Question 1: Define gingiva.
Answer:
The gingiva is defined as that part of the oral mucosa that covers the alveolar processes of the jaw and surrounds the necks of the teeth.
Question 2: Describe the normal anatomy of gingiva.
Answer:
The gingiva is divided anatomically into marginal, attached, and interdental or papillary gingiva.
.Read And Learn More: Periodontology Important Question And Answers
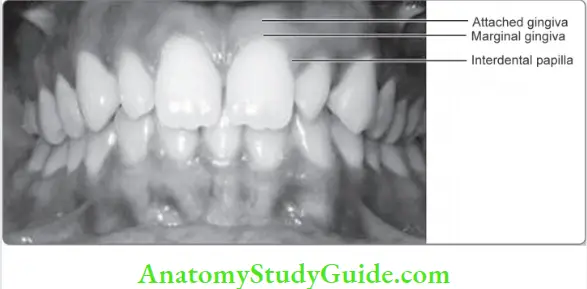
Marginal Gingiva Or Free Gingiva Or Unattached Gingiva
The free gingiva or the unattached gingiva is the terminal portion that forms a collar around the teeth and which can be deflected from the tooth surface with help of a periodontal probe.
- It is demarcated from the adjacent attached gingiva by a shallow linear groove- the free gingival groove, which may not always be clinically visible.
- The marginal gingiva forms the soft tissue wall of the gingival sulcus (or crevice) which is a V-shaped space between the free gingiva and the tooth surface.
- Apical to the sulcus, the junctional epithelium is firmly attached to the tooth structure at the cementoenamel junction.
- This anatomical landmark represents the only site at which there is a union between tooth and gingiva in health.
- In clinically healthy human gingiva, the clinical probing depth (from the gingival margin to base of the sulcus) of the gingival sulcus is 2 to 3 mm.
- Histologically, the sulcus depth is reported to be 1.8 mm, however, in a germ-free environment, there may be complete absence of a sulcus.
Attached Gingiva
- The attached gingiva, unlike the marginal gingiva, is bound firmly by the periosteum to the alveolar bone, as a result of which it is immobile.
- This film adhesion gives attached gingiva the ability to bear stress during function (e.g., mastication). Attached gingiva extends from the apical border of the marginal gingiva to the mucogingival junction.
- On the palatal aspect, there is no discernable anatomic distinction between attached gingiva and palatal mucosa.
Gingiva Dimensions
The apico-coronal dimension or the width (height) of attached gingiva varies, decreasing from the facial aspect of the anteriors (3.5 to 4.5 mm in the maxilla and 3.3 to 3.9 in the mandible) to the molar areas (1.9 mm in the maxilla and 1.8 mm in the mandible).
It is narrowest on the facial surface of mandibular first premolars partly because of the presence of accessory frenae.
Width of Attached Gingiva
- Width of attached gingiva is measured from mucogingival junction to free gingival groove or the projection of gingival sulcus externally.
- The width of the attached gingiva exhibits considerable variation between individuals. Developmental abnormalities may result in mucogingival deformities in which attached gingiva may be decreased/absent.
- Within the same individual, the width of attached gingiva tends to increase with age and supraeruption.
Papillary Gingiva, Interdental Gingiva
- The portion of the gingiva that occupies the interdental space (gingival embrasure) between two adjacent teeth is the interdental or papillary gingiva.
- It is pyramidal in shape between anterior teeth. In the posterior teeth, the interdental papillae are more tent-shaped with high facial and lingual peaks and the central area is depressed like a saddle- the “col”, and is covered by thin nonkeratinized, epithelium.
Question 3: What are the clinical implications of the anatomical zones of gingiva?
Answer:
Marginal gingiva and interdental papilla together contributes to the esthetics and has important functional implications.
Gingival Zenith
Gingival zenith is the apical most part of the marginal gingiva.
For Good Esthetics
- Gingival zenith needs to be bilaterally symmetrical and in harmony with the lip line.
- Zenith is distal to the midline in central incisors, at the midline in the laterals, and canine.
- Zenith is at a coronal level in the lateral incisors when compared to central incisor and canine, which may be at the same level.
Interdental Papilla
Loss of papilla leads to black triangles and unesthetic appearance in natural teeth, restorations, and implants. Interdental papilla can fill the embrasure space and esthetic results are good if the distance between the contact point and the crest of alveolar bone is 5 mm or less.
The interdental areas in posterior teeth are more susceptible to periodontal disease as:
- This region is inaccessible to regular mechanical plaque control measures and
- The nonkeratinized col allows bacteria and their products into the periodontium resulting in chronic inflmmation and tissue destruction.
Attached Gingiva
The importance of the attached gingiva is that it;
- Acts as a buffer that prevents deflection of the marginal gingiva and accumulation of food in the gingival sulcus.
- As it is keratinized gingiva consists of dense collagen fibers, is more resistant to inflammatory spread and mechanical trauma. The width of the attached gingiva is affcted by changes occurring in the gingival margin as the mucogingival junction remains stationary throughout life.
A minimal width of attached gingiva may contribute to periodontal health, especially in relation to abutment teeth or restorations involving the gingival margin; implants, and during orthodontic treatment.

Question 4: Describe the histological features of gingiva.
Answer:
The gingiva consists of an epithelial component and a connective tissue component (lamina propria) which is separated from each other by a basal lamina (basement membrane).
Gingival Epithelium
The gingival epithelium is classified as a stratified squamous epithelium. The layers of the squamous epithelium are:
- Stratum basale or the formative layer
- Stratum spinosum/prickle cell layer
- Stratum granulosum. These cells are fltter and contain keratohyalin granules
- Stratum corneum or the cornif ed layer. These cells are much more fatter, shrunken and kerati-Stratum corneum or the cornified layer. These cells are much more fltter, shrunken, and keratinized.
The principal cell type of the epithelium is the keratinocyte; while nonkeratinocytes include the melanocytes in the basal or spinous layer, langerhans cells in the suprabasal layer, merkel cells which are tactile receptors.
Gingival Epithelium
Based on their morphology and function, the gingival epithelium is divided into three segments
- The oral (surface) epithelium lining the outer surface of marginal, attached, and interdental gin-Th oral (surface) epithelium lining the outer surface of marginal, attached, and interdental gingiva.
- The sulcular Epithelium which lines the gingival sulcus.
- The junctional Epithelium which is attached to the tooth on one side and basal lamina of the lamina propria of gingiva on the other.
Oral or outer Epithelium
- The oral epithelium is present in the external gingival surface which is keratinized to varying degrees.
- About 15% of the surface gingiva is fully keratinized (ortho keratinized), 10% nonkeratinized, and 75% para keratinized (stratum corneum retaining pyknotic nuclei, keratohyalin granules are dispersed without a stratum granulosum).
- In the gingiva, the epithelium is arranged in the form of down growths called rete ridges.
- Cytokeratins expressed in the outer epithelium include K1,K2, K10 – K12 orthokeratinized areas, K6 and K16 (indicating highly proliferative epithelium), K5 and K14 ( Stratifiation specifi keratins)
Sulcular Epithelium
- The sulcular epithelium has only the basal and spinosal layers. Unlike the oral epithelium, the sulcular epithelium has no regular rete pegs.
- Importantly, there is no keratinization in the sulcular epithelium and it therefore lacks granulosum and corenum strata. Persistent inflammation present in the sulcus may be the reason for the lack of keratinization.
- The sulcular epithelium can become keratinized in germ free conditions and when the sulcular epithelium is exposed to the oral cavity.
Junctional Epithelium
- The Junctional Epithelium mediates attachment to the tooth and consists of a layer of squamous epithelial cells.
- In health, the Junctional Epithelium extends approximately 0.25 to 1.35 mm coronoapically and can be 12–20 layers thick at the coronal part tapering down to 1–2 cells thickness at the apical extent.
- The cells of the junctional epithelium can be divided into three layers based on their primary function as follows; the apical zone which provides germination; the middle zone which is important for tooth adhesion and the coronal zone which is responsible for permeability.
- Epithelial attachment refers to the mechanism through which the junctional epithelial cells are attached to the tooth surface through the internal basal lamina and hemidesmosomes.
- The Junctional epithelium, unlike other epithelia, has two basal lamina- the Internal Basal Lamina which faces the tooth surface, and the External Basal Lamina that faces the connective tissue.
Gingival Connective Tissue
The connective tissue consists of cells and fires, primarily collagen in an amorphous nonfibrous and non cellular matrix made up of noncollagenous proteins such as glycosaminoglycans, proteoglycans, and glycoproteins.
- These components are required for influencing the cells (fibroblasts) to respond to external stimuli and maintain the homeostasis of the gingiva.
- This organization is required to meet the physical stress of mastication.
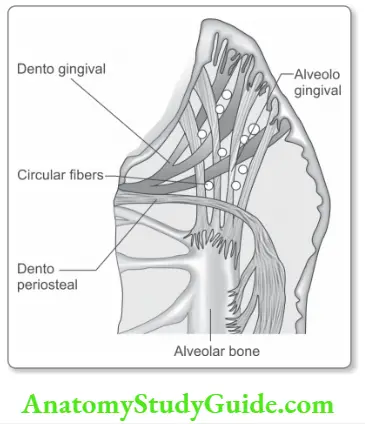
Gingival Fibers
The type I collage fibers are arranged in fier bundles called the gingival fibers, in the marginal gingiva and together with the JE constitute the Dentogingival unit. The functions of the gingival fibers are:
- To brace the marginal gingiva against the tooth
- To provide rigidity to withstand mechanical forces and
- To prevent deflection of the marginal gingiva away from the teeth.
The gingival fibers are arranged into groups;
- Dentogingival fier group: These fibers arise from cervical cementum and pass out in a fan fashion into the lamina propria. They are the most numerous fier group.
- Alveologingival fier group: These fiers run from the alveolar crest into the lamina propria of the gingiva.
- circle the tooth in the lamina propria and interlace with other fibers. This “pursestring” fier arrangement helps hold the marginal gingiva tightly to the tooth.
- Dentoperiosteal fier group: These fibers arise from the cervical cementum and after heading towards the periosteum on the facial/lingual cortical plates/alveolar crest, they terminate in the periosteum of bone.
- Transseptal fier group: These fiers insert in the cementum of one tooth to the cementum of the adjacent tooth. Thy support the interdental gingival papillae and represent an important barrier to apical migration of junctional epithelium.
- Semicircular fiers: These fibers attach at the proximal surface of a tooth, immediately below the cementoenamel junction, go around the facial or lingual marginal gingiva of the teeth and attach on the proximal surface of the same teeth.
- Transgingival fiers: These fibers attach to the proximal surface of one tooth, go around the facial or lingual surface of the adjacent teeth and again transverse the interdental space diagonally and attach in the proximal surface of the next teeth.
Cells of Gingival Connective Tissue
- The majority of cells in gingival connective tissue are fibroblasts. These fibroblasts which make up nearly 50% of the cells produce the connective tissue matrix of the gingiva that offers it mechanical and biological properties.
- Monocytes, macrophages, lymphocytes, and plasma cells are also located in the gingiva.
- These cells are usually present in small numbers in healthy gingiva. Macrophages are usually present as a dense zone very close to the junctional epithelium.
- Mast cells are also found scattered in small quantities in the gingiva.
Question 5: Differences between gingival and periodontal fibers.

Question 6: What are the clinical implications of the histological findings in gingiva?
Answer:
The keratinized oral epithelium consists of cells that are closely packed together through the presence of numerous tight junctions and desmosomes. They function
- To provide a barrier that is impermeable to fluids and bacteria
- As a barrier to resist masticatory stress.
- The oral epithelium is para-keratinized and, therefore not terminally differentiated. Consequently, it retains the ability to de-differentiate- a feature that helps form the long junctional epithelium following periodontal therapy.
- The junctional epithelium on the other hand consists of loosely packed cells with no tight junctions and few desmosomes that allow the presence of neutrophils between the cells.
- Its main function is to provide immune surveillance against bacteria that colonize the sulcus and bacterial products that may penetrate into the tissue through the permeable epithelia.
- There is a need for constant remodeling to replace old tissue with new tissue in the gingiva as it is constantly exposed to mechanical stress – a high cellular activity of the gingival fibroblasts is therefore necessary.
- These cells can also modulate the host response. Most of the changes in the size and shape of the gingiva whether due to inflammatory changes or due to drugs due to changes in the connective tissue more than the epithelium.
Question 7: Write a note on the blood supply and nerve supply.
Answer:
- Superior and inferior alveolar arteries are the sources of the blood supply.
- Branches of these vessels pass into the gingiva from the facial and lingual areas external to the periosteum of the alveolar bone with a rich anastomosis with vessels from the periodontal ligament.
- The interdental gingiva is comparatively less rich in vascularity with a gingival plexus providing an end artery-like blood supply.
- The maxillary and mandibular branches of the trigeminal nerve are the principal sensory fibers of the gingiva.
Question 8: Biological width.
Answer:
Biological width comprises the gingival sulcus, junctional epithelium, and the gingival fibers together. Sometimes referred to as the suprarenal fiers. In health, it is reported to be around 2.04 mm.
Biological Relevance
It is an important clinical parameter to be kept in mind when performing procedures such as crown lengthening.

Question 9: What are the clinical features of a healthy gingiva?
Answer:
Gingiva Color
Healthy gingival tissues are pink in color. The color is dependent upon the thickness of the epithelium, degree of keratinization, vascularity, and the presence of pigments such as melanin in Indian populations.
Gingiva Contour
The healthy gingiva follows the contour of the underlying alveolar bone thus forming a scalloped arcuate outline. This contour may be altered depending on the alignment of teeth in the arch.
Gingiva Consistency
The healthy gingiva is firm and resilient due to the collagenous nature of the connective tissue.
Gingiva Size and Shape
The size and shape of the gingiva are dependent on the cellular and extracellular components in the connective tissue. In healthy gingiva, the interdental papilla is pyramidal and pointed, while the gingival margin is knife-edged.
Gingiva Texture
- In health, the gingival surface is not smooth but pitted, giving the appearance of an orange peel. This is termed stippling.
- Stippling can be appreciated in the interdental papillae and attached gingiva. Stippling is thought to increase the surface area to facilitate resistance to masticatory load.
Gingiva Position
In health, the gingival margin is 1–2 mm coronal to the cementoenamel junction.
Leave a Reply