Conservative Endodontic Therapy In Primary Teeth Introduction
A complete history of the patient, thorough clinical examination, and investigations can help in identifying the stage of inflammation of the pulp.
Table of Contents
The modes of treatment are possible depending upon the extent of pulpal pathology, which is as follows:
1. Conservative endodontic therapy: Indicated when the pulp is healthy or reversibly inflamed. The treatment objective is to restore the vitality of the pulp.
2. Radical endodontic therapy: Indicated when the pulp is irreversibly inflamed or necrosed. The treatment objective is to amputate the pulp in toto or to completely remove its fragments and eliminate the purulent focus.
Read And Learn More: Paediatric Dentistry Notes
3. Extraction: Indicated in the following cases when
- The first two modes cannot eliminate the focus of infection
- Extensive bone loss
- The tooth surface is grossly carious and it cannot be rehabilitated after endodontic therapy
Conservative endodontic therapy includes the following procedures:
- Indirect pulp capping
- Direct pulp capping
- Pulpotomy
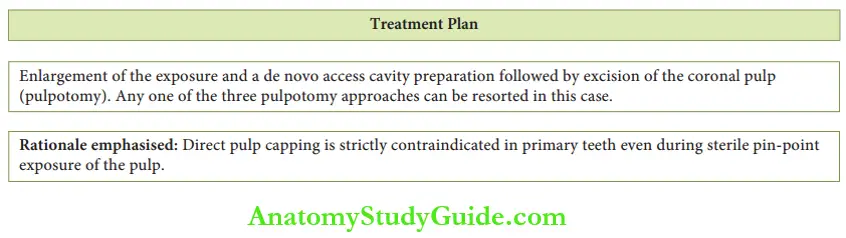
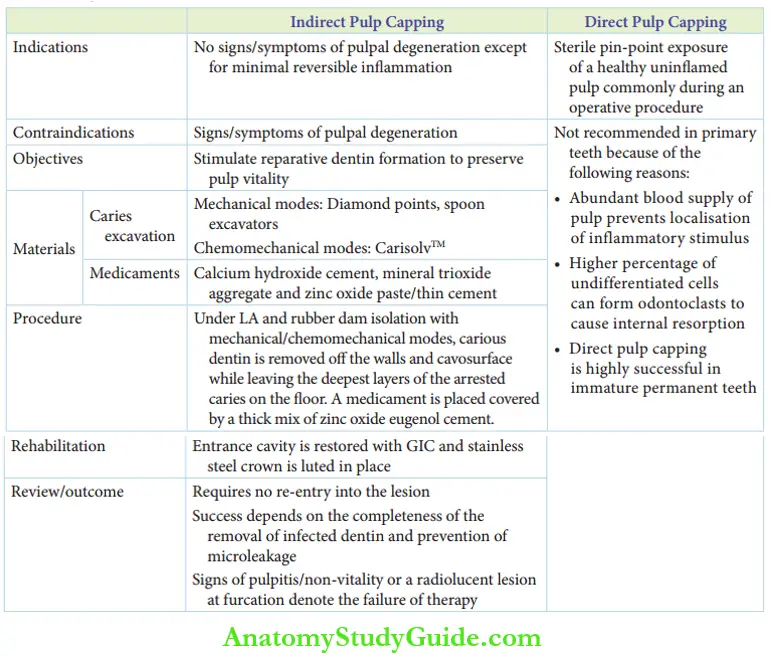
Of these, indirect pulp capping and pulpotomy procedures are performed in primary teeth. Direct pulp capping is contraindicated in primary teeth.
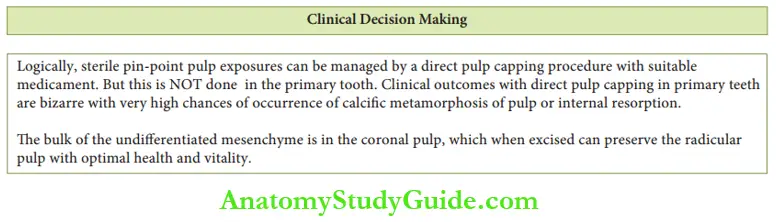
Direct pulp capping is the mode of management of a sterile pin-point exposure of a healthy uninflamed pulp, most commonly during an operative procedure. It is successful in young permanent teeth.
Direct pulp capping is not recommended on primary teeth because of the following reasons:
1. The abundant blood supply in primary teeth contributes to a quicker inflammatory response. Localization of the inflammatory stimulus does not take place. It leads to progressive inflammation of the pulp.
2. The percentage of undifferentiated mesenchymal cells is high in primary teeth. Thy diffrentiate into odontoclasts and cause internal resorption. Hence, a pulpotomy is indicated in case of sterile pin-point exposure of the primary pulp.
Indirect Pulp Capping
Indirect pulp capping is a mode of managing deep carious lesions with no signs or symptoms of pulpal degeneration.
This procedure involves a near-to-complete removal of caries. The deepest layer of carious dentin is not removed.
This remaining layer is covered by a biocompatible material which is expected to fulfill certain requirements, which are as follows:
It should be able to form a film base against which restorative material can be compacted.
It should be a stable, relatively non-porous base to hinder the ingress of microorganisms.
It should be bactericidal to the residual microorganisms.
It should stimulate the odontoblasts in the pulp to secrete tertiary dentin. This tertiary dentin is also called reparative dentin.
Indirect Pulp Capping Rationale
The deepest layer of dentin is left behind to avoid pulpal exposure and further trauma to the tooth. Complete caries excavation is mandatory on the walls of the cavity and at the dentin enamel junction.
This is to obtain an optimal seal between the tooth and restorative material and prevent microleakage. The affected dentin is hard and discolored while the infected dentin is soft and mushy.
The infected dentin has to be completely removed. It is necessary that the dentin left behind on the pulpal floor or the axial walls is affected dentin.
The biocompatible material stimulates secondary dentin formation. This increases the distance between the pulp organ and the carious lesion, thus preserving pulp vitality.
An optimal seal without microleakage will provide the inflamed pulp with a greater opportunity to heal.
Indirect Pulp Capping Indications And Contraindications
The indications of direct pulp capping are as follows:
- A tooth with no signs/symptoms of pulpal degeneration
- The tooth with minimal reversible inflammation of the pulp
- Carious tooth where complete excavation of caries can expose the pulp
The treatment is contraindicated in teeth with signs and symptoms of pulpal degeneration such as spontaneous or persistent pain, tenderness on percussion, abscess, and tooth mobility.
Indirect Pulp Capping Objectives
The objectives of the indirect pulp capping method of deep caries management include the following:
- Arresting the carious lesion
- Promoting dentin sclerosis – closure of open or cut dentinal tubules
- Stimulating the formation of tertiary dentin (reparative dentin)
- Remineralizing the carious lesion
- Preserving pulp vitality
Indirect Pulp Capping Materials
Two different sets of instruments are required for indirect pulp capping. One set consists of materials used for caries excavation.
The other set contains materials used for the pulp capping procedure.
1. Materials used for caries excavation:
Caries excavation/removal can be done with rotary instruments, hand instruments, or chemical agents.
- Rotary instruments: Round diamond burs on an aerator handpiece can be used for the gross removal of caries. Round burs mounted on an air-motor handpiece can be used for the precise removal of caries. This is a quicker mode of caries removal.
- Hand instruments: Small and sharp spoon-shaped excavators complying with the conventional form of the cavity are very useful and efficient in caries removal.
- Chemical agents: CarisolvTM is a gel developed by the Medi team, in Sweden. It contains three amino acids, namely lysine, leucine, and isoleucine. It also contains a low concentration of sodium hydroxide and sodium hypochlorite.
Although the rotary and hand instruments are useful and efficient in removing caries, they remove the affected dentin as well as the sound dentin along with the infected dentin.
There is also a risk of iatrogenic pulp exposure during excavation.
They are relatively more distressing modes that demand the administration of local anesthesia. Hence, the ideal mode of caries removal is a chemomechanical mode.
CarisolvTM gel is applied to the carious tooth for 30–60 seconds. It softens the infected dentin leaving the afflicted/sound dentin unaltered.
The lesion looks frothy on softening of the infected dentin. The softened infected dentin can be scooped out with an excavator (provided with the system) with very minimal pressure application.
The gel may be applied again until no froth appears. As the method uses a chemical agent and an excavator, it is described as a chemomechanical mode of caries removal.
2. Materials used for pulp capping:
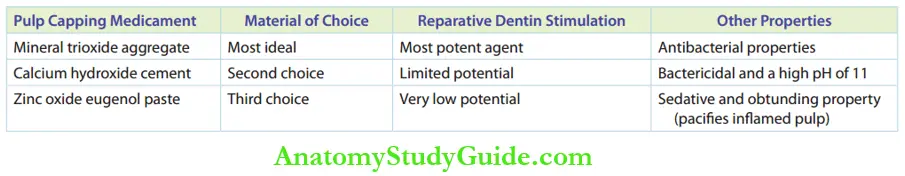
The materials used as pulp capping medicaments are calcium hydroxide cement, mineral trioxide aggregate (MTA), and zinc oxide eugenol paste.
These materials have antibacterial properties. They sedate the pulp and have the potential to stimulate reparative dentin formation.
The table compares the properties of the pulp capping medicaments.
Comparison Between Commonly Used Pulp Capping Medicaments
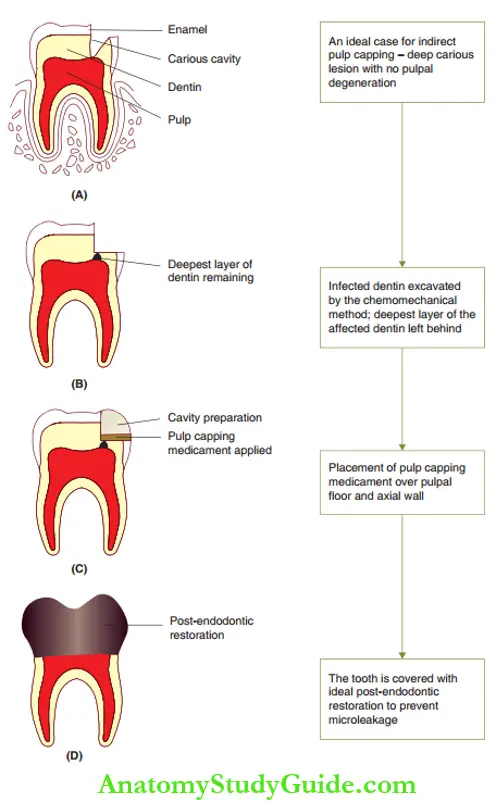
Indirect Pulp Capping Procedure
Indirect pulp capping is a technique done under local anesthesia and rubber dam isolation. It was earlier performed as a two-step procedure.
The chemomechanical or mechanical mode of caries removal is usually preferred.
Carious dentin is excavated from the walls of the cavity. The deepest layer of carious dentin is left behind. Carious enamel at the cavosurface may require rotary instrumentation for removal.
The pulp capping medicament is placed over the pulpal floor and the axial walls. A thick mix of zinc oxide eugenol cement is placed over the medicament.
This zinc oxide eugenol cement forms a temporary restoration of the cavity. After 6 weeks, the lesion is re-entered.
The medicament and the decay are removed entirely. This is followed by a repeat medicament base and a permanent amalgam restoration or stainless steel crown.
The objective was to remove the decay (micro-organism) completely and avert the risk of microbial activity below the restoration.
Current researchers do not favor re-entering the treated lesion after 6 weeks because the number of viable acidogenic bacteria left on the affected dent is few.
These viable bacteria will be inactive as the nutrient supply shall be sealed by an adequate restoration.
So, indirect pulp capping is a single-visit treatment procedure in the current practice. A permanent restoration is placed after a thick mix of zinc oxide eugenol cement.
A stainless steel crown is the ideal post-endodontic restoration. It is the best way to prevent microleakage.
An amalgam restoration is the next best alternative. It is preferred in teeth that are of less strategic value, that is, teeth that would exfoliate within 2 years.
The post-endodontic restoration needs no removal for re-entry into the lesion. The procedure is depicted.
Indirect Pulp Capping Review
The success of indirect pulp capping depends on the elimination of microleakage in the restoration.
Reparative dentin forms at the rate of 1 µm per day. The tooth has to be reviewed within 3 months.
A radiographically discernible hard-tissue barrier can be identified within 3 months.
Failure of the therapy manifests with the sign of pulpitis or abscess formation and radiolucent lesion on the furcation of the tooth.
The absence of clinical and radiographic signs of failure expresses short-term success only.
The tooth has to be reviewed every 6 months with a radiographic review every 2 years (when asymptomatic).
Pulpotomy
Pulpotomy is described as the complete removal of the coronal portion of the dental pulp followed by the placement of a suitable dressing or medicament that will promote healing of the pulp and preserve the vitality or integrity of the tooth.
Pulpotomy Rationale
When the coronal half of the pulp is irreversibly inflamed and its radicular portion is healthy or reversibly inflamed, a pulpotomy is performed.
Amputation of the coronal pulp and placement of a suitable medicament over the radicular pulp can promote healing and maintenance of its vitality.
The medicament should fulfill the following criteria:
- It has to be bactericidal.
- It should be biocompatible with pulp tissue.
- It should promote the healing of the radicular pulp.
- It should not interfere with root resorption.
Pulpotomy Indications And Contraindications
Pulpotomy is indicated when the teeth are vital with signs of reversible pulpitis.
It can also be indicated in case of accidental exposure of the pulp during an operative procedure.
The contraindications of pulpotomy are as follows:
- Presence of clinical and radiographic signs of irreversible pulpitis such as spontaneous or persistent pain or inter-radicular radiolucent foci
- Presence of signs of non-vitality and tenderness on percussion
- Signs of periodontal involvement, abscess, and draining sinus
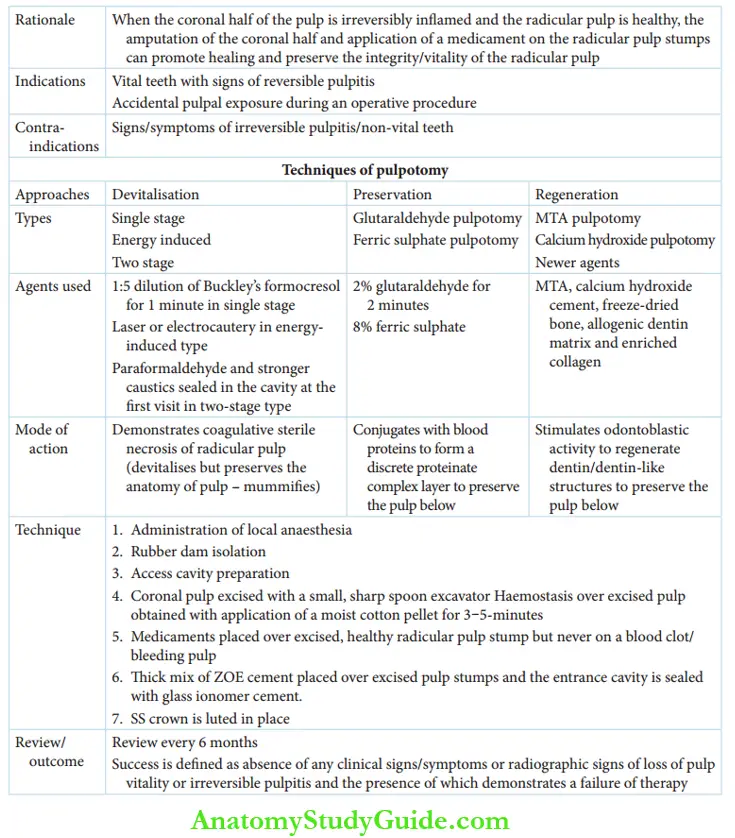
Pulpotomy Techniques
There are three distinct approaches to preserving the integrity and restoring the health of the radicular pulp. They are as follows:
1. Devitalization approach
- Single-stage devitalisation
- Energy-induced techniques
- Laser pulpotomy
- Electrosurgical pulpotomy
- Two-stage devitalisation(mortal pulpotomy)
2. Preservation approach
- Glutaraldehyde pulpotomy
- Ferric sulfate pulpotomy
3. Regeneration approach
1. Devitalisation Approach
The radicular pulp is devitalized with the help of mummifying agents. These agents demonstrate coagulative, sterile necrosis of the radicular pulp.
They halt the physiological activity of the pulp while preserving the anatomical structure, without inciting any pathology. Therefore, the procedure is described as sterile necrosis.
Devitalisation Approach Types
The three types of devitalization procedures are as follows:
- Single-stage devitalisation by Buckley’s formocresol
- Energy-induced techniques such as laser pulpotomy and electrosurgical pulpotomy
- Two-stage devitalization with gysitriopaste, Easlick’s formaldehyde, and para-form devitalizing paste
Single-Stage Devitalisation
The devitalization approach with formoterol is the oldest of the pulpotomy techniques. Formocresol was proposed as a medicament by Buckley as early as the 1900s.
Initially, full-strength formoterol was used. Buckley’s formoresol contains 19% formaldehyde and 35% cresol in a 15% solution of glycerine and water.
A 1:5 concentration of this formula is prepared by adding 3 parts glycerine and 1 part water to 1 part of Buckley’s formoterol.
The devitalization pulpotomy technique was performed by Sweet in the 1930s with a 7-day application of full-strength formoterol.
Berger evaluated the success of a 5-minute application of full-strength formocresol in 1963.
Morawa concluded the success of 1:5 dilution of formocresol over ‘full-strength formocresol’ in 1975. Fuks and Bimstein also emphasized the success of diluted formoterol.
Several authors have concluded that the time of application offormocresol does not increase or decrease the success rate of the pulpotomy.
Hence, the time of application had been reduced to 2 minutes. The current clinical practice involves a 1-minute application of 1:5 dilution of Buckley’s formocresol.
Formocresol evolves three distinct zones in the pulp. The thickness of these zones is wider when the application time is higher or the concentration is stronger. These zones, from the coronal to apical direction, are as follows :
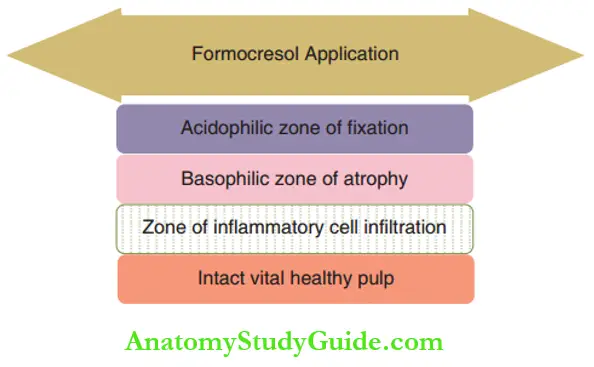
- Broad acid pedophilic zone officiation represents the layer of pulp that has undergone coagulation necrosis.
- The broad basophilic zone of atrophy is the intermediate zone between intact pulp and necrosed pulp.
- The broad zone of inflammatory cell infiltration extends below the intact pulp.
Intact vital pulp tissue is evident below these layers, which have undergone progressive fixation and degeneration. Formaldehyde bonds to proteins by binding with the end peptide chains of certain amino acids.
This changes the overall structure of the protein molecules and preserves the tissue from undergoing autolysis. This altered tissue can be described as a ‘field’.
The fixed tissue is said to have undergone ‘sterile necrosis’. It is revitalized and will not undergo subsequent putrefaction.
The term mummification has also been applied here. According to Egyptians, mummy implies embalming/preserving dead bodies, that is, preserving the anatomy of the body when non-vital or when there is no life.
Similarly, here the pulp is non-vital while its anatomy is preserved, thus rightly said as mummified.
Formocresol has been documented to be associated with the following undesirable consequences:
- Broadening of the acidophilic zone of fiction to encroach on the other layers and into the intact pulp, leaving no intact vital pulp at the end of1 the year.
- Percolation of formoterol vapors (stronger concentration or longer application) into the alveolar bone can cause enamel hypoplasia of succedaneous teeth.
- Systemic absorption of formoterol (owing to its small molecular size and weight) is associated with dermatitis and pharyngitis.
- Formocresol is a proven mutagen/carcinogen.
Minute Pulpotomy
One-minute application of formocresol over the radicular pulp is called a minute pulpotomy.
With a 1-minute application, the undesired consequences of formoterol are minimal.
Also, the layers of degeneration are of minimal width leaving behind a wider zone of healthy pulp tissue below.
There is no decrease in the success rates of the procedure.
Energy-Induced Pulpotomy
Energy-induced pulpotomy is a chemical mode of excision or cauterizing of the coronal pulp tissue, elimination of infection, and mummification of radicular pulp with the help of an energy source.
Electrosurgical Pulpotomy
This method utilizes electrocautery equipment. It carbonizes and denatures the pulp, eliminates bacterial contamination, and obtains hemostasis.
Pulpot I is carried out after the coronal pulp is manually excised and the pulp stumps are electrocauterized.
Mack and Dean (1993) and El-Meligy et al. (2001) elaborated on the efficacy of electrosurgical pulpotomy.
They concluded that electrosurgical pulpotomy has success rates similar to those of formoterol pulpotomy.
Laser Pulpotomy
Laser pulpotomy is a non-pharmacologic, more biologically acceptable hemostatic technique.
Sof lasers, such as Nd: YAG lasers, are used to excise the soft tissue and attain hemostasis of the radicular pulp stump.
Shigeru Shoji et al. (1985) and Jeng–Fen Liu et al. (1999) accounted for a good success rate with carbon dioxide laser pulpotomy.
Two-Stage Devitalisation Procedure
Two-stage devitalization pulpotomy is a less commonly performed procedure that uses stronger caustic materials such as paraformaldehyde.
The medicaments that are used are gypsy triopaste, paraformaldehyde paste, and Easlick’s paste.
The chances of leaving a healthy vital intact pulp tissue below the degenerated zone are absolutely negligible in this procedure.
This is due to the combination of the caustic materials used and the length of time of medicament application (1–2 weeks between the first and the second appointments).
These strong caustic agents make the radicular pulp undergo complete sterile necrosis. So, this technique is also called a mortal pulpotomy.
Two-Stage Devitalisation Procedure Procedure
The procedure is performed in the following two stages:
Stage 1: The access cavity is opened under local anesthesia. Coronal pulp is excavated and the caustic medicament is kept in moistened cotton. This is followed by a temporary restoration.
Stage 2: After 1 –2 weeks, the lesion is re-entered under local anesthesia. The medicament is removed and the cavity is irrigated with saline. The cavity is restored with a thick mix of zinc oxide eugenol followed by a stainless steel crown.
There is only one clinical indication for this technique in current-day practice. It is an alternative for pulpectomy in a pre-cooperative child (younger than 2½ years).
When pulpectomy is indicated for a primary fist molar and the treatment has to be carried out under non-pharmacological modes of behavior management, the pulp can be devitalized with these caustic agents.
The coronal pulp can be incompletely excised and the radicular pulp can be subjected to a two-stage devitalization with the caustic medicaments.
The tooth can then be restored with a thick mix of zinc oxide eugenol followed by intermediate restorative material (IRM).
The tooth can be intervened at a later date, maybe when the child turns 4 years. This, a mortal pulpotomy is a compromised alternative for pulpectomy in a very young child.
2. Preservation Approach
The preservation mode utilizes chemicals that indulge in minimal degeneration of the radicular pulp tissue and preserve its vitality.
Glutaraldehyde and ferric sulfate are the medicaments used in this approach.
Glutaraldehyde Pulpotomy
Glutaraldehyde is a higher/heavier hydrocarbon carrying an aldehyde group whose molecular weight is significantly higher than that of formaldehyde.
Hence, it has poor diffusivity and lower antigenicity. 2%–5% of glutaraldehyde is used.
The poor penetrative ability (owing to the larger molecular size) eliminates the risks of cresol such as toxicity, mutagenicity, and carcinogenicity.
Glutaraldehyde minimally alters pulp tissue, unlike formoterol which creates three thick zones of degeneration. The altered pulp simulates an almost healthy pulp.
Kopel (1979) and later Garcia-Godoy and Fuks et al. demonstrated the efficacy of this medicament in pulpotomy.
Ferric Sulphate Pulpotomy
Ferric sulfate is an inert hemostatic agent. The ferric ions combine with the plasma proteins of the blood to form a metal proteinate clot at the surface of the radicular pulp stump.
The formation of metal-protein clots was proposed by Ranly. This metal-protein clot acts as a passive barrier to maintain the healthy radicular pulp unaltered.
8% ferric sulfate is used as a pulpotomy missing agent. Ferric sulfate, as a pulpotomising agent, was suggested as an on-par substitute for formoterol by Fei et al. in 1991.
3. Regenerative Approach
The ideal and most biocompatible of the three approaches is the regenerative approach as it strives to preserve the radicular pulp, enclosed in a dentinal chamber with an odontoblastic lining.
The medicaments used in this approach stimulate reparative dentin formation over the cut ends of the radicular pulp tissue.
Calcium hydroxide is used for stimulation of reparative dentin formation in operative procedures. But it is strictly contraindicated as a medicament for the regenerative approach in primary pulps.
This is because calcium hydroxide can stimulate undifferentiated mesenchymal cells of the primary pulp. These cells may differentiate into either odontoblasts or odontoclasts.
When odontoblasts result, they form multiple calcific foci in the pulp leading to a calcified metamorphosis of pulp. When odontoclasts result, they form resorption foci leading to internal resorption.
MTA was formulated as a root-end filling material in surgical endodontics by Torabinajed.
MTA powder consists of fine hydrophilic particles of tricalcium silicate, tricalcium aluminate, tricalcium oxide, and silicon dioxide.
Other mineral oxides are added in traces to modify the chemical and physical properties of the material.
Bismuth oxide is added to impart radiopacity to the material. MTA is either white or grey.
Grey MTA has more oxides of iron incorporated and its setting time is longer and alkalinity lesser than white MTA.
MTA with higher walkability is preferred as it is directly proportional to its regenerative capacity.
MTA demonstrates high alkalinity with a pH of 12.5, which is quite similar to but greater than calcium hydroxide cement.
This high alkalinity accounts for odontoblastic and osteoblastic activity.
On mixing, MTA resembles a colloidal gel that hardens in approximately 140 minutes with white MTA or 175 minutes with grey MTA.
MTA is now available commercially. It has demonstrated more significant clinical success than formoterol in recent clinical studies.
However, the use of MTA as a pulpotomising agent is relatively expensive by Indian standards.
The various other medicaments that are being tried at experimental levels and less popularised commercially are as follows:
- Freeze-dried bone
- Allogenic dentin matrix, which is autolyzed and antigen extracted
- Enriched collagen
- Bone morphogenic proteins (BMP)
It gives a comparison of all three approaches to the pulpotomy procedure.

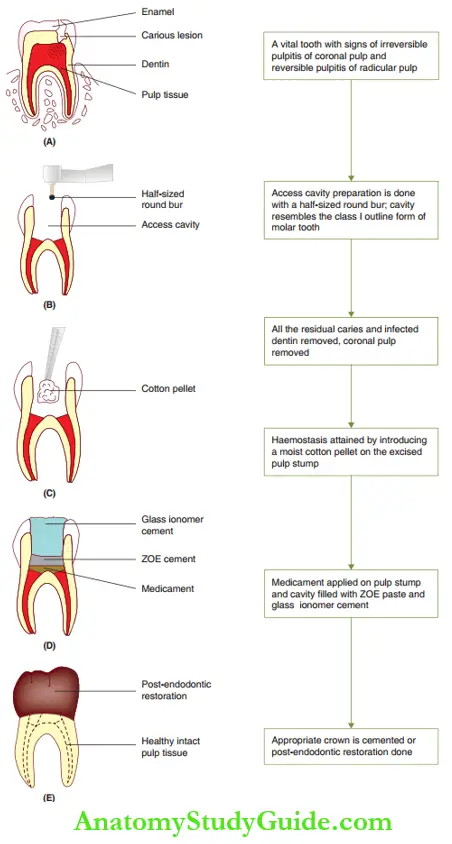
Regenerative Approach Pulpotomy Procedure
The tooth is anesthetized. Rubber dam application is necessary as the medicaments used are caustic and can cause burn injuries. The access cavity is prepared with a half-sized round bur.
The cavity prepared is similar to the outline of a class 1 cavity primary molars. The cavity is deepened to gain entry into the pulp chamber.
Once the entry is gained, the bur is used to pull out dentin in strokes to an extent where no dentin overhangs the pulp chamber. All residual caries and carious dentin are removed.
Initial hemostasis is attained with a wet cotton pellet and visualized. The coronal pulp is excised with a small, sharp spoon excavator. The pulp is amputated till the root canal orifices.
Hemostasis is attained in 3–5 minutes by a moist cotton pellet on the excised pulp stumps.
The inflammatory status of the pulp is diagnosed during the procedure. This can be termed procedural diagnosis.
If bleeding still persists, there could be two possibilities. One is that there could be remaining pulp fragments in the pulp chamber in an undercut.
The second could be a highly inflamed radicular pulp where hemostasis cannot be attained.
Such a tooth is indicated for a radical mode (total removal of radicular pulpal tissue) of endodontic therapy.
On attaining hemostasis, the medicament is applied to the excised pulp stumps.
The thumb rule is that the medicament should not be kept on a blood clot or a bleeding pulp but on an excised healthy, uninflamed pulp.
On treatment with the medicament, one-half of the pulp chamber is filled with a thick mix of zinc oxide eugenol cement. The other half is filled with restorative glass ionomer cement.
The tooth surface preparation is done for a stainless steel crown and an appropriate crown is cemented for rehabilitation.
A stainless steel crown is indicated as a pulpotomy dental structure that has lesser tensile and shear strength.
It is preferred in multi-surface carious lesions as it eliminates coronal microleakage.
The next best mode of restoration is post-endodontic amalgam restoration. However, it is preferred when the life of the primary tooth is less than 2 years.
Regenerative Approach Outcome
A pulpotomies tooth has to be reviewed clinically every 6 months and radiographically every year for the first 3 years.
The absence of signs and symptoms, normal tooth resorption and absence of inter-radicular rarefaction are desired outcomes that describe the success of the therapy.
Signs and symptoms of irreversible pulpitis, dentoalveolar abscess, with or without draining sinus.
Inter-radicular bone loss, internal resorption, diffuse calcifications in the pulp chamber, and unequal root resorption are indications of failure of therapy.
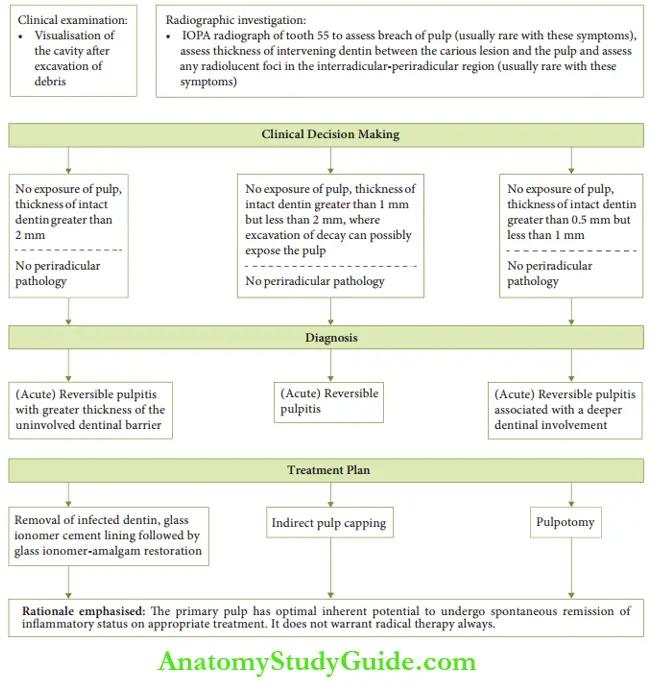
Case Description
Case 1
Chief complaint: A 6-year-old male child complains of discomfort in his right upper back tooth while drinking hot soup or eating ice cream.
Clinical scenario: A 6-year-old child complains of transient discomfort from hot soups and ice creams on his right maxillary second molar. No history of spontaneous pain.
[Baseline data – Pulp of the tooth need not necessarily be exposed to exhibit pain or undergo the pathologic sequelae. Dentin is an innervated tissue, an exposure of which can elicit pain.]
Case 2
Chief complaint: Accidental exposure of the mesiobuccal horn of pulp on 65 while performing indirect pulp capping.
Clinical scenario: A 6-year-old child was indicated for an indirect pulp capping on tooth 65. During the operative procedure, under rubber dam isolation, accidental exposure of the mesiobuccal horn of the pulp occurred.
Summary
1. Conservative endodontic procedures are indirect pulp capping, direct pulp capping, and pulpotomy.
2. Pulp capping
3. Pulpotomy is the complete removal of the coronal portion of the dental pulp followed by the placement of a suitable dressing/medicament that will promote the healing of the pulp and preserve the vitality/integrity of the tooth.
Leave a Reply