Deep Structure in the Neck Anatomy Questions and Answers
Question 1: What forms the right lymphatic duct?
Answer :1. Right jugular trunk, and
2. Right subclavian trunk.
Table of Contents
Question 2: Describe scalenus anterior under the following headings:
1. Scalenus Anterior Attachments,
2. Scalenus Anterior Nerve supply,
3. Scalenus Anterior Actions,
4. Scalenus Anterior Relations, and
5. Scalenus Anterior Applied anatomy
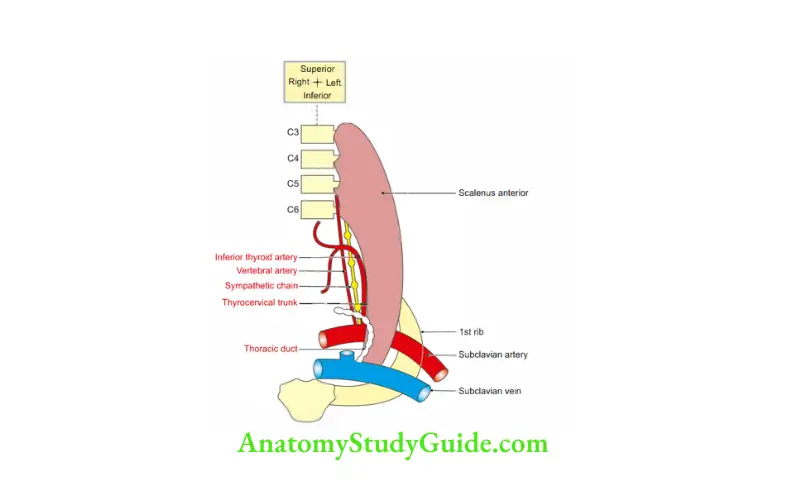
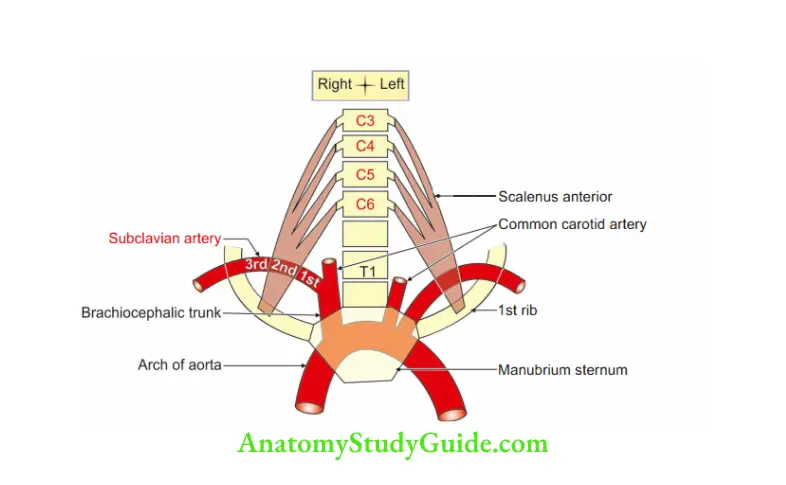
The scalenus (scalene-triangle with unequal sides) anterior is the key muscle of the neck extending from the anterior tubercle of typical cervical vertebrae.
Answer 1. Attachments:
1. Proximal: It arises from the anterior tubercle of the typical cervical vertebrae, i.e. C3, C4, CS and C6.
2. Distal: It is inserted by a narrow tendon to the
- Scalene tubercle on the inner border of lst rib,
- To a ridge on the upper surface of the rib between the grooves for the subclavian artery and vein.
2. Scalenus Anterior Nerve supply: Ventral rami of 4th, 5th and 6th cervical nerves.
3. Scalenus Anterior Actions: Acting from above, it elevates 1st rib and acts as an accessory muscle for inspiration.
Read And Learn More: Neck Anatomy Notes And Important Questions With Answers
4. Scalenus Anterior Relations
Anterior (from before backwards)
1. Skin,
2. Superficial fascia,
3. Platysma, and
4. Investing layer of deep cervical fascia.
5. Clavicle and muscles attached to the clavicle, i.e.
- Subclavius, and
- Sternocleidomastoid.
6. Carotid sheath and its contents
- Common carotid artery,
- Internal jugular vein, and
- Vagus nerve.
7. Termination of the thoracic duct on the left side.
8. Thyrocervical trunk and three branches.
- Suprascapular artery,
- Inferior thyroid artery, and
- Transverse cervical artery
9. Prevertebral fascia,
10. Phrenic nerve. It runs vertically downward.

2. Posterior
- 2nd part of subclavian artery,
- Roots of brachial plexus,
- Scalenus medius, and
- Suprapleural membrane.
3. Superior: Longus capitis
4. Medial
1. Scalenovertebral triangle containing
- 1st part of vertebral artery, and
- Vertebral vein.
2. Sympathetic trunk
5. Lateral: Brachial plexus.
5. Scalenus Anterior Applied anatomy
- Cervical rib: Additional rib from the 7th cervical vertebra.
It passes between the scalenus anterior and medius.
Clinical manifestations are - Wasting of hypothenar muscles
- Sensory loss of medial 1 ½ finger of the hand and part of the forearm due to compression of the lower trunk of the brachial plexus.
Anastomotic sites of carotid and subclavian arteries
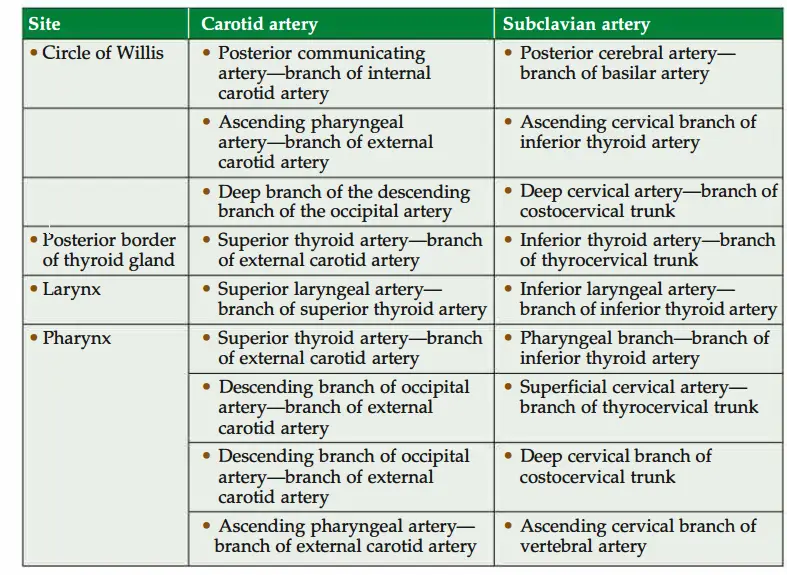
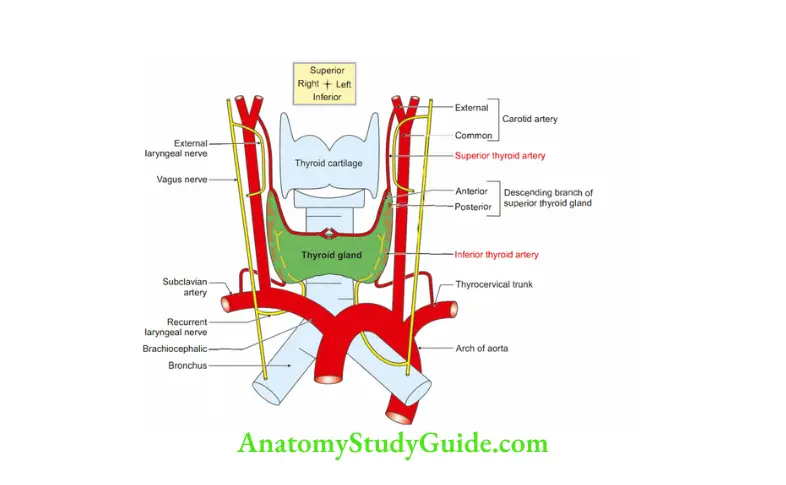
Question 3: Why superior thyroid artery is ligated close to the superior pole and the inferior thyroid artery away from the inferior pole into thyroidectomy?
1. The superior thyroid artery and external laryngeal nerve are away from each other at the superior pole.
Hence, it is safe to ligate the superior thyroid artery at the superior pole, to avoid injury to the external laryngeal nerve.
2. The inferior thyroid artery and the recurrent laryngeal nerve are intimately related to the inferior pole.
It is not safe to ligate the inferior thyroid artery at the inferior pole. Hence, one is advised to ligate the inferior thyroid artery away from the inferior pole to avoid injury to the recurrent laryngeal nerve.
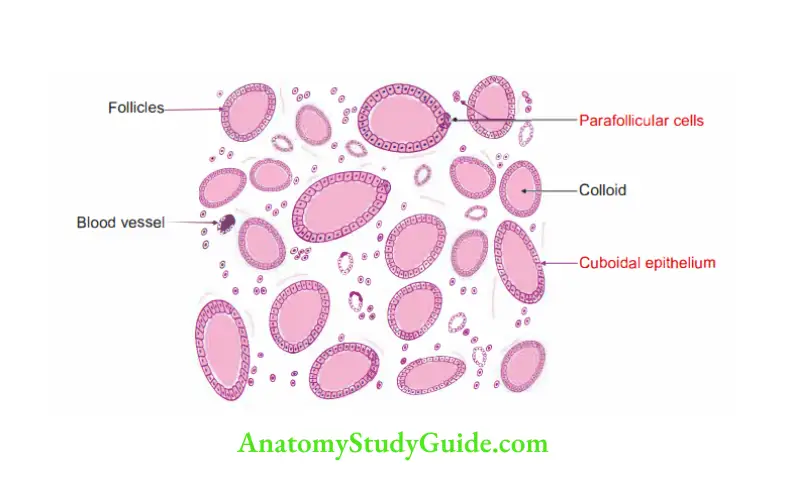
Question 4: What are the lining epithelial cells of the thyroid gland?
Answer: 1. Follicular cells
2. Parafollicular cells
Question 5: What are parafollicular cells? What do they secrete?
Answer :1. Parafollicular cells occur as single cells or in clumps on the periphery of the follicles.
2. They stain somewhat lighter than the follicular cells
3. They are readily visible in the canine (dog) thyroid.
4. They synthesize and secrete the hormone calcitonin.
Question 6: What is the colloid in thyroid follicles made up of?
Answer :1. The colloid is formed by the follicular cells.
2. Its main component is thyroglobulin.
3. Thyroglobulin is the inactive storage form of thyroid hormone.
Question 7:State the two types of cells in the parathyroid gland. What does the parathyroid gland secrete?
Answer: Parathyroid glands contain two types of cells
1. Principal or chief cells
- These are the most numerous cells.
- They are polygonal in shape.
- They are arranged in clumps or irregular cords.
- The cytoplasm of the cells shows numerous secretory granules.
- Each cell has a centrally located spherical nucleus.
- Large capillaries are present in between the cords and clumps.
- They secrete parathyroid hormone (PTH or parathormone).

2. Oxyphil cells
- They are larger in size but fewer in number than chief cells.
- They are arranged in clumps.
- Their function is not clear.
Question: Describe production of thyroid hormones from follicular cells to its release into the capillary.
1. Synthesis and storage
- Thyroglobulin is synthesised by rough endoplasmic reticulum.
- It is carried to Golgi complex.
- It is packed into vesicles.
- These vesicles are transported to the apical surface of the cell.
- The thyroglobulin is discharged into the lumen of the follicle by exocytosis.
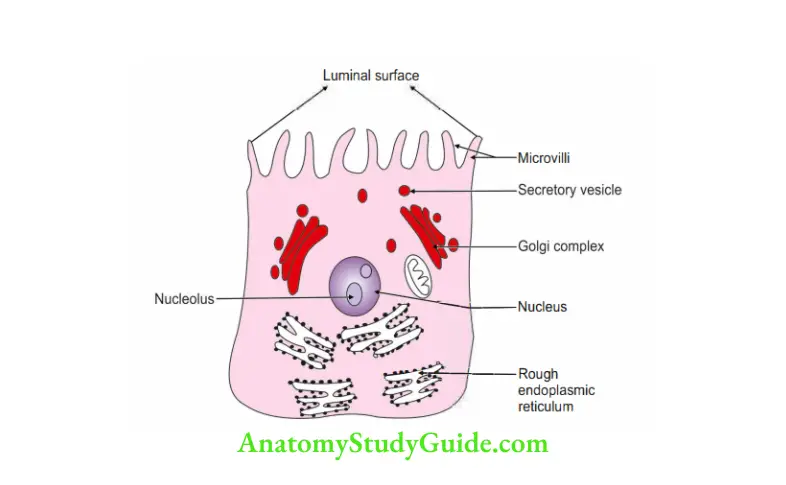
2. Iodide uptake
- Under the influence of TSH, follicular cells take up iodine from the blood.
- Iodide is oxidised to iodine by enzyme thyroid peroxidase.
3. Iodination of thyroglobulin
- Iodination of thyroglobulin occurs at the luminal surface of the follicular cells.
- Triiodothyronine (T) and tetraiodothyronine (T4, also known as thyroxine) are formed
4. Release of thyroid hormones
- Stimulation of follicular cells by TSH causes endocytosis of thyroglobulin.
- Numerous colloid resorption droplets containing iodinated thyroglobulin are formed.
- Lysosomes fuse with the colloid resorption droplets.
- These droplets release T4 and T3 hormones.
- They enter blood circulation.

Question 8: Describe the thyroid gland under the following heads:
1. Thyroid Gland Gross anatomy,
2. Thyroid Gland Histology,
3. Thyroid Gland Development, and
4. Thyroid Gland Applied Anatomy. (Threos-shield, sides-form)
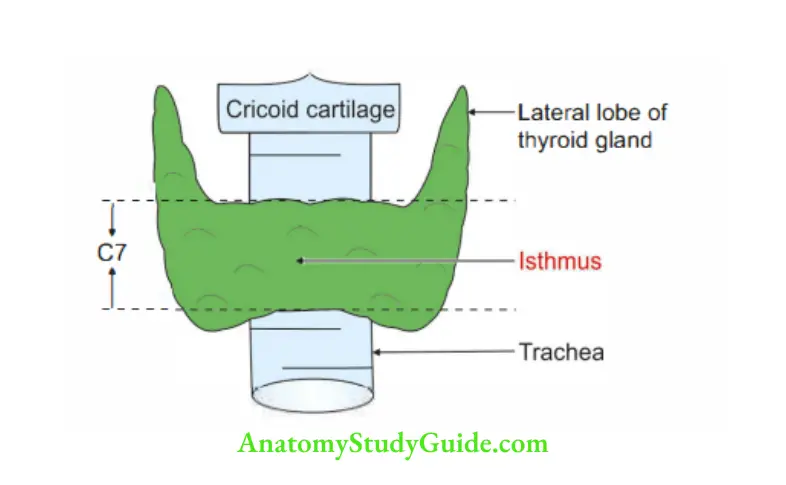
Answer 1. Gross anatomy
Situation
- It is situated in front of the CS, C6, C7 and Tl vertebrae.
Relations of several cervical vertebrae of the third gland are remembered by associating with the number of cervical vertebrae related to the ventral rami of the brachial plexus.
- Each lobe extends from the oblique line of the thyroid cartilage to the 6th tracheal ring.
- The isthmus extends from the 2nd to the 3rd tracheal ring.
2. Dimensions and weight
- Each lobe measures 2″ x l” x l”.
- The isthmus measures ½” x ½”
- Weight: About 25 g
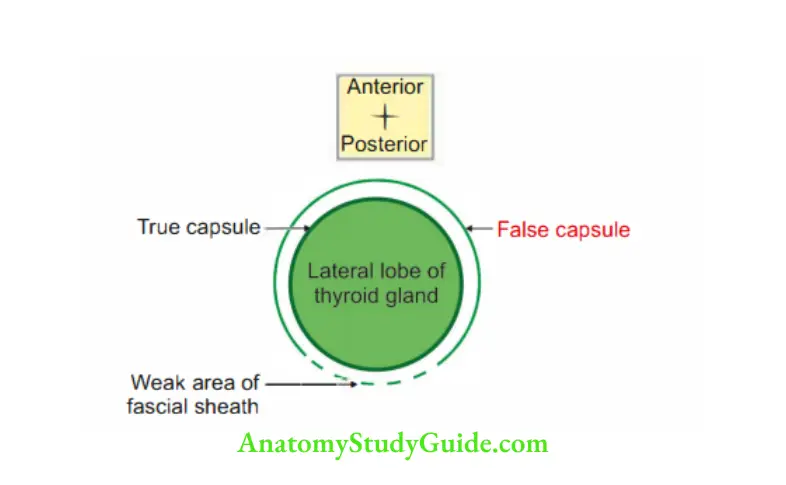
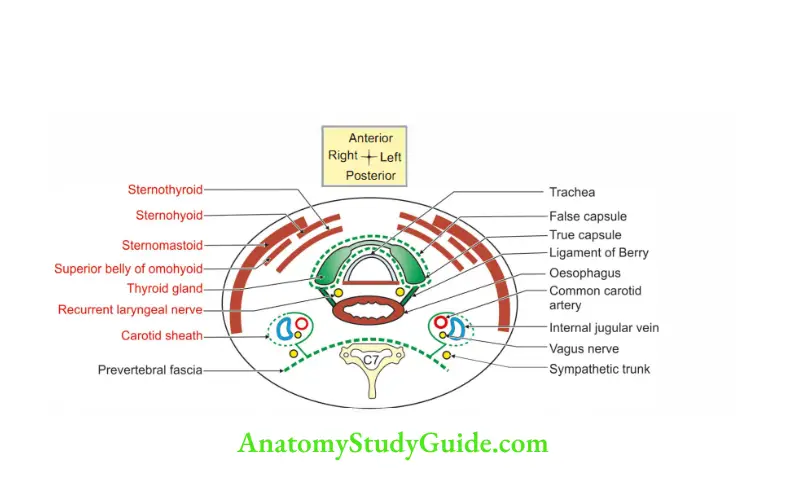
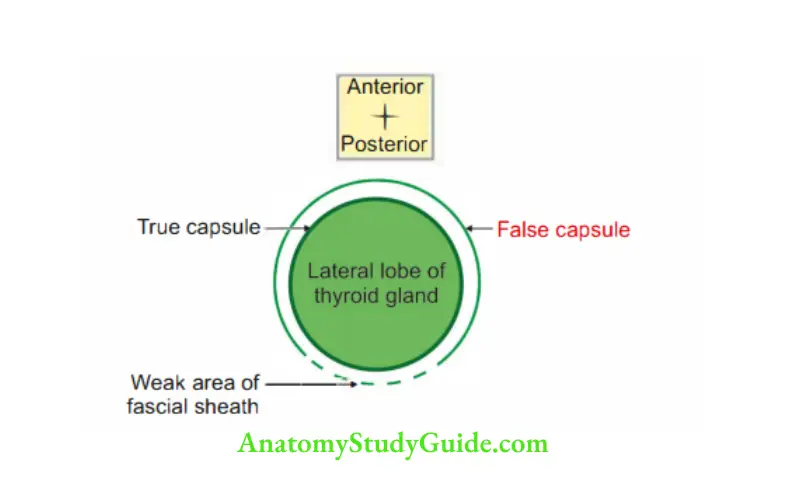
3. Capsules ”
- True capsule: It is a condensation of the peripheral part of the connective tissue of the gland.
- False capsule: It is condensation of pre tracheal layer of deep cervical fascia.
4. Surfaces of
Lateral lobes..Preventive and social medicine)
- Posterior
- Superficial
- Medial
Isthmus
- Anterior, and
- Posterior.
Borders of
Lateral lobe
- Anterior, and
- Posterior.
Isthmus
- Upper, and
- Lower.
6. Relations of lateral lobe of the thyroid gland
1. Relations to surface
- Superficial
- Smohyoid
- Smothyroid,
- Superior belly of omohyoid, and
- Smomastoid.
Medial.
- Muscles:
- Inferior constrictor, and
- Cricothyroid.
Tubes:
- Trachea, and
- Oesophagus.
Nerves:
- External laryngeal nerve, and
- Recurrent laryngeal nerve.
Posterolateral: Carotid sheath.
2. Relations to border
- Anterior: Superior thyroid artery (anterior descending branch).
- Posterior: The parathyroid gland is an important structure. Other structures are
- Inferior thyroid artery.
- Thoracic duct (only on the left side).
- Anastomosis between superior and inferior thyroid arteries.
7. Thyroid Gland Blood supply
Arterial :
1. Inferior thyroid artery:
1. It is a branch of the thyrocervical trunk.
2. It is the chief artery of the thyroid gland.
3. It supplies
- Lower 2/3rd of the lobe of the gland, and
- The lower half of the isthmus.
4. It penetrates the deep surface of the gland and anastomoses with the descending branch of the superior thyroid artery.
5. The anastomosis takes place at the junction of the upper l/3rd with the lower 2/3rd of the posterior border. @
6. It has an intimate relation with the recurrent laryngeal nerve near the gland.
2. Superior thyroid artery
1. It is a branch of the external carotid artery.
2. It supplies
- Upper l/3rd of the gland, and
- The upper half of the isthmus.
3. It descends up to the apex of the thyroid gland and divides into anterior and posterior branches.
The branches descend on the respective borders.
- The anterior branch anastomoses with an artery on the opposite side at the superior border of the isthmus.
- Posterior branch anastomoses with inferior thyroid artery on the posterior border.
4. It is closely related to the external laryngeal nerve.
Thyroid ima: It either arises from the brachiocephalic trunk or arch of the aorta. It supplies the isthmus of the thyroid gland.
Numerous accessory thyroid arteries, and branches of oesophageal and tracheal arteries. These branches supply the gland from the medial or deep surface.
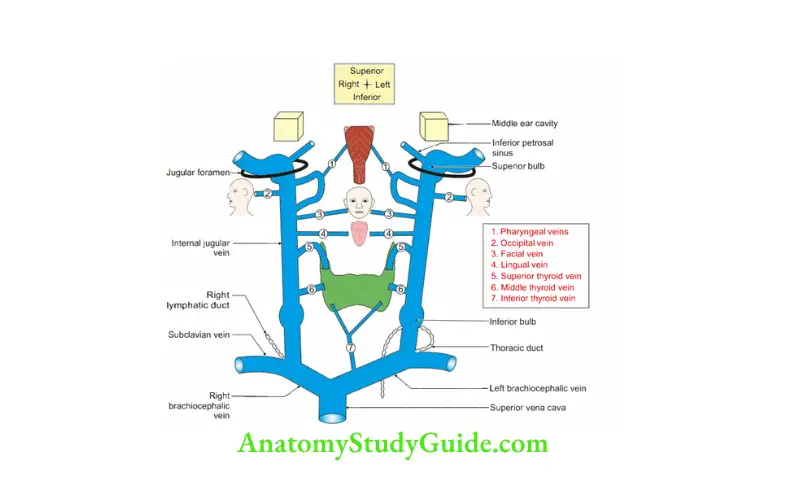
2. Venous drainage: The veins of the thyroid gland form a plexus which is situated deep to the capsule.
They do not accompany arteries.
They drain as follows
- Superior thyroid vein
- Middle thyroid vein
- Kocher’s vein } Drain into the internal jugular vein
- Left and right inferior thyroid veins drain into the brachiocephalic vein.
Note: Kocher’s vein is the 4th vein of the thyroid gland.
It drains the lower pole of the thyroid gland when present.
It is occasionally present between the middle and inferior thyroid veins.
The superior thyroid vein is related to the lateral border of the superior belly of the omohyoid muscle.
The middle thyroid vein is related to the medial border of the superior belly of the omohyoid muscle.
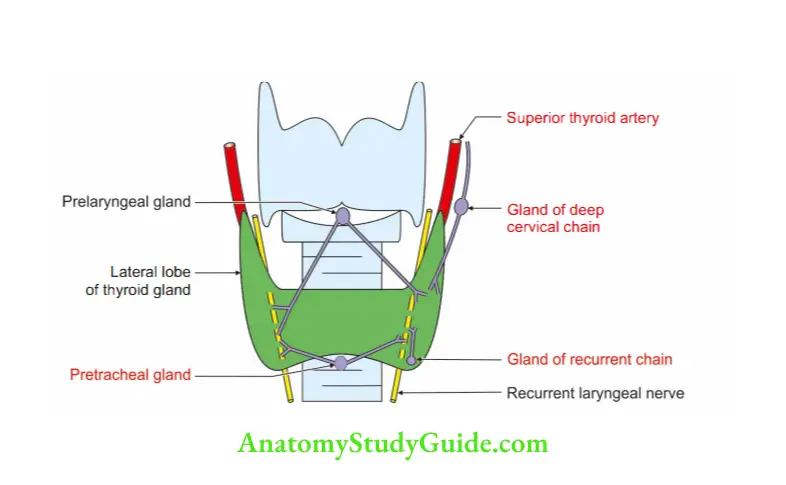
8. Lymphatic drainage: They are arranged into
- Upper group: Prelaryngeal and jugulodigastric group of lymph nodes.
- Lower group: Pretracheal group of lymph nodes along recurrent larynx nerve.
Nerve supply: They are derived
- Mainly from the middle cervical sympathetic ganglion.
- Partly by superior and inferior sympathetic ganglion.
- Function: Vasoconstriction.
2. Histology :
- The Lumen of follicles shows colloid material.
- Follicles are lined by cuboidal epithelium.
- There are clear or light cells called parafollicular cells which produce calcitonin.
- They are polyhedral with oval, eccentric nuclei.
- They are present between follicular cells and lie on the basement membrane.
3. Development
1. Chronological age
- It develops in the 4th week of intrauterine life.
- The descent of the thyroid gland is completed at 7th cervical vertebra. (Number isequal to the number of alphabets of “thyroid”.)
- The secretion of thyroid commences from the 4th month of IUL.
2. Germ layer: It develops from endoderm of
- 2nd pharyngeal arch.
- 4th pharyngeal pouch.
3. Site: Floor of the primitive pharynx behind the tuberculum impar (unpaired) of the developing tongue.
4. Sources
- It develops as a median thyroid diverticulum extending from foramen caecum to thyroid cartilage.
- The distal part becomes bifid.
- The duct divides into a series of double cellular plates.
- The colloid accumulates within the bilaminar plates.
- The bilaminar plate is converted into primary thyroid follicle.
- The buds arise from th primary thyroid follicleand differentiate into secondary or definite follicles.
- The caudal pharyngeal complex (ultimobranchial body) joins each side of the lower end of thyroglossal duct to give origin to parafollicular cells.
- The duct disappears, its cephalic end persists as a foramen caecum and its caudal end occasionally forms the pyramidal lobe.
5. Anomalies:
- Incomplete descent of thyroid gland.
- Ihyroglossal duct.
- Ihyroglossal cyst.
- Agenesis of thyroid gland.
- Lingual thyroid
4. Applied anatomy
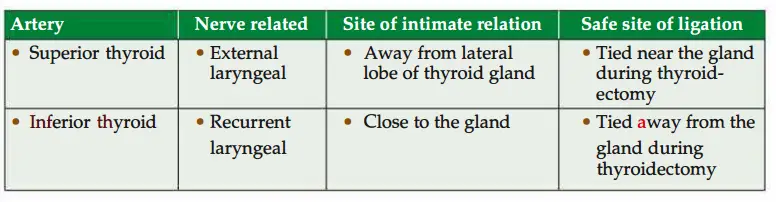
- During thyroid operation, inferior thyroid artery should be tied
from the gland to avoid injury to recurrent laryngeal nerve. - The superior thyroid artery should be tied near the gland to avoid the injury to the external laryngeal nerve.
- Thyroid Swelling moves with Swallowing but does not Swift (move) on protrusion of tongue.
- Kocher vein, if present, may bleed profusely during thyroid operation. Therefore, an attempt should be made to search and ligate.
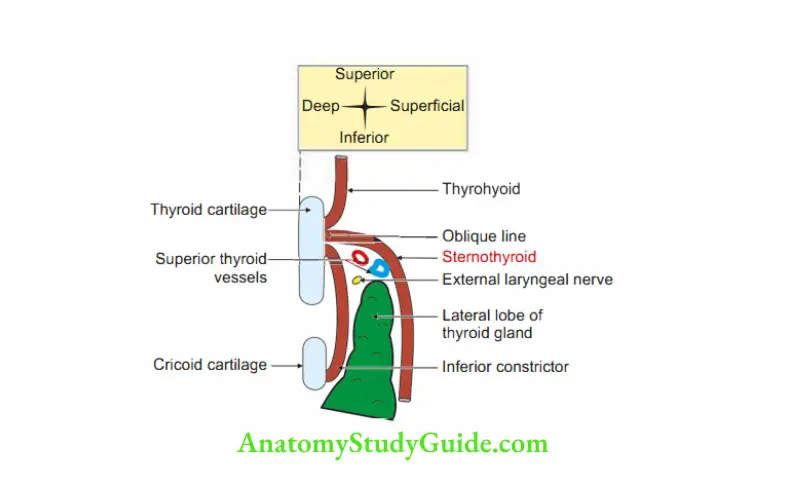
Attachment of stemothyroid muscle to oblique line prevents upward enlargement of thyroid gland.

Question 9: Name the arteries supplying thyroid gland.
1. Inferior thyroid arter
- Chief artery of thyroid gland
- Branch of thyrocervical trunk
- 3. Supplies
- Lower 2/3rd of lateral lobe of thyroid gland, and
- Lower half of the isthmus of thyroid gland.
2. Superior thyroid artery
1. 1st ventral branch of external carotid artery
2. Supplies
- Upper l/3rd of lateral lobe of thyroid gland.
- Upper half of the isthmus of thyroid gland.
3. Thyroid ima (lowest) artery
- Branch of arch of aorta
- Rarely present.
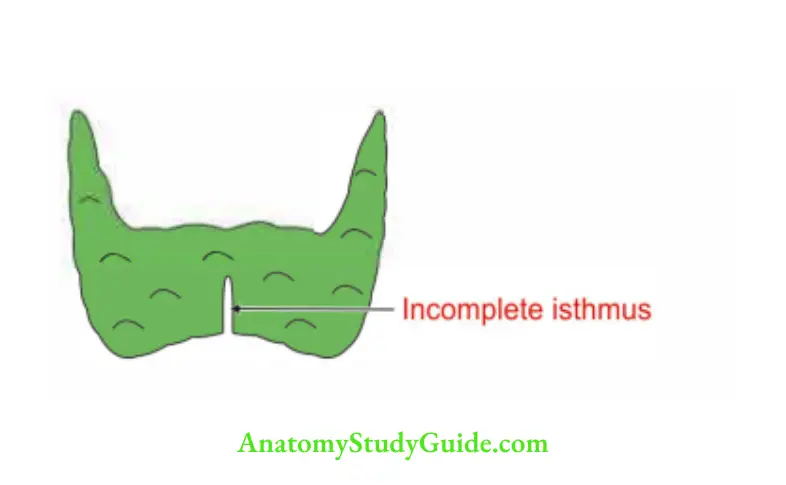
Isthmus of thyroid gland
Introduction: It is median quadrilateral part of gland.
1. Morphology
- Dimension: 1.25 cm in length and breadth
- Surfaces: Anterior and posterior
- Borders: Upper and lower.
- Extent: From 2nd to 3rd tracheal ring.
2. Relations
Upper border
- Site of anastomosis of anterior descending branch of right and left superior thyroid arteries.
- Pyramidal lobe: A small conical mass of thyroid tissue.
- Levator glandulae thyroideae: A fibromuscular band connecting upper border of isthmus to pyramidal lobe of thyroid gland.
Note: It is supplied by external laryngeal nerve.
It is remnant of median thyroid diverticulum.
It never represents remnant of the thyroglossal duct.
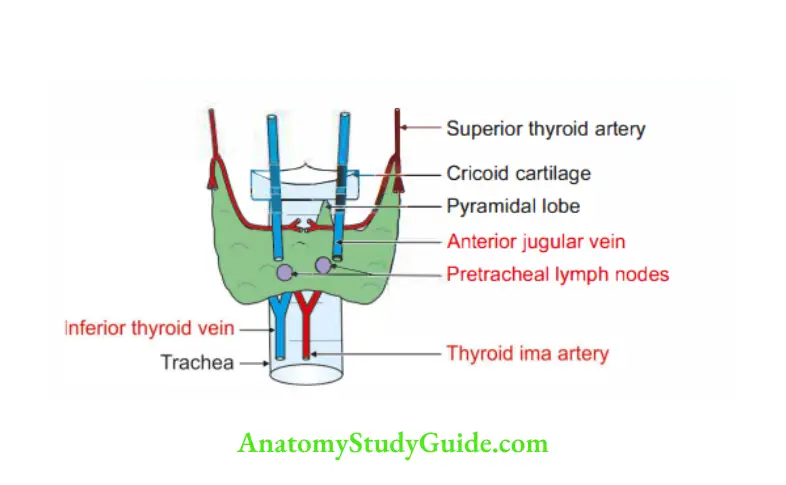
2. Lower border is related to –
- Inferior thyroid vein: It emerges from lower border of isthmus of thyroid gland. C
- Arteria thyroidea ima (lowest): It enters lower border of isthmus of thyroid “gland.
3. Anterior surface: It is related to
- Skin
- Superficial fascia containing anterior jugular vein
- Deep fascia of neck
- Stemohyoid
- Stemothyroid
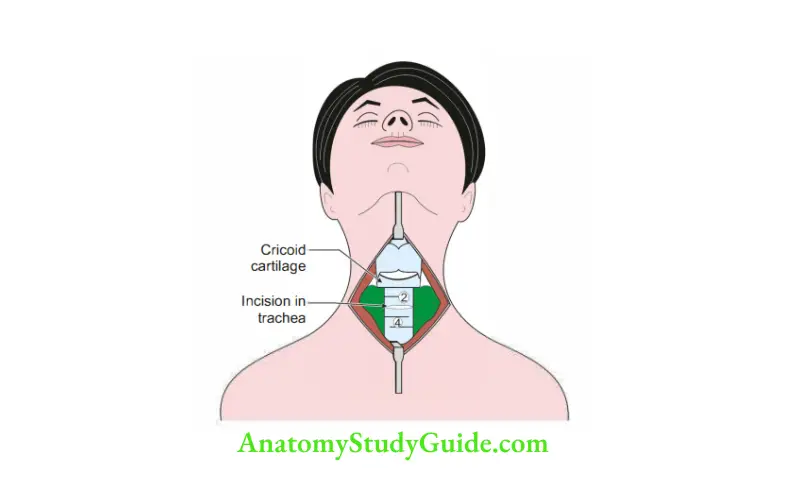
4. Posterior surface: Posterior surface of the isthmus firmly adhere to 2nd, 3rd and 4th tracheal cartilages.
The pretracheal fascia is fixed between them.
3. Applied anatomy: In tracheostomy, the isthmus of thyroid gland is cut and an opening is made through the 2nd and 3rd tracheal rings
Thyroglossal duct
Introduction: A duct extending from the foramen caecum of tongue to thyroid primordium.
It is present in embryonic life.
It is formed by endoderm of 3rd and 4th pharyngeal arches .
1. Fate: Distal part usually differentiates to form pyramidal lobe of thyroid gland and the remainder part obliterates.
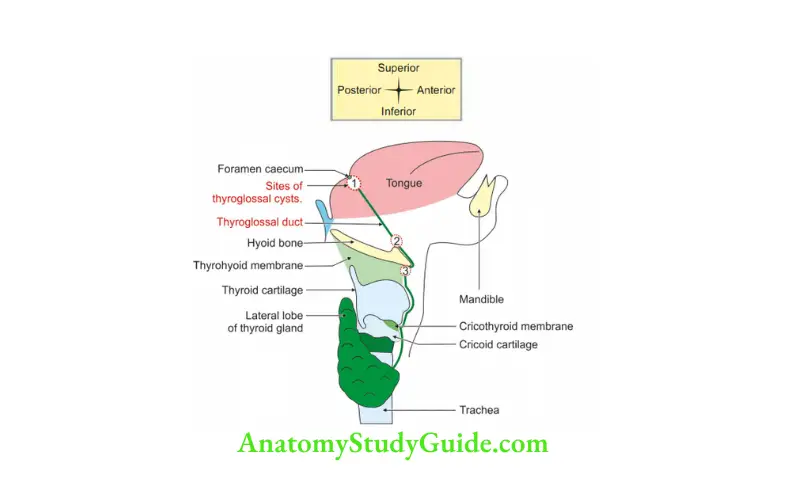
Note: Dotted outlined structure indicates sites of thyroglossal cyst
2. Chronological age: At 7th week of intrauterine life.
3. Applied anatomy: Persistence of fragment of thyroglossal duct results into thyroglossal cysts or fistula.
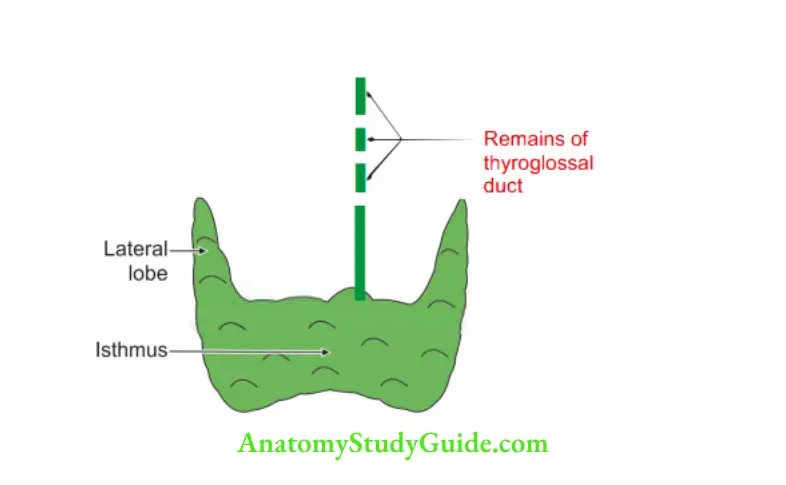
Thyroglossal cyst
1. Aetiology: It results from persistence of a portion of a thyroglossal duct.
2. Incidence: It is the commonest congenital anomaly.
3. Site: Below the level of hyoid bone.
4. Age: It is evident in the late teens presumably because the lining of the thyroglossal duct becomes secretory.
5. Clinical manifestations
- It presents as a swelling along the course of duct.
- The swelling moves with swallowing and when the tongue is protruded out.
- There is recurrence of thyroglossal cyst, if the whole of the thyroglossal duct is not removed.
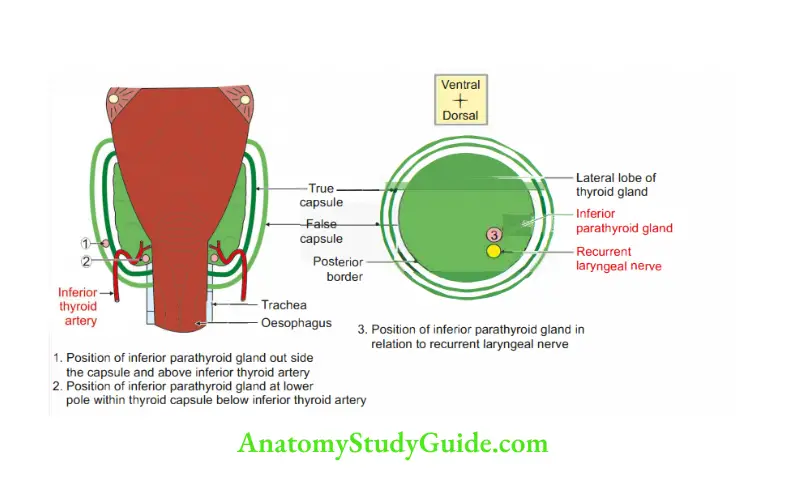
Parathyroid glands
These are two pairs (superior and inferior) of small endocrine glands.
1. Site: On posterior border of lateral lobe of thyroid gland. They are present within the capsule of thyroid gland. I
2. Gross
- Weight: 50 mg each.
- Dimensions: 6 x 4 x 2 mm.
- Position
Superior parathyroid gland
- It is more constant in position.
- It lies at the middle of posterior border of lateral lobe of thyroid gland.
- It lies inside the true capsule and dorsal to recurrent laryngeal nerve.
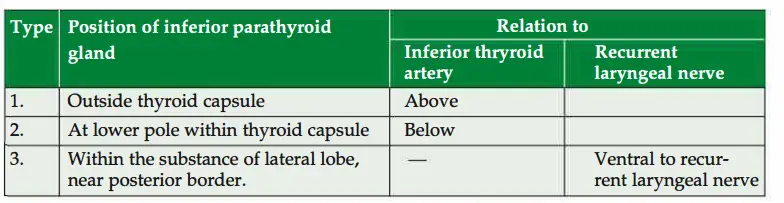
The inferior parathyroid gland
- It is ventral to the recurrent laryngeal ner+ve.
- The position of inferior parathyroid gland is variable.
- The relations of the structures with various positions are shown in.
3. Blood supply: It has rich blood supply.
1. Arterial supply
- Ascending branch of inferior thyroid artery, branch of thyrocervical trunk.
This branch anastomoses with posterior branch of superior thyroid artery. - It also receives blood from anastomotic channel between superior and inferior thyroid arteries.
Venous drainage
- Superior thyroid vein
- Middle thyroid vein } dram. . . . .into internal Jugular vein.
- Inferior thyroid vein drains into left brachiocephalic vein.
4. Applied anatomy
- Tumours of the parathyroid gland enlarge downwards. The descent depends upon the relation of false capsule.
- If tumour is outside the false capsule, it descends in the posterior mediastinum of thorax.
- If tumour is within the false capsule, it descends in the superior mediastinum of thorax.
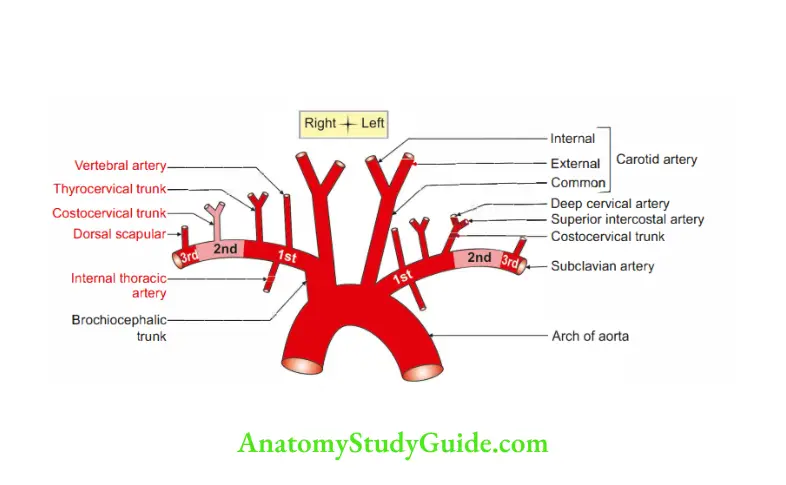
Subclavian artery
Introduction: It is the main artery of upper limb and supplies considerable part of posterior triangle of neck and brain.
1. Origin
- Right subclavian artery arises from brachiocephalic trunk.
- Left subclavian artery arises from arch of aorta.
2. Extent: It extends from stemoclavicular joint to outer border of 1st rib.
At outer border of 1st rib, it continues as axillary artery. u
3. Course and relations: The artery is divided into three parts by scalenus anterior muscle.
- 1st part of subclavian artery is medial to scalenus anterior. (
- 2nd part is posterior to scalenus anterior.
- 3rd part is lateral to scalenus anterior muscle.
4. Branches:
This mnemonic is right for the right side, i.e. VIT for 1st part, C for 2nd part and D for 3rd part. However, on the left side, the branch “C” denoting “Costocervical”arise from 1st part. In that case, there is no branch from 2nd part.
1st part
- Vertebral artery.
- Internal thoracic artery.
- Ihyrocervical trunk which divides into I . .
- Surascapular.
- Inferior thyroid.
- Iransverse cervical.
- Costocervical trunk (on left side).
2. 2nd part: Costocervical trunk (on right side).
3. 3rd part: Dorsal scapular artery.
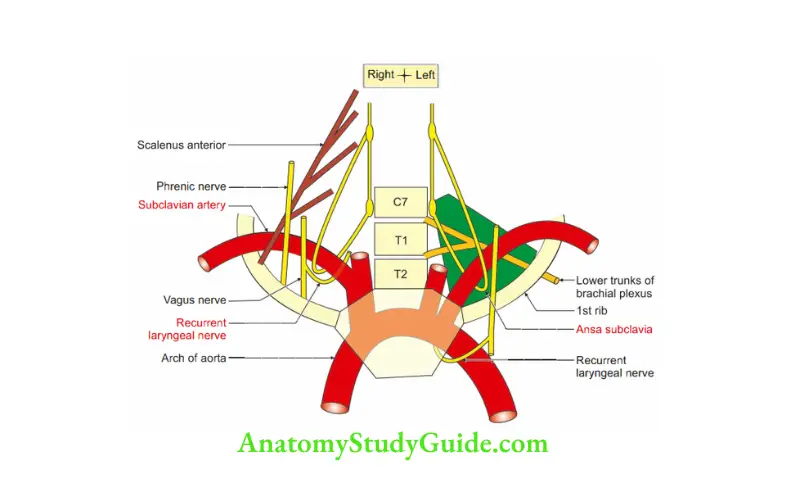
5. Relations
1. 1st part
- Anterior: Ansa subclavia
- Posterior
- Suprapleural membrane,
- Apex of lung, and
- Sympathetic trunk.
- Right recurrent laryngeal nerve winds around the right subclavian artery.
- Lateral: Scalenus anterior muscle.
2. 2nd part: Scalenus anterior is present anteriorly.
3. 3rd part: Scalenus anterior is present medially.
6. Development
Sources:
1. Right subclavian artery is derived from
- Proximal part from the right 4th arch artery.
- Right dorsal aorta cranial to
- Distal part from the right 7th cervical intersegmental artery.
2. Left subclavian artery is developed entirely from the left 7th cervical intersegmental artery.
2. Abnormal right subclavian artery is
Derived by
- Right 7th cervical intersegmental artery
- Right dorsal aorta caudal to right 7th cervical intersegmental artery.
The sources which are disappearing are
- Proximal part from the right 4th arch artery.
- Right dorsal aorta cranial right 7th cervical intersegmental artery
3. Clinical manifestation: The abnormal right subclavian artery goes posteriorly,winds oesophagus and causes dysphagia lusoria.
7. Applied anatomy: Subclavian steal syndrome takes place in obstruction of the subclavian artery proximal to the origin of vertebral artery.
Some amount of blood is stolen from the brain through the opposite vertebral artery.
This is to provide collateral circulation to the affected arm.
This may result in ischaemic neurological symptoms.
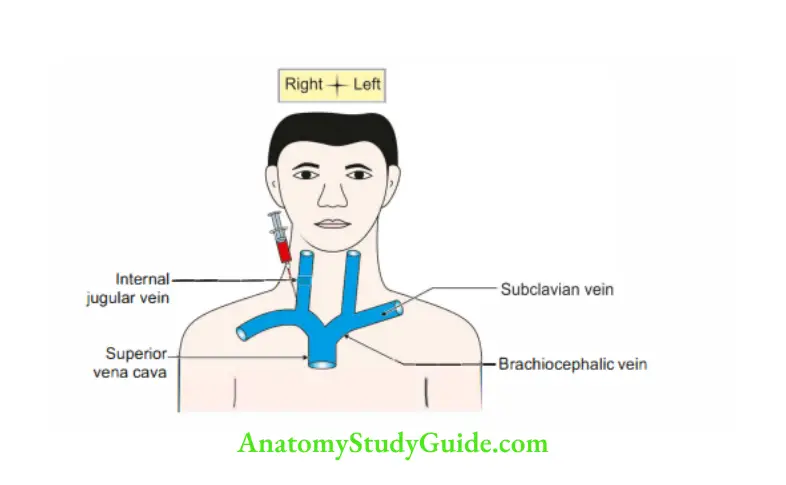
Internal jugular vein
It is direct continuation of sigmoid venous sinus.
1. Extent: It extends from jugular foramen to sternal end of clavicle. It joins the subclavian vein to form brachiocephalic vein.
2. Tributaries
- Inferior petrosal sinus,
- Pharyngeal vein,
- Common facial vein,
- Lingual vein,
- Superior thyroid vein, and
- Middle thyroid vein,
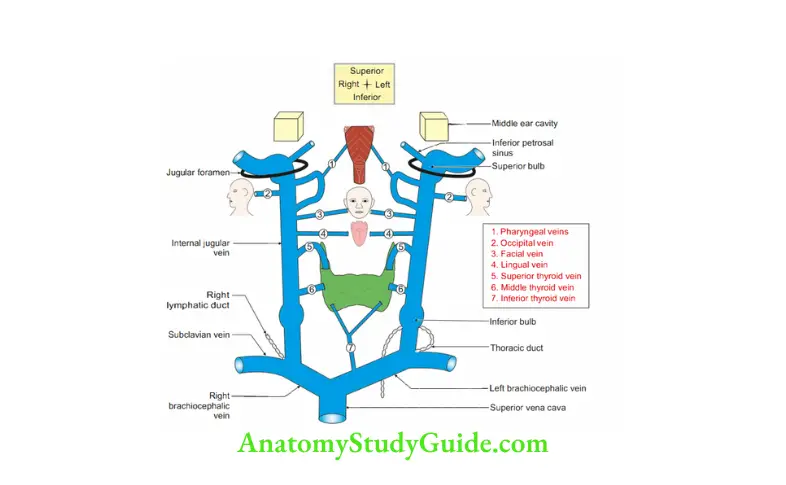
3. Relations
Posteriorly: The relations from above downwards are
- Rectus capitis lateralis,
- Transverse process of atlas,
- Levator scapulae,
- Scalenus medius and cervical plexus of nerves,
- Scalenus anterior and phrenic nerve,
- Thyrocervical trunk,
- 1st part of vertebral artery, and
- 1st part of subclavian artery.
2. Anterolaterally
- It is crossed by superior belly of omohyoid and posterior belly of digastric.
- Below the omohyoid: Stemohyoid and stemothyroid.
3. Medially
- Common carotid artery.
- Vagus nerve.
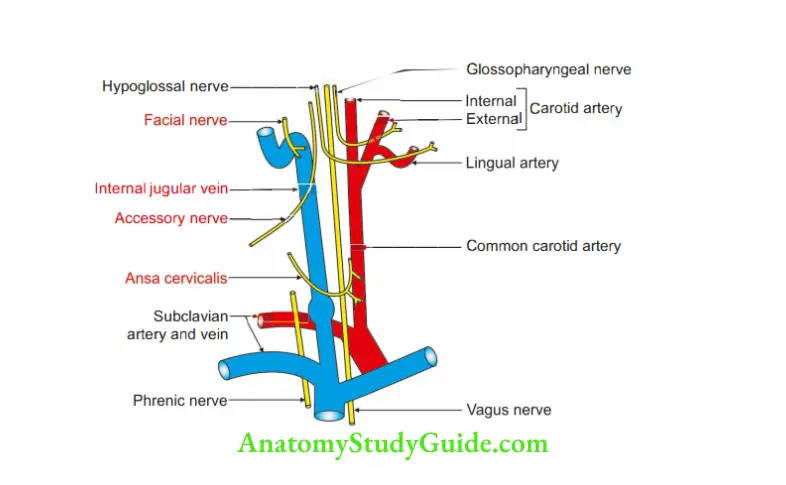
4. Applied anatomy
- The internal jugular vein is accessible deep to the supraclavicular fossa. The vein is used for recording venous pulse pressure .
- In the congestive cardiac failure, the internal jugular vein is most dilated vein.
- The deep cervical lymph nodes lie along the internal jugular vein.
Question 10: Describe glossopharyngeal nerve under the following heads:
1. Functional components,
2. Nuclei,
3. Course and relations,
4. Extracranial course,
5. Branches, and
6. Applied anatomy
Answer: Glossopharygeal nerve: Nerve of 3rd pharyngeal arch
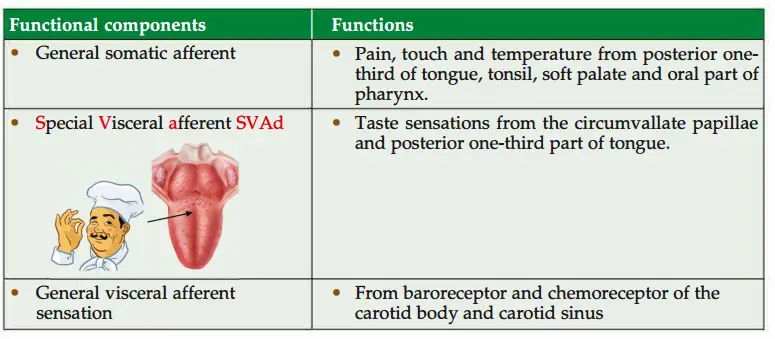
1. Functional components
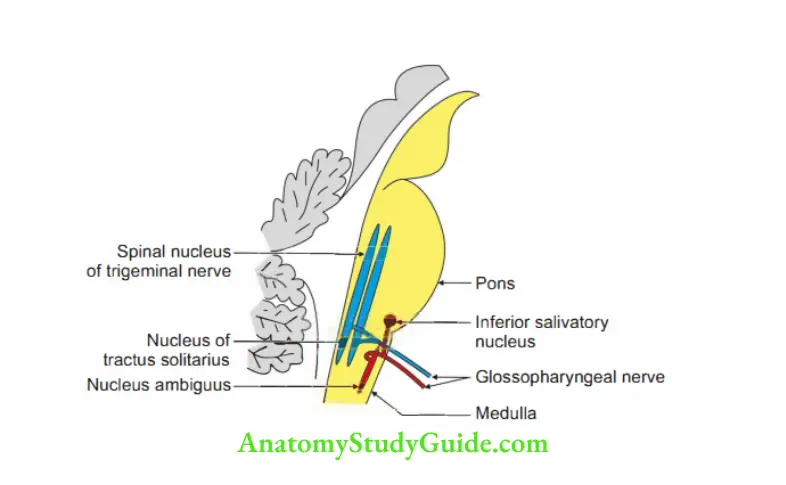
2. Nuclei: The three nuclei in the upper part of medulla are
- Nucleus ambiguus (brachiomotor)
- Inferior salivatory nucleus (parasympathetic)
- Nucleus of tractus solitarius (gustatory)
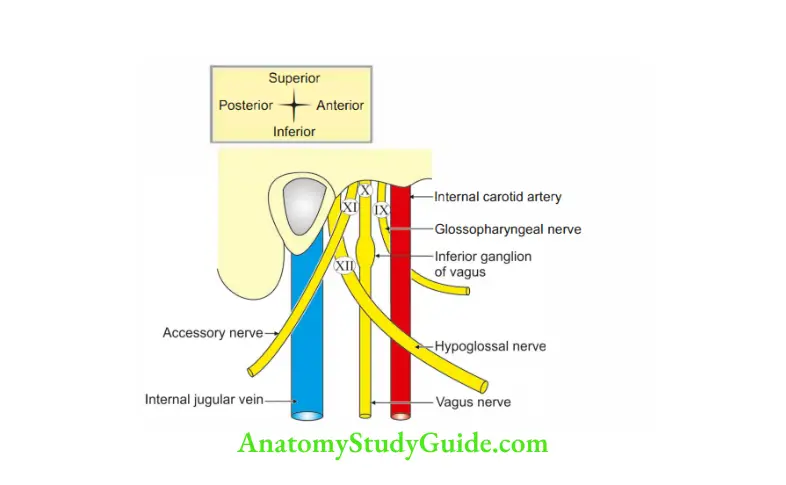
3. Course and relations
1. The nerve arises by 3 to 4 rootlets from posterolateral sulcus of medulla oblongata.
2. It passes through jugular foramen in a separate dural sheath.
3. In the foramen, it has two vessels in front and two behind and two nerves accompanying it.
1. The vessels in front are
- Inferior petrosal sinus, and
- Meningeal branch of ascending pharyngeal artery.
2. The vessels behind are
- Sigmoid sinus, and
- Meningeal branch of occipital artery.
3. The accompanying nerves are
- Vagus, the 10th cranial nerve, and
- Accessory, the 11th cranial nerve.
4. Extracranial course
- The nerve descends between internal jugular vein and internal carotid artery.
- It lies deep to styloid process (i.e. styloid process and the muscles attached to styloid process).
- It passes between external and internal carotid arteries.
- It passes in the gap present between superior constrictor and middle constrictor.
It is accompanied by stylopharyngeus muscle. - It lies on muscles of pharynx.
- Here it gives a pharyngeal branch.
- It enters the submandibular region passes deep to hyoglossus muscle where it breaks up into
- Tonsillar, and
- Lingual branch.
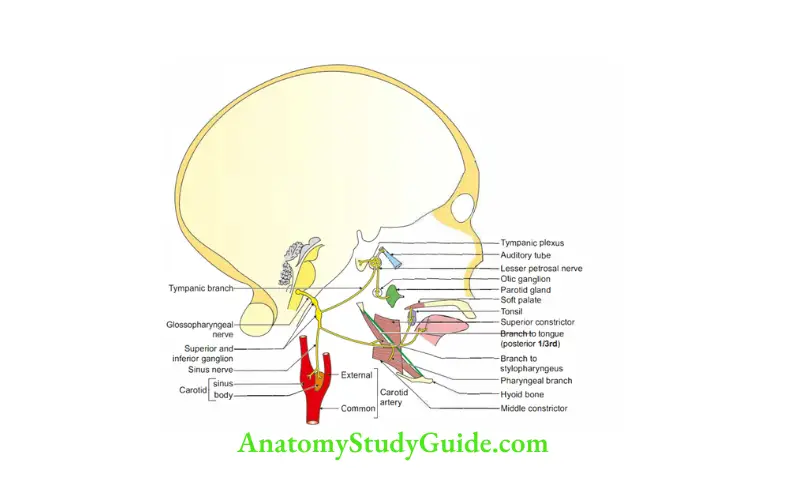
5. Branches
- The word glossopharyngeal indicates glosso = tongue, pharyngeal = pharynx.
- It is sensory nerve of pharynx and tongue.
- It is motor nerve to muscle of pharynx, i.e. stylopharyngeus.
- In addition to this the nerve is renamed as
- Carotico Parotico Tonsili Tympani
- Meaning thereby supplies
- Carotico-Carotid body, and carotid sinus,
- Parotico-Parotid gland,
- Tonsili-Tonsils, and
- Tympani-Middle ear cavity.
1. Tympanic branch
1. It arises from inferior ganglion and enters the tympanic canaliculus in front of the jugular fossa.
2. It reaches the middle ear cavity.
3. It joins with caroticotympanicnerve ( a branch of plexus around internal carotid artery), and form tympanic plexus.NEEr The branches from the plexus are
1. Lesser petrosal nerve: It carries preganglionic parasympathetic fibres to the otic ganglion. It supplies parotid gland.
2. Branch to middle ear cavity: It supplies
- Bony part of eustachian tube,
- Mastoid antrum,
- Mastoid air cells, and
- Tympanic membrane.
2. Muscular branch: Stylopharyngeus muscle.
3. Sinus branch: It arises just below the jugular foramen.
It descends along the internal carotid artery up to the carotid bifurcation and supplies
- Carotid sinus, and
- Carotid body. This branch mediates ‘carotid reflex’.
4. Parotid branch: The lesser petrosal nerve, a branch of tympanic plexus, carries the parasympathetic fibres.
It ends in the otic ganglion where the fibres relay.
Post-ganglionic fibres from the otic ganglion are distributed to the parotid gland through the auriculotemporal nerve.
5. Pharygeal branch supplies
- Fossae,
- Palatine tonsil, and
- Soft palate.
6. Lingual branch carries general and taste sensations from posterior one-third of tongue.
It also carries taste sensations from the circumvallate papillae.
6. Applied anatomy
1. The glossopharyngeal nerve is tested clinically by
- Tickling the posterior wall of pharynx. There is loss of reflex contraction of throat muscle in the lesion of glossopharyngeal nerve.
- Taste sensations from posterior one-third of tongue.
2. Isolated lesion of glossopharyngeal nerve is almost unknown.
3. Following are the features of glossopharyngeal nerve
- Loss of taste sensations in posterior one-third of tongue.
- Patient will have difficulty in swallowing.
- Patient will have decreased secretion from parotid gland.
- Patient will have paralysis of stylopharyngeus muscle.
- Gag reflex will be lost.
4. Whenever an adult complains of constant pain in the middle ear and has no evidence of middle ear disease, a cancer of the pharynx is suspected.
5. Involvement of carotid branch following surgery leads to transient or sustained hypertension.
Question 11: Describe hypoglossal nerve under the following heads:
Answer: 1. Course and relations,
2. Extracranial course,
3. Branches and distribution, and
4. Applied anatomy
1. Course and relations: The rootlets arise from anterolateral sulcus of medulla oblongata.
The nerve leaves the skull through hypoglossal canal.
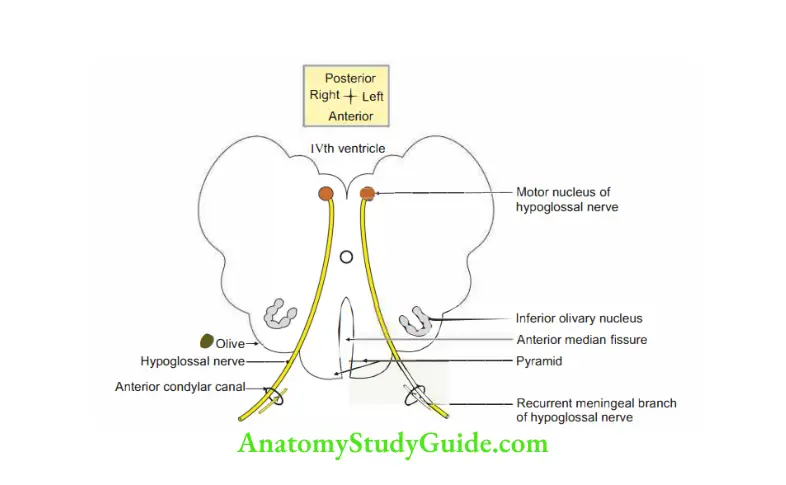
2. Extracranial course
- The nerve 1st lies deep to the internal jugular vein and descends between internal jugular vein and the internal carotid artery.
2. It is present deep to the
- Parotid gland,
- Styloid process and muscles attached to process, i.e. stylohyoid.
- Posterior belly of the digastric and
- Stylohyoid muscle.
3. At the lower border of posterior belly of the digastric, it curves forwards and crosses the internal carotid artery and then external carotid artery. It crosses the loop of lingual artery anteriorly.
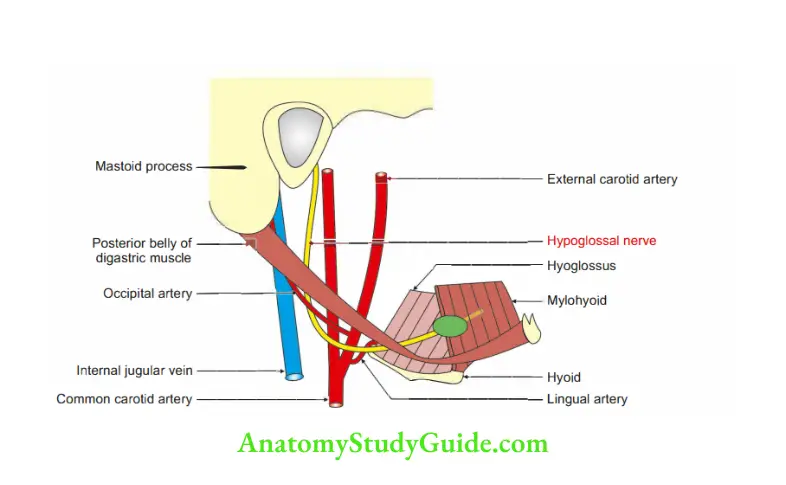
4. The nerve then runs forwards on the hyoglossus and genioglossus muscles.
5. It passes deep to submandibular gland and mylohyoid muscle.
6. It enters the substance of the tongue to supply the muscles of tongue.
7. On the hyoglossus muscle, it is accompanied by two venae comitantes.
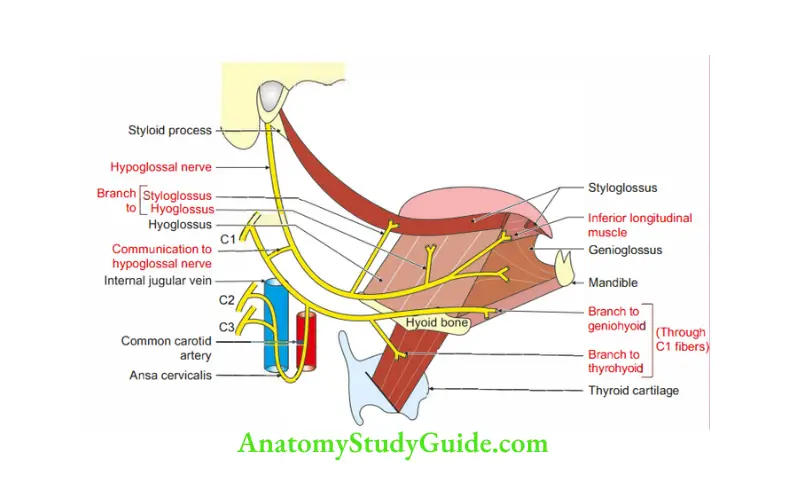
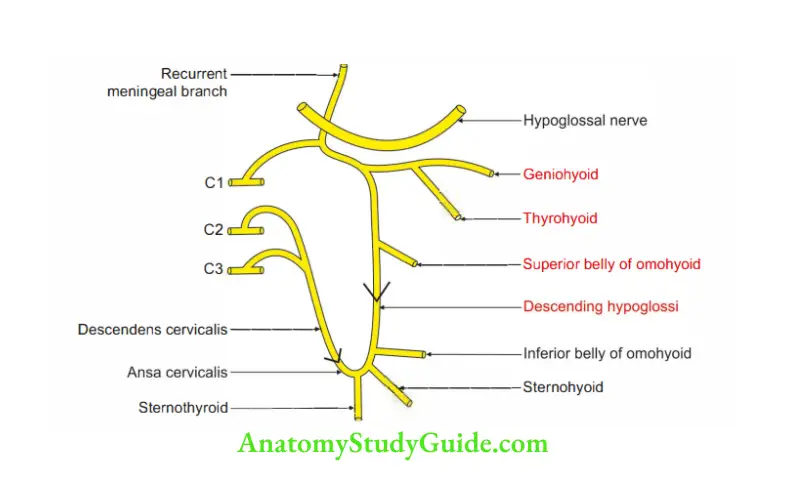
3. Branches and distribution
1. Muscular branches supply intrinsic and extrinsic muscles of the tongue except the palatoglossus, which is supplied by cranial root of accessory nerve.
2. Other branches containing Cl nerve but through hypglossal nerve.
- Meningeal branch.
- Superior root of ansa cervicalis.
- Branches to thyrohyoid and geniohyoid.
4. Applied anatomy
- Hypglossal nerve is tested clinically by asking the patient to protrude th tongue.
- Lesion of the hypoglossal nerve produces protrusion of the tongue to the side of lesion.
The position of the tongue indicates side of the lesion. - If the lesion is infranuclear, there is gradual atrophy on the side of lesion.
Anterior condylar canal (hypoglossal canal)
1. Site: It lies in the posterior cranial fossa.
2. Situation: It lies medial to and below the lower border of jugular foramen. It is at the junction of basilar and condylar part of occipital bone.
3. Transmits
- Hypoglossal nerve.
- Recurrent branch of hypglossal nerve, 12th cranial nerve.
- Meningeal branch of ascending pharyngeal artery (external carotid artery).
- Emissary vein from the basilar venous plexus.
Development of thymus
1. Chronological age: 6th week of intrauterine life.
- It is larger at birth.
- It continuously increases till puberty.
- After puberty, it undergoes atrophy.
2. Germ layer
- Hassall’s corpuscle: It is developed from the ventral part of endodenn of the 3rd pharyngeal pouch.
- Lymphoid tissue is developed from mesoderm of the 3rd pharyngeal arch.
3. Site: Primitive pharynx.
4. Sources: It is very closely associated with the inferior parathyroid gland.
It gets separated from the inerior parathroid gland as the thmic rudiment. This is divided into
- Thinnr portion which forms the cervical part of the thymus.
- Broader portion is divided into two parts, which enters into thorax and forms thoracic part.
These two parts unite with each other by means of connective tissue and the thymus is formed.
5. Anomalies
- DiGeorge syndrome: It is failure of differentiation of 3rd pouch into thymus and parathyroid.
It is associated with hypoplasia or aplasia of thymus and parathyroid glands. It manifests as Immunodeficiency resulting to low grade susceptibility to opportunistic pathogens, and
Low calcium level resulting in tetany. - Abnormal site is the commonest anomaly of thymus. It may remain along the course of development.
- Cervical part of the thymus may get fragmented and give rise to accessory thymic tissue.
Question 12: Describe lymphatic drainage of head, face and neck.
Lymphatics of head, face and neck are classified as
1. Anatomical classification
2. Clinical classification
Answer: 1. Anatomical classification
1. Peripheral group–uter circle
1. Site: Present at the junction of head and neck
2. Groups
1. Submental
- Site: Deep to mylohyoid
- Afferent
- Tip of tongue,
- Incisor teeth, and
- Floor of mouth.
- Efferent: Jugulo-omohyoid
2. Submandibular
- Site: Superficial submandibular gland
- Afferent
- Anterior 2/3rd of tongue,
- Floor of mouth,
- Anterior part of nasal cavity, and
- Teeth.
- Efferent: Jugulo-omohyoid
3. Preauricular (parotid)
- Afferent:
- Forehead,
- Eyelid,
- Temple,
- External ear, and
- Eyelid.
4. Postauricular (mastoid)-middle ear
5. Occipital:
- Afferent: Posterior part of scalp,
- Efferent: Deep cervical
2. Deep circle-inner circle
1. Site: Deep to investing layer of deep cervical fascia
2. Groups
- Pretracheal / prelaryngeal
- Retropharyngeal
3. Inner to inner circle: Mucosa associated lymphoid tissue (Waldeyer’s ring)
1. Site: Submucosal aggregation of lymphoid tissue.
2. Groups:
- Lingual tonsil,
- Palatine tonsil,
- Tubal tonsil, and
- Adenoids (pharyngeal tonsil).
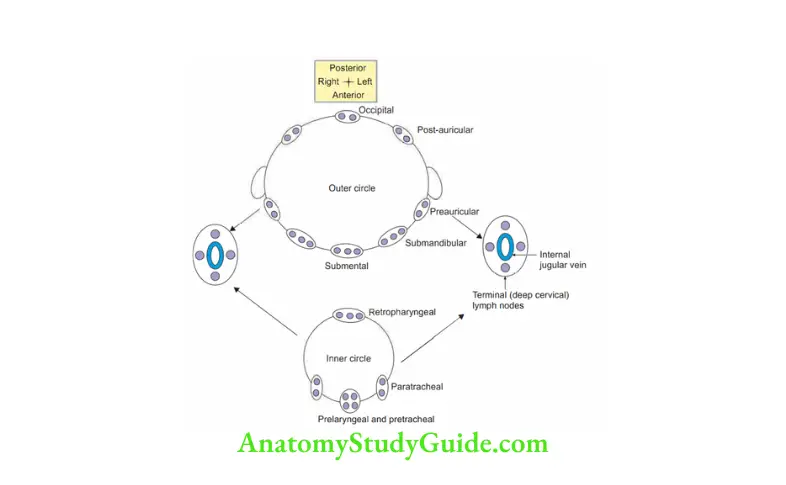
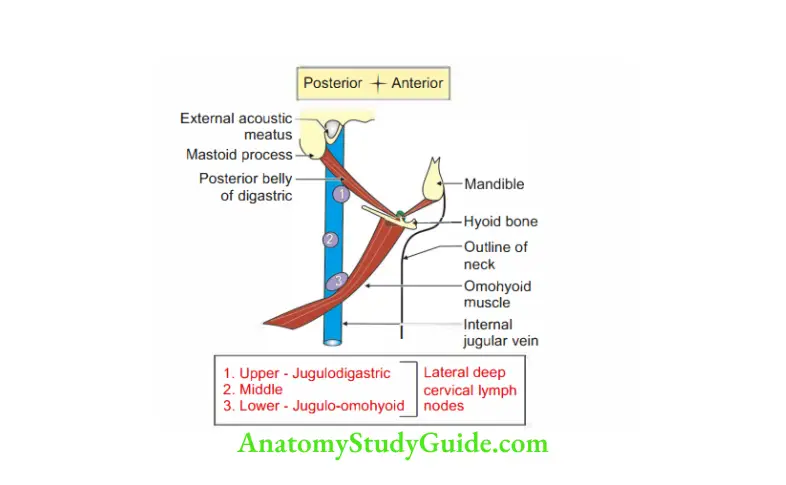
4. Deep cervical lymph nodes
1.Jugulodigastric nodes: The node of tonsil
Site: Triangular area present between
- Internal jugular vein
- Common facial vein
- Posterior belly of digastric muscle
Area: Tonsil
2. Jugulo-OmoHyoidNode-JOHN-means-Tongue.
- Site: Area above the intermediate tendon of omohyoid on internal jugular vein
- Area: Tongue
3. Efferents: Deep cervical lymph nodes.
- Right deep cervical node drain to right lymphatic duct.
- Left deep cervical node drain to thoracic duct.
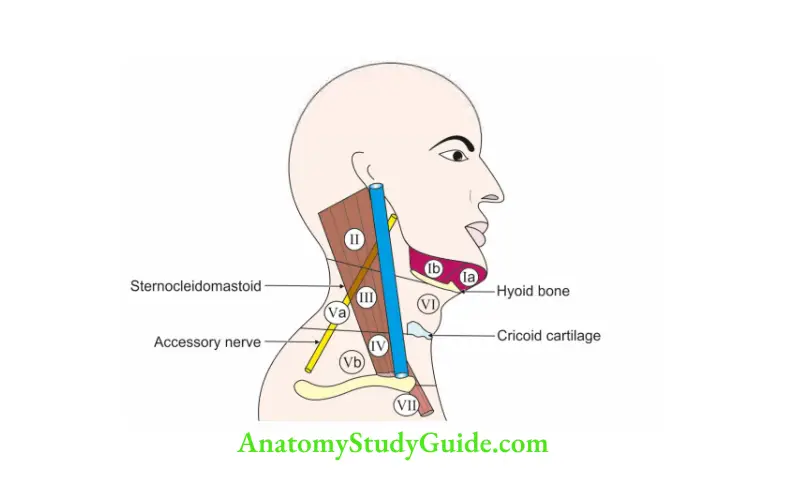
2. Clinical classification of lymph nodes is based on involvement of lymph nodes at various levels.
1. Level I lymph
- Ia: Submental
- lb: Submandibular
2. Level II: Upper jugular-upper part of internal jugular vein
3. Level III: Midjugular-middle part of internal jugular vein
4. Level IV: Lower jugular-lower part of internal jugular vein
5. Level V: Lymph nodes are present in posterior triangle.
They are associated with spinal accessory nerve.
- Va
- Vb
6. Level VI: Lymph nodes are situated between hyoid bone to sternum.
They are present in anterior triangle.
7. Level VII: Supramediastinal lymph nodes.
All these lymph nodes ultimately drain in deep cervical lymph nodes: Jugulodigastric and jugulo-omohyoid lymph nodes.
3. Deep Structure in the Neck 229
Level I lymph
Ia: Submental
lb: Submandibular
Level II: Upper jugular-upper part of internal jugular vein
Level III: Midjugular-middle part of internal jugular vein
Level IV: Lower jugular-lower part of internal jugular vein
Level V: Lymph nodes are present in posterior triangle.They are associated with spinal accessory nerve.
Level VI: Lymph nodes are situated between hyoid bone to sternum.They are present in anterior triangle.
Level: Supramediastinal lymph nodes.
All these lymph nodes ultimately drain in deep cervical lymph nodes: Jugulodigastric and jugulo-omohyoid lymph nodes.
Applied anatomy
1.In radical neck dissection, the surgeons remove following structures
- All lymph nodes,
- Sternocleidomastoid,
- Internal jugular vein, and
- Spinal root of accessory nerve.
2. In modified radical neck dissection, surgeons remove all lymph nodes sparing
- Sternocleidomastoid
- Internal jugular vein
- Spinal root of accessory nerve
Leave a Reply