Pulp Introduction
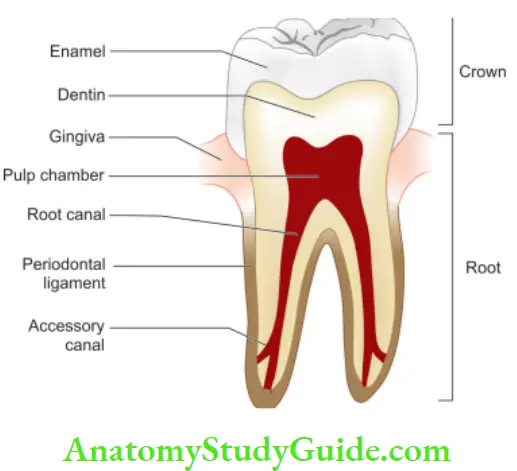
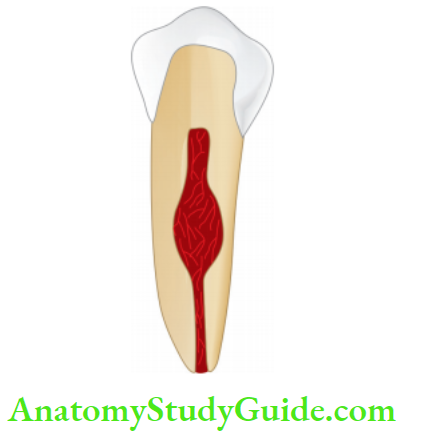
The dental pulp consists of vascular connective tissue contained within the rigid dentin walls. It is the principal source of pain in the oral cavity and also a major site of attention in endodontics and restorative procedures. This, knowledge of pulp is essential not only for providing dental treatment but also to know the rationale behind the treatment provided.
Table of Contents
Read And Learn More: Endodontics Notes
Important features of pulp:
- It is a coherent soft tissue, surrounded by dentin which limits the area for expansion and restricts its ability to tolerate
edema. - Odontoblasts present in the pulp have the ability to form dentin in response to caries and irritants.
- Pulp has an almost total lack of collateral circulation. This limits its ability to cope with bacteria, necrotic tissue, and inflammation.
- It gives a radiographic appearance as a radiolucent line.
Etiology Of Pulpal Diseases
Classification of etiology according to WEINE beginning with the most common irritant
1. Bacterial:
The most common cause of pulpal injury is bacteria or their by-products which may enter the pulp through a break in dentin from
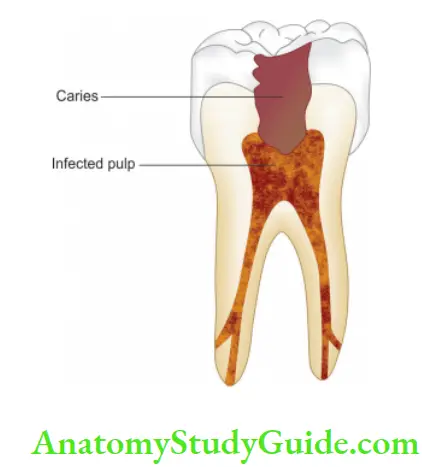
- Caries
- Accidental exposure
- Fracture
- Percolation around a restoration
- Extension of infection from gingival sulcus
- Periodontal pocket and abscess
- Anachoresis (a process by which microorganisms get carried by the bloodstream from another source and localize on inflamed tissue)
2. Traumatic:
- Acute trauma like fracture, luxation, or avulsion of tooth
- Chronic trauma including parafunctional habits like bruxism
3. Iatrogenic:
Pulp inflammation resulting from the clinician’s own procedures is referred to as entactogenic pulpitis. Iatrogenic causes of pulp pathologies can be
- Thermal changes are caused during tooth preparation, restoration, bleaching of enamel, electrosurgical procedures, etc.
- Orthodontic movement
- Periodontal curettage
- Periapical curettage
- Use of chemicals like temporary and permanent
- restorations, liners, bases, and use of cavity desiccants such as alcohol
4. Idiopathic:
- Aging
- Resorption; internal or external
Radiation injury to pulp:
- Pulp cells exposed to ionizing radiation may become necrotic, and show vascular damage and the interference in mitosis of cells.
- Irradiation affects salivary glands resulting in decreased salivary flow, thereby increasing predisposition to dental caries and pulpal involvement.
- Effects of radiation damage to teeth depend on the dose, source, type of radiation, exposure factor, and stage of tooth development at the time of irradiation.
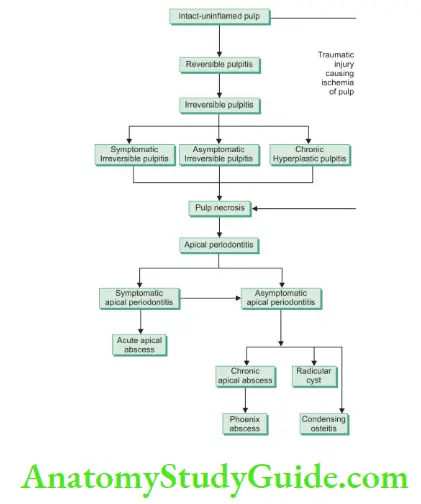
Progression Of Pulpal Pathologies
Pulp reacts to above mentioned irritants the same as other connective tissues. A normal pulp gives a mild-to-moderate response to pulp tests and this response subsides on the removal of stimulus. The degree of inflammation is proportional to the intensity and severity of the tissue damage.
For example, slight irritation like incipient caries or shallow tooth preparation causes little or no pulpal inflammation, whereas extensive operative procedures may lead to severe pulpal inflammation.
Depending on the condition of the pulp, severity, and duration of the irritant, and host response, the pulp may respond from mild inflammation to pulp necrosis. These changes may not be accompanied by pain and thus may proceed unnoticed.
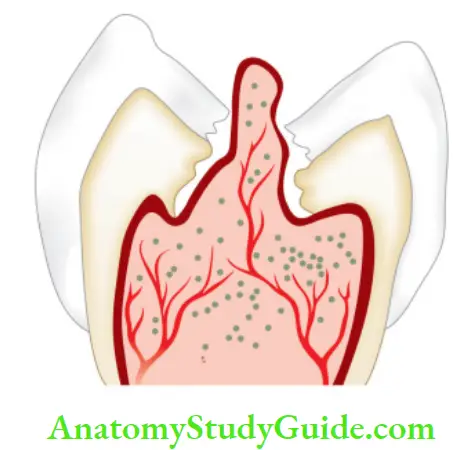
Pulpal reaction to microbial irritation
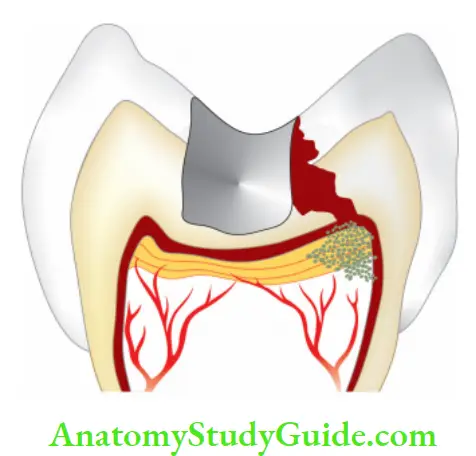
Microorganisms present in carious
enamel and dentin
↓
Penetration of microorganisms in deeper
layers of carious dentin
↓
Pulp is affected before the actual invasion of bacteria via their toxic by-products
↓
By-products cause local chronic cell infiltration
↓
When actual pulp exposure occurs, pulp tissue gets locally infiltrated by PMNs to form an area of liquefaction necrosis at the site of exposure
↓
Eventually, necrosis spreads all across the pulp and periapical tissue resulting in severe inflammatory lesions
Pulp Inflammation and Its Sequelae:
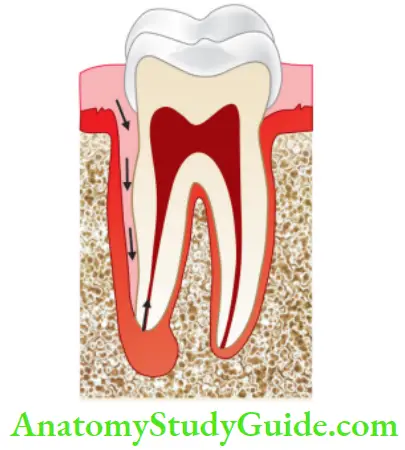
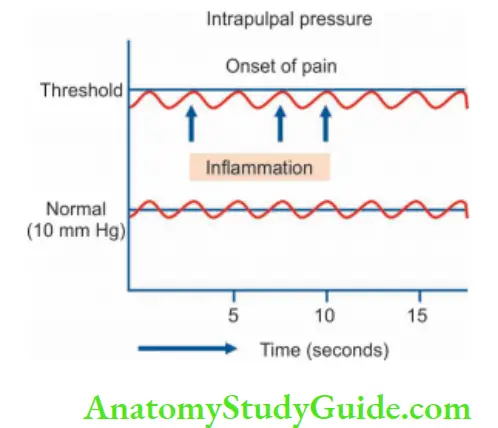
The traditional theory which explained pulpal inflammation and its sequelae was referred to as strangulation theory. Strangulation theory is no longer accepted and a current theory explains the sequelae of pulpal inflammation.
Strangulation Theory:
It says that on irritation, there is local inflammation in the pulp, which results in vasodilation, increased capillary pressure, and permeability. These results in increased filtration from capillaries into tissues, thus increasing tissue pressure. By this, thin vessel walls get compressed resulting in decreased blood flow and increased venous pressure.
This results in a vicious cycle, because the increase in venous pressure further increases capillary pressure. Consequently, choking/strangulation of pulpal blood vessels occur because of increased tissue pressure. This results in ischemia and further necrosis.
Current Theory:
Many studies have shown that an increase of pressure in one area does not affect the other areas of the pulp. Therefore local inflammation in pulp results in increased tissue pressure in inflamed area and not the entire pulp cavity.
It is seen that injury to coronal pulp results in local disturbance, but if the injury is severe, it results in complete stasis of blood vessels in and near the injured area. Net absorption of fluid into capillaries in adjacent uninflamed areas results in increased lymphatic drainage thus keeping the pulpal volume almost constant.
A limited increase in pressure within the affected pulpal area is explained by the following mechanism:
- Increased pressure in inflamed areas favors the net absorption of interstitial fluids from adjacent capillaries in uninflamed tissues.
- Increased interstitial tissue pressure lowers the transcapillary hydrostatic pressure difference, and thus opposes further filtration.
- Increased interstitial fluid pressure increases lymphatic drainage.
- Break in the endothelium of pulpal capillaries facilitate the exchange mechanism.
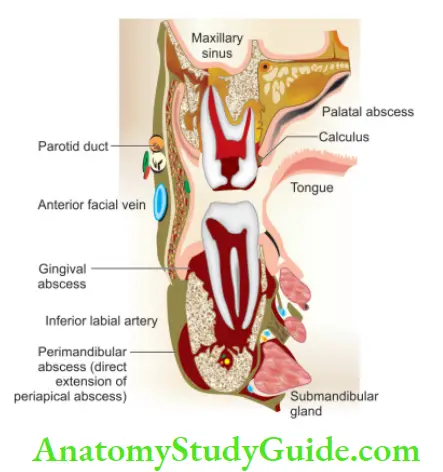
Infectious sequelae of pulpitis include apical periodontitis, periapical abscess/cellulitis, and osteomyelitis of the jaw. Spread from maxillary teeth may cause purulent sinusitis, meningitis, brain abscess, orbital cellulitis, and cavernous sinus thrombosis. Spread from mandibular teeth may cause Ludwig’s angina, parapharyngeal abscess, mediastinitis, pericarditis, and empyema
Diagnosis Of Pulpal Pathology
1. Subjective symptoms: Most common symptom is pain
2. Objective symptoms:
- Visual and tactile inspection—3Cs
- Color
- Contour
- Consistency
- Thermal tests:
- Heat tests: Use of
- Warm air
- Hot water
- Hot burnisher
- Hot gutta-percha stick
- Cold tests:
- Ethyl chloride spray
- Ice pencils
- CO 2 snow (temperature −78°C)
- Heat tests: Use of
- Electrical pulp testing
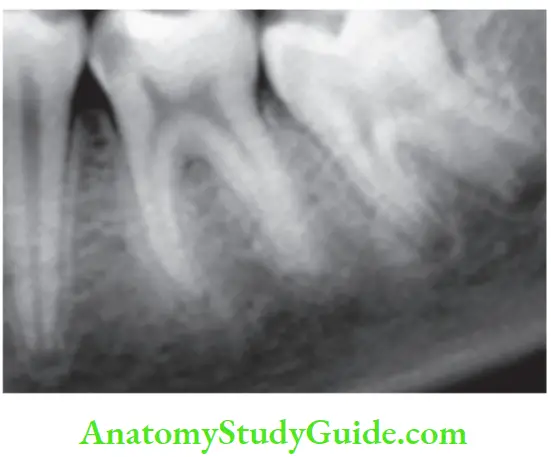
- Radiographs
- Anesthetic tests
- Test cavity
Recent advances in diagnostic aids for pulp pathologies include
3. Laser Doppler flowmetry
4. Liquid crystal testing
5. Hughes probe camera
6. Infrared thermography
7. Thermocouples
8. Pulse oximetry
9. Dual wavelength spectrophotometry
10. Plethysmography
11. Xenon-133 radioisotopes
Classifiation Of Pulpal Pathologies
Grossman’s Clinical Classification:
1. Pulpitis: Inflammatory disease of the dental pulp
- Reversible pulpitis
- Irreversible pulpitis
- Symptomatic irreversible(previously known as acute irreversible pulpitis)
- Asymptomatic irreversible(previously known as chronic irreversible pulpitis)
- Hyperplastic pulpitis
- Internal resorption
2. Pulp degeneration
- Calcifi (radiographic diagnosis)
- Atrophic (histopathological diagnosis)
- Fibrous
3. Necrosis
Baume’s Classifiation
Based on clinical symptoms:
- The asymptomatic, vital pulp which has been injured or involved by deep caries for which pulp capping may be done.
- Pulp with a history of pain which is amenable to pharmacotherapy.
- Pulp was indicated for extirpation and immediate root filling.
- Necrosed pulp involving infection of radicular dentin
accessible to antiseptic root canal therapy.
Seltzer and Bender’s Classification:
Based on clinical tests of pulp and histological diagnosis:
Treatable without Pulp Extirpation and Endodontic Treatment
- Intact uninflamed pulp
- Transition stage
- Atrophic pulp
- Acute pulpitis
- Chronic partial pulpitis without necrosis
Untreatable without Pulp Extirpation and Endodontic Treatment
- Chronic partial pulpitis with necrosis
- Chronic total pulpitis
- Total pulp necrosis
Ingle’s Classification:
1. Inflammatory Changes
- Hyper-reactive pulpalgia
- Hypersensitivity
- Hyperemia
- Acute pulpalgia
- Incipient (may be reversible)
- Moderate (may be referred)
- Advanced (relieved by cold)
- Chronic pulpalgia
- Hyperplastic pulpitis
- Pulp necrosis
2. Retrogressive Changes
- Atrophic purposes
- Calcifi purposes
Barodontalgia Or Aerodontalgia
It is pain experienced in a recently restored tooth during low atmospheric pressure. Pain is experienced either during ascent or descent. Chronic pulpitis which appears asymptomatic in normal conditions may manifest as pain at high altitudes because of low pressure. It is generally seen in altitudes over 5,000 ft but is more likely to be observed in 10,000 ft and above.
Rauch classified bar odontalgia according to the chief complaint:
- Class I: In acute pulpitis, sharp pain occurs for a moment on the ascent.
- Class II: In chronic pulpitis, dull throbbing pain occurs on an ascent.
- Class III: In necrotic pulp, dull throbbing pain occurs on descent but it is asymptomatic on ascent.
- Class IV: In periapical cyst or abscess, severe and persistent pain occurs with both ascent and descent
Possible mechanism of bar odontalgia:
- Direct ischemia results from inflammation itself.
- Indirect ischemia results from increased intrapulpal pressure due to vasodilatation and fluid diffusion to the tissue.
- Due to the expansion of intrapulpal gas which is a by-product of acids, bases, and enzymes of inflamed tissues.
- Due to leakage of gas through vessels because of decreased gas solubility.
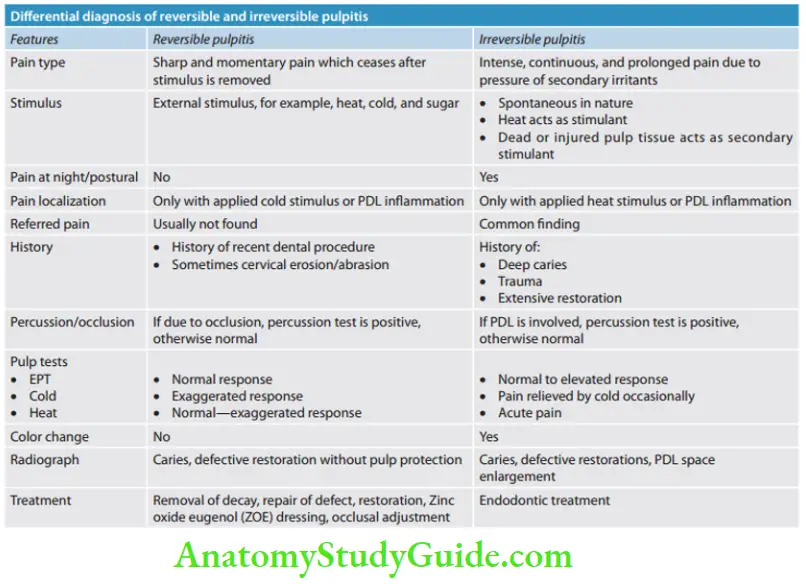
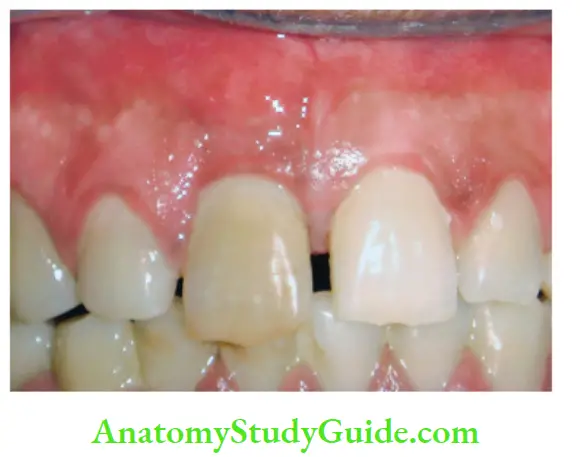
Reversible Pulpitis Or Hyperemia Or Hyperactive Pulpalgia
This is the first stage of pulpitis giving a sharp hypersensitive response to cold, but the pain subsides on the removal of the stimulus. The patient may describe symptoms of momentary pain and is unable to locate the source of pain. This stage can last for months or years.
Reversible Pulpitis Definition:
Reversible pulpitis is a mild-to-moderate inflammatory condition of pulp caused by noxious stimuli in which the pulp is capable of returning to a normal state following the removal of stimuli.
It is an indication of peripheral Aδ-fier stimulation. Determination of reversibility is the clinical judgment which is influenced by a history of the patient and clinical evaluation.
Etiology:
In normal circumstances, enamel and cementum act as an impermeable barriers to block the patency of dentinal tubules. When a stimulus interrupts this natural barrier, dentinal tubules become permeable, causing inflammation of the pulp. Etiological factors can be
- Dental caries
- Trauma: Acute or chronic occlusal trauma
- Thermal injury:
- Tooth preparation with dull bur without coolant
- Overheating during the polishing of a restoration
- Keeping bur in contact with teeth too long
- Chemical stimulus—like sweet or sour foodstuff
Reversible Pulpitis Symptoms:
- Characterized by sharp momentary pain, commonly caused by cold stimuli.
- Pain does not occur spontaneously and does not continue after the removal of the irritant.
- Following the insertion of deep restoration, the patient may complain of mild sensitivity to temperature changes, especially cold. Such sensitivity may last for a week or longer but gradually, it subsides. This sensitivity is a symptom of reversible pulpitis.
Reversible Pulpitis Histopathology:
- It shows hyperemia to mild-to-moderate inflammatory changes
- Evidence of disruption of the odontoblastic layer
- Formation of reparative dentin
- Dilated blood vessels
- Extravasation of edema flid
- Presence of immunologically competent chronic inflammatory and occasionally acute cells.
Reversible Pulpitis Diagnosis:
1. Pain:
It is sharp but of short duration, usually caused by cold, sweet, and sour stimuli. Pain ceases after removal of the stimulus.
2. Visual examination and history:
It may reveal caries, recent restoration, traumatic occlusion, and undetected fractures.
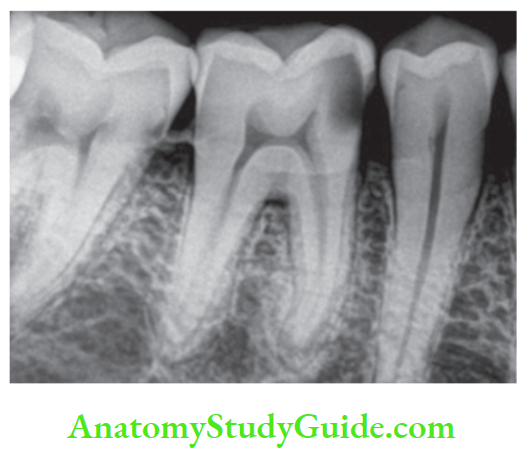
3. Reversible Pulpitis Radiographic examination:
- Shows normal PDL and lamina dura, i.e., normal periapical tissue.
- Presence of deep dental caries or restoration.
4. Reversible Pulpitis Percussion test:
The tooth is normal to percussion and palpation without any mobility
5. Reversible Pulpitis Vitality test:
Pulp responds readily to cold stimuli.
Diffrential Diagnosis:
- In reversible pulpitis, the pain disappears on the removal of stimuli, whereas in irreversible pulpitis, the pain stays longer even after the removal of stimulus.
- The patient’s description of pain, character, and duration leads to the diagnosis.
Treatment:
- The best treatment of reversible pulpitis is prevention.
- Usually, a sedative dressing is placed, followed by permanent restoration when symptoms completely subside.
- Periodic care to prevent caries, desensitization of hypersensitive teeth, and proper pulp protection by using cavity varnish or base before placement of restoration is recommended.
- If pain persists despite of proper treatment, pulpal inflammation should be considered as irreversible and it should be treated by pulp extirpation.
Irreversible Pulpitis
Irreversible Pulpitis Definition:
“It is a persistent inflammatory condition of the pulp, symptomatic or asymptomatic, caused by a noxious stimulus.” It has both symptomatic and asymptomatic stages in pulp.
Etiology:
Irreversible pulpal inflammation can result from
- Dental caries (most common cause)
- Chemical, thermal, and mechanical injuries of pulp
- Untreated reversible pulpitis
Irreversible Pulpitis Symptoms
- Rapid onset of pain, caused by sudden temperature change, sweet, or acidic food. Pain remains even after the removal of the stimulus.
- Pain can be spontaneous in nature which is sharp, piercing, intermittent, or continuous in nature.
- Pain exacerbated on bending down or lying down due to a change in intrapulpal pressure from standard to supine.
- Pain is so severe that it keeps the patient awake in night.
- Presence of referred pain.
- In later stages, pain is severe, boring, and throbbing in nature which increases with hot stimulus. Pain is relieved by using cold water. Sometimes the pain is so severe that the patient may report dental clinic with jar of ice-cold water.
- Apical periodontitis develops in later stages when inflammation extends to the periodontal ligament.
Irreversible Pulpitis Histopathology:
Pulp shows acute and chronic inflammatory changes such as
- Vascular dilatation and edema
- Granular cell infiltration
- Odontoblasts are destroyed
- Formation of minute abscess formation
- In later stages, pulp undergoes liquefaction and necrosis
Irreversible Pulpitis Diagnosis:
1. Visual examination and history:
One may find deep cavities involving pulp or secondary caries under restorations.
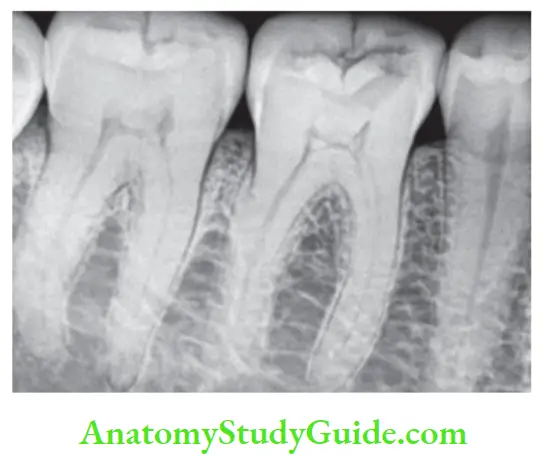
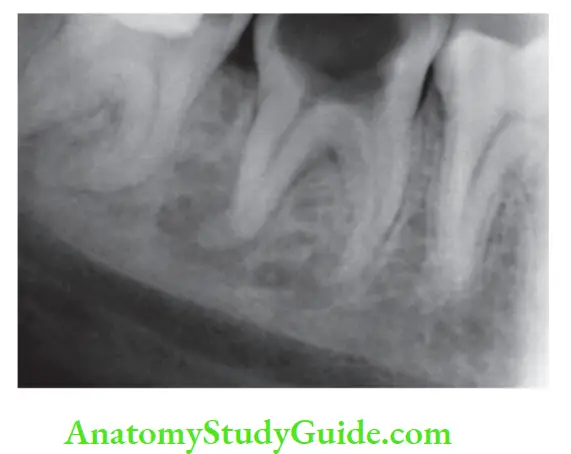
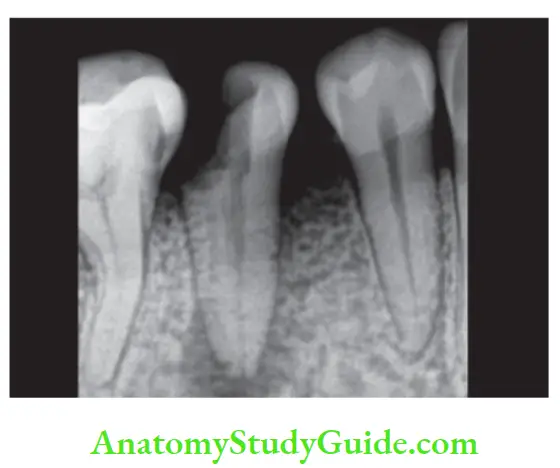
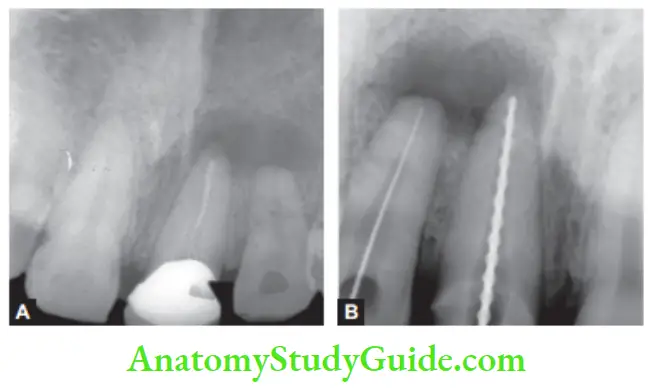
2. Irreversible Pulpitis Radiographic findings:
- Shows depth and extent of caries
- The periapical area shows normal appearance but a slight widening may be evident in advanced stages of pulpitis.
3. Irreversible Pulpitis Percussion:
Sometimes a tooth is tender on percussion because of increased intrapulpal pressure due to exudative inflammatory tissue.
4. Irreversible Pulpitis Vitality tests:
- Thermal test:
Hyperalgesic pulp responds more readily to cold stimulation than for normal teeth, pain may persist even after the removal of the irritant. As pulpal inflammation progresses, heat intensifies the response because of its expansible effect on blood vessels. Cold tends to relieve pain because of its contractile effect on vessels, thereby reducing the intrapulpal pressure.
- Electric test:
Less current is required in the initial stages. As the tissue becomes more necrotic, more current is required to generate the response.
Irreversible Pulpitis Treatment:
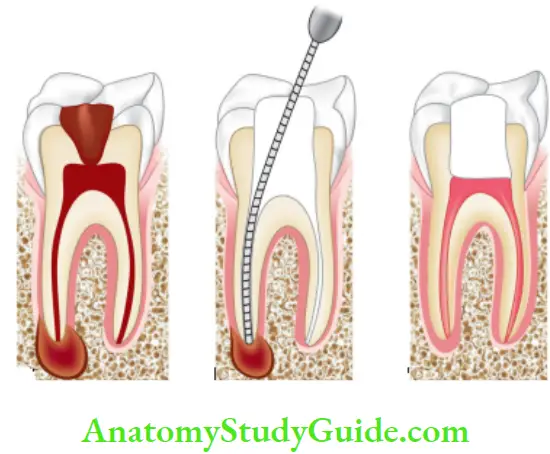
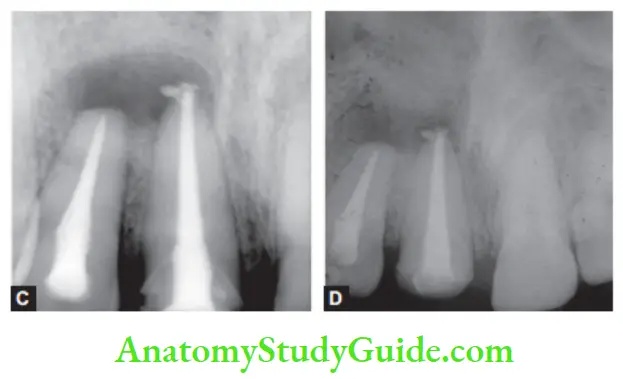
A pulpectomy, i.e., root canal treatment.
Irreversible Pulpitis Signs and Symptoms:
- It is usually asymptomatic.
- Fleshy pulpal tissue fills the pulp chamber. It is less sensitive than normal pulp but bleeds easily due to a rich network of blood vessels.
- Sometimes this pulpal growth interferes with chewing
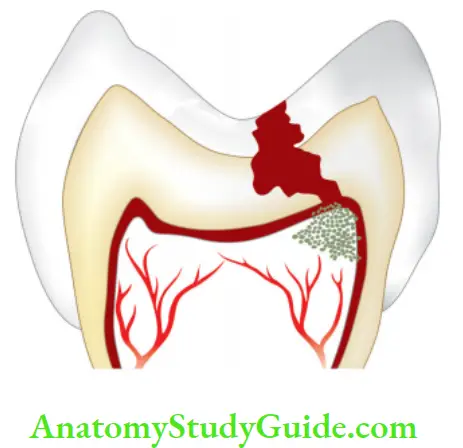
Chronic Hyperplastic Pulpitis
It is an inflammatory response of pulpal connective tissue due to extensive carious exposure of a young pulp. It shows the overgrowth of granulomatous tissue into carious cavity.
Etiology:
The hyperplastic form of chronic pulpitis is commonly seen in the teeth of children and adolescents because in these pulp tissue has high resistance and large carious lesion permits free proliferation of hyperplastic tissue.
Chronic Hyperplastic Pulpitis Histopathology:
- The tissue of pulp chamber is transferred into granulation tissue which projects out from pulp chamber.
- Granulation tissue contains PMNs, lymphocytes, and plasma cells.
- The surface of pulp polyp is usually covered by stratified squamous epithelium which may be derived from gingiva, desquamated epithelial cells of mucosa and tongue.
- Nerve fiers may be present in the epithelial layer.
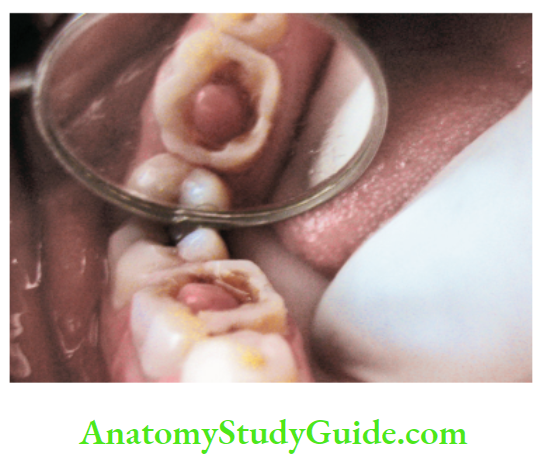
Chronic Hyperplastic Pulpitis Diagnosis:
- Pain: It is usually absent
- The hyperplastic form shows a fleshy, reddish pulpal mass which fills most of the pulp chamber or cavity. It is less sensitive than normal pulp but bleeds easily when probed. When it is cut, it does not produce pain but pain can result due to pressure transmission to the apical part
- Vitality tests
- The tooth may respond feebly or not at all to thermal tests unless one uses extreme cold.
- More than normal current is required to elicit the response by the electric pulp tester.
- Diffrential diagnosis:
Hyperplastic pulpitis should be diffrentiated from proliferating gingival tissue. It is done by raising and tracing the stalk of tissue back to its origin, that is, pulp chamber.
Chronic Hyperplastic Pulpitis Treatment:
- In case of hyperplastic pulpitis, removal of polypoid tissue using a periodontal curette or spoon excavator followed by root canal treatment.
- If a tooth is at the nonrestorable stage, it should be extracted.
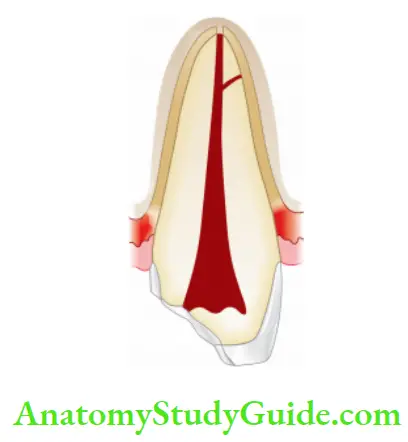
Internal Resorption Or Pink Tooth of Mummery
Internal resorption was first reported by Bell in 1830. It is known as the Pink Tooth of Mummery because of the pink discoloration of the crown and is named after the anatomist Mummery.
Internal resorption is an idiopathic slow or fast progressive resorption occurring in the dentin of the pulp chamber or
root canals of the teeth.
Etiology:
The exact etiology is unknown. A patient may present a history of trauma or persistent chronic pulpitis, or a history of pulpotomy.
Mechanism of resorption Pulp inflammation due to infection
↓
Alteration or loss of predentin and odontoblastic layer
↓
Undifferentiated mesenchymal cells come in contact with mineralized dentin
↓
Diffrentiate into dentinoclasts
↓
Resorption results
Internal Resorption Symptoms:
- Usually asymptomatic, recognized clinically through routine radiograph.
- Pain occurs if resorption perforates the root.
- “Pink tooth” is the pathognomonic feature of internal root resorption.
- Pulp shows either partial or complete necrosis. In actively progressive lesions, pulp is partially vital and may show symptoms of pulpitis.
- In anterior teeth, it is typically seen in the middle of the tooth in the mesiodistal direction but in multirooted teeth, it can be present mesial, distal, or center.
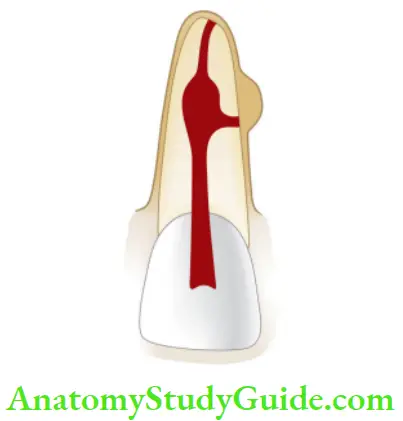
Internal Resorption Diagnosis:
1. Clinically: “Pink tooth” appearance
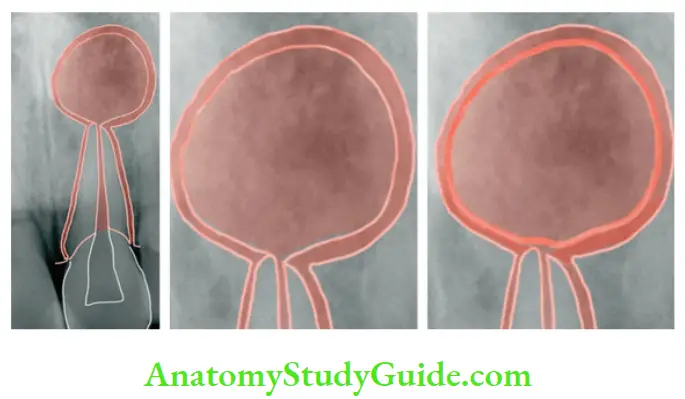
2. Radiographic changes:
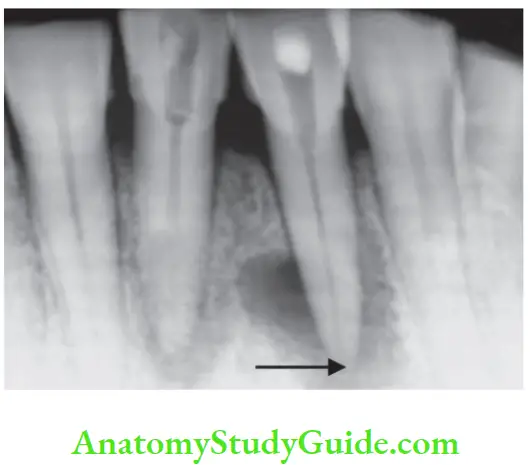
- The classical description of internal resorption, that is, clearly well-defied radiolucency of uniform density which balloons out of root canal was given by Gartner el al.
- The original root canal outline distorted
Bone changes are seen only when root perforation into the periodontal ligament takes place.
3. Pulp tests:
Positive, though a coronal portion of the pulp is necrotic, the apical pulp could be vital.

Internal Resorption Diffrential Diagnosis:
It is difficult to differentiate internal resorption from external resorption when it progresses to periodontal space causing root perforation.
It can be diffrentiated by
- History: Giving the history of trauma, pulpotomy, etc.
- Pink tooth appearance
- Taking radiographs at different angles; radiolucency does not move when a radiograph is taken at different angles, whereas in external resorption, radiolucent lesion changes position on changing angle.
- Uniform ballooning of the root canal is seen in internal resorption, whereas an irregular border with alteration of adjacent bone is seen in external resorption.
Internal Resorption Treatment:
- Pulp extirpation stops internal root resorption.
- Surgical treatment is indicated if conventional treatment fails.
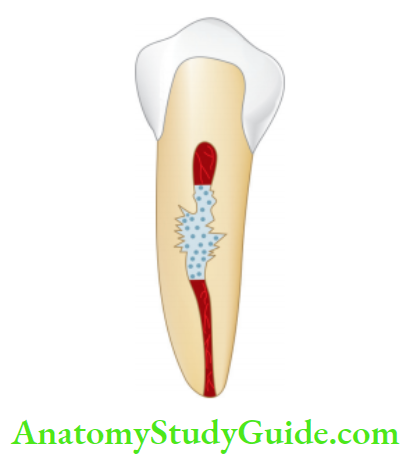
Pulp Degeneration
Pulp degeneration is generally present in old age. In young age, it may result from persistent mild irritation. Common causes of pulp degeneration are attrition, abrasion, erosion, operative procedures, caries, pulp capping, and reversible
pulpitis. Forms of pulp degeneration:
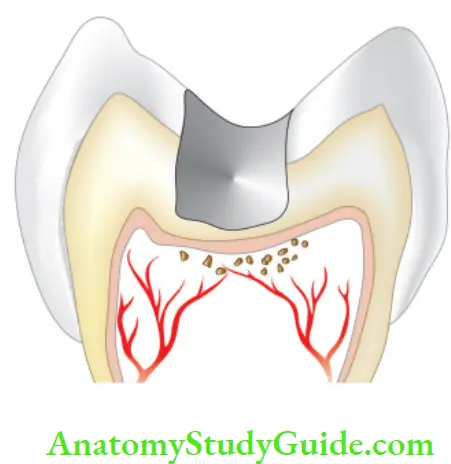
Pulp Degeneration Calcifi Degeneration:
In calcific degeneration, part of pulp tissue is replaced by calcified material. Mainly three types of calcifications are seen in pulp:
- Dystrophic calcifications
- Diffuse calcifications
- Denticles/pulp stones
Pulp Degeneration Dystrophic Calcification :
- They occur by the deposition of calcium salts in dead or degenerated tissue. The local alkalinity of destroyed tissues attracts the salts.
- They occur in minute areas of young pulp affected by minor circulatory disturbances, in blood clots, or around a single degenerated cell.
- They can also begin in the connective tissue walls of blood vessels and nerves and follow their course.

Pulp Degeneration Diffuse Calcifiations:
- They are generally observed in root canals.
- The deposits become long, thin, and fibrillar on fusing
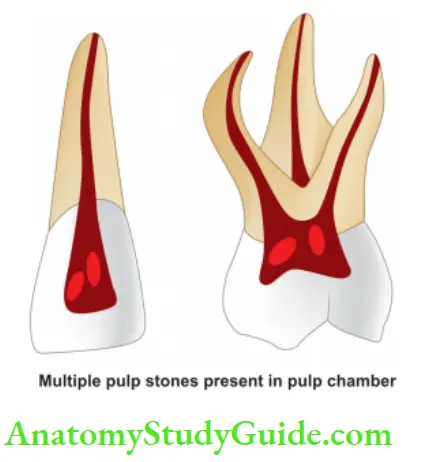
Pulp Degeneration Denticles/Pulp Stones:
These are usually seen in pulp chambers.
Classification of pulp stones:
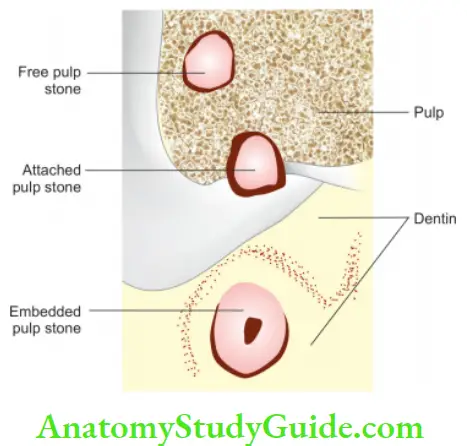
- According to Location:
- Free
- Embedded
- Attached
According to Structure:
-
- True
- False
True denticle:
It is composed of dentin formed from detached odontoblasts or fragments of Hertwig’s enamel root sheath which stimulates the undifferentiated cells to assume dentinoblastic activity.
False denticle:
Here degenerated tissue structures act as a nidus for the deposition of concentric layers of calcified tissues.
Atrophic Degeneration:
- It is wasting away or decreasing in size which occurs slowly as the tooth grows old.
- Here fewer stellate cells are found and pulp is less sensitive than normal.

Fibrosis Degeneration:
- There is a gradual shift in the ratio and quality of tissue elements. Here, the number of collagen fiers/unit area increases leading to fibrosis. Pulp has a characteristic leathery appearance.
- The number and size of cells decrease so cells appear as “shrunken solid particles in a sea of dense fiers”.
- Fibroblastic processes are lost, and cells have round and pyknotic nuclei.
- Dentinoblasts decrease in length and appear cuboidal or flattened.
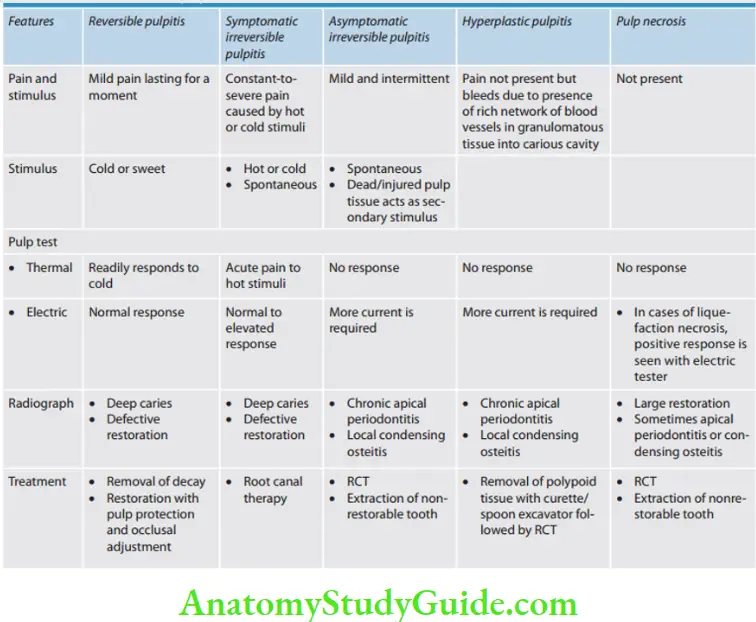
Pulp Necrosis
Pulp necrosis or death is a condition following untreated pulpitis. Pulpal tissue becomes nonvital and if the condition is not treated, noxious materials will leak from pulp space forming the lesion of endodontic origin. Necrosis may be partial or total, depending on the extent of pulp tissue involvement.

Types of pulp necrosis:
1. Coagulation necrosis:
In coagulation necrosis, the protoplasm of all cells becomes fied and opaque. Cell mass is recognizable histologically, and intracellular details are lost.
2. Liquefaction necrosis:
In liquefaction necrosis, the entire cell outline is lost. The liquefied area is surrounded by a dense zone of PMNL (polymorphonuclear leukocytes) and chronic inflammatory cells.
Etiology:
Necrosis is caused by noxious insult and injuries to the pulp by bacteria, trauma, and chemical irritation.
Pulp Necrosis Symptoms:
- Discoloration of a tooth due to extravasation of pulpal blood into dentin as a result of trauma.
- Lack of translucency/dull or opaque appearance
- History from patient
- A tooth might be asymptomatic

Pulp Necrosisv Diagnosis:
1. Pain:
It is absent in complete necrosis
2. Pulp Necrosis History of the patient:
History reveals past trauma or past history of severe pain which may have lasted for some time followed by complete and sudden cessation of pain.
3. Pulp Necrosis Radiographic changes:
The radiograph shows a large cavity or restoration or normal appearance unless there is concomitant apical periodontitis or condensing osteitis.

4. Pulp Necrosis Vitality test:
Usually, vitality tests show a negative response. But multirooted teeth may show mixed responses because only one canal may have necrotic tissue. Sometimes teeth with liquefaction necrosis may show a positive response to an electric test when an electric current is conducted through moisture present in a root canal.
5. Pulp Necrosis Visual examination:
The tooth shows color changes like dull or opaque appearance due to a lack of normal translucency.
6. Pulp Necrosis Histopathology:
Necrotic pulp tissue, cellular debris, and microorganisms are seen in the pulp cavity. If there is concomitant periodontal involvement, there may be presence of slight evidence of inflmmation.
Pulp Necrosis Treatment:
Complete removal of pulp followed by restoration or extraction of the nonrestorable tooth.
Pathologies Of Periradicular Tissues
Periradicular tissue contains apical root cementum, periodontal ligament, and alveolar bone.
Etiology:
- Bacterial
- A root canal is a unique, stringent ecological niche for bacterial growth because of a lack of oxygen. The primary nutrient source for root canal biotics is host tissues and tissue fluids.
- Microorganisms in chronically infected root canals are mainly anaerobic and Gram-negative type.
The most common microorganisms seen in periradicular diseases are
- Streptococcus
- Peptostreptococcus
- Prevotella
Black-pigmented microorganisms
- Porphyromonas
- Enterococcus
- Campylobacter
- Fusobacterium
- Eubacterium
Pathologies Of Periradicular Tissues Routes:
- The untreated pulpal infection leads to total pulp necrosis and further periapical infection.
- Anachoresis
- Invasion of microorganisms into pulp from the periodontal pocket and accessory canals resulting in the formation of lesions of endodontic origin
Pathologies Of Periradicular Tissues Trauma:
- Physical trauma to a tooth or operative procedures result in dental follicle desiccation or heat transfer causing sufficient damage to pulp and its blood supply.
- Severe trauma to the tooth and heat production during tooth preparation causes immediate interruption of blood supply resulting in pulp necrosis even though it is not infected.
- Persistent periapical tissue compression from traumatic occlusion may lead to the apical inflammatory response.
Factors Related to Root Canal Procedures:
- It is impossible to extirpate pulp without initiating an inflammatory response.
- Using strong or excessive amounts of intracanal medicaments between appointments may induce periapical inflammation.
- Improper manipulation of instruments within the root canal or over instrumentation can force dentinal debris, irrigating solution, and toxic components of necrotic tissue in the periapex.
- Overextended endodontic filling material may induce periapical inflammation by directly inducing foreign body reaction which is characterized by the presence of leukocyte infiltration, macrophages, and other chronic inflammatory cells.

Pathologies Of Periradicular Tissues Diagnosis:
- Chief Complaint:
The patient usually complains of pain on biting, pain with swelling, pus discharge, etc.
- Dental History:
The patient gives a history of recurring episodes of pain and sometimes swelling with discharge.
- Objective Examinations:
1. Extraoral examination:
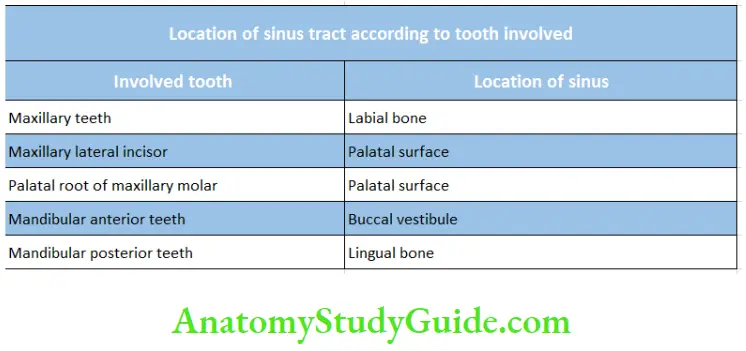
General appearance, skin tone, facial asymmetry, swelling, extraoral sinus, sinus tract, tender or enlarged cervical lymph nodes.
2. Intraoral examination:
It includes an examination of soft tissues and teeth to look for
discoloration, abrasion, caries, restoration, etc.
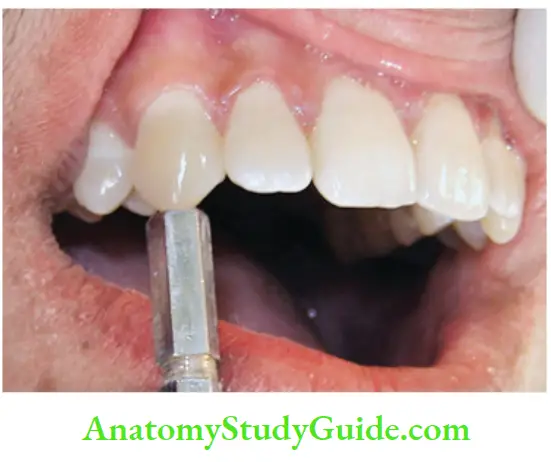
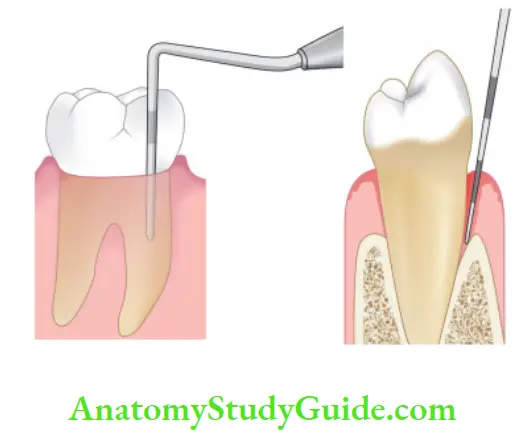
- Clinical Periapical Tests:
1. Percussion:
Indicates inflammation of the periodontium.
2. Palpation:
Determines how far the inflammatory process has extended periodically.
3. Pulp vitality:
- Thermal tests which can be heat or cold
- Electrical pulp testing
4. Periodontal examination
It is important because the periapical and periodontal lesions may mimic each other and require differentiation.
1. Probing:
Determines the level of connective tissue attachment. The probe can penetrate into an inflammatory periapical lesion that extends cervically.
2. Mobility:
Determines the status of periodontal ligament
Radiographic examination:
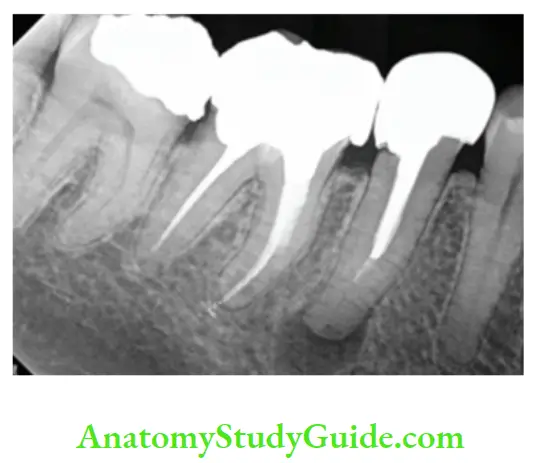
Periradicular lesions of pulpal origin have four characteristics :
- Loss of lamina dura apically
- Radiolucency at apex regardless of cone angle
- Radiolucency resembling a hanging drop
- Cause of pulp necrosis is usually evident
Recent advances in radiography:
- Digital subtraction radiography
- Xeroradiography
- Digital radiometric analysis
- Computed tomography
- Radiovisiography
- Magnetic resonance imaging
Classifiation Of Periradicular Pathologies
Grossman’s Classification:
1. Symptomatic periradicular diseases:
- Symptomatic apical periodontitis previously known as acute apical periodontitis (AAP):
- Vital
- Nonvital
- Acute alveolar abscess
- Phoenix abscess
2. Asymptomatic periradicular diseases:
Asymptomatic apical periodontitis (chronic apical periodontitis)
- Chronic alveolar abscess
- Radicular cyst
- Condensing osteitis
3. External root resorption
4. Persistent Apical periodontitis
5. Disease of the periradicular tissues of nonendodontic origin.
WHO Classification:
- K 04.4 — Acute apical periodontitis
- K 04.5 — Chronic apical periodontitis (apical granuloma)
- K 04.6 — Periapical abscess with sinus
- K 04.60 — Periapical abscess with sinus to the maxillary antrum
- K 04.61 — Periapical abscess with sinus to the nasal cavity
- K 04.62 — Periapical abscess with sinus to the oral cavity
- K 04.63 — Periapical abscess with sinus to skin
- K 04.7 — Periapical abscess without sinus
- K 04.8 — Radicular cyst (periapical cyst)
- K 04.80 — Apical and lateral cyst
- K 04.81 — Residual cyst
- K04.82 — Inflammatory paradental cyst
Ingle’s Classification of Pulpoperiapical Pathosis:
1. Painful pulpoperiapical pathosis:
- Symptomatic Acute apical periodontitis
- Advanced apical periodontitis:
- Acute apical abscess
- Phoenix abscess
- Suppurative apical periodontitis (chronic apical abscess)
2. Nonpainful pulpoperiapical pathosis:
- Condensing osteitis
- Chronic apical periodontitis both incipient and advanced stages
- Chronic apical periodontitis:
- Periapical granuloma
- Apical cyst
- Suppurative apical periodontitis
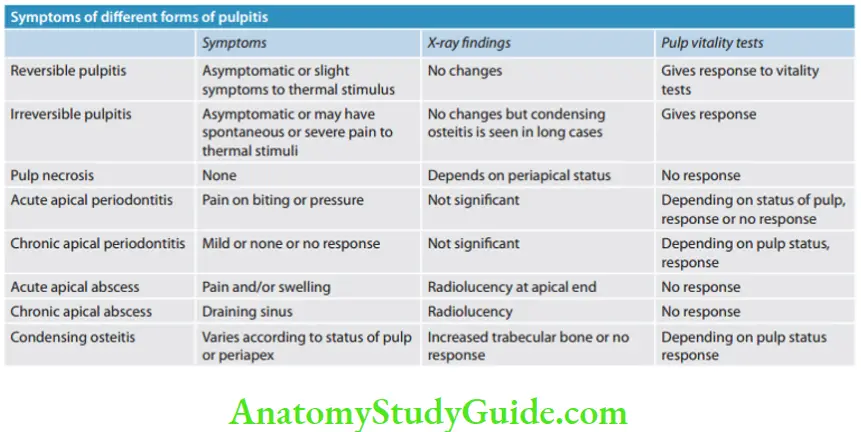
Symptomatic Apical Periodontitis Acute Apical Periodontitis
Symptomatic apical periodontitis is defined as painful inflammation of the periodontium as a result of trauma, irritation, or infection through the root canal, regardless of whether the pulp is vital or nonvital. It is an inflammation around the apex of a tooth.
Etiology:
- In vital tooth, it is associated with occlusal trauma, high points in restoration, wedging or forcing objects between teeth.
- In nonvital tooth, it is associated with sequelae to pulpal diseases.
- Iatrogenic causes can be over instrumentation of a root canal, pushing debris and microorganisms beyond the apex, overextended obturation, and root perforations.
Apical periodontitis Signs and Symptoms:
Apical periodontitis serves as a protective function, confining the microorganisms extruded from root canal space and preventing them from spreading in adjacent bone marrow areas. But it can’t eradicate the source of infection because the defense mechanism of pulp can’t come into play due to lack of vascular supply, once the pulp is nonvital.
This mechanism occurs at the apical area but can’t penetrate in fully matured tooth, so lack of proper treatment can result in chronic lesions.
- The tooth is tender on percussion
- The tooth may present mild-to-severe soreness
- Dull, throbbing, and constant pain
- Pain occurs over a short period of time
- Pain on mastication
Apical periodontitis Histopathology:
Pulp and periradicular tissue may be sterile if periodontitis is due to occlusal trauma or chemical or mechanical irritation during root canal treatment. In some cases, bacteria or their toxic products extrude through the periapex and irritate periradicular area.
Inflammatory reactions occur in the apical periodontal ligament
↓
Dilatation of blood vessels
↓
Initiation of inflammatory response due to the presence of polymorphonuclear leukocytes and round cells
↓
Accumulation of serous exudate
↓
Distention of periodontal ligament and extrusion of tooth, slight tenderness
↓
If irritation continues
↓
Loss of alveolar bone (unavoidable side effect of the defensive process by host to provide a necessary effective immune response
to root canal infection)
Apical periodontitis Diagnosis:
- The tooth is tender on percussion
- A radiographic picture of the vital tooth may show no change, whereas in the case of the nonvital tooth, it may show a widening of apical periodontal ligament space and loss of lamina dura.
Apical periodontitis Diffrential Diagnosis:
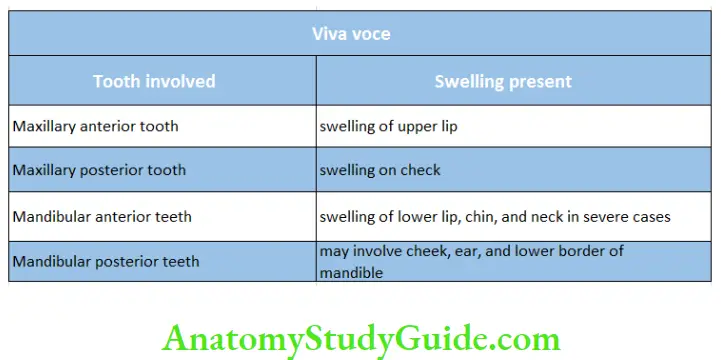
It should be diffrentiated from an acute apical abscess on the basis of history, symptoms, and clinical tests.
Apical periodontitis Treatment:
- If the cause is irreversible pulpitis or necrotic pulp, initiate endodontic treatment.
- If the cause is hyper occlusion, adjust the occlusion for immediate relief.
- To control postoperative pain following initial endodontic therapy, analgesics are prescribed.
- The use of antibiotics, either alone or in conjunction with root canal therapy is not recommended.
- For nonrestorable teeth, extraction is indicated
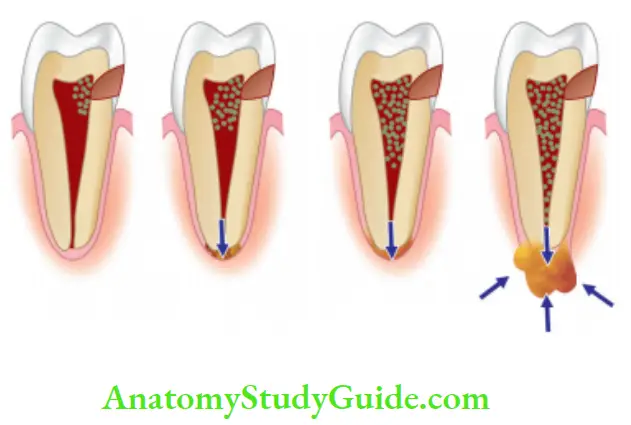
Acute Apical Abscess
Acute Apical Abscess Synonyms:
Acute Abscess, Acute Dentoalveolar, Abscess, Acute Periapical Abscess, and Acute Radicular Abscess. It is an inflammatory reaction to pulp infection and necrosis characterized by rapid onset, pus formation, spontaneous pain, tenderness on percussion, and eventual swelling of associated tissues.
Etiology:
- The most common cause is an invasion of bacteria from necrotic pulp tissue.
- Trauma, chemical, or any mechanical injury resulting in pulp necrosis.
- Irritation of periapical tissue by chemical or mechanical treatment during root canal treatment.
Tissue at surface of swelling appears taut and inflmed and pus starts to form underneath it. Surface tissue may become inflamed from the pressure of underlying pus and finally rupture from this pressure.
Initially, the pus comes out in the form of a small opening but later it may increase in size or number depending upon the amount of pressure of pus and the softness of the tissue overlying it. This process is the beginning of chronic abscess.
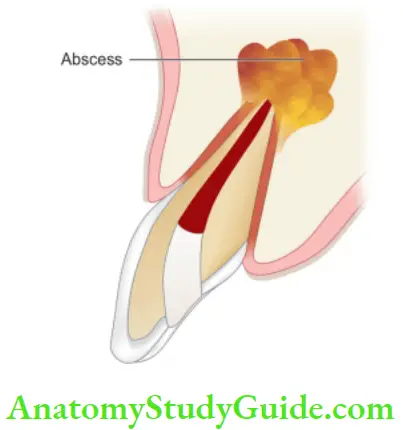
Pathophysiology of Apical Abscess Formation
Increase in pulpal pressure
↓
The collapse of venous circulation
↓
Hypoxia and anoxia of local tissue
↓
Localized destruction of pulp tissue
↓
Formation of pulpal abscess because of the breakdown of PMNs,
bacteria, and lysis of pulp remnants
Acute Apical Abscess Symptoms:
- In the early stage, there is the tenderness of the tooth which is relieved by continued slight pressure on the extruded tooth to push it back into the alveolus.
- Later on, throbbing pain develops with diffuse swelling
of overlying tissue. - Tooth becomes more painful, elongated, and mobile as infection increases in later stages.
- The patient may have systemic symptoms like fever and increased WBC count.
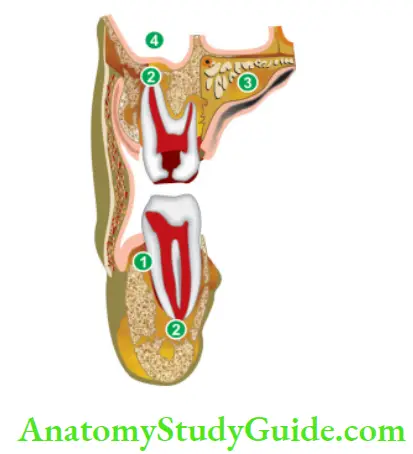
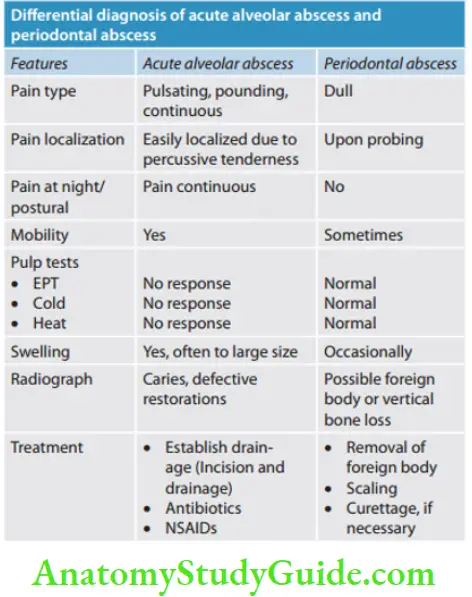
Spread of lesion toward a surface may take place causing erosion of cortical bone or it may diffuse and spread widely leading to the formation of cellulitis. The location of swelling is determined by the relation of the apex of the involved tooth to the adjacent muscle attachment.
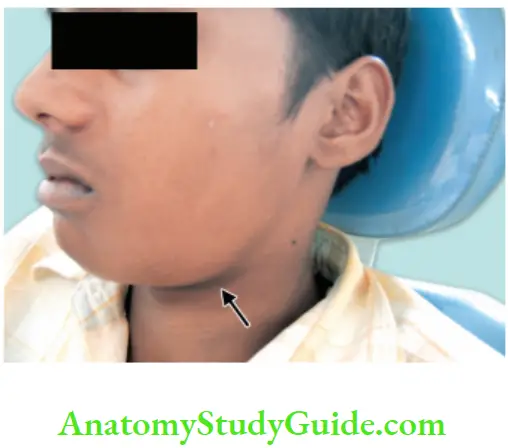
Spread of apical abscess to surrounding tissues, if it isnot treated:
- Vestibular abscess,
- Periapical abscess,
- Palatal abscess, and
- Maxillary sinus.
Acute Apical Abscess Histopathology:
Polymorphonuclear leukocytes infiltrate and initiate inflammatory response
↓
Accumulation of inflammatory exudates in response to active infection
↓
Distention of periodontal ligament
↓
Extrusion of the tooth
↓
If the process continues, the separation of periodontal ligament
↓
Tooth becomes mobile
↓
Bone resorption at the apex
↓
Localized lesion of liquefaction necrosis containing polymorphonuclear leukocytes, debris, cell remnants, and purulent
exudates
Acute Apical Abscess Diagnosis:
- Clinical examination
- In the initial stages, locating a tooth is difficult due to diffuse pain. The location of the offending tooth becomes easier when a tooth gets slightly extruded from the socket.
- A negative response to pulp vitality tests
- Tenderness on percussion and palpation
- The tooth may be slightly mobile and extruded from its socket
- Radiography was helpful in determining the affected tooth as it may show caries or evidence of bone destruction at the root apex.
Acute Apical Abscess vManagement:
- Drainage of the abscess should be initiated as early as possible. This may include
- Nonsurgical endodontic treatment
- Incision and drainage
- Extraction
Considerations regarding the treatment of a tooth with periapical abscess depend on the following factors:
-
- Prognosis of the tooth
- Patient preference
- The strategic value of the tooth
- The economic status of the patient
- In the case of localized infections, systemic antibiotics provide no additional benefit over drainage of abscesses.
- n the case of systemic complications such as fever, lymphadenopathy, cellulitis, or a patient who is immunocompromised, antibiotics should be given in addition to drainage of the tooth.
- Relieve the tooth out of occlusion in hyper occlusion cases.
- To control postoperative pain following endodontic therapy, nonsteroidal anti-inflammatory drugs should be given.
Phoenix Abscess Or Recrudescent Abscess Or Acute Exacerbation of Asymptomatic Apical Periodontitis
Phoenix abscess is defined as an acute inflammatory reaction superimposed on an existing asymptomatic apical periodontitis.
Etiology:
Chronic periradicular lesions such as granulomas are in a state of equilibrium during which they can be completely asymptomatic. But sometimes, inflx of necrotic products from diseased pulp or bacteria and their toxins can cause the dormant lesion to react. This leads to the initiation of acute inflammatory response. Lowered body defenses also trigger an acute inflammatory response.
Phoenix abscess Symptoms:
- Clinically, often indistinguishable from the acute apical abscess.
- At the onset, tenderness of the tooth and extrusion of the tooth from the socket.
- Tenderness on palpating the apical soft tissue.
Phoenix abscess Diagnosis:
- Most commonly associated with the initiation of root canal treatment.
- History from patient
- Pulp tests show a negative response
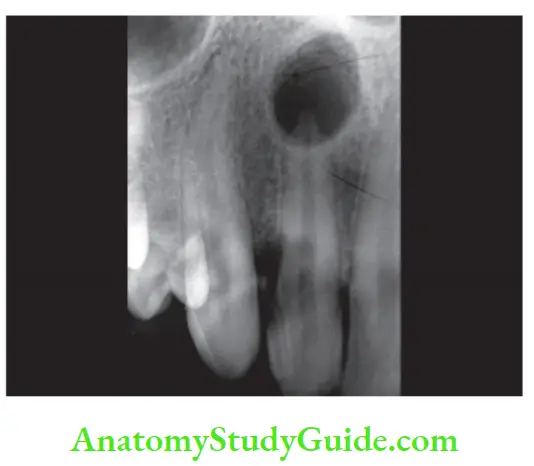
- Radiographs show a large area of radiolucency in the apex created by inflammatory connective tissue which has replaced the alveolar bone at the root apex
- Histopathology of Phoenix abscess shows areas of liquefaction necrosis with disintegrated polymorphonuclear leukocytes and cellular debris surrounded by macrophages, lymphocytes, and plasma cells in periradicular tissues.
- Phoenix abscesses should be differentiated from acute alveolar abscesses by the patient’s history, symptoms, and clinical test results.
Phoenix abscess Treatment:
- Establishment of drainage
- Once symptoms subside—complete root canal treatment
Asymptomatic Apical Periodontitis Or Chronic Apical Periodontitis
It is the sequelae of symptomatic apical periodontitis resulting in inflammation and destruction of periradicular area due to the extension of pulpal infection, characterized by asymptomatic periradicular radiolucency. It is seen as a chronic low-grade defensive response of periradicular area to pulpal infection.
Etiology:
Necrosis of pulp causing continued irritation and stimulation of periradicular area resulting in the formation of granulation tissue.
Apical Periodontitis Clinical features:
- Tooth is nonvital
- Usually asymptomatic but in the acute phase, dull, throbbing pain may be present
Possible complications of chronic apical periodontitis
- Formation of periapical granuloma, radicular cyst, sinus tract, and acute exacerbation of the disease.
Apical Periodontitis Diffrential Diagnosis:
A main characteristic feature is a nonvital pulp with a periapical lesion. If the pulp is vital:
- Rule out lateral periodontal abscess, central giant cell granuloma, and cemental dysplasia.
- Check medical history to rule out hyperparathyroidism or the presence of malignant lesions.
Apical Periodontitis Treatment:
- Endodontic therapy of affected tooth.
- In the acute phase, treatment is the same as acute apical abscess, i.e. cleaning and shaping of canals followed by analgesics if required.
- Extraction of nonrestorable teeth.
Chronic Alveolar Abscess
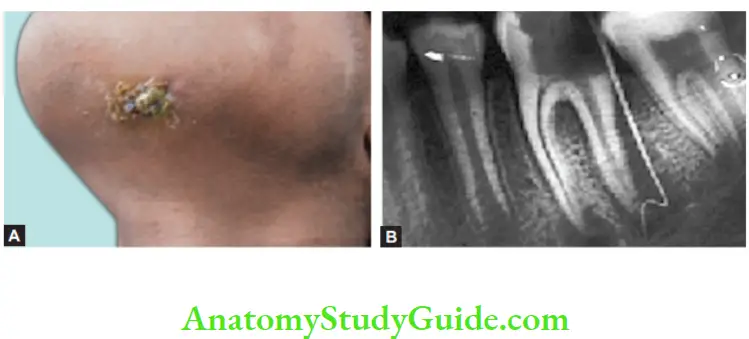
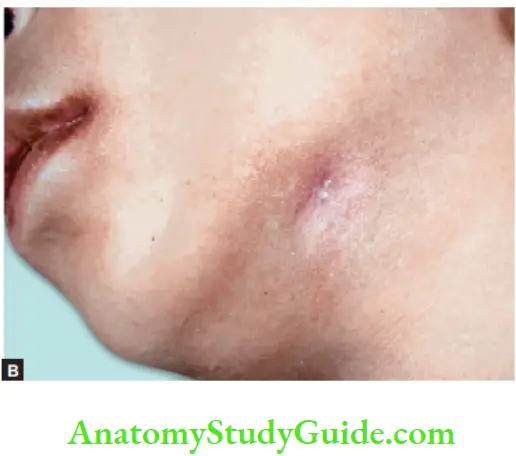
A chronic alveolar abscess is a long-standing low-grade infection of periarticular bone characterized by the presence of an abscess draining through a sinus tract.
Chronic Alveolar Abscess Synonyms:
Chronic suppurative apical periodontitis, Chronic apical abscess, Suppurative periradicular periodontitis, Chronic periradicular/periapical abscess.
Etiology:
It is similar to an acute alveolar abscess. It also results from pulpal necrosis and is associated with chronic apical periodontitis that has formed an abscess.
Chronic Alveolar Abscess Symptoms:
- Generally asymptomatic
- Detected either by the presence of a sinus tract or on the routine radiograph.
- In the case of an open carious cavity, the drainage through the root canal sinus tract prevents swelling or exacerbation of the lesion.
Chronic Alveolar Abscess Diagnosis:
- A chronic apical abscess is associated with an asymptomatic or slightly symptomatic tooth.
- The patient may give a history of sudden sharp pain which subsided and has not reoccurred.
- The clinical examination may show a large carious exposure, discoloration of the crown, or restoration.
- The presence of a sinus tract prevents exacerbation or swelling so usually asymptomatic but may show symptoms if the sinus tract gets blocked.
- Vitality tests show a negative response because of the presence of necrotic pulps.
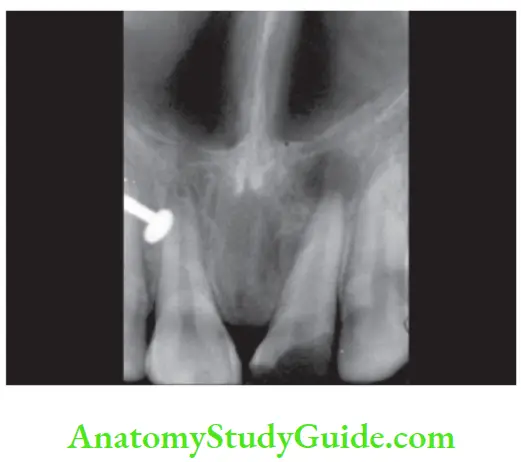
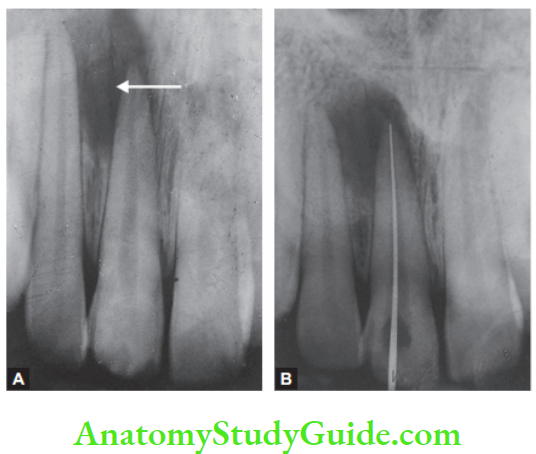
- The site of origin is diagnosed by radiograph after insertion of gutta-percha in the sinus tract.
- Radiographic examination shows diffuse areas of rarefaction. The rarefied area is so diffuse that fades indistinctly into normal bone.
Chronic Alveolar Abscess Diffrential Diagnosis:
The chronic alveolar abscess must be differentially diagnosed from a granuloma or cyst by carrying histopathological examination. It should also be diffrentiated from cementoma which is associated with the vital tooth.
Chronic Alveolar Abscess Treatment:
Removal of irritants from a root canal and establishment of drainage is the main objective of the treatment. Sinus tract resolves following the endodontic treatment.
The draining sinus is active with pus discharge surrounded by reddish-pink color mucosa. It can be detected by inserting gutta-percha. Healed sinus shows the absence of pus discharge and normal-colored mucosa.


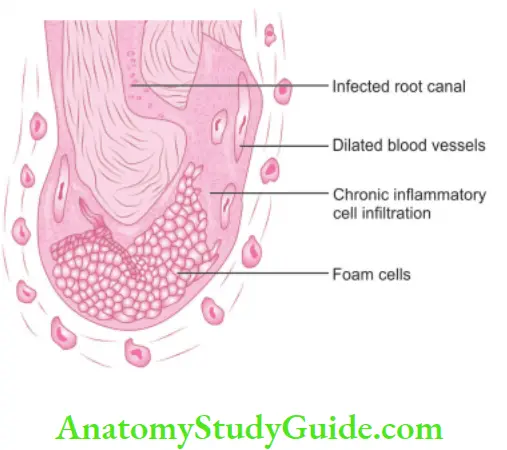
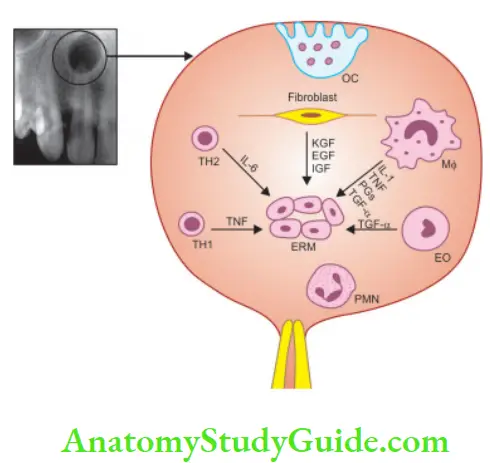
Periapical Granuloma
Periapical granuloma is one of the most common sequelae of pulpitis. It is usually described as a mass of chronically inflamed granulation tissue found at the apex of a nonvital tooth.
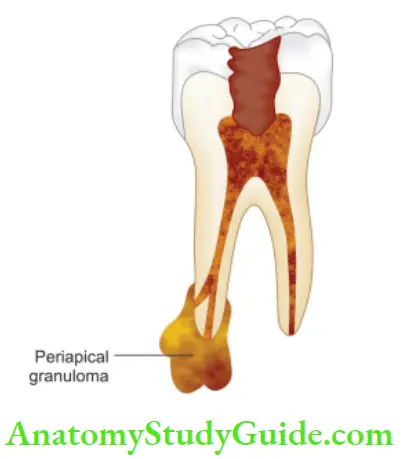
Etiology of Periapical Granuloma:
Periapical granuloma is a cell-mediated response to pulpal bacterial products. Bacterial toxins cause mild irritation of periapical tissues. This leads to cellular proliferation and thus granuloma formation
Periapical Granuloma Clinical Features:
- Most of the cases are asymptomatic but sometimes pain and sensitivity is seen when acute exacerbation occurs.
- The tooth is not sensitive to percussion
- No mobility
- Soft tissue overlying the area may/may not be tender
- No response to thermal or electric pulp test
- Mostly, lesions are discovered on routine radiographic examination
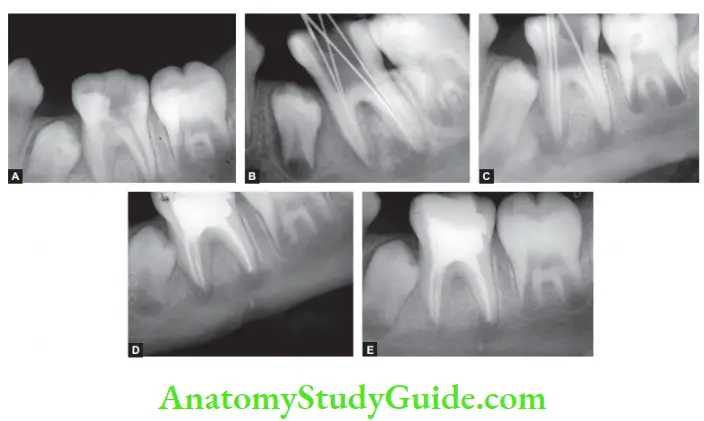
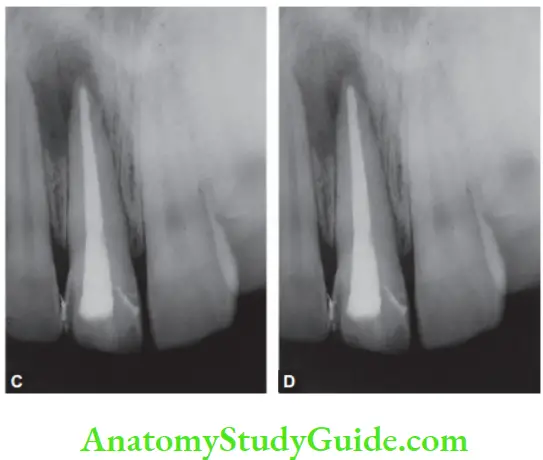
Periapical Granuloma Radiographic Features:
- Mostly discovered on routine radiographic examination.
- The earliest noticeable change seen is a thickening of the periodontal ligament at the root apex.
- The lesion may be well-circumscribed or poorly defied.
- Size may vary from small lesion to large radiolucency exceeding >2 cm in diameter.
- The presence of root resorption is also seen
Periapical Granuloma Histopathologic Features.
- It consists of inflamed granulation tissue that is surrounded by a firous connective tissue wall.
- The granulation consists of dense lymphocytic infiltrate which further contains neutrophils, plasma cells, histiocytes, and eosinophils.
- Sometimes, Russell bodies may also be present
Periapical Granuloma Treatment and Prognosis.
- In restorable teeth, endodontic treatment is, and in case of the nonrestorable tooth, extraction followed by curettage of apical soft tissue is recommended.
Radicular Cyst Or Cystic Apical Periodontitis
The radicular cyst is an inflammatory cyst which results because of the extension of infection from the pulp into the surrounding periapical tissues.
Etiology:
- Caries, physical, chemical, or mechanical injury resulting in pulp necrosis.
- Irritating effects of restorative materials.
- Trauma.
- Pulpal death due to developmental defects.
Radicular Cyst Pathogenesis:
Periapical granulomas are initiated and maintained by the degradation products of necrotic pulp tissue. Stimulation of epithelial rests of Malassez occurs in response to inflammatory products.
According to Nair, cyst formation occurs as a result of epithelial proliferation, which helps to separate the inflammatory stimulus from the surrounding bone. By this mechanism, a cyst is formed and it is explained by the following two hypotheses:
Radicular Cyst Nutritional Defiient Theory:
It says that periapical inflammatory changes cause the epithelium to proliferate and make the center mass deprived of nutrition from peripheral tissues. It results in necrotic changes in the center lined by epithelial cells at the periphery.
Radicular Cyst Abscess Theory:
It says when an abscess is formed in connective tissue, epithelial cells proliferate and form a wall around the cavity because of their inherent tendency to cover the exposed connective tissue.
Valderhaug (1972) explained the following stages of cyst formation:
1. Initial stage:
Bacterial endotoxins cause inflammation in the apical region of a nonvital tooth which leads to the proliferation of epithelial cells of Malassez.
2. Cyst development stage:
Proliferative epithelial cells serve as building blocks for cyst wall development. This occurs due to simultaneous decomposition of epithelial and granulation tissue and convergence of multiple cavities, with subsequent epithelialization.
3. Cyst growth stage:
Due to the decomposition of epithelial cells, leukocytes, and accumulation of plasma exudates, the osmolality of the cyst fluid becomes higher than that of the serum. As a result, hydrostatic internal pressure becomes greater than capillary pressure. Tissue fluid, therefore, diffuses into the cyst, making it increase in size.
With osteoclastic bone resorption, the cyst expands. Other bone-resorbing factors, such as prostaglandins, interleukins, and proteinases, from inflammatory cells and cells in the peripheral portion of the lesion, permit additional cyst enlargement
Types of Radicular Cysts:
Nair gave the following two types of radicular cysts:
Periapical Pocket or Bay Cyst:
When proliferation occurs within the body of the granuloma, it plugs the apical foramen which limits the egress of bacteria. Sometimes, epithelial plugs protrude out from the apical foramen resulting in a pouch connected to the root and continuous with the root canal. This is termed as pocket or bay cyst.
Periapical True Cyst:
It is the cavity which is completely enclosed in epithelium lining and is independent of root canal of the offending tooth.
Radicular Cyst Clinical Features:
- Cyst is generally asymptomatic. It is discovered when periapical radiographs of a nonvital tooth is taken.
- Males are affected more than females.
- Peak incidence in the third or fourth decades.
- Commonly found in the anterior maxilla. In mandibular posterior teeth, separate small cysts may arise from each apex of multirooted teeth.
- The involved tooth is nonvital, discolored, fractured, or shows failed root canal.
- It grows as a slowly enlarging swelling. As the cyst increases in size, the covering bone becomes thin and exhibits springiness due to fluctuation.
- In the maxilla, palatal expansion is commonly seen with the maxillary lateral incisor.
Radiographic Features:
Radiographically, the radicular cyst appears as round, pear, or ovoid-shaped radiolucency, outlined by a thin radiopaque margin.
Diffrential diagnosis:
1. Periapical granuloma:
Histological and radiological features differentiate these lesions. Moreover, the cyst is usually larger than a periapical granuloma.
2. Periapical cemento-osseous dysplasia:
It is seen associated with vital teeth or in regions of extractions. Lesion tends to become more opaque internally with time and does not exhibit extensions into adjacent bone.
3. Traumatic bone cyst:
Hollow cavity, not lined by epithelium but by fibrous tissue. Treated by aspiration of fluid from the cavity.
4. Globulomaxillary cyst:
A fissural cyst, a tooth may be vital and develops between the maxillary lateral incisor and canine
5. Lateral periodontal cyst:
It is associated with periodontal signs and symptoms.
6. Normal bony cavity:
It appears dissociated from the root apex whereas the residual cyst remains attached to the root apex.
7. Previously treated apical pathology/surgical defect or periapical scar.
8. Odontogenic tumors:
Ossifying fibroma is commonly seen in the posterior region of the mandible, adenomatoid odontogenic tumor in the anterior maxilla, and calcifying cystic odontogenic tumor is associated with unerupted teeth. In these lesions, the pulp is usually vital.
9. Giant cell lesion
10. Metastatic lesion
Radicular Cyst Treatment:
Different options for the management of residual cysts are
- Endodontic treatment
- Apicoectomy
- Extraction (severe bone loss)
- Enucleation with primary closure
- Marsupialization (in case of large cysts)
Condensing Osteitis
Condensing osteitis is a diffuse radiopaque lesion believed to form a localized bone reaction to a low-grade inflammatory stimulus, normally seen at an apex of a tooth in which there has been a long-standing pulp disease.
Condensing Osteitis Clinical Features:
- Usually asymptomatic, it is commonly seen around the apices of mandibular molars and premolars with chronic pulpitis.
- The pulp can be vital and chronically inflamed or necrotic.
- The tooth has a radiopaque area due to the overproduction of bone in the periapical area. Radiopacity may or may not disappear after endodontic treatment or tooth extraction.
Condensing Osteitis Diagnosis:
Usually discovered on routine radiographs, it appears as a localized area of radiopacity surrounding the offending tooth.
Condensing Osteitis Histopathology:
The dense bone around the root apex shows less trabecular pattern and borders lined with osteoblasts along with the presence of chronic inflammatory cells in bone marrow.
Condensing Osteitis Treatment:
- Endodontic treatment may result in complete resolution.
External Root Resorption
Resorption is associated with either a physiologic or a pathologic process that results in the loss of tissues like dentin, cementum, or alveolar bone.
In external root resorption, root resorption affects the cementum or dentin of the root. It can be
- Apical root resorption
- Lateral root resorption
- Cervical root resorption
Etiology:
Periradicular inflammation due to
- Infected necrotic pulp
- Over-instrumentation during root canal treatment
- Trauma
- Granuloma/cyst applying excessive pressure on the root
- Replantation of teeth
- Adjacent impacted tooth
External Root Resorption Symptoms:
- Asymptomatic during development
- When the root is completely resorbed, the tooth becomes mobile
- When external root resorption extends to the crown, it gives a “pink tooth” appearance.
- When replacement resorption results in ankylosis, the tooth becomes immobile with a characteristic high percussion sound.
External Root Resorption Radiographic Features:
- Radiolucency at the root and adjacent bone
- Irregular shortening or thinning of the root tip
- Loss of lamina dura
External Root Resorption Diffrential Diagnosis:
It should be diffrentiated from internal resorption which shows ballooning of pulpal space.
External Root Resorption Treatment:
- Removal of the stimulus of underlying inflammation
- Nonsurgical endodontic treatment should be tried first before attempting surgical treatment.
Persistent Apical Periodontitis
It is post-treatment apical periodontitis in an endodontically treated tooth. Enterococcus faecalis is the most consistently reported organism in persistent apical periodontitis.
Etiology:
- It may result because of incomplete cleaning of complex pulp space which is inaccessible to instrumentation, irrigation, and thus obturation.
- Nair listed the following extraarticular factors which contribute to persistent apical periodontitis:
- Foreign body reaction to gutta-percha
- Periapical biofilms
- Cholesterol crystals
- Periapical scar tissue
- Actinomyces infection
Diseases Of Periradicular Tissue Of Nonendodontic Origin
Periradicular lesions may arise from the remnants of odontogenic epithelium.
Benign Lesions:
- Early stages of periradicular cemental dysplasia
- Early stages of monostotic fibrous dysplasia
- Ossifying fibroma
- Primordial cyst
- Lateral periodontal cyst
- Dentigerous cyst
- Traumatic bone cyst
- Central giant cell granuloma
- Central hemangioma
- Hyperparathyroidism
- Myxoma
- Ameloblastoma
Radiographic Features of Lesions of Nonodontogenic Origin:
- Presence of radiolucent areas
- Intact lamina dura
Diagnosis:
Teeth associated with nonodontogenic lesions are usually vital. The final diagnosis is based on a surgical biopsy and histopathological examination.
Malignant Lesions:
They simulate endodontic periradicular lesions and are often metastatic in nature:
- Squamous cell carcinoma
- Osteogenic sarcoma
- Chondrosarcoma
- Multiple myeloma
Diagnosis:
1. Vitality:
The involved tooth is vital but disruption of sensory nerves may show no response
2. Radiographic features:
Lesions are associated with rapid and extensive loss of hard tissue, that is, bone and tooth.
3. Biopsy:
Histological evaluation of diagnosis.
Conclusion:
One of the most important clinical factors for pulpal pain is caries which affects pulp by bacteria or their byproducts. Once the pulp gets affected by bacteria or their by-products, its inflammation starts, which if not timely treated, might develop into pulp necrosis.
Toxic byproducts formed as a result of pulp decomposition act as irritants on the periapical tissues and give rise to many forms of reactions and the latter involve periradicular tissues.
Some of these reactions occur for a short time accompanied by signs and symptoms, others develop slowly and are asymptomatic. To save a tooth from sacrificing, a proper diagnosis based on clinical, radiographically, and histological basis should be made so as to provide optimal treatment to the lesion.
In suspicious cases, a biopsy of the lesion, referral to the pathologist, and long-term follow-up is required.
Leave a Reply