Coccidian Parasites
- Toxoplasma gondii
- Sarcocystis lindermanii
- Cryptosporidium parvum
- Cyclospora cayetanensis
- Cystoisospora belli
Read And Learn More: Micro Biology And Immunology Notes
Table of Contents
Toxoplasma Gondii
Life Cycle
- Worldwide distribution, infects a wide range of animals.
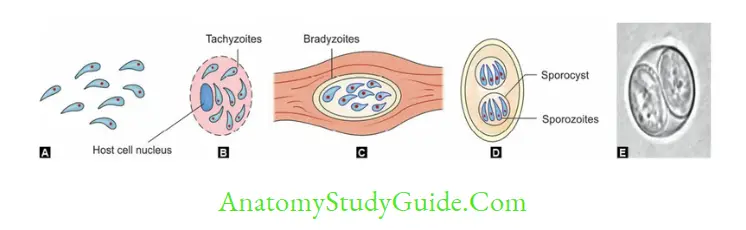
- Three morphological forms: Sporulated oocyst (sexual form, found in cats), crescentic tachyzoite (actively multiplying form), tissue cyst containing bradyzoites (found in muscle and viscera)
- Infective form: All three morphological forms are infectious
- Definitive hosts are cats and other felines
- Intermediate hosts are man and other mammals (goat, sheep)
- Transmission:
- Ingestion of tissue cyst containing bradyzoites from undercooked meat (most common route)
- Ingestion of sporulated oocysts from contaminated soil, food, or water
- By blood transfusion, needle stick injuries, organ transplantation, transplacental transmission, or laboratory accidents-Tachyzoites are the infective form.
- Sporulated oocyst transforms into tachyzoites which multiply actively in blood, then finally transform into tissue cysts containing the bradyzoites (resting stage) which get deposited in various organs like the brain, skeletal and cardiac muscles, eye, and liver to form tissue cysts.
Epidemiology
Toxoplasmosis is one of the most common parasitic zoonotic infections affecting a wide range of mammals and birds.
Prevalence
- Global prevalence is about 25–30%. The world is divided into:
- Low seroprevalence (10–30%): Observed in North America, Southeast Asia, North Europe, and Sahelian countries of Africa
- Moderate prevalence (30–50%): Found in countries of Central and Southern Europe.
- High prevalence (>50%): Has been found in Latin America and tropical African countries.
Various Risk Factors for Infection
- The geographical area (cold area, hot arid climatic conditions, high altitudes are associated with a low prevalence)
- Age: It commonly affects the elderly and fetus
- Exposure to cat and cat’s feces
- Food habits: Ingestion of uncooked cat and other animal meat (seen in countries like France)—at higher risk
- Immune status: Patients associated with HIV, malignancies, and other immunocompromised conditions are at high risk
- Patients undergoing blood transfusion, and organ transplantations are at higher risk
- Genetic factor: HLA DQ3 is associated with encephalitis in AIDS patients and hydrocephalus in fetuses infected with Toxoplasma, whereas HLA DQ1 appears to be protective.
Clinical Features
Congenital toxoplasmosis:
- 1st Trimester: The incidence of transplacental infection is lowest (15%), but the disease in the neonate is most severe.
- 3rd Trimester: The incidence of transplacental infection is maximum (65%), but the infant is usually asymptomatic at birth.
- If the Mother is previously infected: the Fetus is asymptomatic.
- Incidence: Approximately 1 per 1000 live births.
- The classical triad comprises chorioretinitis, hydrocephalus, and intracranial calcifications
- Other manifestations include stillbirth, psychomotor disturbance, and microcephaly
- Ocular involvement: Eyes are involved later in life (2nd-3rd decade) when the cysts rupture
- Most common manifestation is chorioretinitis
- Diagnosis:
- IgM detection in fetal blood, IgA can also be used (experimental but better sensitivity)
- Toxoplasma Ag in amniotic fluid, PCR to detect Toxoplasma genes.
- Adult: Mostly asymptomatic, most common manifestation – Cervical LN↑
- In HIV pt:
- Association rate 15–40%.
- MC manifestation encephalitis
- MC site involved: Brainstem, basal ganglia, pituitary gland and corticomedullary junction
- Occurs when CD4 < 100/µl
- Other manifestations: Pulmonary infections and chorioretinitis.
Diagnosis
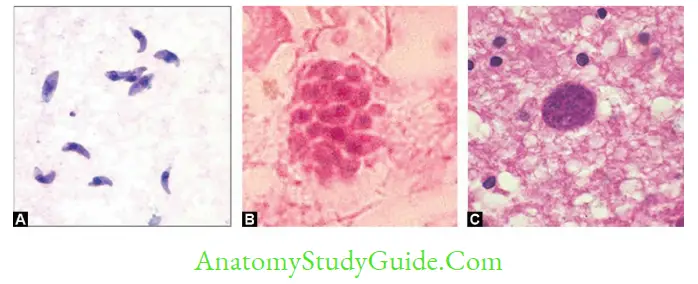
- Direct microscopy—detect tachyzoites (coma-shaped) in blood, body fluids, CSF, bone marrow aspirate, BAL, and tissue cyst in tissue biopsy:
- Giemsa, PAS, silver stains, immunoperoxidase stain
- Direct fluorescent antibody test (DFA).
- Antibody detection
- Detection of IgG in serum (ELISA, IFA)—four-fold rise indicates recent infection
- Detection of IgM in serum by ELISA, IgM-IFA (indirect immunofluorescence antibody), and IgM immunosorbent agglutination assay (IgM-ISAGA)—marker of acute and congenital infection
- IgG avidity test by ELISA, ELFA (enzyme-linked immunofluorescence assay)— low avidity indicates recent infection
- Detection of IgA in serum (ELISA or IgA-ISAGA)—useful for acute and congenital infection
- Detection of IgE in serum—useful for acute and congenital infection
- Sabin-Feldman dye test—specific, but cannot differentiate recent and past infection.
- Detection of Toxoplasma antigen—ELISA; useful in situations where antibodies are low like immunocompromised, early acute stage or monoclonal gammopathies.
- Molecular diagnosis (e.g. PCR)— useful for diagnosis (for acute, congenital infection) and for genotyping.
- Animal inoculation—intraperitoneal inoculation into mice.
- Tissue culture—murine alveolar and peripheral macrophage cell line.
- Imaging methods—CT and MRI to detect Toxoplasma encephalitis.
Treatment
- Immunocompetent patients: Do not require specific treatment. Patients with ocular toxoplasmosis are usually treated for 1 month with promethazine plus either sulfadiazine or clindamycin and sometimes with prednisolone.
- Congenital toxoplasmosis: Neonates with congenital toxoplasmosis are treated with daily oral promethazine (1 mg/kg) and sulphadiazine (100 mg/kg) with folinic acid for 1 year.
- Toxoplasmosis during pregnancy: Spiramycin is DOC.
- HIV +ve patients Co-trimoxazole: DOC. Dapsone-pyrimethamine, atovaquone with or without promethazine can be given as alternate
- Primary Prophylaxis:
- Started in AIDS patients with Toxoplasma CD4 <100/µL
- Discontinued if response to ART and CD4>200/µL for 3 months
- Secondary Prophylaxis (Long-Term Maintenance Therapy):
- Started if the CD4 < 200/µL.
- Discontinued if pt asymptomatic, CD4 + T > 200/µL for 6 months.
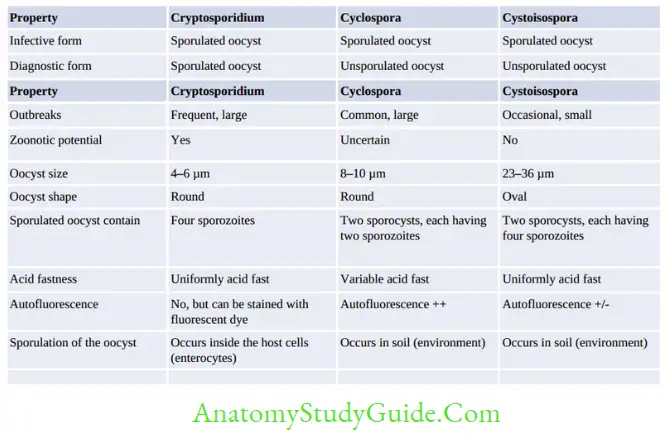
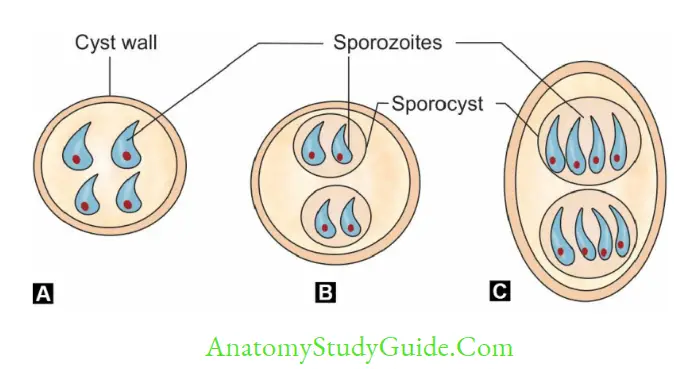
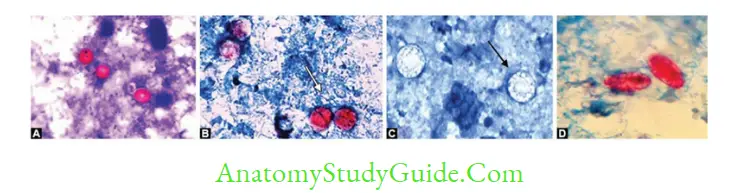
Comparison Of Coccidian Parasites Causing Diarrhea In Immunocompromised Host
Leave a Reply