Root Resorption Introduction
Resorption is a condition associated with either a physiologic or a pathologic process resulting in a loss of dentin, cementum, and/or bone.
Table of Contents
It causes loss of the tooth structure either internal or external which may lead to extraction of the tooth if not treated well at the time.
There are many classifications and terms coined for resorption defects depending upon their location and etiology.
Read And Learn More: Endodontics Notes
The etiology of any resorption defect is inflammation which starts from injury in form of dental trauma, surgical procedures, chemical injury from bleaching agents or excessive pressure from an impacted tooth.
A tooth can be saved if treatment is given at the initial stage but if resorption continues without treatment, it may lead to extraction of the tooth.
Identification of stimulating factors and removal of the etiology are the requirements to render proper treatment to the tooth undergoing resorption.
Root Resorption Definition
According to the American Association of Endodontics in 1944 (Glossary—Contemporary Terminology for Endodontics), resorption is defined as “A condition associated with either a physiologic or a pathologic process resulting in the loss of dentin, cementum or bone.”
Root resorption is the resorption affecting the cementum or dentin of the root of tooth. Resorption is a perplexing problem for which etiologic factors are vague.
External Root Resorption: When resorption is initiated in the periodontium and initially affects the external surface of the tooth.
Internal Root Resorption: When resorption is initiated within the pulp space affcting the internal dentin surface.
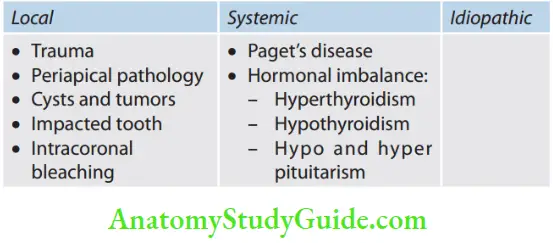
Etiology of Root Resorption
Classification of Resorption (Flowchart)
1. Cohen’s classification of root resorption
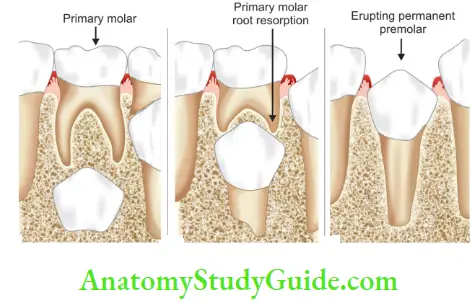
- According to nature
- Physiologic [(in deciduous teeth during the eruption of permanent teeth]
- Pathologic (in teeth due to underlying pathology)
- According to the anatomic region of occurrence
- Internal
- External
- Based on cause
- Local
- Inflammatory
- External
- Internal
- Pressure
- Orthodontic tooth movement
- Impacted tooth
- Dentoalveolar ankylosis
- Inflammatory
- Local
- Systemic
- Idiopathic
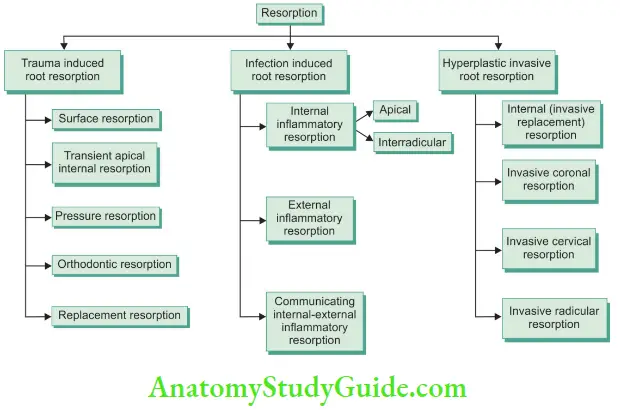
Andreasen classification of root resorption
Internal resorption
- Root canal replacement resorption
- Internal inflammatory resorption
External resorption
- Surface resorption
- Inflammatory resorption
- Replacement resorption
- Dentoalveolar ankylosis
Protective Mechanism Against Resorption
There are a few hypotheses that tell the protective mechanism against resorption. These are as follows.
Remnant of Epithelial Root Sheath
Remnants of epithelial root sheath surround the roots like a net and impart resistance to resorption and subsequent ankylosis
Intrinsic Factors
Intrinsic factors found in dentin and cementum act as inhibitors of resorption
Presence of Osteoprotegerin (OPG)
OPG a member of tumor necrosis factor (TNF) binds to the receptor activator of NF-κB ligand and reduces its concentration and further inhibiting its ability to stimulate osteoclast production (osteoclastogenesis) and subsequently inhibiting resorption
Anti-Invasion Factors
Low-molecular-weight proteolytic activity inhibitor is present in cartilage, blood vessel walls, and teeth.
It causes loss of ruffled border, attachment ability of osteoclasts to the bone, and thus bone resorption.
Intermediate Cementum
The presence of a hyaline layer of Hopewell-Smith (intermediate cementum) is hypercalcemia in relation to adjacent dentin and cementum.
It prevents the development of inflammatory resorption in replanted teeth with pulpal pathosis, possibly by forming a barrier against the egress of noxious agents from the dentinal tubules to the PDL.
Anti-Resorptive Factors
Like estrogen, calcitonin, platelet-derived growth factor, calcium, tumor growth factor, interleukin,-17, etc.
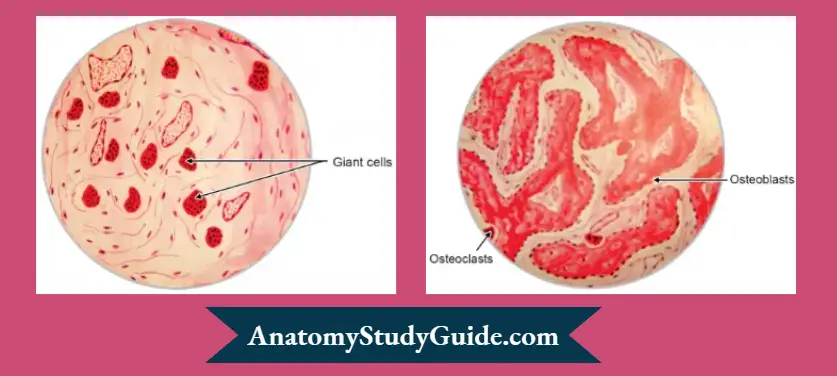
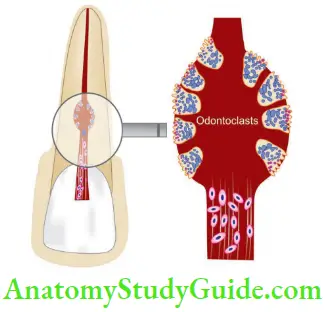
Cells Involved In Root Resorption
- Clast Cells
Odontoclasts, Dentinoclasts, Osteoclasts, and Cementoclasts
All these cells belong to the group of clast cells and they have a common origin, that is, circulating monocytes that form macrophages.
When the inflammation gets out of control, these monocytes/macrophages join to form giant cells. These are highly vacuolated and contain numerous mitochondria.
The majority of odontoclasts have 10 or fewer nuclei, that is, 96% are multinucleated and the rest 4% are mononucleated.
Oligonuclear odontoclasts are cells with <5 nuclei. They resorb more dentin per nucleus when compared with cells with a higher number of nuclei.
Monocytes and Macrophages
Monocytes and macrophages along with osteoclasts are found in tissue surfaces adjacent to bone, for example, in resorption surfaces of rheumatoid arthritis, periodontal diseases, periradicular granulomas, cysts, and in metastatic bone tumors.
Though macrophages have structures similar to osteoclasts and like osteoclasts, can become multinucleated giant cells, macrophages lack a ruffle border, that is, attached to hard tissue substrates during resorption and do not create lacunae on the dentinal surface.
Mechanism of Root Resorption
Resorption of hard tissue takes place in two events:
- Degradation of inorganic crystal structures—hydroxyapatite
- Degradation of the organic matrix—principally Collagen Type 1
Degradation of the Inorganic Crystal Structures
The degradation of inorganic structures initiates when pH is 3–4.5 at the site of resorption.
This is created by the polarized proton pump formed in the ruffled border of the clast cells.
Below the pH of 5, the dissolution of hydroxyapatite occurs.
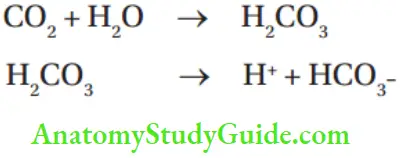
Enzymes carbonic anhydrase II which catalyzes the conversion of CO2 and H2CO3 intracellularly also maintains an acidic environment at the site of resorption which is a readily available source of H+ ions. The enzyme acid phosphatase also favors the resorption process.
Degradation of the Organic Matrix
Three main enzymes involved in this process are collagenase, matrix metalloproteinases (MMP), and cysteine proteinases.
Collagenase and MMP act at a neutral or just below neutral pH—7.4. They are found more toward the resorbing bone surface where the pH is near neutral, because of the presence of the buffering capacity of the resorbing bone salts.
MMP is more involved in odontoblastic action.
Cysteine proteinases are secreted directly into the osteoclasts into the clear zone via the ruffl border.
Cysteine proteinases work more in an acidic pH and near the ruffl border, the pH is more acidic.
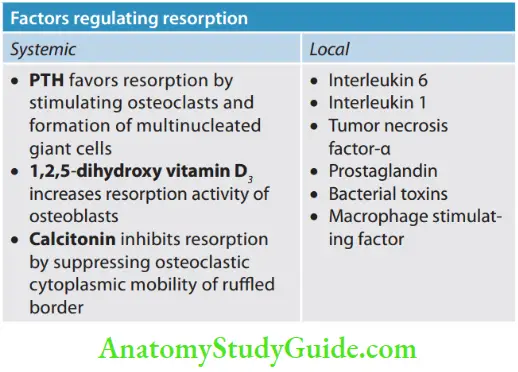
Factors regulating resorption
Diagnosis of Resorption
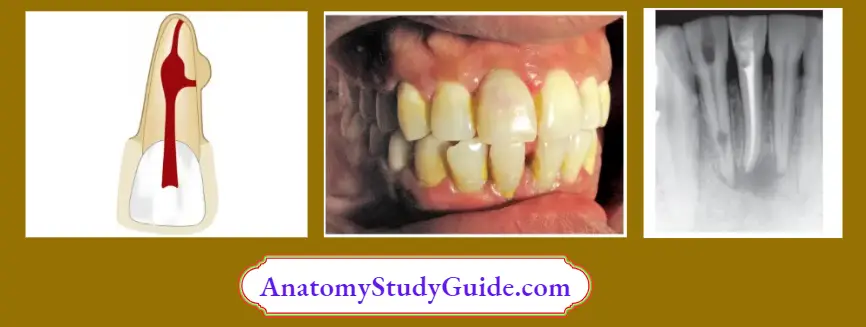
Root Resorption Clinically: Pink spot in case of internal resorption
Root Resorption Imaging
- Conventional radiograph
- Digital radiographs
- CT scan
- The rapid prototyping tooth model
- Cone beam computed tomography (CBCT)
Root Resorption Vitality testing
If a tooth is vital: Internal root resorption or subepithelial external root resorption.
If a tooth is nonvital: External inflammatory root resorption with infected pulp or internal root resorption with necrotic coronal pulp.
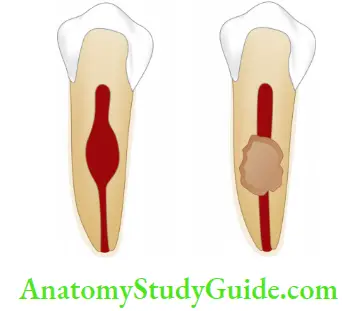
Internal Resorption
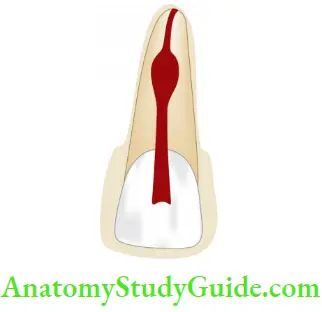
According to Shafer, “internal resorption is an unusual form of tooth resorption that begins centrally within the tooth, apparently initiated in most cases by a peculiar inflammation of the pulp.” It is characterized by oval-shaped enlargement of root canal space.
Synonyms of Internal Resorption
- Chronic perforating hyperplasia of the pulp
- Internal granuloma
- Odontoblastoma
- Pink tooth of mummery
Internal Resorption Etiology
Though etiology is unknown but it is most often seen in the following cases:
- Long-standing chronic inflammation of the pulp
- Caries-related pulpits
- Traumatic injuries
- Luxation injuries
- Iatrogenic injuries
- Preparation of tooth for a crown
- Deep restorative procedures
- Application of heat over the pulp
- Pulpotomy using Ca(OH)2
- Idiopathic
Internal Resorption Clinical Features
- Internal root resorption is usually asymptomatic until the root is perforated. It is detected coincidentally by routine radiographs
- The patient may complain of pain when the lesion perforates and tissue is exposed to oral fluids
- The most commonly affected teeth are maxillary central incisors
- Usually single tooth is involved but sometimes multiple teeth are also involved
- It occurs in permanent as well as in deciduous teeth. In primary teeth, it spreads more rapidly
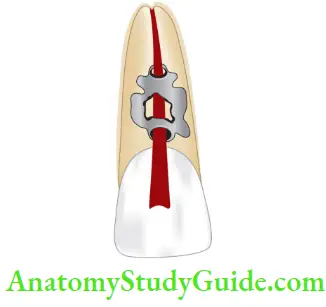
- Granulation tissue can clinically manifest itself as a “pink spot” where crown dentin destruction is severe leading to pink tooth appearance.
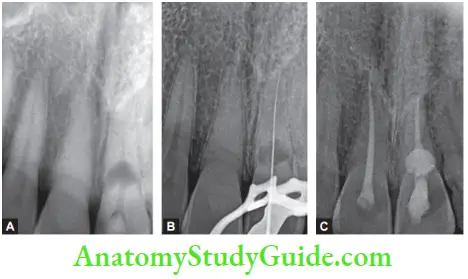
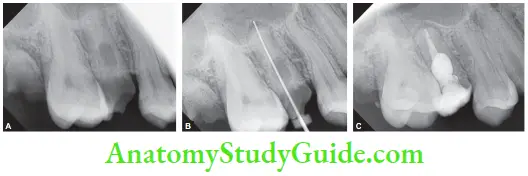
Radiographic Features
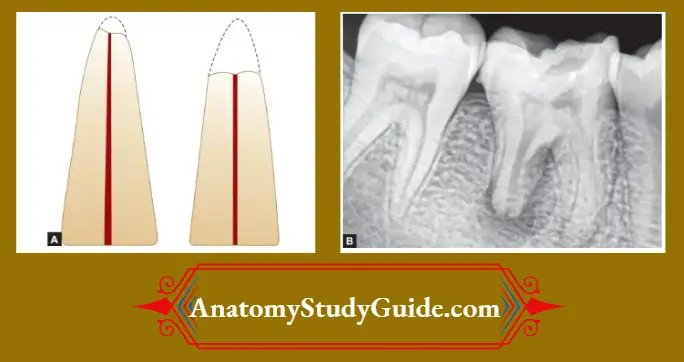
Radiographic Outline of lesion: Lesion appears as uniform, round-to-oval radiolucent enlargement of the pulp space.
Radiographic Outline of root canal: There is a distortion of the original root canal outline.
Radiographs are taken from different angles to show the resorptive lesion in the central location.
Types of Internal Resorption
- Internal replacement resorption
- Internal inflammatory resorption
Internal Replacement Resorption (Metaplastic Resorption)
Resorption of dentin and subsequent deposition of hard tissues are found that resemble bone or cementum or osteopontin, but not dentin.
They represent areas of destruction and repair. This occurs mainly due to low-grade irritation of pulpal tissue.
Internal Replacement Resorption (Metaplastic Resorption) Etiology
- Trauma
- Extreme heat to the tooth
- Chemical burns
- Pulpotomy procedures
Internal Replacement Resorption (Metaplastic Resorption) Radiographic Features
Radiographically, the tooth shows an enlargement of the canal space. This space is later gets engorged with a material of radiopaque appearance giving the expression of hard tissue.
Internal Replacement Resorption (Metaplastic Resorption) Histopathology
Histological studies of internal resorption demonstrate the replacement of normal pulp tissue by a periodontal-like connective tissue with both osteogenic and resorptive potential.
Origin of metaplastic Hard Tissue
- Metaplastic hard tissue formed in replacement resorption is produced by postnatal dental pulp stem cells present in the apical part of root canal as a reparative response to restorative insult
- Both granulation tissue and metaplastic hard tissue are non pulpal in origin and might be derived from cells that transmigrated from the vascular compartment from periodontium.
Internal Inflammatory Resorption
This is that form of internal resorption in which progressive loss of dentin is present without deposition of any form of hard tissue in the resorption cavity.
Pathophysiology
- Long-standing injury leads to chronic pulp inflammation and circulatory changes within the pulp. Active hyperemia with high oxygen pressure supports and induces the osteoclastic activity
- Electric activity Piezoelectricity arising due to increased blood flow adds to the resorptive process
- Sudden trauma leads to intrapulpal hemorrhage, which later organizes to form clots and forms the granulation tissue.
- Proliferating granulation tissues compress the dentinal walls and stimulate the formation of odontoblasts which differentiate from the connective tissue. Then, the resorption process starts.
- According to Heithersay, the internal resorption may result from collateral blood supply via an interconnecting large accessory canal, which provides a vascular bed for the process
Internal Inflammatory Resorption Clinical Features
Clinical characteristics of internal root resorption are dependent on the development and location of the resorption.
- It is asymptomatic in most of cases, but when resorption is actively progressing, it may present symptoms of pulpitis
- If it occurs in or near the crown, a pinkish or reddish color is seen through the crown and appears gray/dark gray if the pulp becomes necrotic
- In advanced cases of resorption, perforation of the root is usually followed by the development of a sinus tract
- Internal resorption is active only in teeth where a part of the pulp remains vital. Therefore, pulp tests may show different responses, a positive pulp test if the coronal pulp is vital, or a negative pulp test if the coronal pulp becomes necrotic while the apical pulp is vital
Internal Inflammatory Resorption Radiographic Features
It presents a round or ovoid radiolucent area in the central portion of the tooth with smooth well-defied margins. The defect does not change its relation to the tooth when the rays are projected from an angulation.
Internal Inflammatory Resorption Histology
Pulp tissue shows chronic inflammation reaction and resorption lacunae irregularly occupied by “dentinoclasts” similar to osteoclasts. The granulation tissue present in this type of resorption is highly proliferating in nature.
Internal Inflammatory Resorption Classification
Internal inflammatory resorptions may be classified according to location as
- Apical
- Intraradicular
Apical internal inflammatory resorption
- Seen in teeth with inflammatory periapical pathologies
- Management: There are two approaches to the endodontic management of apical internal resorption:
- To extend instrumentation only to the position of the resorption with the expectation that removal of microorganisms followed by root canal filing, hard tissue repair will occur in the resorbed apical region of the tooth
- To enlarge and prepare the apical region, either with hand or rotary firing techniques, to include the resorbed region and then root files to the root canal “terminus”
Intraradicular inflammatory resorption
- Internal resorption fully contained within an otherwise intact root will be referred to as intraarticular internal inflammatory resorption
- Ths can be recognized as round- or oval-shaped radiolucencies contained within the root
- A common finding is a large accessory canal communicating from the periodontal ligament to the resorbed area; this may have allowed the passage of a collateral blood supply which probably played an important role in the development and maintenance of the internal resorptive process
- Treatment is endodontic therapy. The obturation of the canal can be done by using vertically condensed gutta-percha, obtura, or micro seal technique
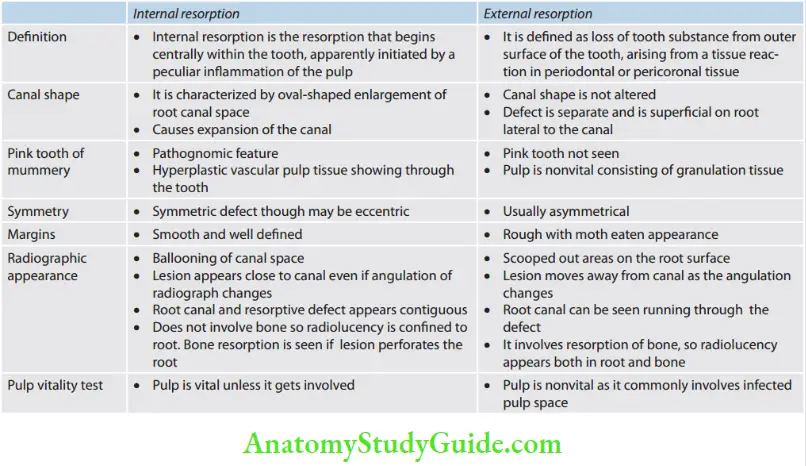
Differences Between Internal And External Resoration
Management of Internal Root Resorption
- Early diagnosis is important to prevent the weakening of the remaining root structure by the resorptive process
- Conventional root canal therapy should be instituted as soon as the diagnosis of internal resorption is made
- If the apical third is not involved, then the cases are treated as usual and the resorbed area is filed with the warm gutta-percha technique
- Teeth with perforation often need both surgical and nonsurgical procedures
Treatment options in teeth with internal resorption
- Without perforation: Endodontic therapy
- With perforation
- Nonsurgical: Ca(OH)2 therapy—obturation
- Surgical:
- Surgical flap
- Root resection
- Intentional replantation
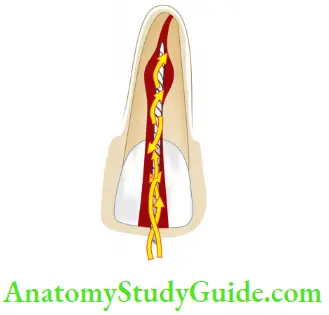
Management of Nonperforating Resorption
Pulp removal and canal preparation: Removal of all, inflamed tissue from the resorptive defect is the basis of the treatment.
But sometimes complete extirpation of the inflamed tissue may become difficult by hand instruments.
Evidence shows that ultrasonic instruments can give better results as compared to hand instruments. Ultrasonic vibration is unparalleled in its ability to enhance cleaning with irrigant.
Canal obturation: Because of the size, irregularity, and inaccessibility of the resorption defects, obturation of the canal may be technically difficult.
The canal apical to the defect is filled with solid gutta-percha while the resorptive area is usually filled with material that will fill in the irregularities.
The warm gutta-percha technique, thermoplasticized gutta-percha technique, and the use of chemically plasticized gutta-percha are methods of obturation to be used.
Various materials used include:
- MTA
- Glass ionomer cement
- Super EBA
- Hydrophilic plastic polymer (2-hydroxyethyl methacrylate with barium salts)
- Zinc oxide eugenol and zinc acetate cement
- Amalgam alloy
- Thrmoplasticized gutta-percha administered either by injection or condensation techniques
Management of Perforating Internal Resorption
When the internal root resorption has progressed through the tooth into the periodontium, there are additional problems of periodontal bleeding, pain,and difficulty in obturation.
The presence of perforation cannot be determined radiographically unless a lateral radiolucent lesion is present adjacent to the lesion.
Clinically in some cases, a sinus tract may be present and there will be continued hemorrhage in the canal after the pulp is removed.
Nonsurgical repair
Indications of nonsurgical repair:
- When the defect is not extensive
- When defect is apical to epithelial attachment
- When hemorrhage can be controlled
In this technique, after thorough cleaning and shaping of the canal, the intracanal calcium hydroxide dressing is placed and over it a temporary filling is placed to prevent interappointment leakage.
The patient is recalled after 3 months for the replacement of calcium hydroxide dressing and for radiographic confirmation of the barrier formation at the perforation site.
Afterward, 2 months of recall visits are scheduled until there is a radiographic barrier at the resorption defect. After the barrier is formed, the canal is obturated with gutta-percha as in the non perforating internal resorption.
Surgical repair
If it is not possible to get access to the lesion through the canal, surgical repair of the defect should be considered.
Treatment options in surgical repair can be
Surgical flap: The defect is exposed to allow good access. The resorptive defect is curetted, cleaned, and restored using an alloy, composite, glass ionomer cement, super EBA, MTA, dentine, etc. Final obturation is done using gutta-percha
Root resection: If the resorbed area is located in the apical third, the root may be resected coronal to the defect and the apical segment is removed afterward.
Following root resection, retrofitting is done. If one root of a multirooted tooth is affected, root resection may be considered based on anatomical, periodontal, and restorative parameters
Intentional replantation: If the perforating resorption with minimal root damage occurs in an inaccessible area, intentional replantation may be considered.

External Root Resorption
External root resorption is defined as loss of tooth substance from the outer surface of the tooth, arising from a tissue reaction in periodontal or pericoronal tissue.
External Root Resorption Classification
According to Rita F Ne, Gutman et al. (Quintessence International, 1999), external resorption is of three types:
- Surface resorption
- Inflammatory root resorption
- Replacement resorption
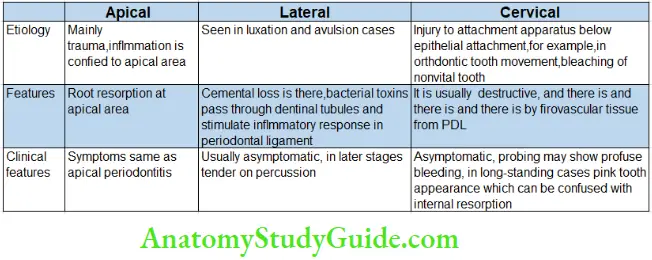
According to Cohen, on the basis of the location:
- Cervical
- Lateral
- Apical
External resorption may be found in the following conditions:
- Periodontal disease
- Luxation injuries
- Hypoparathyroidism
- Hyperparathyroidism
- Turner syndrome
- Paget disease
- Gaucher disease
- Radiation therapy
Surface Resorption
External surface resorption is a transient phenomenon in which the root surface undergoes spontaneous destruction and repair.
It is the least destructive form of external root resorption and is a self-limiting process; hence, it requires no treatment.
Surface Resorption Etiology
- As part of the repair process
- Indirect physical injury, caused by physiologic function, to localized areas of periodontal ligament or cementum on the root surface
- In trauma, it occurs because of direct mechanical contact of the root surface and alveolar bone proper
Surface Resorption Clinical Evaluation
No significant signs of external surface resorption are detectable on the supragingival portion of the tooth.
Surface Resorption Radiographic Evaluation
External surface resorption is usually not visible on radiographs because of its small size.
Later, it appears as small excavations on the lateral surface or at the root apex resulting in the appearance of shorter roots.
Histologic Evaluation
Small, superficial lacunae in the cementum and outermost layer of dentin are seen which are simultaneously being repaired with new cementum.
Histologic Evaluation Classification
Surface resorption can be
- Transient
- Progressive
Transient surface resorption: In this type, the tooth has a vital, healthy pulp that has recovered from a traumatic event.
In such cases, the resorbed area will be restored completely to normal surface contour by deposition of new cementum.
Progressive surface resorption: In this type, surface resorption is the beginning of more destructive resorption, either inflammatory resorption or replacement resorption.
Histologic Evaluation Classification Treatment
No treatment is indicated.
External Inflammatory Root Resorption
It is the most common and most destructive type of resorption and is thought to be caused by the presence of infected or necrotic pulp tissue in the root canal.
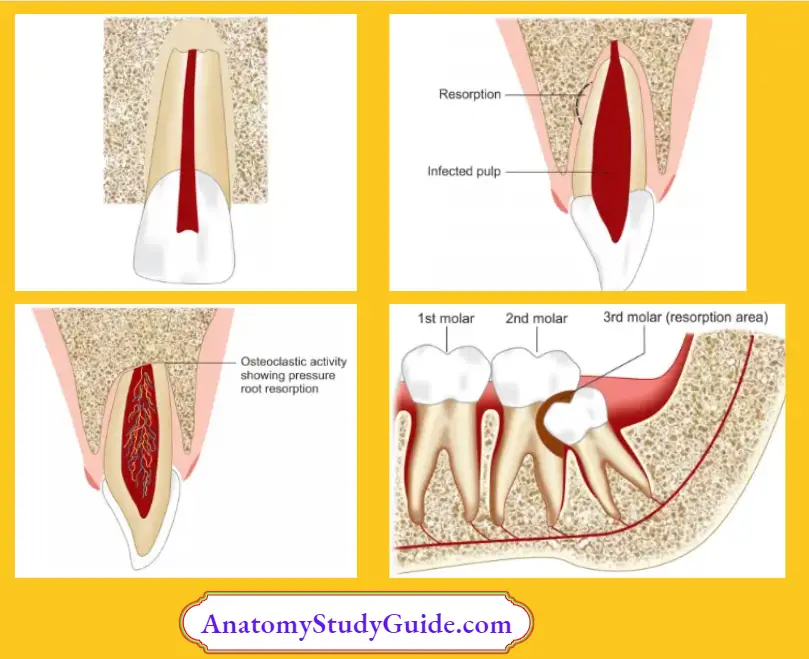
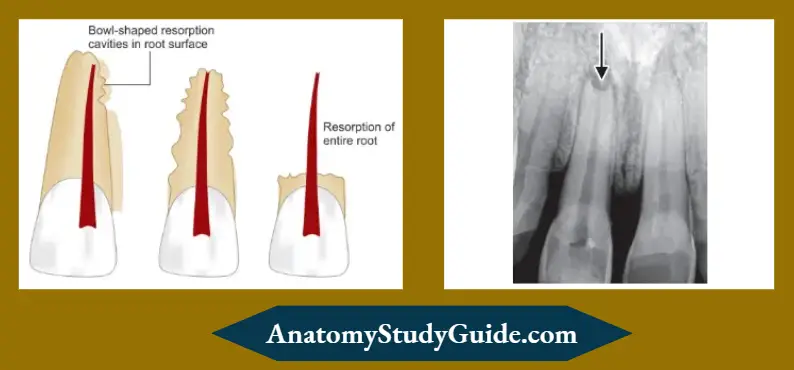
It is best described as a bowl-shaped resorptive defect that penetrates the dentin.
External Inflammatory Root Resorption Etiopathology
- Injury or irritation to the periodontal tissues where the inflammation is beyond repair
- Trauma leads to pulpal necrosis which may further cause periodontal inflmmation due to the passage of the toxins and microorganisms from the infected pulp, lateral canals, apical foramen, accessory canals, dentinal tubules where there is a discontinuity of cementum
- Orthodontic tooth movement using excessive forces
- Trauma from occlusion—leading to periodontal inflmmation
- Avulsion and luxation injuries
- Pressure resorption occurring from pressure exerted by tumors, cysts and impacted teeth
- In the initial stages, bowl-shaped lacunae are seen in cementum and dentin, if not controlled, it may resorb the entire root in latter stages
External Inflammatory Root Resorption Clinical Features
- The patient gives history of trauma
- Signs of necrotic pulp/irreversible pulpitis
- The tooth is usually mobile
- Inflammation of periodontal tissue
- Percussion sensitivity is present
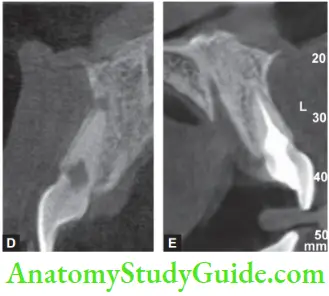
External Inflammatory Root Resorption Radiographic Features
Bowl-like radiolucency with ragged irregular areas on the root surface is commonly seen in conjunction with loss of tooth structure and alveolar bone. Small lesions of external root resorption usually go undetected.
Histologic Evaluation
Histologically, EIRR is represented by a bowl-shaped resorption area into cementum and dentin with inflmmation of adjacent periodontal tissue and infected or necrotic pulp in the root canal
Histologic Evaluation Treatment
Treatment of external inflammatory root resorption is dependent on the etiology:
- If it is because of orthodontic treatment, remove the pressure of orthodontic movement to arrest resorption
- In cervical resorption
- If the pulp is vital and treatment of cervical resorption is unlikely to cause pulpal injury, restore the defect and carry on baseline thermal and electrical pulp tests for records
- If treatment of the cervical resorption is likely to cause pulpal injury, restore the defect and perform endodontic treatment
- If pulp is nonvital, restore the defect and perform endodontic treatment. If required, calcium hydroxide dressing is also given
- In case of infected gingival tissues, remove plaque and calculus and maintain periodontium
- Calcitonin can also be used as an interim root canal medicament to assist in the inhibition of osteoclastic bone and dentin resorption
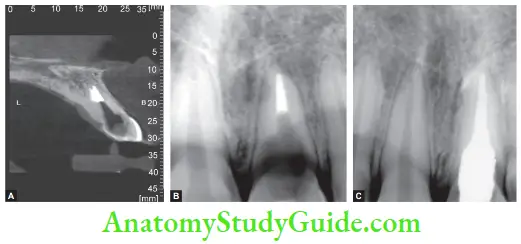
Replacement Resorption/Dentoalveolar Ankylosis
This is similar to ankylosis, but there is the presence of an intervening inflamed connective tissue, always progressive and highly destructive.
In this, tooth becomes a part of the alveolar bone remodeling process and thus, progressively resorbed.
Ankylosis may be transient or progressive.
In the transient type, <20% of the root surface becomes ankylosed. In such cases, reversal may occur, resulting in the re-establishment of a periodontal ligament connection between tooth and bone.


Etiopathogenesis
- Replacement resorption occurs after a severe dental injury like intrusive luxation or avulsion resulting in drying and death of periodontal ligament cells
- An inflammatory process removes the necrotic debris from the root surface which results in root surface being devoid of cementum
- To compensate for this, cells in the vicinity of the root surface try to repopulate it. Cells that form bone move across the socket wall and colonize the damaged root wall.
- By this, bone comes in direct contact with root without an intermediate attachment apparatus resulting in dentoalveolar ankylosis
Etiopathogenesis Histological Examination
Direct fusion between dentin and bone without separating cemental or periodontal ligament layer
Active resorption lacunae with osteoclasts are seen in conjunction with apposition of normal bone laid by osteoblasts
Etiopathogenesis Clinical Features
- Replacement resorption is usually asymptomatic
- Infraocclusion, incomplete alveolar process development (if the patient is young), and absence of normal mesial drift
- The pathognomonic feature is the immobility of the affected tooth and a distinctive metallic sound on percussion.
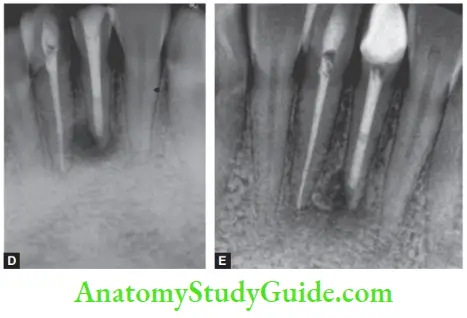
Etiopathogenesis Radiographic Features
Moth-eaten appearance with an irregular border, absence of periodontal ligament, and lamina dura are seen in radiographs of an ankylosed tooth.
Etiopathogenesis Diagnosis
- Lack of mobility and high-pitched metallic sound on percussion
- Radiographically, loss of periodontal ligament space with replacement by bone and uneven contour of root is indicative of ankylosis
Etiopathogenesis Treatment
Currently, there is no treatment for replacement resorption.
To slow down the resorptive process, root surface is treated with fluoride solution prior to replantation if the extraoral time for the tooth was >2 h and it was not kept moist to protect the periodontal ligament.
Etiopathogenesis Prevention
The following points should be considered in cases of avulsion:
- Immediate replantation without much of extraoral dry time
- Proper extraoral storage to prevent dehydration
- In case of an extended period of extraoral time, soak the tooth in a fluoride gel
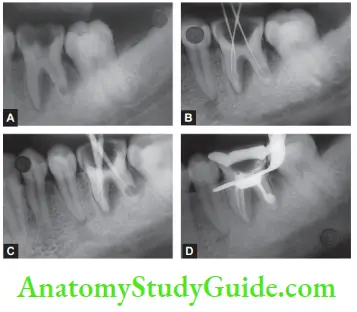
Cervical Root Resorption (Extracanal Invasive Resorption)
According to Cohen, it is the type of inflammatory root resorption occurring immediately below the epithelial attachment of tooth.
Epithelial attachment need not be always exactly at the cervical margin but can also be apical to the cervical margin. So the term “cervical” is a misnomer.
Extracanal Invasive Resorption Etiology
According to Heithersay, etiology can be
- Orthodontic treatment
- Trauma
- Bleaching of nonvital teeth
- Periodontal treatment
- Bruxism
- Idiopathic
Etiopathogenesis
Though it is a relatively common occurrence, it is not well recognized and often classified as idiopathic resorption because of difficulty in establishing a cause and effect relation.
It appears to originate in the cervical area of the tooth below the epithelial attachment and often proceeds from a small surface opening to involve a large part of dentin between the cementum and the pulp.
The resorption can proceed in several directions due to its invasive nature, hence the term invasive resorption.
It can extend coronally under the enamel, giving the tooth a pink spot appearance. Because cervical resorption is not always associated with infected or necrotic pulp, the treatment options vary accordingly.
Theories of Cervical Root Resorption
- Some procedures like bleaching, trauma, or orthodontic treatment cause alteration in the organic and inorganic cementum, finally making it more inorganic. Ths makes the cementum less resistant to resorption
- The immunological system senses the altered root surface, as a different tissue, attacks as a foreign body
Clinical Features
Initially, the cervical root resorption is asymptomatic in nature. Pulp is vital in most of the cases
It initially starts as a small lesion progresses, and reaches the present. Prevention is more resistant to spreads laterally in apical and coronal directions “enveloping” the root canal
In long-standing cases, extensive loss of tooth structure is replaced by granulation tissues which undermines the enamel in due course giving rise to a pink spot appearance.
It is misdiagnosed as internal resorption but confirmed with a radiograph. Rarely, it perforates into the tooth causing secondary involvement of pulp
Heithersay’s Classification
Class 1: A small invasive resorptive lesion near a cervical area with shallow penetration into dentin.
Class 2: Well-defied resorptive defect close to the coronal pulp chamber, but little or no involvement of radicular dentin.
Class 3: Deep resorptive lesion involving coronal pulp and also a coronal third of the root.
Class 4: Resorptive defective extending beyond the coronal third of root canal.

Frank’s Classification of Cervical Root Resorption
- Supraosseous: Coronal to the level of alveolar bone
- Intraosseous: Not accompanied by a periodontal breakdown
- Crestal: At the level of the alveolar bone
Frank’s Classification of Cervical Root Resorption Radiographic Features
Radiographically, one can see the moth-eaten appearance with the intact outline of the canal. Because bone is often involved, resorption may give the appearance of an infrabony pocket.
Frank’s Classification of Cervical Root Resorption Treatment
Main aim of the treatment is to restore the lost tooth structure and to disrupt the resorptive process.
Since pulp is most vital, repair of the resorbed area without removing the pulp is done.
Heithersay recommended topical application of a 90% solution of trichloroacetic acid (to cause coagulation and necrosis of necrotic tissue), curettage, and then restoration with glass ionomer cement.
If symptoms of pulpitis develop later, endodontic treatment is done.
Conclusion
Tooth resorption is a perplexing problem where the etiologic factors are vague and less clearly defied.
For the best treatment outcome, the clinician should have a very good knowledge of the etiopathology of resorptive lesions.
Early diagnosis and prompt treatment in such cases are the key factors that determine the success of the treatment.
More clinical studies and research with animal models are required to explain more about this phenomenon scientifically.
Leave a Reply