Histology Of Pulp And Peri radicular Dental Tissue Development Notes
Dental Pulp Introduction
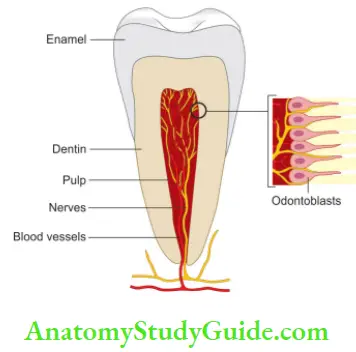
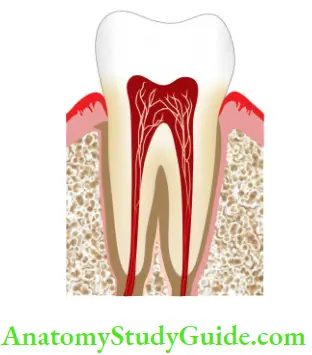
The dental pulp is the soft tissue of mesenchymal origin located in the center of a tooth. It consists of specialized cells, and odontoblasts arranged peripherally in direct contact with the dentin matrix. This close relationship between odontoblasts and dentin is known as the “pulp–dentin complex”.
Table of Contents
| Body Fluids | Muscle Physiology | Digestive System |
| Endocrinology | Face Anatomy | Neck Anatomy |
| Lower Limb | Upper Limb | Nervous System |
Read And Learn More: Endodontics Notes
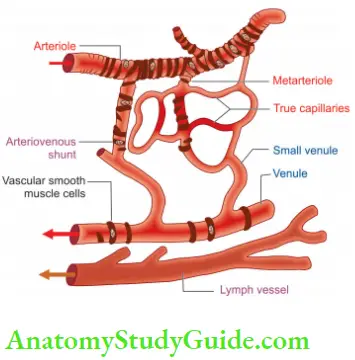
The connective tissue of the pulp consists of cells, ground substance, fibers, interstitial fluid, odontoblasts, fibroblasts, and other cellular components. It has soft gelatinous consistency. Pulp is a microcirculatory system consisting of arterioles and venules as the largest vascular component.
Due to a lack of true collateral circulation, the pulp is dependent upon a few arterioles entering through the foramen. In this chapter, we would discuss the comprehensive description of pulp embryology, anatomy, histology, physiology, and pulp changes with age.
Features of pulp, which distinguish it from tissue found elsewhere in the body:
- Pulp is surrounded by rigid walls and so is unable to expand in response to injury as a part of an inflammatory process. Therefore, pulpal tissue is susceptible to changes in pressure affecting the pain threshold.
- There is minimal collateral blood supply to pulp tissue which reduces its capacity for repair following injury.
- Due to the presence of specialized cells (odontoblasts and other cells which can differentiate into hard tissue-secreting cells), pulp retains its ability to form dentin throughout life.
- The innervation of the pulp tissue is both simple and complex. Simple in that there are only free nerve endings and consequently the pulp lacks proprioception. Complex because of the innervation of the odontoblast processes which produces a high level of sensitivity to thermal and chemical change.
Development Of Dental Pulp
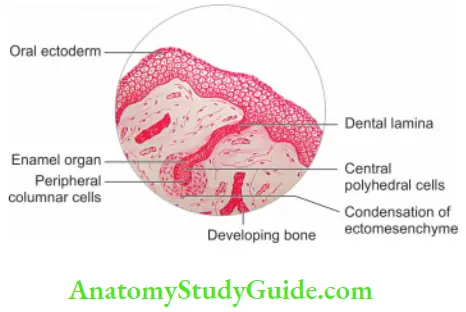
Initiation of tooth development begins at 37 days of development with the formation of a continuous horseshoe band of thickened epithelium in the location of upper and lower jaws called as a primary epithelial band. Each band of epithelium forms two subdivisions:
- Dental lamina
- Vestibular lamina
1. Dental Lamina:
- Dental lamina appears as a thickening of the oral epithelium adjacent to condensation of ectomesenchyme.
- In this, 20 knob-like areas appear, which form tooth buds for the 20 primary teeth. These areas appear at different times. The first ones to form are in the mandibular anterior region.
- Dental lamina begins to function at the 6th prenatal week and continues to the 15th year of birth. Successional lamina is the lamina from which permanent teeth develop Tooth development is a continuous process.
which can be divided into three stages:
- Bud stage
- Cap stage
- Bell stage
1. Bud stage:
It is the initial stage where epithelial cells of dental lamina proliferate and produce a budlike projection into adjacent ectomesenchyme
Pulp Cavity Of Tooth
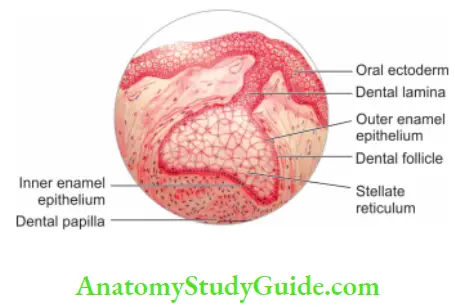
2. Cap stage:
It is formed when cells of dental lamina proliferate to form a concavity which produces a cap-like appearance. It shows outer and inner enamel epithelia and stellate reticulum. The Rim of the enamel organ, that is, where inner and outer enamel epithelia are joined is called the cervical loop.
3. Bell stage: As the cells of the loop proliferate, the enamel organ assumes the bell stage. Differentiation of epithelial and mesenchymal cells into ameloblasts and odontoblasts occurs during the bell stage. Pulp is initially called as dental papilla; it is designated as pulp only.
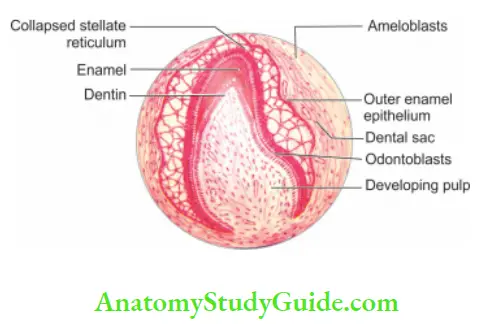
when dentin forms around it. The differentiation of odontoblasts from undifferentiated ectomesenchymal cells is accomplished by the interaction of cell and signaling molecules mediated through basal lamina and extracellular matrix. Dental papilla has high cell density and a rich vascular supply because of the proliferation of cells in it.
Cells of dental papilla appear as undifferentiated mesenchymal cells; gradually these cells differentiate into fibroblasts. The formation of dentin by odontoblasts heralds the conversion of dental papilla into pulp.
The boundary between the inner enamel epithelium and odontoblast forms a future dentin enamel junction. The junction of inner and outer enamel epithelium at the basal margin of the enamel organ represents the future cementoenamel junction. As the crown formation with enamel and dentin deposition continues, the growth and organization of pulp vasculature take place.
At the same time, as the tooth develops, unmyelinated sensory nerves and autonomic nerves grow into pulpal tissue. Myelinated fibers develop and mature at a slower rate and
plexus of Raschkow does not develop until after the tooth has erupted.
Histology Of Dental Pulp
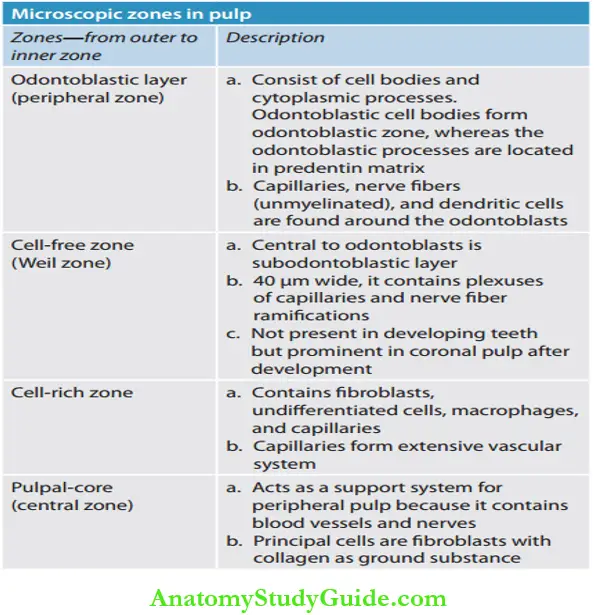
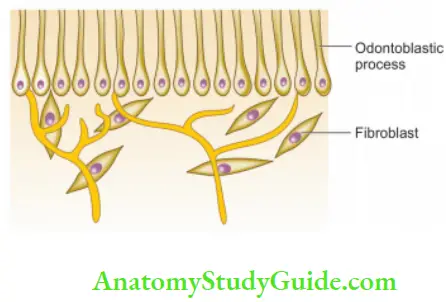
The pulp can be distinguished into the following four distinct zones from dentinopulpal junction toward the center of the tooth
Zones of pulp are:
- An odontoblastic layer at the pulp periphery
- Cell-free zone of Weil
- Cell rich zone
- Pulp core
Contents of the pulp
- Cells
- Odontoblasts
- Fibroblasts
- Undifferentiated mesenchymal cells
- Defense cells
- Macrophages
- Plasma cells
- Mast cells
- Matrix
- Collagen fibers
- Type 1
- Type 2
- Ground substance
- Glycosaminoglycans
- Glycoproteins
- Water
- Collagen fibers
- Blood vessels: Arterioles, venules, capillaries
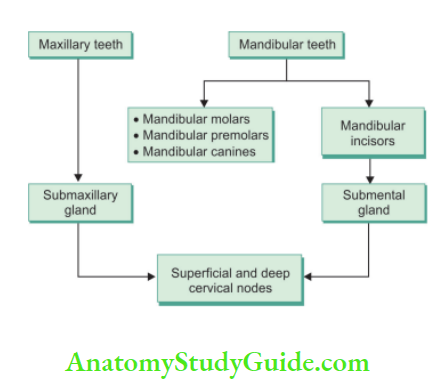
- Lymphatics: Draining to submandibular, submental, and deep cervical nodes
- Nerves
- Subodontoblastic plexus of Raschkow
- Sensory afferent from Vth nerve and superior cervical ganglion
Structural Or Cellular Elements
Odontoblasts:
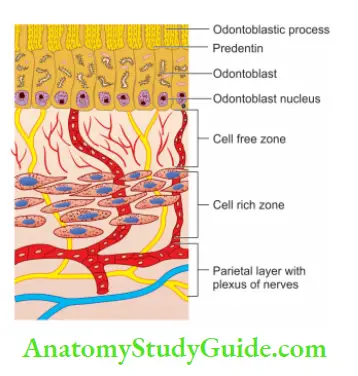
- These are first types of cells which come across when the pulp is approached from dentin
- The number of odontoblasts ranges from 59,000 to 76,000 per square millimeter in coronal dentin, with a lesser number in root dentin.
- Cell bodies of odontoblasts appear tall, pseudostratifid columnar in coronal pulp, a single row of cuboidal cells in radicular pulp, and flattened squamous type in the apical part.
- The morphology of odontoblasts reflects their functional activity which ranges from an active synthetic phase to a quiescent phase
- ultrastructure of odontoblast shows a large nucleus which may contain up to four nucleoli
- The nucleus is situated at the basal end. Golgi bodies are located centrally. Mitochondria, rough endoplasmic reticulum (RER), and ribosomes are distributed throughout the cell body.
- Odontoblasts synthesize mainly Type 1 collagen, and proteoglycans. They also secrete sialoproteins, alkaline phosphatase, phosphophoryn (phosphoprotein involved in extracellular mineralization).
- Irritated odontoblast secretes collagen, amorphous material, and large crystals into the tubule lumen which result in decreased permeability to an irritating substance.
During dentin formation in the crown, odontoblasts are pushed inwards to form the periphery of the pulp chamber. This circumference is smaller than the circumference at DEJ (Dentinoenamel junction) making odontoblasts to pack in pseudostratifid fashion in the coronal pulp.
Space in the root is not compressed, so odontoblasts maintain their cuboidal or columnar shape in the root area.
Tooth Pulp Function and Inflammation
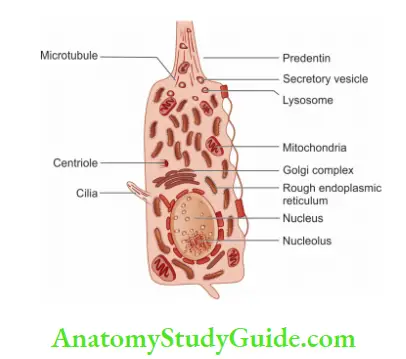
Fibroblasts:
- Fibroblasts are found in the greatest numbers in pulp
- “Baume” refers them to mesenchymal cells/pulp oblasts or adipocytes in their progressive levels of maturation
- These are spindle-shaped cells which secrete extracellular components like collagen and ground substance
- These cells have a dual function
- Formation and maintenance of fibrous components and ground substance of the connective tissue
- Degradation and ingestion of excess collagen by the action of lysosomal enzymes
- Fibroblasts of pulp are much like “Peter Pan” because they “never grow up” and remain in a relatively undifferentiated state
Reserve Cells/Undifferentiated Mesenchymal Cells:
- Undifferentiated mesenchymal cells are descendants of undifferentiated cells of dental papilla which can dedifferentiate and then re-differentiate into many cell types like odontoblasts and fibroblasts depending upon the stimulus
- These are found throughout the cell-rich and pulp core area
- They appear as large polyhedral cells possessing a large, lightly stained, centrally placed nucleus with abundant cytoplasm and peripheral cytoplasm extensions.
- In older pulps, the number of undifferentiated mesenchymal cells diminishes, along with a number of other cells in the pulp core. This reduces the regenerative potential of the pulp.
Defense Cells:
- Histiocytes and macrophages:
They originate from undifferentiated mesenchymal cells or monocytes.
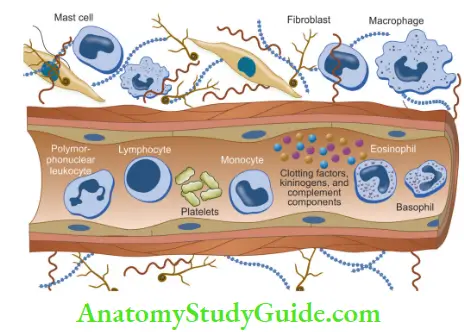
These cells appear as large oval or spindle shapes and are involved in the elimination of dead cells, debris, bacteria, and foreign bodies, etc.
- Polymorphonuclear leukocytes:
The most common form of leukocyte is neutrophil, though it is not present in the healthy pulp. These cells are mainly found in cases of microabscess formation. They are effective in destroying and phagocytizing bacteria and dead cells.
- Lymphocytes:
These are found extravascularly in normal pulps. They appear at the site of inflammation after invasion by neutrophils. These cells are associated with injury and resultant immune response. Thus their presence indicates the presence of persistent irritation.
- Mast cells:
On stimulation, degranulation of mast cells releases histamine which causes vasodilatation, increases vessel permeability and thus allows fluids and leukocytes to escape.
Extracellular Components:
Extracellular components include fibers and the ground substance of pulp:
Fibers:
- Principally Type 1 and Type 3 collagen fibers are found. Type 1 (55%) are present as thick striated fibrils, mainly responsible for pulp architecture. Type 3 (45%) are thinner fibrils and contribute to the elasticity of the pulp.
- The overall collagen content of the pulp increases With age but the ratio between Type 1 and Type 3 remains stable.
- Collagen is synthesized and secreted by odontoblasts and fibroblasts. Fibers produced by these cells differ in the degree of cross-linkage and variation in hydroxylysine content. Fibers secreted by fibroblasts do not calcify.
- Collagen with age becomes coarser and can lead to the formation of pulp stones
- In peripheral pulp, collagen fibers have unique arrangements forming von Korffs fiers. These are corkscrew-like originating between odontoblasts and passing into the dentin matrix
Reticular fibers termed argyrophilic fibers are common in young pulps. A small number of oxytalan fiers occur in the pulp. There are no elastic fibers in the pulp except those present in large blood vessels.
Clinical Tips:
Fibers are more numerous in radicular pulp than coronal and the greatest concentration of collagen occurs in the most apical portion of pulp. Thus engaging pulp with a barbed broach in apical area offers removal of the tissue intact than engaging the broach coronally, where the pulp is more gelatinous and liable to tear.
Ground Substance:
The ground substance of the pulp is a structureless mass with a gel-like consistency forming the bulk of the pulp. Chief components of ground substance are
- Glycosaminoglycans
- Glycoproteins
- Water (90%)
Tooth Pulp Inflammation
Depolymerization by enzymes produced by microorganisms found in pulpal inflammation may change the ground substance of the pulp. Alexander et al. in 1980 found that these enzymes can degrade the ground substance of the pulp by disrupting the glycosaminoglycan–collagen linkage.
Alterations in the composition of ground substances caused by age or disease interfere with metabolism, reduced cellular function, and irregularities in mineral deposition. This, ground substance plays an important role in the health and diseases of the pulp and dentin.
Functions of ground substance:
- Forms the bulk of the pulp
- Supports the cells
- Acts as a medium for transport of nutrients from the vasculature to the cells and of metabolites from cells to the vasculature
Systemic Factors Affecting Pulp
Vitamin Deficiency:
Vitamin C deficiency causes shriveling of fibroblasts. Since fibroblasts don’t develop fully, Fiers produced by them are shorter, thinner, and less dense resulting in an increase in permeability and bleeding tendency.
Steroids:
Prolonged use of steroids
- Inhibits collagen synthesis
- Affects odontoblasts and thus inhibits dentinogenesis and reparative dentin formation
- Reduction in the number of fibroblasts
Thyroid Deficiency:
- It reduces the vascularity of pulp
- Causes hypermineralization of bone and dentin
- Rapid deposition of dentin results in a smaller pulp cavity
Diabetes:
- Causes degenerative and inflammatory changes in pulp
Tooth Pulp Infection
Viral Infection:
- Systemic viral infection can result in injury to odontoblasts and pulp inflammation.
Hypoparathyroidism:
- It can interfere mineralization of roots of teeth which are not fully formed
- Affected teeth have shorter roots than normal teeth
Supportive Elements
Pulpal Blood Supply
Blood flow reflects the functional capacity of an organ. The normal rate of pulpal blood flow is 20–60 mL/min/100 g pulp tissue. It is higher than that of surrounding oral tissues and skeletal muscles but lower than that of the heart, kidney, or spleen.
Teeth are supplied by branches of the maxillary artery. Blood vessels enter the pulp via apical and accessory foramina. One or two arterioles enter the apical foramen with sensory and sympathetic nerve bundles.
Arterioles course up through radicular pulp and give of branches that spread laterally toward the odontoblasts layer and form capillary plexus. As they pass into coronal pulp, they diverge toward dentin, diminish in size and give rise to the capillary network in sub odontoblastic region. This network provides odontoblasts with a rich source of metabolites.
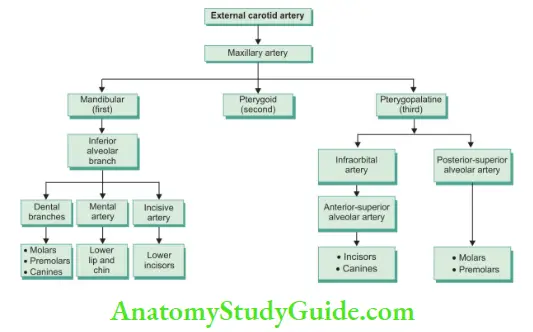
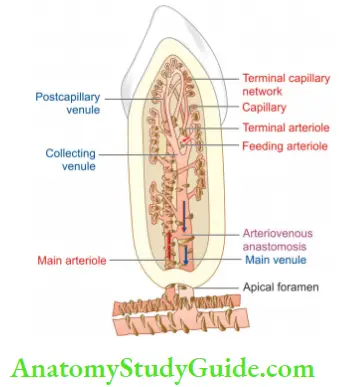
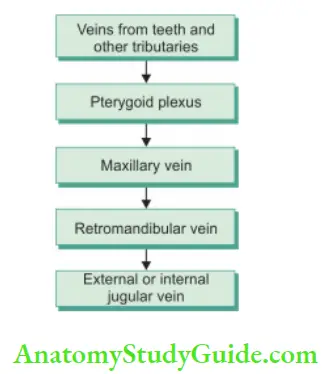
Blood passes from the capillary plexus into venules which constitute the efferent (exit) side of pulpal circulation and are slightly larger than corresponding arterioles. Venules enlarge as they merge and advance toward the apical foramen. Efferent vessels are thin-walled and show only scanty smooth muscle.
Tooth Pulp Function and Inflammation
Lymphatic Vessels
Lymphatic vessels arise as small, blind, thin-walled vessels in the coronal region of the pulp and pass apically through middle and radicular parts of pulp. Thy exit via one or two large vessels through the apical foramen.
Lymphatic vessels can be diffrentiated from small venules in the following ways:
- Lack of continuity in vessel walls
- Absence of RBC in their lumina
Regulation of Pulpal Blood Flow
Walls of arterioles and venules are associated with smooth muscles which are innervated by unmyelinated
sympathetic fibers. When stimulated by stimulus (for example, epinephrine containing local anesthetics), muscle fibers contract resulting in a decrease in blood supply.
Pulpal Response to Inflammation
Whenever there is an inflammatory reaction, there is the release of lysosomal enzymes which cause hydrolysis of collagen and the release of kinins. These changes further lead to increased vascular permeability.
The escaping fluid accumulates in the pulp interstitial space. Since space in the pulp is confined, so pressure within pulp chamber rises. In severe inflammation, lymphatics are closed resulting in the continued increase in flid and pulp pressure which may result in pulp necrosis.
Effect of Posture on Pulpal Flow
In a normal upright posture, there is less pressure effect in the structures of head. On lying down, pulpal blood pressure elevates because of following reasons:
- Removal of gravitational effect:
It causes an increase in pulpal blood pressure and a rise in tissue pressure and thus pain on the lying down position
- Inactivity of the sympathetic nervous system:
When a person is upright, baroreceptors maintain a high degree of sympathetic stimulation which leads to slight vasoconstriction. Lying down will reverse this effect leading to an increase in blood flow to pulp.
Clinical Correlation:
- Temperature changes
- Increase in temperature:
- A 10–15°C increase in pulp temperature causes arteriolar dilation and an increase in intrapulpal pressure of 2.5 mmHg/°C, but it is transient in nature.
- Irreversible changes occur when vasodilation is sustained by heating the pulp to 45°C for prolonged periods, resulting in a persistent increase in pulp pressure.
- Decrease in temperature:
- Increase in temperature:
A temperature lower than −2°C causes pathological changes in pulp tissue like vascular engorgement and necrosis
- Local anesthetics:
The effect of local anesthetics on pulp vasculature is mainly due to the presence of a vasoconstrictor in an anesthetic solution. Epinephrine present in local anesthetic causes a decrease in blood flow in the pulp Which is due to stimulation of α-adrenergic receptors located in pulpal blood vessels.
- Intrapulpal anesthesia:
It is obtained by injecting anesthesia into pulp under pressure. Because of this, pulp microcirculation decreases resulting in a transient increase in nerve excitability, and then decreases to zero.
- General anesthetics:
General anesthetics affect the velocity of blood flow in the pulp.
- Endodontic therapy:
During endodontic therapy, if only the coronal pulp is extirpated, profuse bleeding occurs, whereas removal of the pulp close to the apex results in less bleeding. This is because of the larger diameter of blood vessels in the central part of the pulp.
- Aging:
With increasing age, pulp shows a decrease in vascularity, an increase in fibrosis, a narrowing of the diameter of blood vessels, and a decrease in circulation. Finally, circulation gets impaired because of atherosclerotic changes and calcifications in the blood vessel leading to cell atrophy and cell death.
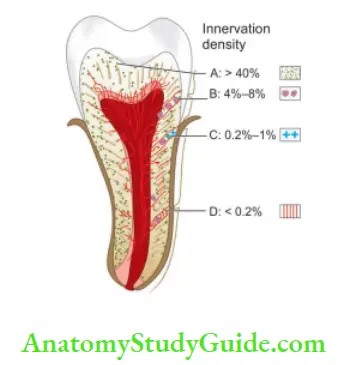
Innervation Of Pulp
The dental pulp is abundantly innervated by both sensory as well as autonomic nerve fibers. Nerve fibers enter the pulp through the apical foramen along with blood vessels. After entering the pulp, nerve bundles run coronally and divide into smaller branches until a single axons form a dense network near the pulp–dentin margin, termed as plexus of Raschkow.
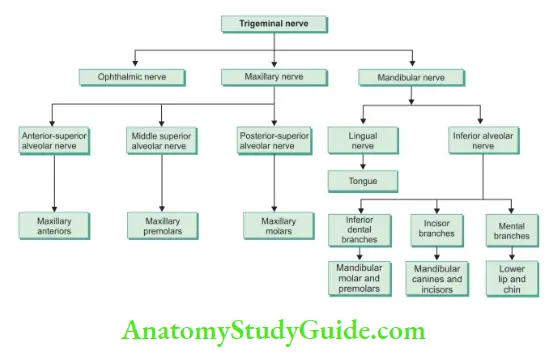
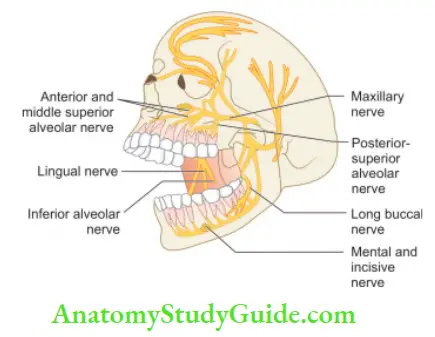
Also, the individual axons may branch into numerous terminal filaments which enter the dentinal tubules. Sensory nerves are encased in myelin sheaths. Myelin sheath is mainly composed of fatty substances or lipids and proteins.
Myelin appears to be an internal proliferation of Schwann cells. Unmyelinated fibers are surrounded by a single layer of Schwann cells, but in these myelin spirals are absent. Unmyelinated fibers are surrounded by a single layer of Schwann cells and are generally found in the autonomic nervous system.
Nerve fibers are classified according to their diameter, velocity of conduction, and function.
Fibers having the largest diameter are classified as A-fiers while those having the smallest diameter are classified as C-fiers. Aδ fiers are faster conducting and are responsible for localized, sharp dentinal pain. C-fibers are slower conducting and are responsible for dull and throbbing pain.
Electrical pulp tester stimulates Aδ fiers fist because of their lower threshold. As the intensity of the stimulus is increased along with Aδ fibers, some of the C-fibers also get stimulated resulting in a strong unpleasant sensation.
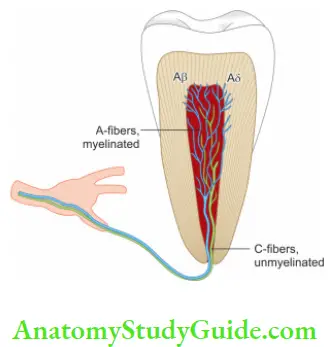
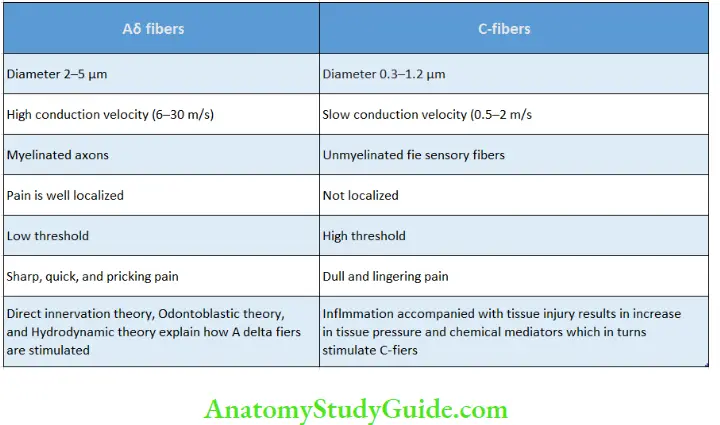
Aδ nerve fibers:
- Most of the myelinated nerve fibers are Aδ fiers
- At the odontoblastic layer, they lose their myelin sheath and anastomose forming a network of nerves called “plexuses of Raschkow.” They send free nerve endings into dentinal tubules
- The diameter of these fibers ranges from 2 to 5 µm and the conduction velocity 6–30 m/s.
- These are large files with fast conduction velocities
- Pain transmitted through these fibers is perceived as a sharp, quick, and momentary type
- Pain disappears quickly on the removal of stimulus
C-nerve fiers:
C-nerve fiers are small unmyelinated fie sensory afferent nerves
- They have slow conduction velocities and high threshold
- The diameter ranges from 0.3 to 1.2 µm and the conduction velocity is 0.5–2 m/s
- They are stimulated by intense cold or hot stimuli or mechanical stimulation
- Even in presence of radiographic lesion, C-fiers can show response because these are more resistant to hypoxic conditions or compromised blood flw as compared to Aδ fiers.
- These are responsible for pain occurring during instrumentation of teeth.
- Eighty percent of nerves of pulp are C-fiers and remaining are Aδ fiers
Anatomy Of Dental Pulp – Pulp Cavity Of Tooth
Pulp lies in the center of tooth and shapes itself to miniature form of tooth. This space is called pulp cavity which is divided into pulp chamber and root canal. In the anterior teeth, the pulp chamber gradually merges into the root canal and this division becomes indistinct .

But in case of multirooted teeth, there is a single pulp chamber and usually two to four root canals. As the external morphology of the tooth varies from person to person, so does the internal morphology of crown and the root.
Pulp Chamber:
It reflcts the external form of enamel at the time of eruption, but anatomy is less sharply defied. Roof of pulp chamber consists of dentin covering the pulp chamber occlusally.
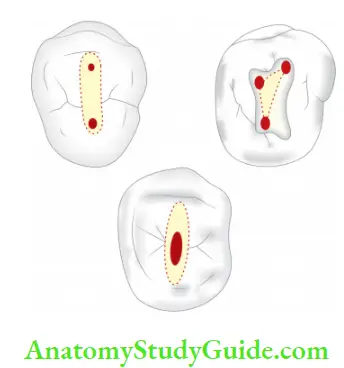
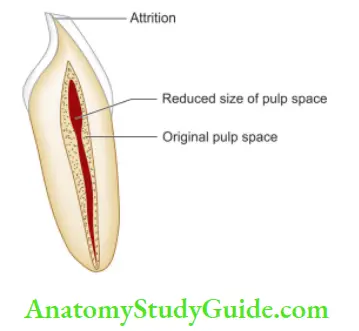
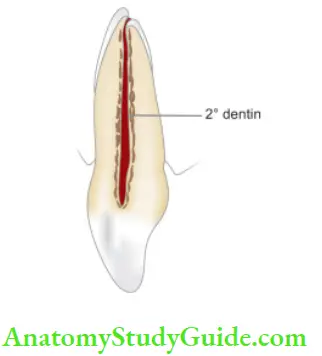
Canal orifies are openings in the flor of pulp chamber leading into the root canals. Because of caries, irritants, and advancing age, pulp chamber shows reduction in size due to deposition of secondary or tertiary dentin.
Pulp Cavity Of Tooth
Root Canal:
Root canal is portion of pulp cavity which extends from canal orifie to apical foramen. Shape of root canal varies with size, shape, number of the roots in diffrent teeth. A straight root canal throughout the entire length of root is uncommon.
Curvature is found commonly along root length which can be gradual or sharp. In most cases, numbers of root canals correspond to number of roots but a root may have more than one canal.
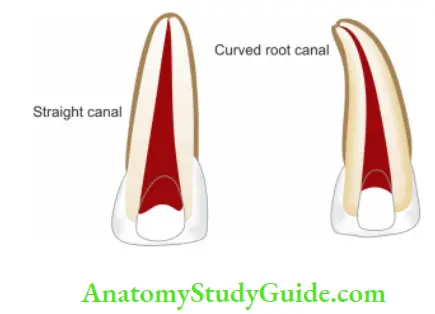
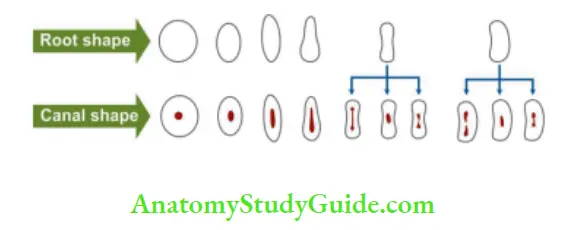
According to Orban, the shape of the canal can be determined by shape of the root. Root canals can be round, tapering elliptical, broad, thin, etc.
“Meyer” stated that roots which are round and cone
shaped usually contain one canal but roots which are elliptical with flt or concave surfaces frequently have more than one canal.
Pulp Cavity Of Tooth
The apical foramen is an aperture at or near the apex of a root through which nerves and blood vessels of the pulp enter or leave the pulp cavity. In young newly erupted teeth, it is wide open, but as the root develops, apical foramen becomes narrower. The inner surface of the apex is lined with the cementum which may extend for a short distance into the root canal.
Thus we can say that CDJ (Cementodentinal junction) does not necessarily occur at the apical end of the root but may occur within the main root canal. Multiple foramina are found in multirooted teeth. The majority of single-rooted teeth have a single canal which terminates in a single foramen.
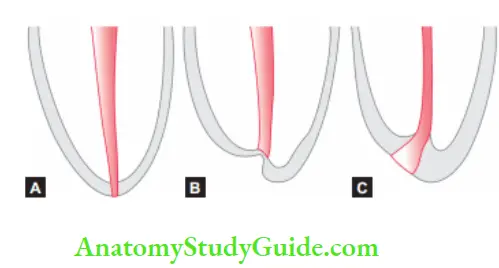
Change in shape and location of foramen can occur during the posteruptive phase due to functional forces (tongue pressure, mesial drift) acting on the tooth. These forces cause resorption and deposition of cementum on walls of the foramen resulting in shifting of its position.
- There are a total of 52 pulp organs, 32 in the permanent, and 20 in the deciduous teeth.
- The total volume of all permanent pulp organs is 0.38 cm 3 with a mean of 0.02 cm 3.
- The average size of an apical foramen in maxillary teeth is 0.4 mm.
- The average size of an apical foramen in mandibular teeth is 0.3 mm
Accessory canals:
These are the lateral branches of the main canal that form communication between the pulp and periodontium. Accessory canals contain connective tissue and vessels and can be seen anywhere from furcation to the apex but tend to be more common in the apical third of posterior teeth.
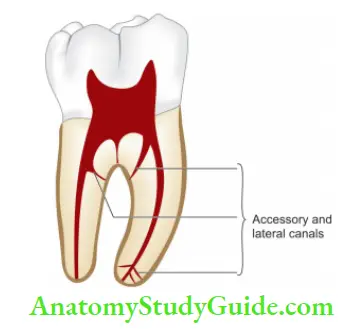
Mechanism of formation:
- Accessory canals occur in areas of premature loss of root sheath cells because these cells induce the formation of odontoblasts.
- In areas where developing root encounters a blood vessel. When dentin is forming; hard tissue may develop around a blood vessel resulting in accessory canal formation.
Dental Pulp Function – Functions Of Pulp
Pulp lives for dentin and the dentin lives by the grace of the pulp.
Four basic functions of pulp:
- Formation of dentin
- Nutrition of dentin
- Innervation of tooth
- Defense of tooth
1. Formation of dentin:
It is the primary function of pulp both in sequence and importance. From the mesodermal aggregation (dental papilla) arises a special layer of odontoblasts adjacent to the inner layer of the ectodermal enamel organ. On the interaction of ectoderm and mesoderm, odontoblasts initiate dentin formation
Pulp primarily helps in
- Synthesis and secretion of the organic matrix.
- Initial transport of inorganic components to the newly formed matrix.
- Creating an environment favorable for matrix mineralization
2. Nutrition of dentin:
Nutrients exchange across capillaries into the pulpal interstitial fluid. This flid travels into the dentin through the network of tubules formed by the odontoblasts to contain their processes.
3. Innervation of tooth:
Pulp and dentin show innervation due to the presence of fluid movement between dentinal tubules and peripheral receptors and thus to sensory nerves of the pulp.
4. Defense of tooth:
Odontoblasts form dentin in response to injury in the form of caries, attrition, trauma, or restorative procedure. Formation of reparative dentin and sclerotic dentin forms the defense mechanisms of the tooth. Formation of reparative dentin occurs at the rate of 1.5 µm/day. The quantity and quality of formed reparative dentin is directly related to the severity and duration of injury to the pulp.
Pulp also shows an inflammatory and immunologic response in an attempt to neutralize or eliminate the invasion of microorganisms and their byproducts in dentin.
Age Changes In The Pulp
Pulp-like other connective tissues undergoes changes with time. These changes can be natural or may be the result of injuries
such as caries, trauma, or restorative dental procedure. Regardless of the cause, the pulp shows changes in appearance (morphogenic) and functions (physiologic).
Morphologic Changes:
- Reduction of tubular diameter due to continuous deposition of intratubular dentin.
- Reduction in pulp volume due to an increase in secondary dentin deposition. It gives the root canal a very thin or obliterated appearance.
- Presence of dystrophic calcification and pulp stones.
- Decrease in the number of pulp cells. Cell density decreases to 50% by the age of 70.
- Decrease in sensitivity due to degeneration and loss of myelinated and unmyelinated axons.
- Reduction in the number of blood vessels, displaying arteriosclerotic changes.
- The presence of collagen in pulp becomes more apparent because of the formation of collagen bundles. Recent studies have shown that collagen content does not increase with age but stabilizes after the completion of tooth formation.
Physiologic Changes:
- Decrease in dentin permeability giving a protective environment to the pulp.
- Reduced ability of pulp to react to the irritants and repair itself.
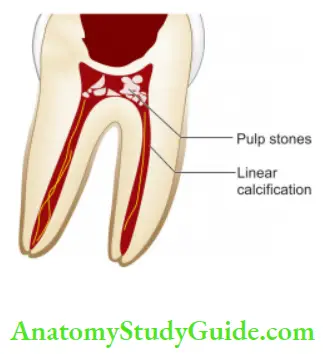
Pulpal Calcifiations Or Pulp Stones Or Denticles
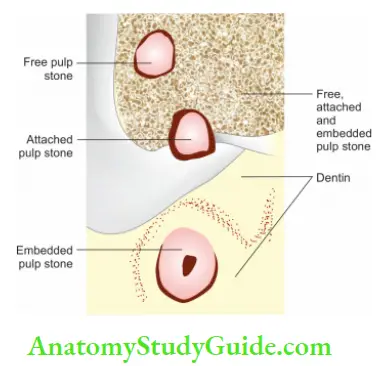
Pulp stones are nodular calcified masses present in mature teeth. Larger calcifications are called denticles. Sometimes denticles become extremely large, almost obliterating the pulp chamber or the root canal.
The incidence of pulp stones increases with age, but they are also found in young ages.
Classification of pulp stone:
- According to structure
- True
- False
- According to size
- Fine
- Diffuse
- According to location
- Free
- Attached
- Embedded
According to Structure:
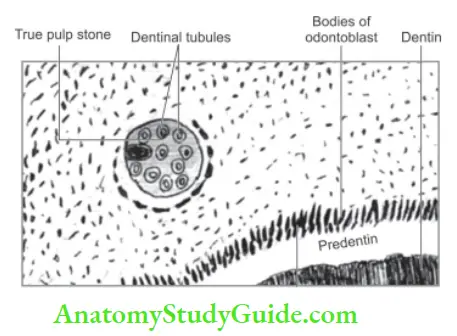
True Denticle:
A true denticle is made up of dentin and is lined by odontoblasts. These are rare and usually located close to the apical foramen. The development of true denticles is caused by inclusions of remnants of epithelial root sheath within the pulp. These epithelial remnants induce the cells of pulp to differentiate into odontoblasts which form dentin masses.
False Denticles:
Appear as concentric layers of calcified tissue. These appear within bundles of collagen fibers. They may arise around vessels. Calcification of thrombi in blood vessels, called phleboliths, may also serve as nidi for false denticles.
All denticles begin as small nodules but increase in size by incremental growth on their surface.
According to Size:
According to size, pulp stones can be fine and diffuse mineralizations. Diffuse calcifications are also known as fibrillar or linear calcifications because of their longitudinal orientation. These can be found in any area but are more frequently found in the radicular pulp.
They are aligned close to blood vessels, nerves, or collagen bundles. These are not visible on radiographs because of their size and dispersion.
According to Location:
- Free denticles are like islands, that is, entirely surrounded by pulp tissue.
- Attached denticles are free pulp stones which partially fuse to continuously growing dentin.
- Embedded denticles are attached stones that are now entirely surrounded by dentin.
Clinical Significance of Pulp Stones:
The presence of pulp stones may alter the internal anatomy of the pulp cavity, making the access opening of the tooth difficult. Thy may deflect or engage the tip of the exploring the instrument.
Since the pulp stone can originate in response to chronic irritation, the pulp chamber which appears to have diffuse and obscure outline may represent a large number of irregular pulp stones which may indicate chronic irritation of the pulp.
Periradicular Tissue
Periradicular Tissue consists of cementum, periodontal ligament, and alveolar bone.
Periradicular Tissue Cementum:
Cementum is a hard, avascular connective tissue that covers the roots of the teeth. It is light yellow in color and can be differentiated from enamel by its darker hue and lack of luster. It is very permeable to dyes and chemical agents, from the pulp canal and the external root surface.
Periradicular Tissue Types:
Two main types of cementum are:
1. Acellular cementum
- Covers the cervical third of the root
- Forms before tooth reach the occlusal plane
- It does not contain cells
- Thickness varies between 30 and 230 µm
- The abundance of Sharpey’s fires
- The main function is anchorage
2. Cellular cementum
- Forms after tooth reach the occlusal plane
- It contains cells
- Less calcifid than acellular cementum
- Sharpey’s fibers are present in lesser numbers as compared to acellular cementum
- Mainly found in the apical third and inter-radicular region
- The main function is an adaptation
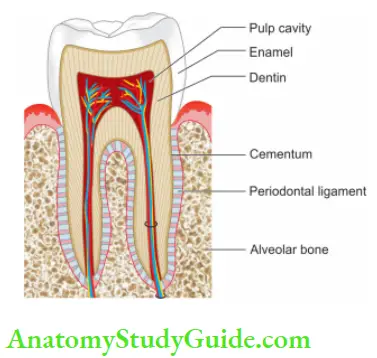
Periodontal Ligament:
The periodontal ligament is a unique structure as it forms a link between alveolar bone and cementum. It is continuous with the connective tissue of the gingiva and communicates with the marrow spaces through vascular channels in the bone.
The periodontal ligament houses the fiers, cells, and other structural elements like blood vessels and nerves.
The periodontal ligament comprises of the following components:
- Periodontal fiers
- Cells
- Blood vessels
- Nerves
Periodontal Fibers:
The most important component of the periodontal ligament is the principal fiers. These fiers are composed mainly of collagen Type 1. Apart from the principal fiers, xylan and elastic fiers are also present. The principal fiers are present in six arrangements.
Horizontal group:
These fiers are arranged horizontally emerging from the alveolar bone and attached to the root cementum.
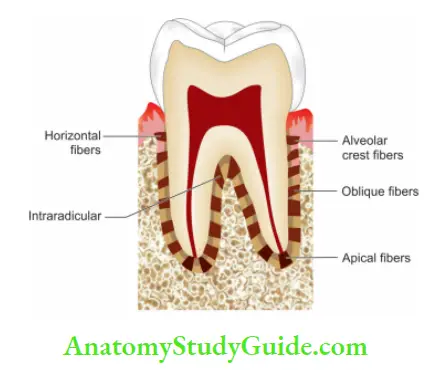
Alveolar crest group:
These fiers arise from the alveolar crest in a fan-like manner and attach to the root cementum. These fiers prevent the extrusion of the tooth.
Oblique fibers:
These fibers make the largest group in the periodontal ligament. They extend from the cementum to bone obliquely. They bear the occlusal forces and transmit them to the alveolar bone.
Trans-septal fiers:
These fiers run from the cementum of one tooth to the cementum of another tooth crossing over the alveolar crest.
Apical fiers:
These fiers are present around the root apex.
Inter-radicular fiers:
These fiers are present in furcation areas of multirooted teeth.
Cells
The cells present in the periodontal ligament are:
-
- Fibroblast
- Macrophages
- Mast cells
- Neutrophils
- Lymphocytes
- Plasma cells
- Epithelial cell rests of Malassez
Nerve Fibers:
The nerve fiers present in the periodontal ligament are either of myelinated or non-myelinated type.
Blood Vessels:
The periodontal ligament receives blood supply from the gingival, alveolar, and apical vessels.
Functions:
1. Supportive:
The tooth is supported and suspended in an alveolar socket with the help of the periodontal ligament.
2. Nutritive:
The periodontal ligament has a very rich blood supply. So, it supplies nutrients to adjoining structures like cementum, bone, and gingiva via blood vessels. It also provides lymphatic drainage.
3. Protective:
These fiers perform the function of protection absorbing the occlusal forces and transmitting to the underlying alveolar bone.
4. Formative:
The cells of PDL (periodontal ligament) help in the formation of surrounding structures like alveolar bone and cementum.
5. Resorptive:
The resorptive function is also accomplished with the cells like osteoclasts, cementoblasts, and fibroblasts provided by the periodontal ligament.
Alveolar Bone
Bone is specialized connective tissue which comprises of inorganic phases that is very well designed for its role as the load-bearing structure of the body.
Cells
Cells present in bone are:
- Osteocytes
- Osteoblasts
- Osteoclasts
Intercellular Matrix:
Bone consists of two-thirds inorganic matter and one-third organic matter. Inorganic matter is composed mainly of minerals calcium and phosphate along with hydroxyapatite, carbonate, citrate, etc. while the organic matrix is composed mainly of collagen Type 1 (90%).
Bone consists of two plates of compact bone separated by spongy bone in between. In some areas, there is no spongy bone. The spaces between trabeculae of spongy bone are filled with marrow which consists of hemopoietic tissue in early life and fatty tissue later in life. Bone is a dynamic tissue that continuously forms and resorbs in response to functional needs.
Both local as well as hormonal factors play an important role in the metabolism of bone. In healthy conditions, the crest of the alveolar bone lies approximately 2–3 mm apical to the cementoenamel junction, but it comes to lie more apically in periodontal diseases. In periapical diseases, it gets resorbed easily.
Leave a Reply