Blood
Hematinics
Hematinics are compounds required in the formation of blood and are used in the treatment of anemias. Hematinics include iron, vitamin B12 and folic acid and are essential for normal erythropoiesis.
Iron
Iron is essential for hemoglobin production. Total body iron is about 2.5–5 g, two-thirds of which is present in hemoglobin. Each molecule of hemoglobin has 4 iron-containing residues. It is also present in myoglobin, cytochromes, and other enzymes.
Read And Learn More: Pharmacology Question And Answers
Distribution of Iron in the Body:
- Hemoglobin 66%
- Ferritin, hemosiderin 25%
- Adult female 1–2 mg
- Myoglobin (in muscles) 03%
- Enzymes (cytochromes, etc.) 06%
Daily Requirement of Iron:
- Adult male 0.5–1 mg
- Adult female 1–2 mg
- Pregnancy and lactation 3–5 mg
Dietary Sources Of Iron
Liver, egg yolk, meat, fish, chicken, spinach, dry fruits, wheat, and apple.
Absorption:
- 10% of iron is absorbed. Heme iron (iron in meat) is absorbed better and faster because it can be absorbed as such and does not need to be dissociated into elemental iron.
- Iron in vegetables and grains is inorganic iron and is relatively poorly absorbed because it is tightly bound to organic compounds.
- It is mostly absorbed from the upper gut in the ferrous form.
Factors that Influence Iron Absorption:
Ascorbic acid, amino acids, meat, gastric acidity → Increase absorptionAntacids, phosphates, phytates, tetracyclines → Decrease absorption
Adverse effects of oral iron:
- Epigastric pain, nausea, vomiting, gastritis, metallic taste, constipation (due to astringent effect), or diarrhea (irritant effect) are the usual adverse effects.
- Liquid preparations of iron cause staining of the teeth.
- Patient should be informed that there would be blackening of the stools.
Parenteral Iron
Question 1. Short note on parenteral iron therapy/preparations.
Answer:
Iron can be administered parenterally as a deep IM injection or intravenously. Iron is given parenterally only in the following condition:
Indications:
- When oral iron is not tolerated.
- Failure of absorption—as in malabsorption, chronic bowel disease.
- Noncompliance.
- Severe deficiency with bleeding.
- Patients who have undergone gastrectomy.
- Patients receiving erythropoietin—oral iron absorption may not be enough.
Parenteral iron preparations:
IM injection of iron is given deep into the gluteal region using the ‘Z’ technique to avoid staining of the skin. IV iron is given slowly over 5–10 minutes or as an infusion after a test dose.
1. Iron dextran complex: A complex of ferric iron and dextran has 50 mg elemental iron/mL.
- It is the only preparation that can be given intravenously and also deep IM.
- Hypersensitivity reactions can be serious but uncommon. The incidence of allergy is more in patients who were previously exposed to iron dextran and have a history of other allergies.
- A 0.5 mL test dose of iron dextran complex is injected IV slowly over 5–10 minutes.
- If no obvious allergic response is observed, 2 mL of the IV preparation diluted in 500 mL glucose may be injected over 10 minutes every day.
- Patients should be constantly monitored for signs of allergy.
2. Iron-sorbitol-citric acid complex: Contains 50 mg elemental iron/mL; it is given only by
IM. This preparation should not be given IV because it quickly saturates the transferrin stores. As a result, free iron levels in the plasma rise and can cause toxicity.
![]()
3. Iron sucrose and sodium ferric gluconate: Given only by IV route. Allergy is lower than with iron dextran.
4. Ferric carboxymaltose and ferumoxytol:
- Ferric carboxymaltose contains iron embedded in a carbohydrate polymer.
- Ferumoxytol is an aqueous preparation containing superparamagnetic iron oxide nanoparticle which is coated with a carbohydrate.
Parenteral Iron Disadvantage:
- Ferumoxytol interferes with MRI for 3 months after the last dose and the patients should be educated to inform the radiologist if any MRI is required.
- The serum concentration of ferritin and transferrin should be monitored to avoid iron overload.
The dose is calculated using a formula:
- Iron requirement (mg) = 4.4 × body weight (kg) × Hb deficit (g/dL)
- This also includes the iron needed for the replenishment of stores.
Parenteral Iron Adverse Effects:
- Local: Pain at the site of injection, pigmentation of the skin, and sterile abscess.
- Systemic: Fever, headache, joint pain, palpitation, difficulty in breathing, urticaria, flushing, lightheadedness, nausea, vomiting, lymph node enlargement, and rarely, anaphylaxis. Deaths
have been reported due to bronchospasm.
Acute Iron Poisoning:
- More common in infants and children → about 10 tablets (1–2 g) can be lethal.
- Manifestations of vomiting, abdominal pain, hematemesis, bloody diarrhea, shock, drowsiness, cyanosis, acidosis, dehydration, cardiovascular collapse, and coma. Immediate diagnosis and treatment are important as death may occur in 6–12 hours.
Iron Treatment:
- Gastric lavage with sodium bicarbonate solution.
- Antidote-Desferrioxamine is instilled into the stomach after lavage, to prevent iron absorption; also injected IV/IM.
- Correction of acidosis and shock.
Iron Uses:
- Iron deficiency anemia is both for prophylaxis and treatment. The cause of iron deficiency should be identified.
- Treatment should be continued depending on the response for 3–6 months to replenish iron stores.
- Prophylactically, iron is given in conditions with increased iron requirement as in pregnancy, infancy, and professional blood donors.
Vitamin B12 and Folic Acid
- Vitamin B12 and folic acid are water-soluble vitamins, essential for normal DNA synthesis.
- Deficiency results in megaloblastic anemia characterized by the presence of red cell precursors in the blood and bone marrow.
- Vitamin BVitamin B12 and folic acid and folic acid are, therefore, called maturation factors.
- Other manifestations of deficiency include glossitis, stomatitis and malabsorption. Neurological manifestations can also be seen.

1. Vitamin B12:
- Vitamin B12 (cyanocobalamin) is synthesized by microorganisms. Liver, fish, egg yolk, meat, cheese, and pulses are the dietary sources of B12.
- Vitamin B12 or extrinsic factor is absorbed with the help of intrinsic factor, a protein secreted by the stomach.
- It is carried in the plasma by B12 -binding proteins called transcobalamin and is stored in the liver.
Deficiency: Vitamin B12 deficiency may be due to:
- Addisonian pernicious anemia:

- Other causes: Gastrectomy, chronic gastritis, malabsorption, and fish tapeworm infestation (fish tapeworm consumes B12).
Signs and symptoms of deficiency:
Abnormal maturation of RBCs and defective DNA synthesis result in megaloblastic anemia with hypercellular marrow, weakness, lethargy, palpitations, angina, vertigo, and neurological manifestations with paraesthesias of hands and feet, and in more severe cases spasticity, ataxia, loss of memory, confusion, delusions, hallucinations and psychosis can occur.
Vitamin B12 Preparations:
- Cyanocobalamin: 100 mg inj. IM/deep SC—hypersensitivity reactions can occur.
- Hydroxocobalamin injection: 500, and 1000 mg injections are preferred as it has a longer-lasting effect because of their high protein binding but hydroxocobalamin administration can result in the formation of antibodies.
- Sublingual vitamin B12 preparation is claimed to have good bioavailability.
- Multivitamin preparations contain variable amounts of vitamin B12.
Vitamin B12 Uses:
1. Megaloblastic anemia due to vitamin B12 deficiency:
- Pernicious anemia IM/SC Vit B12 → IF deficiency → no oral B12 absorption
- Lifelong treatment Vit B12 induced brisk hemopoiesis → ↑ Iron and folic acid demand → add 5 mg folic acid and iron
- Prophylaxis of B12 deficiency: Prophylactic dose of vitamin B12 is 3–10 mg daily.
2. Neuropathies:
- Neuropathies are thought to be due to B12 deficiency like tropical neuropathy response to vitamin B12.
- Vitamin B12 is also given in many other conditions like trigeminal neuralgia, multiple sclerosis, some psychiatric disorders, and even general weakness.
- There is no evidence to recommend such use for vitamin B12.
2. Folic Acid:
Folic acid or pteroylglutamic acid was first isolated from spinach and named as folic acid (from leaf).
- Dietary sources: Green vegetables, liver, yeast, egg, milk, and some fruits. Prolonged cooking with spices destroys folic acid.
- Absorption: Takes place in the duodenum and jejunum is widely distributed in the body and stored in the liver.
Folic Acid Functions:
Folic acid is converted to dihydrofolic acid and then to tetrahydrofolic acid which serves as a coenzyme for many vital (one-carbon transfer) reactions necessary for DNA synthesis.
Folic Acid Deficiency:
- May be due to dietary folate deficiency, malabsorption, and other diseases of the small intestine or drug-induced.
- Phenytoin, phenobarbitone, oral contraceptives, methotrexate, and trimethoprim can induce folate deficiency.
- Increased requirements in children, pregnancy, and lactation can also cause deficiency.
- Manifestations include megaloblastic anemia, glossitis, diarrhea, and weakness.
Folic Acid Uses:
- Megaloblastic anemia due to folate or B12 deficiency folic acid 2–5 mg/day orally along with vitamin B12. In malabsorption syndromes, folic acid is given IM.
- Prophylactically in pregnancy, lactation, infancy, and other situations with increased requirement of folic acid 500 mg daily orally.
- Folinic acid (citrovorum factor, leucovorin) is N-formyl tetrahydrofolic acid and is the active coenzyme form that is utilized by the cells in place of THF and overcomes methotrexate
toxicity.
Hematopoietic Growth Factors
Hematopoietic growth factors regulate erythropoiesis and have been produced for clinical use by recombinant DNA technology. Frequent blood counts are needed to monitor therapy with these growth factors.
- Erythropoietin
- Myeloid growth factors:
- GM-CSF
- G-CSF
- M-CSF
- Megakaryocyte growth factors:
- Thrombopoietin
- Interleukin 2
Hematopoietic Erythropoietin:
It is produced by the kidney in response to hypoxia and anemia. It binds to erythropoietin receptors on red cell progenitors and stimulates red cell production.
Epoetin alpha:
- Epoetin alpha is human recombinant erythropoietin.
- It is given thrice weekly to treat anemia in chronic renal failure and is not cleared by dialysis.
Darbepoetin alpha:
- Darbepoetin alpha is modified EPO with a longer half-life—given once a week.
- Epoetin beta attached to polyethylene glycol is much longeracting to be given once in 2–4 weeks.
Hematopoietic Adverse effects:
- They can cause allergic reactions hypertension, hypertensive encephalopathy, headache, tachycardia, arthralgias, and myalgia.
- The rapid rise in hematocrit → Thrombotic complications (MI, stroke) → ↑ ↑ Mortality (monitor Hb)
Hematopoietic Uses:
- Anemia due to the following conditions:
- Chronic renal failure
- Zidovudine treatment in AIDS patients
- Cancer chemotherapy
- Aplastic anemia
- Multiple myeloma and cancers of bone marrow
- Treatment of iron overload.
- Anemia of prematurity.
Myeloid Growth Factors:
- Granulocyte–macrophage colony-stimulating factor (G-CSF) and monocyte colony-stimulating factor (M-CSF).
- Sargramostim and molgramostim are recombinant human granulocyte–macrophage colony-stimulating factors (GM-CSF) that stimulate the proliferation and differentiation of neutrophils and monocytes.
Myeloid Adverse effects:
Including bone pain, fever, arthralgia, myalgia, dyspnea, and heart failure.
Filgrastim
Human recombinant G-CSF → stimulates the production of neutrophils.
Filgrastim Adverse effects: Filgrastim is better tolerated and can cause bone pain and rarely allergic reactions.
Filgrastim Uses:
Sargramostim and filgrastim are used to shorten neutropenia in bone marrow transplantation, following cancer chemotherapy, aplastic anemia, congenital neutropenia, myelodysplasia, and in AIDS patients with neutropenia.
Megakaryocyte Growth factors:
- Thrombopoietin increases the production of platelets by binding to the receptors on the platelet progenitor cells.
- Recombinant thrombopoietin is tried in severe thrombocytopenia following cancer chemotherapy.
Anticoagulants
Hemostasis is the spontaneous arrest of bleeding from damaged blood vessels. In the process, complex interactions take place between the injured vessel wall, platelets, and clotting factors

Anticoagulants are drugs that reduce the coagulability of the blood. They are classified as:
Anticoagulants Classification:

Indirect Thrombin Inhibitors
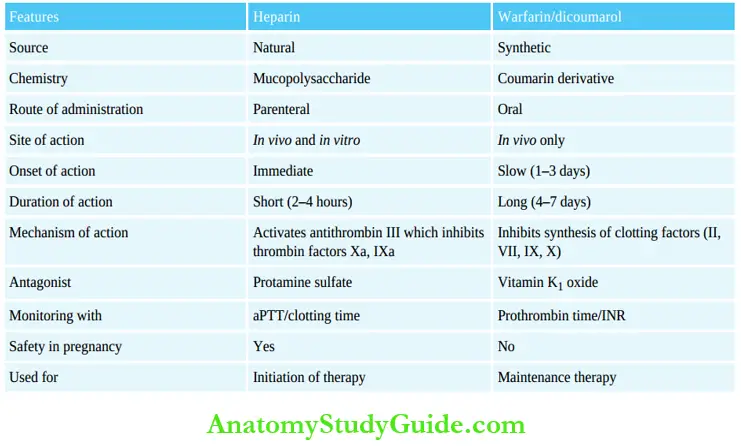
Heparin: Heparin (discovered by McLean, a medical student) is a mucopolysaccharide found in the mast cells of the liver, lungs, and intestinal mucosa.
- Heparin is the strongest acid in the body.
- It is a glycosaminoglycan.
Actions: Heparin is a powerful anticoagulant that acts immediately both in vivo and in vitro.
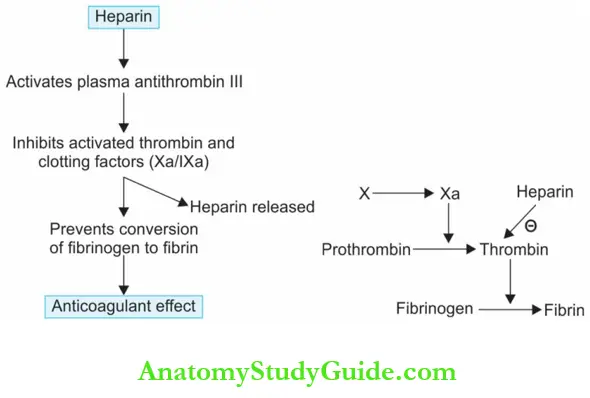
Thrombin Inhibitors Mechanism of action:
- Heparin activates plasma antithrombin III which inhibits the activated thrombin and coagulation factors (Xa and IXa).
- This is a physiological reaction, but heparin accelerates it by 1,000 times. Clotting time is prolonged.
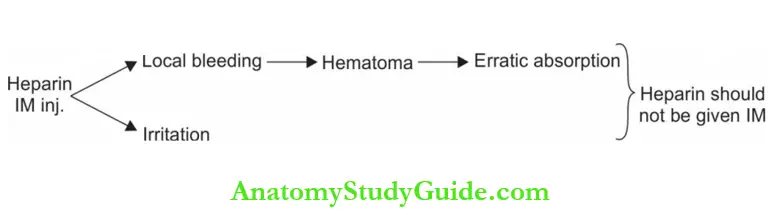
Question 2. Explain why heparin should not be given IM.
Answer:
IM Pharmacokinetics:
Heparin is not effective orally—given IV or SC. It should not be given IM.
- Given intravenously the onset of action is immediate, reaches peak in 5–10 minutes, and clotting time returns to normal in 2–4 hours.
- Treatment is monitored by the activated partial
thromboplastin time (aPTT) (preferable) or clotting time. - Heparin is metabolized by heparinase in the liver.
Because of its large molecular size, heparin does not cross the placental barrier. Therefore, heparin can be used in pregnancy, if an anticoagulant is needed.
Heparin administration:
- 5,000 units bolus dose followed by 800–1,000 units per hour IV infusion.
- For prophylaxis, subcutaneous low-dose heparin is given—5,000 U 2–3 times a day.
IM Adverse Reactions:
Bleeding:
Bleeding is the most common, major adverse effect of heparin. Careful monitoring and dose control will prevent this to a great extent.
Hypersensitivity reactions:
Because of its animal origin, (bovine lung or porcine intestine), allergic reactions are common.
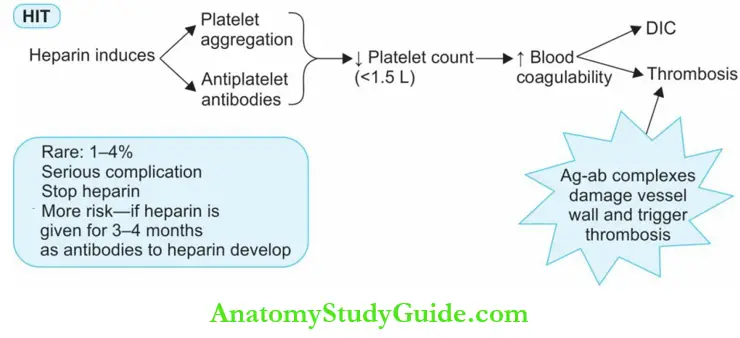
3. Heparin-induced thrombocytopenia (HIT):
- Heparin-induced platelet aggregation and the formation of antiplatelet antibodies—both result in thrombocytopenia and a state of hypercoagulability.
- Though both venous- and arterial thrombosis can occur, venous thrombosis is common. The incidence is higher in surgical patients.
- The confirmatory test is by heparin-independent platelet activation assay.
- This paradoxical complication is seen with standard heparin given at least a week but can be serious, (less common with LMW heparins).
4. Alopecia: Alopecia is reversible seen in 0.5% of patients after about 5–10 days of starting heparin.
5. Osteoporosis: Osteoporosis can occur on long-term use of heparin—cause unknown.
6. Hypoaldosteronism: Heparin can inhibit the synthesis of aldosterone and may result in hyperkalemia.
Question 3. What are the advantages of LMW heparins? Write a short note on LMW heparin.
Answer:
Low molecular weight (LMW) heparins:
- Include enoxaparin, dalteparin, reviparin, nadroparin, etc. obtained by chemical/enzymatic treatment of standard or unfractionated heparin (UFH).
- They are equally effective and have a favorable pharmacokinetic profile. They have a shorter chain and lower molecular weights when compared to UFH.
- Since LMW heparins inhibit factor Xa only and have just a weak effect on thrombin, aPTT or clotting time are not prolonged.
- Plasma LMW levels can be determined by assay of anti-Xa units and therapeutic levels should be maintained.
- LMW heparins should be used carefully in patients with renal dysfunction → Anti-Xa assay is used to monitor the dose.
LMW heparins have the following advantages over standard heparins:
- Better bioavailability following SC injection.
- Longer action—once or twice daily dose.
- Predictable pharmacokinetics and plasma levels—frequent aPTT monitoring not required.
- Lower risk of bleeding.
- Lower risk of osteoporosis.
- Lower incidence of thrombocytopenia and thrombosis.
LMW heparins Use:
- Prevention and treatment of venous thrombosis and pulmonary embolism.
- Standard Heparin and LMW Heparin
- In unstable angina.
- To maintain the patency of tubes in dialysis patients.
Heparin antagonist: Mild heparin overdosage can be treated by just stopping heparin because heparin is short-acting.
Standard Heparin And LmH Heparin:

In severe heparin overdose, an antagonist may be needed. Protamine sulfate a protein obtained from the sperm of certain fish is given IV to neutralise heparin (1 mg for every 100 units of heparin). A whole blood transfusion may be needed.
![]()
Synthetic heparins:
- Fondaparinux a factor Xa inhibitor, is a synthetic compound, that binds to antithrombin and mediates the inhibition of factor Xa. Given by SC inj.
- 2.5 mg once daily, has a rapid onset of action, the response is predictable, t½ 17–21 hours, and is excreted in the urine.
- It does not require frequent coagulation monitoring. The risk of HIT is lower than with even LMW heparins. However, it should not be given to patients with renal dysfunction.
Synthetic heparins Uses:
- Prevention and treatment of deep vein thrombosis and pulmonary embolism
- For thromboprophylaxis in patients undergoing hip or knee surgery.
Idraparinux:
Idraparinux a longer-acting derivative of fondaparinux, has a t½ of 5–6 days.
Heparinoids:
- Danaparoid is a mixture of heparinoids and acts by inhibiting factor Xa. It does not prolong aPTT and is longer acting.
- Used subcutaneously in deep vein thrombosis and as an alternative to heparin.
Direct Thrombin Inhibitors
Parenteral Direct Thrombin Inhibitors (Dtis):
Hirudin: Hirudin present in the saliva of leeches has been synthesized by recombinant DNA technology for clinical use. Lepirudin and bivalirudin are hirudin analogs. They:
- Irreversibly bind thrombin on both the fibrin binding site and the catalytic site and inhibit its activity.
- They can inactivate fibrin-bound thrombin in the clots.
- The action is monitored by aPTT; there is no specific antidote, unlike heparin.
- Lepirudin is excreted by the kidneys → use carefully in renal impairment. Bivalirudin is only 20% excreted through the kidneys → safer.
- Antibodies develop to lepirudin and on re-exposure, the risk of anaphylaxis exists.
- Lepirudin can be used in patients with heparin-induced thrombocytopenia. Bivalirudin may be used in patients undergoing coronary angioplasty.
- Argatroban, a direct thrombin inhibitor, binds thrombin and has a quick but short action.
- Given as an IV infusion, it may be used in HIT and treatment monitored with aPTT.
Oral Anticoagulants
Cattle that were fed on spoiled sweet clover hay, developed a hemorrhagic disease in North America. This was found to be due to bis hydroxy coumarin, an anticoagulant in the spoiled sweet clover.
Oral Anticoagulants Mechanism Of Action:
- Warfarin and its congeners are anticoagulants only in vivo because they act by interfering with the synthesis of vitamin K-dependent clotting factors in the liver.
- They block the gamma-carboxylation of glutamate residues in factors II, VII, IX, and X. Gamma-carboxylation is necessary for these factors to participate in coagulation.
- The onset of action is slow; it develops over 1–3 days because oral anticoagulants do notdestroy the already circulating clotting factors.
- Prothrombin time (PT) is measured to monitor the treatment. It takes 5–7 days for PT to return to normal after stopping oral anticoagulants.

Oral Anticoagulants Pharmacokinetics:
- Warfarin is completely absorbed orally and is 99% bound to plasma proteins.
- It is metabolized by microsomal enzymes CYP2C9. People inheriting a genetic variant of Heparin and Warfarin/dicoumarol
- Bishydroxycoumarin (dicumarol) and nicoumalone are poorly tolerated because of gastrointestinal (GI) disturbances. Diphenadione is used as a rodenticide.
Oral Anticoagulants Adverse Effects:
1. Hemorrhage: Hemorrhage is the main side effect. Bleeding in the intestines or brain can be troublesome. Minor episodes of epistaxis and bleeding gums are common. Treatment depends on the severity.
- Stop the anticoagulant.
- Fresh blood transfusion is given to supply clotting factors.
- Antidote: The specific antidote is vitamin K1 oxide. It promotes the synthesis of clotting factors but even on IV administration, the response to vitamin K1 oxide needs several
hours. Hence in an emergency, fresh whole blood is necessary to counter the effects of oral anticoagulants
Heparin and Warfarin / Dicoumarol:
2. Other Adverse Effects: Allergic reactions, GI disturbances, and teratogenicity
Orally Acting Dtis
Dabigatran is a newly developed orally effective direct thrombin inhibitor.
Advantages of Dabigatran (Oral DTIs) Over Warfarin:
- Rapid onset of action.
- Predictable absorption and plasma levels.
- Frequent monitoring of anticoagulant therapy is not essential.
- Lower risk of bleeding.
- Fewer drug interactions.
Idaricizumab:
- Idaricizumab an antidote to dabigatran (recently developed) binds to dabigatran with high affinity and completely reverses the actions of dabigatran in 5 minutes.
- Because of the above advantages, dabigatran may soon replace warfarin for long-term anticoagulation therapy.
- In patients with renal impairment, dose should be reduced. Adverse effects include GI disturbances and bleeding. PTT and thrombin time will be prolonged. It is given once daily.
Idaricizumab Uses:
Dabigatran is approved for the prevention of venous thromboembolism in patients who have undergone surgeries for hip or knee replacement.
Factor XA Inhibitors
Rivaroxaban and apixaban:
- Rivaroxaban and apixaban are orally effective direct inhibitors of factor XA. Rivaroxaban has fast onset of action and apixaban is gradually absorbed and has a long t½.
- Both are metabolized by CYP450 enzymes.
- Rivaroxaban is approved for the prevention and treatment of deep vein thrombosis and the prevention of venous thrombosis in hip and knee surgery.
- Apixaban is approved for the prevention of stroke in atrial fibrillation (without valvular heart disease).
- Edoxaban is studied for use in deep vein thrombosis and pulmonary embolism.
Drug interactions of oral anticoagulants:
Some drugs potentiate warfarin action—
1. NSAIDs + warfarin/other anticoagulant (antiplatelet effect) → ↑ bleeding

Some drugs reduce the effect of oral anticoagulants (OAC)
3. Microsomal enzyme inducer → ↑ metabolism of OAC → ↑ OAC levels (phenytoin, rifampin, alcohol)
Sudden withdrawal of inducer drug → ↑ OAC levels → toxicity
4. Hormonal contraceptives → ↑ clotting factor synthesis → ↓ OAC effect
Uses of anticoagulants:
Anticoagulants can prevent the extension of thrombus but cannot destroy the existing clots.
Heparin has rapid- and short action which makes it suitable for initiating or starting treatment, while warfarin is suitable for long-term maintenance due to.
Its slow and prolonged action and convenience of oral use:
- Venous thrombosis and pulmonary embolism: Anticoagulants prevent extension of thrombus and recurrence of embolism.
- Postoperative, poststroke patients: Bedridden patients due to leg fractures—who cannot be ambulant for several months anticoagulants prevent venous thrombosis and
pulmonary embolism in such patients. - Rheumatic valvular: Rheumatic valvular disease anticoagulants prevent embolism.
- Unstable angina: Unstable angina heparin reduces the risk of MI in patients with unstable angina.
- Vascular surgery, artificial heart valves, and hemodialysis—anticoagulants prevent thromboembolism.
Contraindications to Anticoagulant Therapy:
- Bleeding disorders including thrombocytopenia
- Bacterial endocarditis
- Severe hypertension
- Liver and kidney diseases.
- Malignancies
Thrombolytics (fibrinolytics)
Question 4. Write a short note on thrombolytics/fibrinolytics.
Answer:
Thrombolytics lyse the clot or thrombi by activating the natural fibrinolytic system. Plasminogen circulates in the plasma and also some of it is bound to fibrin. Tissue plasminogen activator (tPA) activates plasminogen which is converted to plasmin. Plasmin degrades fibrin—thereby dissolving the clot.

Thrombolytics include:
- First-generation agents—streptokinase, urokinase
- Second generation agents—alteplase, duteplase, tenecteplase, reteplase, anistreplase
Streptokinase:
- Streptokinase obtained from β-hemolytic streptococci activates plasminogen. Antistreptococcalantibodies present in the blood due to previous streptococcal infections inactivate a large amount of streptokinase.
- Streptokinase is antigenic and can cause allergy.
- The antibodies formed may persist for 5 years. Hence, if thrombolytics are required during that period, others like tPA or urokinase should be used. Streptokinase also causes hypotension.
Anistreplase:
- Anistreplase [anisoylated plasminogen streptokinase activator complex, (APSAC)] is a form of streptokinase that is long-acting and can be injected in a single IV bolus of 30 units over 3–5 minutes. Hence it is more convenient to use.
- Has greater activity for clot than for free plasminogen, but it also causes fibrinogenolysis and allergic reactions.
Urokinase:
Urokinase is an enzyme prepared from cultures of human kidney cells (first isolated from human urine—hence the name).
Tissue plasminogen activator:
- Tissue plasminogen activator preferentially activates plasminogen that is bound to fibrin which means circulating plasminogen is largely spared.
- Chances of occlusion may be reduced by the use of heparin and antiplatelet drugs.
Alteplase, duteplase and tenecteplase: Alteplase, duteplase and tenecteplase are tPA produced by recombinant DNA technology.
Reteplase: Reteplase is a modified human tPA obtained by genetic engineering.
Advantages of tPA:
- Faster reperfusion
- Negligible bleeding tendency.
Thrombolytics Adverse Effects:
- Bleeding is the major toxicity of all thrombolytics.
- Hypotension and fever can occur.
- Allergic reactions are common with streptokinase.
Thrombolytics Uses:
- Acute myocardial infarction: IV thrombolytics to be given immediately—because early treatment largely reduces mortality.
- Severe deep vein thrombosis and large pulmonary emboli, ascending thrombophlebitis.
- Peripheral vascular diseases—intra-arterial thrombolytics have been tried.
Contraindications to Thrombolytic Therapy:
- Recent surgery, injury, gastrointestinal bleeding, stroke.
- Severe hypertension.
- Bleeding disorders.
Antifibrinolytics
Question 5. Write a short note on antifibrinolytics.
Answer:
Antifibrinolytics are drugs that inhibit fibrinolysis they block the binding of plasminogen to fibrin and inhibit the dissolution of clots.
Epsilon aminocaproic acid (EACA):
- It is an analog of the amino acid lysine that interacts with the lysine binding sites on plasminogen and plasmin and blocks them.
- Thus plasminogen activation at higher doses proteolytic activity of the plasmin are inhibited and the clot is stabilized.
- Given orally it is rapidly absorbed.
Antifibrinolytics Adverse effects:
- Including nausea, abdominal discomfort, dyspepsia, conjunctival erythema, giddiness, skin rashes, and rarely intravascular thrombosis.
- If injected rapidly intravenously, it can cause hypotension and bradycardia.

Dose: 100 mg/kg loading dose (max 10 g) followed by 50 mg/kg (max 5 g) 6 hourly for 2–3
days.
Tranexamic acid (TA):
TA is more potent and longer-acting than EACA. TA is given by oral, topical, and by IV routes. Dose: 1–1.5 g 6–8 hourly 500 mg tab.
Antifibrinolytics Uses:
To arrest bleeding in hyperplasminemic states which result from damage to tissues that are rich in plasminogen activators as in the following conditions:
- Antidote in overdosage of fibrinolytic
- Menorrhagia, postpartum hemorrhage
- After cardiac surgeries including cardiopulmonary bypass
- Bleeding peptic ulcer
- Following dental procedures to prevent bleeding in patients with hemophilia as a mouthwash
- After prostate surgery, tonsillectomy
- Epistaxis, bleeding from eye injury
- Hereditary angioedema—in this rare condition, plasmin-induced uncontrolled activation of the complement system takes place.
Aprotinin:
Aprotinin is a naturally occurring protease inhibitor—it inhibits kallikrein, plasmin, trypsin, and chymotrypsin. It also protects platelets from mechanical injury—thus aprotinin inhibits the
initiation of clot formation and fibrinolysis. Aprotinin is used intravenously but can also be used topically.
Aprotinin Uses:
- Cardiac surgeries like cardiopulmonary bypass surgery and heart valve replacement to reduce blood loss.
- Fibrinolytic overdosage.
Aprotinin Adverse effects:
- Aprotinin is obtained from bovine lungs and can, therefore, cause allergic reactions.
- It can also cause thrombosis and renal toxicity.
Contraindications for Antifibrinolytics:
- Hematuria—the risk of ureteric obstruction, colic due to the unlysed clot (called clot colic)
- Intravascular coagulation.
Antiplatelet Drugs
Platelets form the initial hemostatic plug at the site of vascular injury and are also involved in the formation of atherosclerosis. By inhibiting platelet function, thrombosis and atherosclerotic vascular disease can be largely prevented.
Antiplatelet Drugs Classification:


Aspirin:
- The prostaglandin thromboxane A2 promotes platelet aggregation. Aspirin inactivates the cyclooxygenase enzyme (COX) and thereby inhibits the synthesis of thromboxane A2 even in low doses (75 mg/day). Reason for using low-dose aspirin.
- The COX inhibition is irreversible and the effect lasts for 7–10 days—till fresh platelets are formed.
- Aspirin inhibits the synthesis of both TXA2 which promotes platelet aggregation and PGI2 which inhibits it. However, in low doses, it inhibits only TXA2 production without a significant effect on PGI2 production.
- Hence aspirin is used in low doses for thromboprophylaxis.
- Low doses also reduce the risk of gastrointestinal adverse effects of aspirin.
- Aspirin and other antiplatelet drugs effectively reduce the incidence of stroke and MI in susceptible individuals.
- Dose: 50–300 mg/day.
Aspirin resistance:
When thrombosis occurs in spite of aspirin prophylaxis, it can be considered as aspirin resistance. The incidence of resistance is about 30%. The cause for it is not exactly known.
Dipyridamole:
- Dipyridamole is a phosphodiesterase inhibitor that interferes with platelet function by increasing platelet cyclic-AMP levels.
- It is used along with aspirin or warfarin for the prophylaxis of thromboembolism in patients with prosthetic heart valves and in patients with transient ischemic attacks or stroke → the effects are additive with aspirin.
- It does not increase the risk of bleeding. Headache has been reported.
- Dose: 25–100 mg TDS.
Adp Antagonists:
- ADP binds to the receptors on platelets to bring about platelet aggregation. Clopidogrel, prasugrel, ticlopidine, cangrelor and ticagrelor are ADP antagonists. ‘
- They are all prodrugs and the active metabolites bind to and irreversibly block the ADP receptors (P2Y12) and thereby prevent activation of platelets thus inhibiting platelet aggregation.
- The effects are additive with aspirin because the mechanisms of action are different but the combination is more expensive.
- Though the onset of action is slow (3–7 days), an oral loading dose of 300 mg clopidogrel can attain antithrombotic effects within about 5 hours. The antiplatelet effects remain for 7–10 days after stopping the drug.
Adp Antagonists Adverse effects:
- Clopidogrel is preferred to ticlopidine because it is—safer and better tolerated.
- They can cause rash, diarrhea, epigastric pain, neutropenia and rarely bleeding.
Adp Antagonists Uses:
- For preventing MI and stroke in patients with angina and transient ischemic attacks.
- For thromboprophylaxis in coronary angioplasty.
- Acute coronary syndrome.
Compared to clopidogrel, prasugrel has a more rapid onset of action and more efficient platelet inhibition but has the risk of bleeding. Cangrelor and ticagrelor are approved for use in acute coronary syndrome.
Glycoprotein 2B/3A Receptor Antagonists:
- Fibrinogen, vitronectin, fibronectin, and von Willebrand factor bind to glycoprotein IIb/IIIa receptor complex on the platelets and mediate platelet aggregation by platelet agonists like thrombin, collagen, and TXA2.
- Thus their receptor complex acts as the final common pathway for platelet aggregation.
- Abciximab (monoclonal antibody), eptifibatide, and tirofiban block these receptors and inhibit platelet aggregation.
- They can cause bleeding and rarely—allergic reactions during coronary angioplasty and in acute coronary syndromes.
Glycoprotein Others:
- Epoprostenol (PGI2) can be used during hemodialysis to prevent platelet aggregation and platelet loss, as an alternative to heparin when heparin is contraindicated. The other indications are severe pulmonary hypertension and circulatory shock since PGI2 is also a potent vasodilator.
- Cilostazol is a phosphodiesterase III inhibitor with vasodilator and antiplatelet aggregatory properties. It is used in intermittent claudication as it increases pain-free walking distance.
- Ridogrel: Has dual actions of blocking thromboxane A2 receptor and also inhibiting the synthesis of TXA2.
Uses Of Antiplatelet Drugs
Cardiac Conditions:
- Ischemic heart disease: Thromboprophylaxis prevents the formation of clot and thereby prevent MI.
- Myocardial infarction: 300 mg aspirin is given immediately after diagnosis of MI to reduce the risk of reinfarction, improve survival and reduce mortality. Clopidogrel or abciximab may be added. In post-MI patients, long-term low-dose aspirin (75–150 mg daily) is continued to prevent reinfarction.
- Unstable angina: Aspirin 150 mg daily reduces the risk of acute MI.
- Stable angina pectoris: All patients with IHD including angina need prophylaxis with 75–150 mg aspirin daily to prevent MI.
- Cardiac procedures: Following coronary artery angioplasty, stenting, and coronary bypass grafting, aspirin with or without clopidogrel or abciximab reduces the risk of occlusion.
- Atrial fibrillation: If oral anticoagulants cannot be used, antiplatelet drugs may be given.
- Prosthetic heart valves: Formation of microthrombi on the artificial heart valves is an expected risk—emboli can also develop. In order to prevent these complications, aspirin given may be combined with warfarin.
Noncardiac Conditions:
- Hemodialysis: Epoprostenol (PGI2) is injected into the blood entering the dialysis unit in order to prevent platelet aggregation and thereby thrombus formation during hemodialysis and in hemofiltration.
- Pulmonary hypertension: Epoprostenol is used in both primary- and secondary pulmonary hypertension.
- Vascular grafts: To prevent occlusion and maintain patency of the vascular grafts.
- Cerebrovascular disease: Transient cerebral ischemic attacks called ‘ministrokes’ require thromboprophylaxis to reduce the incidence of stroke. In cerebral thrombosis patients, long-term use of antiplatelet drugs prevents recurrence. Aspirin may be combined with dipyridamole for a synergistic effect. Clopidogrel is also effective.
- Peripheral vascular disease: For thromboprophylaxis in intermittent claudication.

Coagulants
Coagulants are drugs that promote coagulation (procoagulants) and control bleeding. They are also called hemostatics. They may be used locally or systemically. Physical methods like the application of pressure, tourniquet, or ice can control bleeding.
Styptics: Styptics are local hemostatics that are used on bleeding sites like tooth sockets and wounds.
They are:

- Adrenaline: Sterile cotton soaked in a 1:10,000 solution of adrenaline is commonly used in tooth sockets and as nasal packs for epistaxis. Adrenaline arrests bleeding by vasoconstriction but is not a true procoagulant.
- Thrombin powder: Thrombin powder is dusted over the bleeding surface following skin grafting.
- Fibrin: Fibrin obtained from human plasma is available as sheets for covering or packing bleeding surfaces.
- Gelatin foam: Gelatin foam is porous spongy gelatine used with thrombin to control bleeding from wounds. It gets completely absorbed in 4–6 weeks and can be left in place after suturing of the wound.
- Thromboplastin: Thromboplastin powder is used in surgery as a styptic.
- Astringents: Astringents like tannic acid, are used on bleeding gums.
Coagulants Used Systemically:
Vitamin K is a fat-soluble vitamin essential for the biosynthesis of clotting factors. They are:
- Vitamin K1 Present in food from plant source
- Vitamin K2 Produced in the gut by bacteria
- Vitamin K3 A synthetic compound used therapeutically.
Actions: Vitamin K is essential for the biosynthesis of clotting factors prothrombin and factors VII, IX, and X by the liver. Deficiency results in bleeding tendencies.
Adverse reactions are seen on parenteral administration allergic reactions and jaundice.
Coagulants Uses:
- Vitamin K deficiency may result from various causes. Dietary deficiency is uncommon.
- Prolonged use of antibacterials destroys the intestinal flora leading to vitamin K deficiency.
- Malabsorption syndrome, prolonged parenteral nutrition, obstructive jaundice, and liver disease all result in vitamin K deficiency and require adequate vitamin K supplementation
- 5–10 mg/day orally or parenterally till the deficiency is corrected.
- Newborn babies lack intestinal flora and have low levels of prothrombin and other clotting factors. Routine administration of vitamin K (1 mg IM) prevents hemorrhagic disease of the newborn.
- Oral anticoagulant toxicity antidote.
Other Coagulants:
1. Fresh plasma:
- Fresh plasma or whole blood is useful in most coagulation disorders as they contain all the clotting factors.
- Other concentrated plasma fractions like fibrinogen, factors II, VII, VIII, IX, and X are available for the treatment of specific deficiencies.
2. Fibrinogen: Fibrinogen obtained from pooled human plasma is used to control bleeding in hemophilia, antihemophilic globulin (AHG) deficiency, and acute afibrinogenemic states.
3. Antihemophilic: Antihemophilic factor is used in hemophiliacs and in AHG deficiency to control bleeding episodes.
4. Desmopressin: Desmopressin An analog of vasopressin increases factor VIII and von Willebrand factor levels by 3–5 folds in patients with mild hemophilia A and in von
- Willebrand’s disease. It normalizes the bleeding time in patients with congenital defects of platelet function and is also useful in bleeding secondary to other conditions like uremia and NSAID-induced bleeding.
- Adverse effects include flushing, headache, tachycardia, water retention, mild hypertension, and hyponatremia.
5. Ethamsylate:
- Ethamsylate reduces capillary bleeding by increasing capillary wall stability through an anti-hyaluronidase activity. It may correct abnormal platelet adhesion and promote platelet aggregation by inhibition of PGI2 synthesis.
- Ethamsylate is used to arrest or prevent bleeding in PPH, menorrhagia, epistaxis, after tooth extraction, and in similar indications as tranexamic acid.
- It does not stabilize fibrin and, therefore, has no antifibrinolytic activity.
6. Snake venom: Venom of some snakes like Russell’s viper venom stimulate thrombokinase and promotes coagulation.
Hypolipidemic Drugs
Elevated plasma levels of LDL cholesterol and low levels of HDL cholesterol increase the risk of coronary heart disease along with the other risk factors, viz. smoking, family history of coronary artery disease, male sex, metabolic syndrome, diabetes mellitus, and hypertension.
Hence hypercholesterolemia needs to be controlled. Hypolipidemic are drugs that lower plasma lipid levels in the body

Hypolipidemic Drugs Classification:
- HMG-CoA reductase inhibitors: Lovastatin, simvastatin, pravastatin, atorvastatin, rosuvastatin, fluvastatin, pitavastatin
- Fibrates: Gemfibrozil, clofibrate, fenofibrate, bezafibrate, ciprofibrate
- Bile acid binding resins: Cholestyramine, colestipol, colesevelam
- Miscellaneous: Ezetimibe, nicotinic acid, probucol, guggulipid, neomycin
- Newer drugs: CETP inhibitors, anacetrapib, anacetrapib, DGAT1 inhibitor, pradigastat

Hmg-Coa Reductase Inhibitors (Statins):
- Hydroxymethylglutaryl-CoA (HMG-CoA) is the rate-controlling enzyme in the biosynthesis of cholesterol.
- Lovastatin and other statins are structurally similar to HMG-CoA and are, therefore competitive inhibitors of the enzyme HMG-CoA reductase—‘reductase inhibitors‘.
- The synthesis of cholesterol in the liver is reduced. The concentration of HDL–cholesterol increases by about 10% .

Statins Pleiotropic effects: Statins can produce multiple beneficial effects in reducing the risk of CV diseases called pleiotropic effects of statins.

Statins Pharmacokinetics:
- Statins are well absorbed when given orally-food increases their absorption.
- Statins are metabolized by the enzyme cytochrome P450 and drug interactions are expected.
Statins Adverse effects: Gastrointestinal (GI) disturbances, headache, insomnia, rashes.
Hepatotoxicity:
- Hepatotoxicity is not common—serum transaminases may be elevated on prolonged therapy.
- Watch for hepatotoxicity particularly if also on other hepatotoxic drugs or are chronic alcoholics.
Myopathy:
- All statins can cause myopathy, myositis (with myalgia and weakness), and rarely rhabdomyolysis (<1%).
- Creatine phosphokinase (CPK) activity may be raised.
- In patients with an inherited genetic variation, statins can induce severe myopathy and rhabdomyolysis.
- Statins are contraindicated in pregnancy and lactation as they are not proven to be safe in them.
Statins Uses:
- First-line drugs in primary- and secondary hyperlipidemias.
- Coronary heart disease, stroke, transient ischemic attacks—to lower cholesterol levels.
Fibrates (Fibric Acids)
Gemfibrozil, fenofibrate, and bezafibrate increase the activity of the enzyme lipoprotein lipase which degrades VLDL resulting in the lowering of triglycerides.

Fibrates Adverse effects:
- Gastrointestinal upset, skin rashes, headache, myositis, muscle cramps, and blurred vision.
- Fibrates can cause rhabdomyolysis, particularly in patients with renal failure and when used with statins, the risk of myopathy gets added up.
- Fibrates should be avoided in patients with renal and hepatic dysfunction.
Fibrates Uses: Drug of choice in hypertriglyceridemia and in type 3, type 4, and type 5 hyperlipoproteinemias.
Bile Acid Binding Resins
- Cholestyramine and colestipol (bile acid sequestrants) are not absorbed → bind bile acids in the intestine and increase their excretion.
- These ion exchange resins are highly positively charged and, therefore, bind bile acids which are negatively charged. Bile acids are required for the intestinal absorption of cholesterol.
- Plasma cholesterol and LDL levels fall but this is also associated with an elevated triglyceride production.
- Hence bile acid sequestrants should be avoided in patients with increased TG levels. The resins are safe since they are not absorbed.

Bile Acid Binding Disadvantages:
- As powder is inconvenient to take
- Unpalatable
- ↑ TG levels
Colesevelam:
Colesevelam is a recently developed bile acid sequestrant with the following advantages:
- Not much increase in TG levels.
- Available as a tablet → convenient to take while other resins are taken as powders.
Colesevelam Uses: To lower LDL levels—BAB resins can be used along with statins.
Miscellaneous
Ezetimibe: Ezetimibe selectively inhibits the absorption of cholesterol from the intestines. The plasma LDL cholesterol decreases by 15–20% with a slight increase in HDL.
The effects are synergistic with statins:

Ezetimibe undergoes glucuronide conjugation, and enterohepatic circulation and is largely excreted through the gut. It is well-tolerated, and can occasionally cause reversible hepatic dysfunction and myositis.
Miscellaneous Uses:
- Monotherapy (10 mg OD) in mild hypercholesterolemia or in combination with a low dose of statins.
- It may also be used in phytosterolemia.
- However, it is not preferred now.
Nicotinic acid:
Nicotinic acid a B group vitamin, in large doses, inhibits triglyceride synthesis in the liver and VLDL production resulting in a decrease in LDL, and an increase in HDL-cholesterol.

- Niacin flush can be avoided by taking niacin after food or 300 mg aspirin taken 30 minutes before niacin.
- Tolerance develops to this effect in a few days. Other adverse effects are dyspepsia, dryness, and pigmentation of the skin.
Nicotinic acid Use: In hypertriglyceridemia with low HDL levels.
Gugulipid:
- Gugulipid obtained from ‘gum guggul’ lowers plasma cholesterol and triglycerides.
- It is well tolerated but can cause diarrhea.
Drug Interactions With Hypolipidemic
- Most statins are metabolized by the cytochrome P450 enzyme system.
- Statins + microsomal enzyme inhibitors → ↑ statin levels → toxicity (erythromycin, ketoconazole, metronidazole)
- Statins + microsomal enzyme inducers → ↓ statin levels → therapeutic failure (rifampicin, phenytoin)
- Statins + fibrates → ↑ toxicity to muscle
- Bile acid resins bind drugs like warfarin, digoxin, phenobarbitone, and chlorothiazide in the intestines → preventing their absorption. To avoid this, other drugs should be taken 1 hour before or 4 hours after the resins.
- Hypolipidemic + hepatotoxic drugs (like alcohol) → ↑ hepatotoxicity
- Fibrates + warfarin/anticoagulants → ↑ anticoagulant effect → ↓ anticoagulant dose
Diet In Dyslipidemia
- Total fat content in the food should be cut (~20–25% fat).
- Avoid alcohol—increases hepatic secretion of VLDL → hypertriglyceridemia.
Omega-3 fatty acids:
- Omega-3 fatty acids viz eicosapentaenoic acid and docosahexenoic acid reduce triglycerides by reducing VLDL and triglyceride synthesis in the liver. Fish oils are rich in omega-3 fatty acids.
- They activate peroxisome proliferator-activated receptor alpha (PPAR-α) leading to a reduction in triglycerides.
- However, LDL-CH levels could increase because of increased conversion of VLDL to LDL.
- The omega-3 fatty acids also have anti-inflammatory, antiplatelet aggregatory, and antiarrhythmic effects.
- Fish oil may be given as a supplement in—hypertriglyceridemia (in combination with fibrates) and in rheumatoid arthritis.
Treatment Of Dyslipidemia
Lipoproteinemia may be primary or secondary. All of them require lifestyle modification

Treatment of lipoproteinemia depends on the fraction raised and the severity of it. Drugs are not indicated only to raise HDL unless other components also need treatment.
When adequate control of dyslipidemia is not achieved with a single agent or when more than one lipid fraction needs to be corrected drugs from two different groups are generally combined

Drugs Used In The Treatment Of Obesity
- Obesity is a common problem in developed countries but is now also increasing in developing countries.
- It is largely due to a sedentary lifestyle and excessive or high-calorie food intake.
- Obesity is recognized as a risk factor for several diseases including cardiac diseases and is included as a factor in metabolic syndrome.
- Low-calorie diet and adequate physical activity are the primary measures.
- If these fail to control body weight, drugs may be used but only for a short period as none of them is safe for long-term use.
Drugs In Obesity:
- Orlistat
- Rimonabant
- Metformin
- Dietary fiber
Drugs In Obesity Orlistat:
- Orlistat acts by irreversibly inhibiting the enzymes gastric and pancreatic lipases because of which it prevents the breakdown of dietary fat to fatty acids and glycerol. Therefore, it decreases the absorption of lipids.
- On prolonged administration, orlistat brings about a significant reduction in body weight.
- The patient should also receive a low-calorie diet and an exercise program. Orlistat is poorly absorbed from the gut and is mostly excreted unchanged.
Drugs In Obesity Adverse Effects:
- Limited to the gut with abdominal cramps, fecal urgency, fecal incontinence, oily feces, and flatulence.
- It interferes with the absorption of vitamins hence supplementation is needed.
- There is also a decreased absorption of oral contraceptives and ciclosporin.
Drugs In Obesity Uses:
- Obesity
- Type 2 diabetes mellitus
Leave a Reply