermectin acts by paralysing the worms by binding to glutamate-gated chloride channels. It also increases the GABAergic transmission in the nerves of the nematodes.

Ivermectin Adverse effects:
- Ivermectin is well-tolerated. Apart from nausea and vomiting, allergic reactions can occur due to hypersensitivity to the dying microfilaria proteins (mazotti reaction).
- Ivermectin should not be used with other drugs that influence GABA activity (for example, Benzodiazepines, valproic acid) and in patients with meningitis and sleeping sickness as these conditions impair the BBB.
Ivermectin Uses:
- Onchocerciasis: Ivermectin drug of choice. Single dose of 150 mg/kg given orally once or twice a year till the adult worms die. Microfilariae in the anterior chamber may need prior glucocorticoids to avoid inflammatory reactions in the eye.
- Filariasis: 400 mg/kg ivermectin with 400 mg albendazole is given once a year.
- Strongyloidiasis: A single dose of 200 mg/kg repeated after 2 weeks is curative.
- Ivermectin: Ivermectin is also useful in cutaneous larva migrans, ascariasis, in scabies, and lice infestations in a single dose of 200 mg/kg.
- Doxycycline: Doxycycline is lethal to the adult worms of W. Bancrofti and Onchocerca volvulus. It has a unique mechanism of action—it kills the bacterium Wolbachia which exists in symbiosis with filaria. It may have an important role in the treatment of filariasis.
- Metrifonate: Metrifonate is a prodrug that is converted to dichlorovas—an organophosphorus insecticide.
- Oxamniquine: Oxamniquine is effective against S. mansoni → used as an alternative to praziquantel. It is well absorbed when given orally (15 mg/kg single dose) and it is safe and effective.
Drugs Used In Scabies
Scabies is caused by Sarcoptes scabiei or Acarus scabies (itch mite) more common in people with poor hygiene and is transmitted by close body contact with an infected person. Drugs used in scabies.
Permethrin:
- Permethrin, a synthetic pyrethroid, is an insecticide effective against scabies and lice. 5% cream is applied all over the body below the chin and washed after 12 hours.
- The insects are paralysed and a single application is sufficient in most patients. It is safe, effective, convenient to use and well-tolerated with nearly 100% cure rates.
Benzyl benzoate:
- After a hot scrub bath the emulsion should be applied over the entire body below the chin including the soles of the feet.
- The application should be repeated after 12 hours and after the next 12 hours, the hot scrub bath should be repeated. Benzyl benzoate can cause irritation, especially when repeated frequently.
Ivermectin:
- An antihelmintic is effective in scabies and pediculosis. A single dose of 200 mg/kg given orally is highly effective and cure rates have been 91–95%.
- It is well-tolerated but should be avoided in pregnant and lactating women and in children.
Lindane or gamma benzene-hexachloride (Gammexane, BHC):
- 1% lindane cream is applied over the body and the treatment is repeated after 2–3 days. It is an effective scabicide as well as pediculocide and resistance to lindane can be prevented by combining it with benzyl benzoate which improves efficacy.
- A disadvantage is that lindane is highly lipid-soluble because of which it can be absorbed through intact skin resulting in systemic toxicity. Lindane can cause arrhythmias and seizures—it is a CNS stimulant. It can rarely cause aplastic anemia.
Other drugs:
- Crotamiton is effective against both lice and scabies. 10% cream is applied 2–3 times at an interval of 24 hours followed by a wash.
- It is unlikely to cause irritation because of which it may be preferred in children.
Sulfur:
- 10% sulfur ointment—now not preferred because of an unpleasant smell and needs to be applied repeatedly.
- DDT is applied as a 2% lotion for pediculosis and scabies. It paralyses the insects. It is now not preferred because of the availability of better scabicides and pediculicides.
Tetmosol (monosulfiram):
- Tetmosol is related to disulfiram. A 5% solution is applied three times in 24 hours for scabies. It is an effective sarcopticide.
- It can cause mild irritation. Alcohol consumption should be avoided and cytosol should not be used in children below 5 years of age.
Drugs For Pediculosis
- Pediculosis is caused by the louse Pediculus humanus. Lice can infest scalp, body, or pubic region. Drugs used in lice infestations include:
- Permethrin 1% lotion or cream rubbed over the scalp, allowed to remain for 10 minutes, and then washed off. Permethrin is preferred for topical use.
- Ivermectin (200 mg/kg) is given orally as a single dose.
- DDT 2% lotion, gammaxane 2% shampoo, malathion 0.5% lotion but not preferred because of weak ovicidal action.
Cancer Chemotherapy
- The treatment of cancers, after so many years of research and experience, is still unsatisfactory due to certain special characteristics of the cancer cells—like capacity for uncontrolled proliferation, invasiveness, and metastasis.
- The host defense mechanisms which help us in infections are not doing so in cancers because these cancer cells are also host cells.
- To further complicate the problem, the cancer cells can remain in a resting phase during which they are not sensitive to anticancer drugs but can start multiplying later resulting in recurrence. These features have made the treatment of cancers quite difficult.
Phases of cell cycle: In the multiplication process of a cancer cell, 4 phases are involved—G1, S, G2, and M.
Cell cycle specific and non-specific drugs:
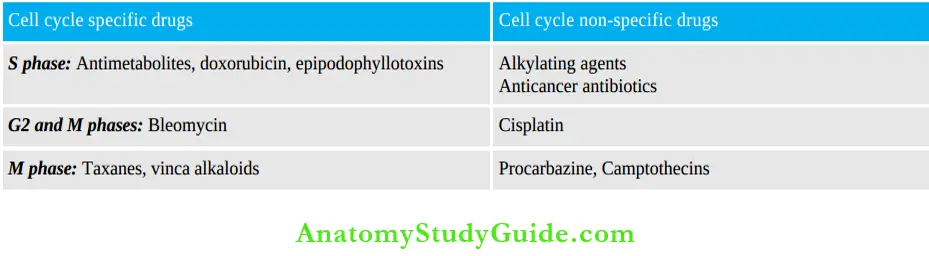

Common Adverse Effects of Anticancer Drugs
As most anticancer drugs act on the rapidly multiplying cells, they are also toxic to the normal rapidly multiplying cells in the bone marrow, epithelial cells of skin and mucous membranes, lymphoid organs, and gonads. Thus the common adverse effects are:
- Bone marrow: Bone marrow depression results in leukopenia, anemia, thrombocytopenia, and in higher doses—aplastic anemia. In such patients, infections and bleeding are common.
- Other rapidly multiplying cells:
- GIT—stomatitis, esophagitis, glossitis, and proctitis can be painful. Diarrhea and ulcers along the gut are common.
- Alopecia (loss of hair)—partial to total alopecia is seen on treatment with most anticancer drugs but is reversible after the chemotherapy is stopped.
- Reduced spermatogenesis in men and amenorrhea in women (due to damage to the germinal epithelium) can occur. For example, men treated with mechlorethamine for 6 months can become infertile.
- Immediate adverse effects: Nausea and vomiting → From stimulation of the CTZ → Starts about 4–6 hours after treatment and may continue for 1–2 days. Prior treatment with powerful antiemetics is required.
- Hyperuricemia: Rapid tumor cell lysis can result in increased plasma uric acid levels and may lead to ‘tumor lysis syndrome’ and renal failure.
- Teratogenicity: All cytotoxic drugs are teratogenic → Contraindicated in pregnancy.
- Carcinogenicity: Treatment with cytotoxic drugs may cause secondary cancers, for example, Leukemias may follow the treatment of Hodgkin’s lymphoma.
The adverse effects unique to some anticancer drugs are listed in Table Measures to prevent adverse effects to anticancer drugs are mentioned in Table 22.
Specific adverse effects of some anticancer drugs:

Measures to prevent the adverse effects of anti-cancer drugs:

Drugs used in cancer may be classified as follows.
Drugs Classification:

Alkylating
Alkylating agents are drugs that alkylate (donate an alkyl group to) other molecules by covalent bonds. They also alkylate DNA, RNA, and various enzymes and there is interstrand crosslinking of DNA.
Alkylating Actions:
Alkylating agents produce the following effects
- Cytotoxic effects: Alkylating agents destroy the rapidly multiplying cells—both cancer cells and normal host cells.
- Immunosuppressant effects: Alkylating agents are good immunosuppressants for which they are used in rheumatoid arthritis and other autoimmune disorders.
- Radiomimetic effects: The actions of alkylating agents resemble that of radiotherapy.
Alkylating Mechanism of action:
- On administration, alkylating agents form highly reactive derivatives (carbonium ions) which transfer alkyl groups to various cellular constituents like sulfhydryl, amino, hydroxyl, carboxyl, amine, and phosphate groups and bind them with covalent bonds.
- Thus such constituents are not available for normal metabolic reactions. They also bind to
- DNA and alkylate DNA which results in breakage of the DNA strand. Thus they produce cytotoxicity


Nitrogen Mustards
Question 14. Write short note on cyclophosphamide. Explain why mesna is given with cyclophosphamide.
Answer:
Cyclophosphamide: Cyclophosphamide is a prodrug converted to the active metabolite aldophosphamide in the liver.
- Aldophosphamide: Aldophosphamide is in turn converted to phosphoramide mustard and acrolein.
- Phosphoramide: Phosphoramide is responsible for cytotoxic activity and acrolein causes adverse effects.
- Cyclophosphamide is well absorbed in oral administration with high bioavailability; it can also be given IV.
- It also has immunosuppressant properties.

Cyclophosphamide Adverse Effects:
- Common adverse effects to anticancer drugs.
- Cystitis due to a metabolite acrolein can be prevented by giving IV Mesna, irrigating the bladder with acetylcysteine, and by giving large amounts of fluids.
- Mesna (sodium-2- mercaptoethane sulfonate) and acetylcysteine contain SH groups which bind the toxic metabolites and inactivate them.
Cyclophosphamide Uses:
- Hodgkin’s lymphoma
- In non-Hodgkin’s lymphomas (NHL), doxorubicin (hydroxydaunomycin), vincristine (oncovin), and prednisolone (CHOP regimen).
- Cyclophosphamide is also useful in Burkitt’s lymphoma in children, leukemias, and myeloma.
- As an immunosuppressive agent.
- Ifosfamide, an analog of cyclophosphamide, is longeracting.
- Chlorambucil is very effective against lymphomas.
- Melphalan is given orally in multiple myeloma and in ovarian tumors. Its actions and toxicities are similar to other nitrogen mustards.
Other Alkylating Agents
Busulfan: Busulfan An alkyl sulfonate, has selective activity against cells of the myeloid series and was the drug of choice in chronic myeloid leukemia—but now other drugs are preferred. Busulfan can cause skin pigmentation, hyperuricaemia, gynaecomastia, and pulmonary fibrosis.
Mind Map Cyclophosphamide:
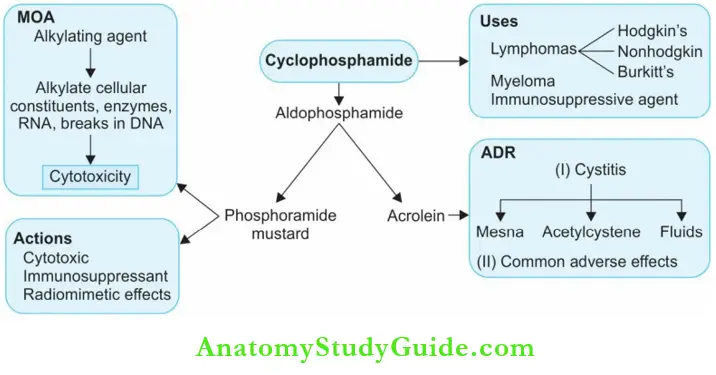
- Carmustine: Carmustine is effective in meningeal leukemias and brain tumors because it crosses the blood–brain barrier. It is also used in lymphomas and malignant melanoma.
- Temozolomide: Temozolomide is used in gliomas and melanoma. Photosensitivity and elevated liver function tests are noted apart from common adverse reactions.
- Procarbazine: Procarbazine is effective orally in Hodgkin’s lymphoma (MOPP regimen component) and in non-Hodgkin’s lymphoma and brain tumours. It damages DNA and produces breakages and chromosomal damage. This may make it carcinogenic.
Platinum Analogs
Cisplatin, carboplatin, and oxaliplatin are platinum-containing compounds. They get converted to the active form in the cell, inhibit DNA synthesis and cause cytotoxicity like alkylating agents.
Cisplatin:
- Cisplatin causes ototoxicity with tinnitus, loss of hearing, and nephrotoxicity. To reduce nephrotoxic effects, cisplatin is given as slow infusion with adequate hydration and a diuretic.
- Cisplatin is highly emitogenic–controlled with a 5-HT3 antagonist like ondansetron. Though peripheral neuropathy can occur, cisplatin is less toxic to bone marrow.

Cisplatin Uses:
Solid tumors like ovarian, testicular, and bladder cancer and cancers of the head and neck; particularly being useful in germ cell tumors.
Carboplatin: Carboplatin is a less toxic derivative of cisplatin.
The advantages over cisplatin are:
- Less nephrotoxic
- Less toxic to gutless vomiting
- Milder neurotoxicity
- Milder ototoxicity
- Better tolerated → Often preferred to cisplatin but more bone marrow toxic.
Oxaliplatin:
Oxaliplatin with fluorouracil and leucovorine called the FOLFOX regimen is used in advanced colorectal cancer and in other cancers like ovarian and cervical cancers. It is neurotoxic.
Antimetabolites
Folate Antagonists:
Methotrexate (MTX):
- Methotrexate is a prodrug converted to its active form (polyglutamate’s) in the cells and the reaction is catalyzed by the enzyme folypolyglutamate synthase (FPGS). The active metabolites bind to dihydrofolate reductase and prevent the formation of tetrahydrofolate (THF).
- This THF serves as a coenzyme essential in several reactions in DNA, RNA and protein synthesis (provides methyl groups). THF deficiency results in inhibition of DNA, RNA and protein synthesis.
- Thus rapidly multiplying cells are the most affected. Methotrexate is most effective on cells in the ‘S’ phase of the cell cycle.
Methotrexate Actions:
- Cytotoxic actions: Affects the bone marrow, skin, gastrointestinal mucosa, and other rapidly dividing cells.
- Also has immunosuppressant and some anti-inflammatory properties.
Methotrexate Pharmacokinetics:
Methotrexate is well absorbed when given orally; it is excreted mostly by the kidneys → Dose should be reduced in renal failure.
Methotrexate Adverse Effects
- Common adverse effects—bone marrow suppression, nausea, vomiting, diarrhea, alopecia, and dermatitis.
- Nephrotoxicity because it is precipitated in renal tubules → Contraindicated in renal impairment.
- Allergic pneumonitis can be fatal.
Leucovorin rescue:
Methotrexate toxicity can be largely prevented by administering folinic acid which (also called leucovorin or citrovorum factor) gets converted to a form of THF that can be utilized by the cells.
Leucovorin rescue Uses:
- Choriocarcinoma: Methotrexate is curative when treated early.
- ALL in children: Induces remission.
- Other cancers: Methotrexate is a component of multidrug regimens in lymphomas, breast cancer, bone sarcomas, and soft tissue sarcomas.
- Psoriasis: Methotrexate is effective in severe psoriasis.
- Rheumatoid arthritis: Low-dose methotrexate is used to induce remission in rheumatoid arthritis due to its immunosuppressant property.
Anti-inflammatory actions also help.
Pemetrexed, pralatrexate and ralitrexate are other folate antagonists used in cancer.
Mind Map—Methotrexate:

Purine Antagonists
6-mercaptopurine, thioguanine, fludarabine, pentostatin, and cladribine are purine analogs that act as purine antagonists because they are structurally similar to purines.
Purine Antagonists Mechanism of action:
- Purine analogs enter the cells and get converted to active metabolites (triphosphates) which are taken up into DNA in place of regular purines.
- They cause breakages in DNA strands and inhibit protein synthesis.
- Purine antagonists are used in leukemias and lymphomas.
Mercaptopurine (MP, 6-MP): Is metabolized by xanthine oxidase.

Purine Antagonists Adverse effects:
- Include bone marrow depression, anorexia, diarrhea, nausea, vomiting, stomatitis, jaundice, and dermatitis. Hyperuricemia may require treatment with allopurinol— the dose of MP should be reduced.
- Increased risk of squamous cell carcinoma of the skin and AML has been noted after prolonged use of MP.
Purine Antagonists Uses:
- Acute leukemias in children, choriocarcinoma, and some solid tumors.
- Azathioprine is converted to 6-MP in the cells and is a potent immunosuppressant used in rheumatoid arthritis.
Purine Antagonists Drug interaction:
- Mercaptopurine is metabolized by xanthine oxidase. Allopurinol inhibits xanthine oxidase (XO) and thus prolongs the action of 6-MP.
- When both drugs are given together, the dose of MP should be reduced by 50–75%.

- Thioguanine: Thioguanine is an analog of guanine, and is used in acute leukemias (acute granulocytic leukemia).
- Fludarabine: Fludarabine an analog of vidarabine (antiviral drug), is used in CLL and non-Hodgkin’s lymphomas.
- Pentostatin: Obtained from Streptomyces antibioticus inhibits DNA synthesis. It is used in Hairy cell leukemia, other chronic leukemias, and non-Hodgkin’s lymphomas.
- Cladribine: It is considered the drug of choice in hairline cell leukemia and is also useful in CLL, AML, and some lymphomas.
Pyrimidine Antagonists
- Pyrimidine antagonists are converted to active metabolites which resemble natural nucleotides.
- They are taken up into DNA in place of natural nucleotides and inhibit DNA synthesis. 5-fluorouracil (5-FU) is given intravenously and has a short t½ of 10–20 minutes.
- The majority of the drug is metabolized by an enzyme called dihydropyrimidine dehydrogenase (DPD).
- A small percentage of patients lack this enzyme—a pharmacogenetic variation and even therapeutic doses of 5-FU can result in toxicity in them.
- Leucovorin potentiates the antitoxic effects of 5-FU and, therefore, can be administered along with it.
Pyrimidine Antagonists Uses:
Carcinoma of the stomach, colon, rectum, breast, and ovaries.
Topical uses: Fluorouracil ointment is used topically in many precancerous (1% point) and cancerous (5% point) conditions:
- Seborrheic keratosis – Polyps – Solar keratoses
- Warts ( Verrica vulgaris) – Benign skin tumors – Superficial basal cell carcinoma
Cytosine arabinoside or cytarabine:
- Cytosine arabinoside or cytarabine is the most effective agent in acute myeloblastic leukemia.
- It enters the cells and is converted to an active metabolite which inhibits DNA synthesis.
- Cytarabine is used in acute leukemias particularly myeloid leukemia and in relapsed cases of acute lymphocytic leukemia.
Gemcitabine:
- Gemcitabine an analog of cytarabine is similar to it. It is used in pancreatic, lung, cervical, bladder, ovarian, and breast cancers.
- Adverse effects include myelosuppression, nausea, vomiting, thrombocytopenic purpura, and nephrotoxicity.
Natural And Semisynthetic Products
Question 15. Natural agents in the treatment of cancers.
Answer:
Antibiotics
Actinomycin D: Actinomycin D is obtained from the fungus of Streptomyces species. It binds to DNA and inhibits DNA-dependent RNA synthesis and also causes breaks in the DNA.
- It is given intravenously in Wilms’ tumor, rhabdomyosarcoma, choriocarcinoma, and some soft tissue sarcomas, Kaposi’s sarcoma, and Ewing’s tumor. It is also an immunosuppressant and is used in renal transplants.
- Toxic effects include myelosuppression, nausea, vomiting, and dermatological manifestations. Extravasation of the drug can cause local pain.
Anthracycline Antibiotics
Daunorubicin and doxorubicin are vesicants—that cause blisters on the skin and therefore, should be carefully injected to avoid extravasation. They are all metabolized by the liver → ↓ Dose in hepatic dysfunction
Drugs Causes and Curable Cancers:

Anthracycline Antibiotics Mechanism of Action:
Anthracyclines inhibit topoisomerase 2 and also cause breakages in DNA.
Anthracycline Antibiotics Adverse effects:
- Cardiotoxicity with hypotension, tachycardia, arrhythmias, cardiomyopathy, and CCF is unique to both these drugs. Cardiomyopathy is of two types—an acute form with arrhythmias may be seen within 24 hours of administration. Pericarditis, myocarditis, and pericardial effusion may follow.
- Long-term toxicity with CCF and myocardial damage may be seen years after treatment with anthracyclines.
- Anthracyclines also cause vomiting, stomatitis, alopecia, and bone marrow depression. They may color the urine red.

Anthracycline Antibiotics Uses
- Daunorubicin—used in acute leukemias.
- Doxorubicin—in solid tumors, acute leukemias, and non-Hodgkin’s lymphomas.
Epirubicin, idarubicin, valrubicin, and mitoxantrone are anthracyclines that are less cardiotoxic.
Bleomycin: Bleomycin is obtained from Streptomyces verticillus. It binds with iron and generates free radicals and causes breakage in DNA strands.

Bleomycin Advantages:
- The unique mechanism of action
- Less toxic to the bone marrow → advantageous in combination regimens.
Bleomycin Adverse effects:
Pulmonary fibrosis and cutaneous toxicity (dermatographia—scleroderma-like changes) but bone marrow depression is negligible.
Bleomycin Uses:
Solid tumors— testicular tumors, squamous cell carcinoma of the head, neck, and esophagus.
Epipodophyllotoxins
- Etoposide and teniposide bind to topoisomerase II as well as to DNA and result in DNA strand breakages.
- The cells in the S and G2 phases of the cell cycle are susceptible to these drugs.
Epipodophyllotoxins Adverse effects:
Including thrombophlebitis at the site of injection, nausea, alopecia, allergic reactions, and myelosuppression.
Epipodophyllotoxins Uses:
- Etoposide—in germ cell cancers (testicular and ovarian), lung and stomach cancers, leukemias, and lymphomas.
- Teniposide is used in acute lymphoblastic leukemia.
Camptothecins
- Camptothecins—topotecan and irinotecan are obtained from the Chinese tree Camptotheca acuminata. They inhibit topoisomerase I resulting in DNA strand breakages leading to cell death. They act on the S phase of the cell cycle.
- Toxicity—diarrhea, reversible bone marrow suppression, nausea, weakness, and skin rash.
- Irinotecan inhibits the enzyme acetylcholinesterase resulting in the accumulation of acetylcholine causing excessive salivation, abdominal cramps, miosis, bradycardia, and sweating which respond to treatment with atropine.
Camptothecins Uses:
- Topotecan → In advanced ovarian cancer and lung cancer.
- Irinotecan → Metastatic colorectal cancer.
Taxanes
- Paclitaxel is obtained from the bark of the Western yew tree. It binds to the beta-tubulin of microtubules and arrests mitosis—mitotic spindle poison.
- It is metabolized by the liver microsomal enzymes and drugs that induce and inhibit microsomal enzymes can alter the plasma levels of paclitaxel.
Taxanes Adverse effects:
- Including myelosuppression, myalgia, allergic reactions, hypotension, arrhythmias, and peripheral neuropathy.
- The vehicle used to administer paclitaxel can cause allergic reactions. Dexamethasone and diphenhydramine are used to prevent the allergic response.
- A formulation of paclitaxel now available is unlikely to cause allergic reactions and causes less neurotoxicity and myelosuppression.
Taxanes Uses:
- Various solid tumors include breast cancers and ovarian cancers, cancers of the ovary, head and neck, breast, esophagus, and lungs.
- Paclitaxel is incorporated into drug-eluting stents used for coronary angioplasty.
- Docetaxel and cabazitaxel are similar in actions, toxicity, and uses to paclitaxel.
Vinca Alkaloids
Question 16. Short note: Vinca alkaloids.
Answer:
Vinca Alkaloids:
Vincristine and vinblastine are vinca alkaloids obtained from the leaves of vinca rosea, the periwinkle plant. Vinorelbine is a semisynthetic derivative.
Mechanism of action:
- Vinca alkaloids bind to microtubules in the mitotic apparatus and arrest cell division in metaphase.
- They are spindle poisons. They are cell-cycle specific and act on the ‘M’ phase of the cell cycle.
- Vinca alkaloids are metabolized in the liver by microsomal enzymes and excreted through the gut.

Vincristine:
- Vincristine is neurotoxic but bone marrow depression is less. Peripheral neuropathy and mental depression can occur. Autonomic side effects like constipation may need prophylactic laxatives.
- Urinary retention, orthostatic hypotension, nausea, vomiting, alopecia and inappropriate secretion of ADH (SIADH) are reported.
Vincristine Uses:
- Leukaemias, Hodgkin’s lymphoma (MOPP regimen), non-Hodgkin’s lymphoma, breast, lung, and cervical tumors. Vincristine is also used in many pediatric solid tumors like Wilms’ tumor, Ewing’s sarcoma, brain tumor, and rhabdomyosarcoma.
- Vinblastine causes bone marrow depression, alopecia, and vomiting. It is a vesicant and should be injected carefully. It is used with bleomycin and cisplatin (VBC) in testicular tumors; it is also useful in Hodgkin’s and non-Hodgkin’s lymphoma.
- Vinorelbine is a semisynthetic vinca alkaloid used intravenously in lung cancers, breast and ovarian cancers. It can cause bone marrow suppression, nausea, vomiting, and neurotoxicity.
Miscellaneous
- Hydroxyurea is an analog of urea and acts by inhibiting DNA synthesis. It acts on the ‘S’ phase of the cell cycle. It is orally effective, almost completely and rapidly absorbed.
- Adverse effects are myelosuppression, nausea, vomiting, and skin pigmentation. Hydroxyurea is a first-line drug in chronic myeloid leukemia.
L-asparaginase:
- The amino acid asparagine is synthesized by the normal cells but malignant cells are unable to synthesize asparagine and depend on the host for the supply.
- Asparaginase is an enzyme that converts asparagine to aspartic acid and deprives the malignant cells of asparagine supplies resulting in the inhibition of protein synthesis.

Asparaginase is used in acute leukemias. Hypersensitivity reactions are common as it is a foreign protein (obtained from E. coli); it can cause Hemorrhage due to inhibition of clotting factors.
Hepatotoxicity with raised serum transaminases and pancreatitis. Inhibition of insulin synthesis may result in Hyperglycemia. It also causes nausea, vomiting and CNS depression. Bone marrow suppression and effects on GI epithelium are mild and it does not cause alopecia.
Protein Tyrosine Kinase Inhibitors
Imatinib:
- Imatinib dasatinib and nilotinib act by inhibiting some tyrosine kinases which are involved in the pathogenesis of chronic myeloid leukemia.
- They are effective orally and metabolized by microsomal enzymes—CYP3A4—should be used cautiously to avoid drug interactions.
- Adverse effects are skin rashes, nausea, vomiting, muscle cramps, edema and elevated liver enzymes.
Imatinib Uses:
- Imatinib is the drug of choice in chronic myeloid leukemia.
- Imatinib is also used in gastrointestinal tumors that express tyrosine kinase.
- Dasatinib is effective in imatinib-resistant CML and Philadelphia chromosome positive acute lymphoblastic leukaemia.
Other Anticancer Drugs
Thalidomide:
- Thalidomide is useful in the treatment of multiple myeloma—may act by stimulation of T cells and natural killer cells, inhibition of angiogenesis and tumor cell proliferation, and modulation of hematopoietic stem cell differentiation.
- Sedation, constipation, peripheral neuropathy, and carpel tunnel syndrome are the adverse effects. Thromboembolic events are rare.
Lenalidomide: Lenalidomide is a derivative of thalidomide which is more potent and safer than it.
Monoclonal antibodies:
- Cancer cells express several antigens which may be targeted by monoclonal antibodies.
- Many monoclonal antibodies are now available for the treatment of lymphomas and solid tumors.
Rituximab:
- Rituximab targets the CD20 antigen on the B cells causing lysis of these cells. It is effective in B cell lymphomas and CLL.
- It is synergistic with chemotherapy because rituximab sensitizes the lymphoma cells so that they are susceptible to the apoptotic effects of chemotherapy.
- It can cause infusion reactions and rarely dermatological toxicity.
Some antigens, Monocol antibodies, and their indications in cancer:
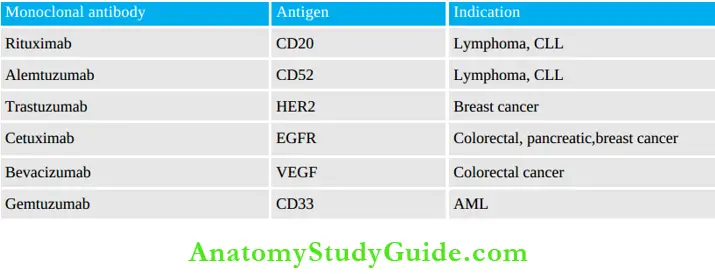
Alemtuzumab:
- Alemtuzumab binds to the CD52 antigen on B and T cells causing cell death in lymphomas and CLL.
- Since CD52 antigen is also expressed on normal neutrophils and lymphocytes, infections as expected can be quite serious particularly if the patient is already immunosuppressed due to chemotherapy. Allergic reactions are common.
Trastuzumab:
- Trastuzumab is a humanised antibody against HER2 receptors. These HER2 receptors which belong to EGF family of receptors are overexpressed in breast cancer cells and are involved in resistance to chemotherapy.
- Trastuzumab can directly induce the death of breast cancer cells. It is used along with chemotherapy in (HER2 positive) breast cancers and stomach cancer. Allergic reactions and cardiac dysfunction have been reported.
Cetuximab:
Cetuximab panitumumab: Several epithelial cell cancers including colorectal cancer, breast, lung, kidney, prostate, pancreas, brain as well as head and neck cancers have shown an overexpression of these epidermal growth factor receptors.
Cetuximab and panitumumab:
Cetuximab and panitumumab are monoclonal antibodies targeting the EGFR and are approved for the treatment of EGFR-positive metastatic colorectal cancer.
Bevacizumab:
- Vascular endothelial growth factor (VEGF) is an angiogenic growth factor that controls the growth of new blood vessels. VEGF receptors are present in large numbers in the tumor.
- Bevacizumab targets VEGF, prevents the binding of VEGF to its receptors, and thereby suppresses tumor growth.
- Bevacizumab is the first-line treatment for metastatic colorectal and lung cancer along with chemotherapy and in breast and cervical cancers.
Hormones In Cancer Chemotherapy
Question 17. Discuss briefly the use of hormones in cancer chemotherapy.
Answer:
Glucocorticoids:
- Due to their lymphocytic action, glucocorticoids are used in acute leukemias and lymphomas.
- Rapid clinical improvement is seen but duration can vary from 2 weeks to 9 months.
- They are used for the initiation of therapy due to their rapid action. Prednisolone and dexamethasone are commonly used.
Glucocorticoids are also of value in the following:
- Radiation therapy to reduce radiation edema.
- In intracranial tumors to reduce cerebral edema.
- For symptomatic relief in critically ill patients.
Estrogens:
- Estrogens are physiological antagonists of androgens. Hence they are useful in prostatic carcinoma as it is an androgen-dependent tumor.
- Fosfestrol is a prodrug of estrogen—gets converted to stilbestrol in prostatic tissue. It has another advantage that it attains high concentration in the prostate. Hence it is preferred in prostatic cancer.
Progestins: Progestins are useful in the palliative management of endometrial carcinoma.
Androgens: Androgens are used in the palliative treatment of breast cancer in postmenopausal women along with oophorectomy.
Hormone Antagonists
Aromatase inhibitors:
The enzyme aromatase catalyzes the conversion of androgens to estrogens.
Exemestane, anastrozole, and letrozole are aromatase inhibitors effective in breast cancers.
- Aminoglutethimide and trilostane inhibit the conversion of cholesterol to pregnenolone (the first step in corticosteroid synthesis) and thereby inhibit the synthesis of adrenocorticoids.
- Octreotide: A somatostatin analog, is useful to reduce the secretion of growth hormone, insulin, glucagon, and peptide hormones in carcinoid tumors and islet cell carcinomas of the pancreas.
- Antioestrogens: Tamoxifen is an estrogen receptor antagonist used in estrogen receptor-containing breast cancer.
- Fulvestrant: Fulvestrant is a SERD used in ER-positive breast cancer. It downregulates the estrogen receptors and is effective even in those resistant to tamoxifen.
- GnRH analogs: Long-term administration of leuprolide, goserelin, and buserelin are useful in prostatic and breast cancers. They may be combined with tamoxifen in breast cancers.
- Estramustine: Estramustine is a molecule containing both estradiol and nitrogen mustard. It is useful in prostatic cancers which do not respond to estrogens.
- Adverse effects are similar to that of estrogen administration.
Antiandrogen: Flutamide and bicalutamide are used in prostatic cancer.
Radioactive Isotopes
Some radioactive isotopes can be used in the treatment of certain specific cancers.
- Radiophosphorus: Radiophosphorus P32 is used in polycythemia vera. It is taken up by the bone where it emits beta rays and has a half-life of about 14 days.
- Strontium chloride: Strontium chloride emits beta rays and has a longer t½ in the bony metastases—used to reduce pain in bony metastases.
- Radioactive iodine: Radioactive iodine 131I is used in the treatment of thyroid cancers.
Biological Response Modifiers
Several agents are used to beneficially influence the patient’s response to treatment and to overcome some adverse effects. These have also been termed biological response modifiers.
They are as follows:
- Hematopoietic: Hematopoietic growth factors like erythropoietin and myeloid growth factors like GM-CSF, G-CSF, M-CSF, and thrombopoietin are used to treat bone marrow suppression.
- Interferons: Interferons like interferon alpha are used in hairy cell leukemia, Kaposi’s sarcoma, and condylomata acuminata.
- Aldesleukin: Aldesleukin is recombinant interleukin 2: It increases the cytotoxic activity of T cells, induces the activity of natural killer cells, and also induces interferon production. It is useful in inducing remission in renal cell carcinoma. Hypotension is the most troublesome side effect.
- Tretinoin: Tretinoin (all-trans retinoic acid) induces differentiation in leukemic cells and the leukemic promyelocytes loose their ability to multiply. It is useful to induce remission in acute promyelocytic leukemia.
- Amifostine: Amifostine provides selective protection to normal tissues from the effects of cytotoxic drugs.
- Amifostine activates: Amifostine activates an enzyme in the normal tissues which can inactivate the active form of cisplatin and radiation. It has also been shown to stimulate the bone marrow in some bone marrow disorders.
The salient features of commonly used anticancer drugs is given in.
Salient features of some commonly used anticancer drugs:


Antiseptics And Disinfectants
Disinfection:
- Disinfection is the destruction of all pathogenic organisms but not spores. If spores are also killed, it is called sterilization.
- A disinfectant is used on inanimate objects.
Antiseptic:
- Antiseptic is an agent that destroys microorganisms and can be used on living tissues.
- The term germicide can be used for either drug. Germicides are widely used in domestic products like soaps, toothpaste and aftershave lotions.
Antiseptics And Disinfectants Classification:
- Acids: Boric acid, benzoic acid
- Alcohols: Ethanol, isopropyl alcohol
- Aldehydes: Formaldehyde, glutaraldehyde
- Surfactants: Soaps, benzalkonium, cetrimide, cetylpyridinium chloride, dequalinium chloride
- Phenol derivatives: Phenol, cresol, resorcinal, chlorhexidine, chloroxylenol, hexachlorophene
- Halogens: Iodine, iodophors, chlorine, chloramines
- Oxidizing agents: Hydrogen peroxide, benzoyl peroxide, potassium permanganate
- Dyes: Gentian violet, methylene blue, brilliant green, acriflavine, proflavine
- Metallic salts: Mercurial compounds, silver nitrate, zinc compounds
Antiseptics And Disinfectants Mechanism of action: Germicides may act by the following mechanisms—
- Oxidation of bacterial protoplasm
- Denaturation of bacterial proteins
- Detergent like action
- Competition with essential substrates for the important enzymes in the bacterial cell.
An ideal germicide should have a wide antibacterial spectrum, should be chemically stable, should have rapid action, nonirritating to the tissues, and not interfere with wound healing activity even in the presence of pus, exudates, and tissue degradation products; it should not be absorbed into systemic circulation.
Acids
Boric acid and sodium borate (borax):
- Boric acid and sodium borate have weak bacteriostatic and fungistatic activity.
- Aqueous solutions of boric acid are used for irrigating eyes, bladder, vagina, and large wounds.
Benzoic acid:
Benzoic acid is an antibacterial (below pH 5) and antifungal agent used as a preservative in the laboratory.
Salicylic acid:
- Salicylic acid has bacteriostatic, fungicidal, and keratolytic properties.
- It is used as a dusting powder or 2% ointment for seborrhoeic dermatitis, warts, and corns. 6%, 12%, 18% and 24% point
Alcohols
Ethyl alcohol:
- Ethyl alcohol is used as an antiseptic at 60–90% concentration.
- The antiseptic activity decreases above 90%. It rapidly denatures the bacterial proteins.
Ethyl alcohol Disadvantages:
- Poor activity against spores, some viruses and fungi.
- Irritant → Causes burning when applied on open wounds
- Alcohols are flammable—should be allowed to evaporate before using cautery or laser surgery.
Ethyl alcohol Uses: To clean the skin before injections and surgeries.
- Isopropyl alcohol is more potent and more toxic than ethanol.
- It is used in 68–72% concentration as skin antiseptic.
Aldehydes
- Formaldehyde is a gas at room temperature used for fumigation; the 40% aqueous solution is noncorrosive and has a broad antimicrobial spectrum.
- It has a pungent odor and is an irritant— highly irritating to respiratory mucous membranes and eyes.
- Formaldehyde is also a carcinogen and Occupational Safety and Health Administration (OSHA) has set standards to limit exposure of healthcare workers to formaldehyde.
Aldehydes Mechanism of action:
Aldehydes alkylate chemical groups in proteins and nucleic acids.
Aldehydes Uses:
Formaldehyde gas:
- For fumigation and for sterilizing instruments which cannot be moistened with solution.
- Formaldehyde 40% solution (100% formalin) in water: Disinfection of surgical instruments and gloves, embalming and preservation of tissues, fibreoptic endoscopies, respiratory therapy equipment, hemodialysis, and dental handpieces that cannot withstand high temperatures of steam sterilization are disinfected.
- Automatic circulating baths are used which increase penetration of aldehyde solution into the instruments and decrease operator exposure to the chemical.
- Glutaraldehyde is a dialdehyde used as a 2% solution. It is bactericidal, sporicidal, fungicidal and viricidal.
- pH should be between 7.4 and 8.5. It is less irritant than formaldehyde; has greater sporicidal activity; does not damage lenses and cementing material in endoscopes.
- Glutaraldehyde is superior to formaldehyde for sterilizing rubber, plastic, and metal appliances. 2% solution is used for local application in idiopathic hyperhidrosis of palms and soles.
Surfactants
- Surfactants are chemicals that lower the surface tension of solutions and are termed detergents.
- They may be anionic, cationic, ampholytic surfactants, or polysorbates.
Anionic surfactants: For example, soap.
- Dissociate in aqueous solutions to form large and complex anions which lowers the surface tension.
- Effective for gram-positive and acid-fast organisms.
- Microorganisms are enmeshed in the lather and washed away on rinsing.
- Have a narrow spectrum; precipitate in hard water; cause drying of the skin.
Cationic surfactants:
For example, benzalkonium chloride, cetrimide, cetylpyridinium chloride, and dequalinium chloride. Cationic surfactants dissociate into large cations.
They are:
- Active against gram-positive and gram-negative organisms (less active against spores, viruses, and fungi)
- Most effective in neutral solution
- Non-irritating and safe
- Incompatible with anionic surfactants
- Absorbed by cotton and rubber
- One of the most commonly used germicidal agents.
Benzalkonium chloride: Benzalkonium chloride has an aromatic odor and is soluble in water.
Benzalkonium chloride Uses:
- 1:1,000 solution for cleansing skin
- 1:2,000 for mucous membranes and denuded skin
- 1:20,000 for irrigation of the bladder and urethra
- 1:1,000–4,000 for storing sterilized surgical instruments but instruments should be thoroughly washed before use.
Cetrimide:
- Cetrimide 1% solution is used like above. It is also used as a cream. It is very effective for cleaning wounds.
- In combination with chlorhexidine is one of the most popular antiseptics.
Savlon:
- Savlon is cetrimide 3% + chlorhexidine. Salvon causes irritation to the eyes and rarely the skin. Allergic reactions can also occur.
- Hence Salvan should be wiped off the skin after application.
- Accidental exposure of the eyes to Salvon can cause intense burning, pain, and abrasions of the cornea and conjunctiva.
- It should be immediately washed off followed by a few days of prednisolone eye drops to suppress inflammation under the supervision of an ophthalmologist.
Dequalinium chloride: Dequalinium chloride is used in gum paints and lozenges.
Cetylpyridinium chloride: Cetylpyridinium chloride is used in mouthwashes and lozenges.
Phenol Derivatives
Phenol:
- Phenol is one of the oldest antiseptics introduced by Lord Lister in 1867. It is bactericidal and fungicidal but has poor action against spores and viruses. It acts by denaturing bacterial proteins. It also has a mild local anesthetic action.
- Phenol rapidly penetrates even intact skin and mucous membranes. It is a protoplasmic poison.
- Phenol is extremely irritant to exposed tissues (corrosive)—when swallowed, it burns buccal, esophageal, and gastric mucous membrane.
Phenol Uses:
Phenol is used to disinfect the urine, feces, and sputum of patients and is sometimes used as an antipruritic because of its local anesthetic action.
Cresol:
Cresol is methyl phenol which is as toxic as phenol but is more active. It is used as a disinfectant for utensils and excreta.
Lysol:
Lysol is cresol with soap solution. It has higher antiseptic activity and is a useful disinfectant for hospital and domestic use.
Chloroxylenol:
- Chloroxylenol is a less toxic chlorinated phenol, effective against gram-positive and gram-negative organisms.
- Surgical Dettol contains 1.4% of chloroxylenol for skin; 6.25% for instruments and 1–3% in antiseptic cream. Dettol liquid (13%); obstetric cream (1.4%).
Hexachlorophene:
- This chlorinated phenol acts by inhibiting bacterial enzymes and causing lysis. It is effective mainly against gram-positive organisms and has weak action against gram-negative organisms.
- It is odorless and nonirritating to use on the skin. It is used in soaps for surgical scrubbing, for cleaning the skin in obstetrics, carbuncles, and seborrhoeic dermatitis.
- It may cause allergic reactions. It also reduces body odor by preventing bacterial decomposition of organic material and therefore, is used as a deodorant.
- In the USA, hexachlorophene was used to wash newborn babies which resulted in brain damage in such babies, and, therefore, the use of >3% hexachlorophene is banned.
Chlorhexidine:
- Chlorhexidine is effective against gram-positive, gram-negative organisms and fungi. It is rapid acting and nonirritating.
- Salvon chlorhexidine + cetrimide.
Halogens
Iodine: Iodine is one of the oldest antiseptics. It has a broad spectrum of activity, is a powerful bactericidal, sporicidal, fungicidal, and viricidal agent. The activity is inhibited by organic material but enhanced by alcohol.
Iodine Disadvantages:
- It is irritating, painful, stains the area, and may delay wound healing.
- Rashes, fever, and generalized skin eruptions may develop in some patients who are sensitive to iodine.
Prolonged systemic use causes iodism.
Iodine Uses:
- Tincture iodine (I2 in KI + alcohol) is used to clean the skin before surgery.
- Iodine crystals are used to sterilize water for soaking vegetables and cleaning before use.
- Mandl’s paint (compound iodide paint) is used in the treatment of tonsillitis and pharyngitis.
- Iodine ointment as a fungicide in ringworm. Iodides have no antibacterial action.
Iodophors:
- Iodophors are soluble complexes of iodine with surfactants like detergents.
- The detergents serve as carriers and slowly release iodine, for example, Povidone iodine—5% solution; iodine—10% solution, betadine 10% paint, 5% point, cream.
Iodophors Advantages:
Iodophors are nonirritating, nonstaining, water-soluble, less toxic, and nonsensitizing to the skin.
Iodophor Uses:
Used for preoperative scrubbing, skin preparation, disinfection of instruments, and as a local antiseptic in boils, furunculosis, burns, ulcers, ringworm, and in oral/vaginal moniliasis.
Chlorine:
- Chlorine is a potent germicide and is bactericidal against several gram-positive and gram-negative organisms in a very low concentration (0.1 PPM in 30 seconds). It also destroys protozoa and viruses.
- The antibacterial activity of chlorine is reduced in the presence of organic matter since they bind chlorine and therefore, need a higher concentration of free chlorine.
Chloramines are compounds that release chlorine slowly.
- Chlorinated lime (bleaching powder) is obtained by the action of chlorine on lime. It is used for disinfection of water in swimming pools and water for drinking.
- Chloramine is an organic chloride. The freshly prepared solution is used for mouthwash, irrigating the bladder and urethra.
- Eusol is a solution of chlorinated lime with boric acid.
Oxidizing Agents
Hydrogen peroxide:
- Hydrogen peroxide is a colorless and odorless liquid. It liberates nascent oxygen when applied to tissues and then oxidizes bacteria and necrotic tissue.
- On application, there is effervescence and this helps in removing tissue debris, ear wax, etc.
- Hydrogen peroxide has poor penetrability and the action is of short duration. On keeping, it loses its potency. It is also a deodorant.
Hydrogen peroxide Uses:
- Hydrogen peroxide is used for cleansing wounds, abscesses, and irrigation. In dentistry, it is used to clean septic sockets and root canals and also as a mouthwash and deodorant gargle.
- It is used as ear drops while removing ear wax.
Potassium permanganate:
- It is an oxidizing agent and an astringent. The purple crystals are water-soluble. It acts by liberating oxygen which oxidizes bacterial protoplasm.
- Organic matter reduces its activity and the solution gets decolorized.
- It promotes rusting; the concentrated solution is caustic and causes burns and blistering.
Hydrogen peroxide Uses
- 1:4,000–1:10,000 solution used for gargling, irrigating cavities, urethra, and wounds.
- For stomach wash in alkaloidal poisoning (except atropine and cocaine).
- 1% solution in mycotic infections like athlete’s foot.
- 5% solution as a styptic.
- Topically to oxidize venom in case of snake and scorpion bite.
- To purify well water.
- To disinfect vegetables and fruits.
Dyes:
Gentian violet:
- Gentian violet (aniline dye, crystal violet, or medicinal gentian violet) is effective against gram-positive organisms and fungi. Staining is the only disadvantage.
- It is a nonirritant and potent antiseptic. 0.5–1% solution is used topically on furunculosis, burns, boils, chronic ulcers, infected eczema, thrush, ringworm, and mycotic infections of the skin and mucous membranes.
Brilliant green:
Actions are similar to gentian violet. It is used as a 0.5–1% solution in the treatment of burns, impetigo, and infected wounds like gentian violet.
Methylene blue: Methylene blue is used systemically in cyanide poisoning as it converts methemoglobin to hemoglobin.
Acriflavine and proflavine:
- Acriflavine and proflavine are acridine dyes active against gram-positive bacteria and gonococci (proflavine is better).
- They are nonirritant; efficacy is unaffected by organic matter but is increased in an alkaline medium; 1:1,000 solution is used in infected wounds and burns, 2% pessary in vaginitis and cervicitis.
Triple-dye lotion: Triple-dye lotion contains gentian violet 0.25% + brilliant green 0.25% + acriflavine or proflavine 0.1%—it is used in burns dressing.
Metallic Salts
- Silver compounds have antiseptic, astringent, and caustic properties.
- Silver nitrate kills microbes rapidly and the action is prolonged due to the slow release of silver ions from silver proteinate that is formed by interaction with tissue proteins.
- The reduced silver gets deposited and stains the
tissues black. - Silver nitrate is used for the prophylaxis of ophthalmia neonatorum.
Silver sulfadiazine:
- Silver sulfadiazine is active against.
- Pseudomonas is used in burn wounds.
Colloidal silver:
- Colloidal silver is a compound that slowly releases silver.
- They are non-corrosive, nonirritant, nonastringent and have better penetrability, and are used as nasal and eye drops.
Zinc salts:
- Zinc salts like zinc oxide have astringent and mild antiseptic properties.
- Zinc oxide is used as an ointment or lotion in eczema, impetigo, and psoriasis.
Mercury:
- Mercury compounds act by inhibiting the sulphydryl enzymes of bacteria.
- They are bacteriostatic and are poor antiseptics—not commonly used.
Leave a Reply