Formation Of Germ Layers
Fertilization
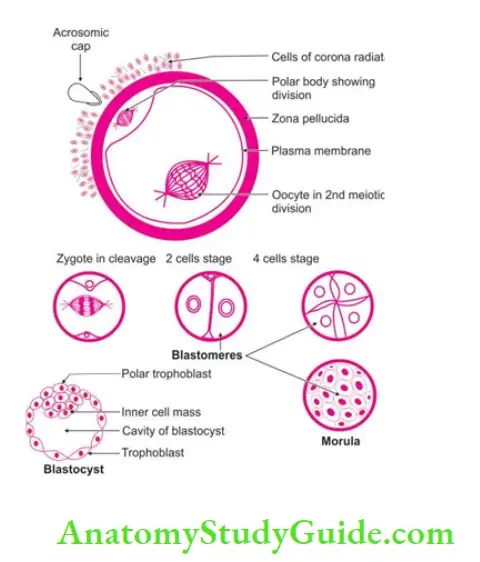
Fertilization Introduction: It is the fusion of male ♂ and female ♀ pronuclei (sperm and secondary oocyte) to form the zygote.
Table of Contents
1. Fertilization Site: Fertilization occurs in the ampulla of the fallopian tube.
2. Fertilization Duration: It occurs within 24 hrs of ovulation.
3. Fertilization Prerequisite (capacitation): It needs to cross three barriers. Barrier of
- The cells of the corona radiata,
- Zona pellucida, and
- Vitelline membrane.
Read And Learn More: General Histology Question And Answers
4. Fertilization Mechanism:
1. Cells of corona radiata are disintegrated by the enzyme hyaluronidase.
2. Zona pellucida is digested by the enzyme acrosin and neuraminidase.
3. Many sperms get embedded in zona pellucida but when 1 sperm reaches vitelline membrane. Following changes occur in the structure.
- Calcium wave spreads in secondary oocyte.
- The cortical granules are released.
- Ovum is formed.
- Second meiotic division is completed.
- The cortical granules react with zona pellucida and make it impermeable to other sperms (i.e. acro-reaction is inhibited).
4. Only head enters the cytoplasm and gets changed into male ♂ pronucleus. There is a replication of DNA material. (Chromosome number may be 22X
5. female ♀ Pronucles is also formed.
6. Nuclear membrane disappears and the mixing of chromosomes occur.
7. It results into a diploid number of chromosomes.
8. The zygote is formed.
9. The cleavage starts.
5. Results of fertilization:
- The oogenesis cycle is complete.
- The chromosomal number is restored.
- The sex is determined.
- The cleavage starts.
- The genetic combination leads to variations in the human species.
6. Effects on:
1. Ovary: The corpus luteum changes to the corpus luteum of pregnancy.
2. Uterus: The secretory changes start in the endometrium.
3. Zygote: The cleavage starts.
7. In vitro fertilization: The pre-ovulatory oocyte is taken out with laparoscopy and is fertilized outside.
Amnion
Amnion Introduction: It is thin but tough extra-embryonic membrane derived from angiogenic cells. It forms the wall of the amniotic cavity. It excludes the cells of the ectoderm.
It forms the hydrostatic bag. It contains fluid which envelopes the embryo, umbilical cord and fetal part of placenta.
1. Chronological age: 2nd week after fertilization.
2. Responsible cells: Responsible cells are angiogenic cells. They are derived from the trophoblast cells which are present on the roof of ectoderm cells.
3. Sources of amniotic fluid: Sources of amniotic fluid are mainly from
- Maternal blood
- Amniotic cells, and
- Urine secreted by fetus.
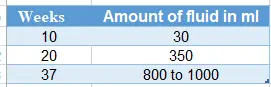
The volume of amniotic fluid
4. Circulation of amniotic fluid:
- Part of the fluid goes into maternal blood.
- Part of it is swallowed by the fetus.
- Excess of water in fetal blood is excreted by urine and to the amniotic cavity.
5. Composition of amniotic fluid:
- Desquamated fetal epithelial cells
- Water
- Fats
- Enzymes
- Pigments, and
- Hormones.
6. Significance of fluid:
- Allows free movement of the fetus which helps in the development of the musculo¬skeletal system.
- Permits symmetrical external growth of the embryo.Prevents adherence of amnion to the embryo.
- Prects embryo against injuries.
- Regulates the body temperature of the embryo.
- Dilates cervix during the act of parturition along with chorionic membrane.
7. Anomalies:
1. Oligohydramnios: The amniotic fluid is less than 400 ml. The complications of the oligohydramnios include fetal abnormalities. These are
- Pulmonary hypoplasia
- Facial defects
- Limb defects
- Urinary agenesis, and
- Compression of the umbilical cord.
2. Polyhydramnios: The amniotic fluid is more than 2000 ml. It is associated with the
- Severe anomalies of the central nervous system, and
- Oesophageal atresia.
8. Applied anatomy:
1. Amniocentesis: It is a process by which amniotic fluid is removed and studied for the cells by 16 to 20 weeks.
2. Detection of the abnormal fetus, for example, spina bifida. It is detected by the estimation of alpha-fetoprotein. The level is increased in neural tube defects like spina bifida.
3. Determination of the sex.
Yolk sac
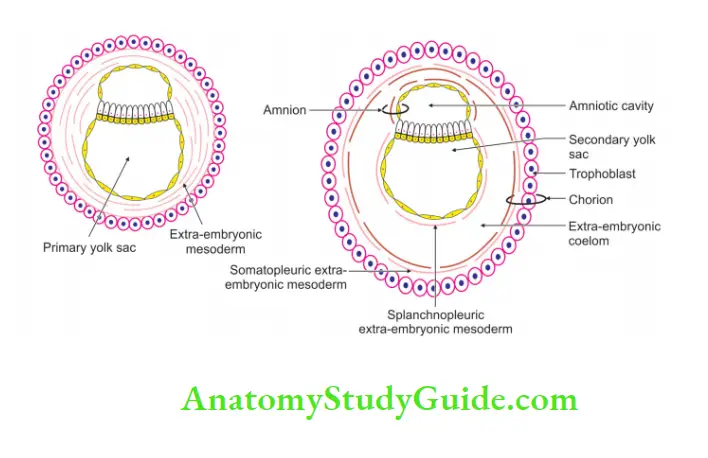
Yolk sac Introduction: The inner wall of the cavity of the blastocyst is lined by flattened cells called Heuser’s membrane (future endodermal cells). Such a structure is called a primary yolk sac. It is described in three stages.
1. Primary yolk sac: During the 9th day of development, flattened cells originating from the endoderm form a thin membrane. This is called Heuser’s membrane. This membrane together with the cells of endoderm forms the primary yolk sac.
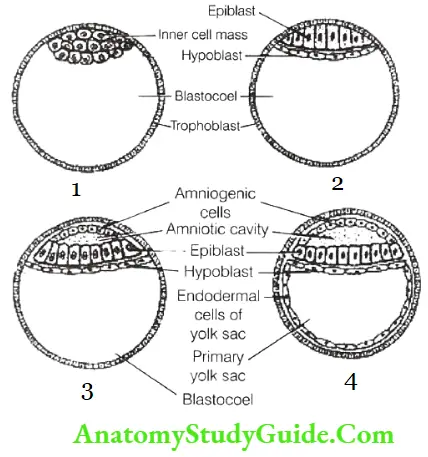
2. Definitive or secondary yolk sac: By the 13th day, the extra-embryonic mesoderm is filled by
The cavity is called extra-embryonic coelom. This is much smaller than the primary yolk sac cavity. The decrease in the size is accompanied by a change in the nature of lining cells. They are no longer flattened cells. They become cubical.
3. Tertiary yolk sac: It is a remnant of the secondary yolk sac. It is divided into the following parts.
- Intra-embryonic part: It gives rise to the foregut, midgut, and hindgut.
- Intermediate or connecting part: It is also called the vitellointestinal duct.
- Extra-embryonic part: This is called the tertiary yolk sac.
4. Yolk sac Chronological age: 2nd week after fertilization.
5. Yolk sac Functions:
1. Nutrition to the embryo.
2. Haemopoiesis
3. Formation of
1. Epithelium of
- Gastrointestinal tract
- Respiratory tract, and
- Urinary bladder.
2. Male ♂ and female ♀ primordial genn cell.
6. Yolk sac Fate:
1. The yolk sac detaches from the midgut loop. Its stalk (vitellointestinal duct) remains in continuation with the midgut loop. It persists as a diverticulum called Meckel’s diverticulum.
2. Allantois in its distal part form a remnant called urachus. It extends from the apex of the bladder to the umbilicus. With the folding of the embryo
The yolk sac incorporates into the developing gut tube and it reduces considerably. It lies in connecting stalk.
Primitive Streak
Primitive Streak Introduction: It is a thickened band of ectodermal cells at the caudal end of the embryo. It is in the midline.
1. Primitive Streak Cells involved: The pluripotent cells, i.e. ability to transform into any type of cells.
2. Primitive Streak Chronological age: 15th day of intrauterine life. It is a very important stage in the formation of the embryo. It is recollected by associating with the 15th of August, the Independence Day of India.
3. Primitive Streak Description:
1. It continues laterally up to the margins of the embryonic disc.
2. It continues caudally up to the cloacal membrane and goes into the connecting stalk.
3. The cells of the primitive streak are absent at
- Prochordal plate, and
- Cloacal membrane.
4. The cells passing beyond the prochordal plate form a cardiogenic area.
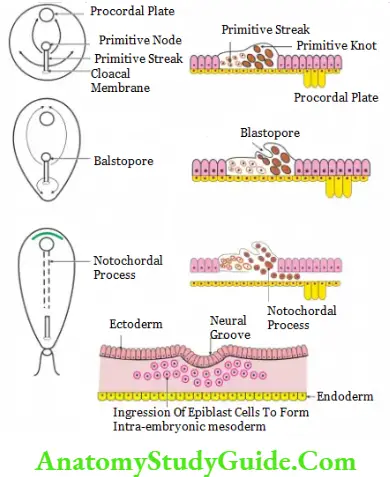
4. Primitive Streak Functions:
1. It organizes intra-embryonic mesoderm (i.e. 3rd germ layer).
2. It confirms the future craniocaudal axis of the embryo.
3. It divides into the left and right half of the embryo.
4. It differentiates into notochord.
5. Primitive Streak Fate:
Cells of primitive streak are continuously formed up to 3rd week. They regress but remain up to 4th week. Cells of primitive streak give rise to
Lateral part of paraxial mesoderm
1. Primordial germ cells
2. Intra-embryonic mesoderm, and
3. Extra-embryonic mesoderm.
6. Primitive Streak Applied anatomy:
If the cells of the primitive streak persis even after 4th week, they give rise to the teratogenic tumor at the sacrococcygeal region.
7. Primitive Streak Recent view: Primitive node gives rise to
- Notochord
- Medial part of paraxial mesoderm, and
- Endoderm.
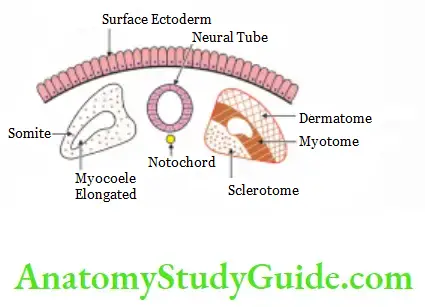
Somites
Somites Introduction: The solid brick-like segmentation of paraxial intra-embryonic mesoderm on either side of notochord is called somites.
1. Somites Extent: It extends from the cranial end of the notochord to the coccygeal end.
2. Somite’s Chronological age: 20 to 30 days.
3. Somites Total number of somites: They are as follows
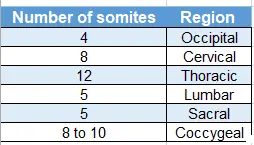
4. Derivatives:
1. Sclerotome:
- Axial skeleton
- Ribs, and
- Sternum.
2. Myotome: Muscles of
- Back
- Front, and
- Lhnbs.
3. Dermatome: Dermis of skin of the
- Back, and
- Front
5. Somites Never supply: Mesodermal somites are supplied by corresponding segments of the spinal card.
6. Somites Applied anatomy
1. The age of the fetus can be determined by counting the number of somites.
2. Spina bifida: The two halves of the neural arch may fail to fuse in the midline.
3. Hemivertebrae: Incomplete development of one-half of a vertebra.
Trophoblast
Trophoblast Introduction: The cells lining the surface of the morula constitute the trophoblast.
The trophoblast has the property of attaching itself to and invading any tissue it comes in contact with. Once the zona pellucida disappears, the cells of the trophoblast stick to the uterine endometrium. This is called implantation.
Villi are formed as offshoots from the surface of the trophoblast. The trophoblast along with the underlying extra-embryonic mesoderm forms the chorion. The villi arising from the chorion is called the chorionic villi.
Initially, the trophoblast is made up of a single layer of cells. As these cells multiply, two distinct layers are formed. The cells, close to the decidua (most superficial cells), lose their cell walls.
Thus, a continuous sheet of cytoplasm containing many nuclei is formed. Such a tissue is called a syncytium. Hence, the layer of trophoblast is called syncytiotrophoblast or plasmodiotrophoblast.
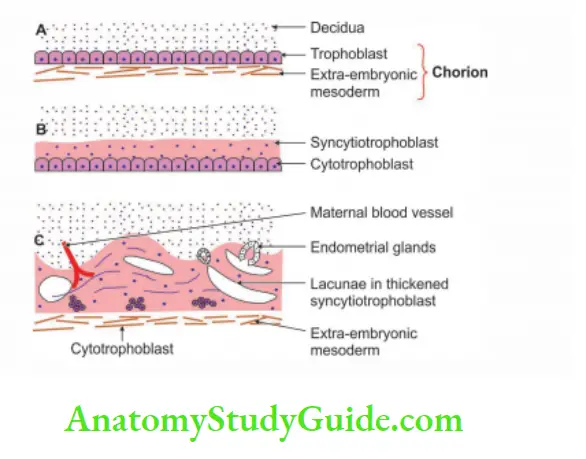
Deep to the syncytium, the cells of the trophoblast retain their cell walls and form the 2nd layer called cytotrophoblast [Langhans layer].
Leave a Reply