Hypersensitivity
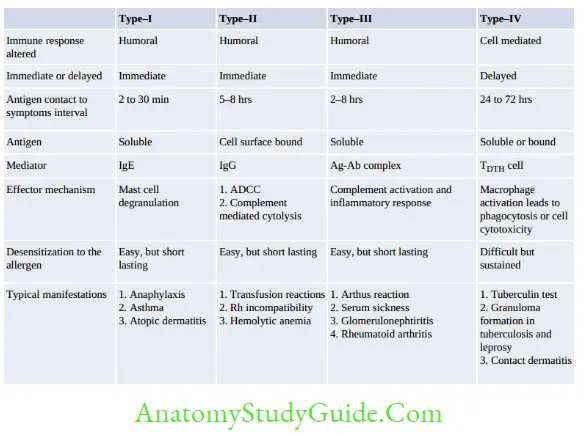
Hypersensitivity or allergy refers to the injurious consequences in the sensitized host, following subsequent contact with specific antigens.
Table of Contents
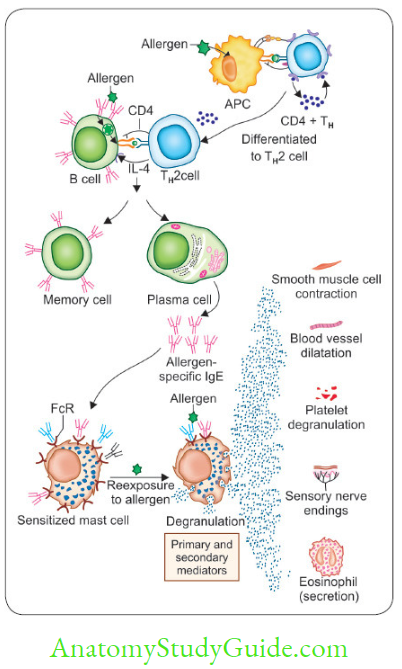
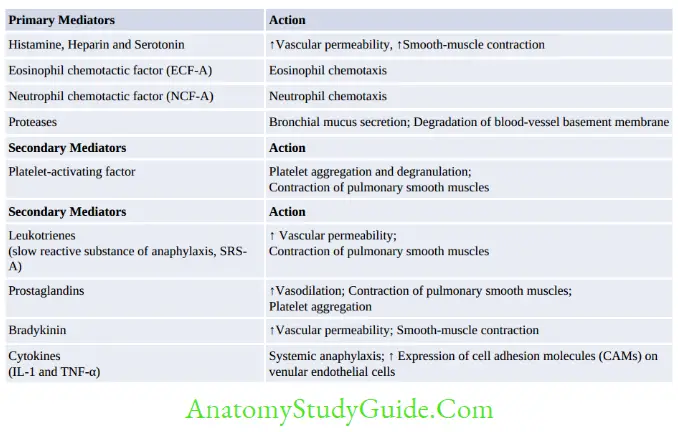
Type-1 Hypersensitivity Reaction
Mechanism
Type-1 Hypersensitivity reaction occurs through two phases:
Read And Learn More: Micro Biology And Immunology Notes
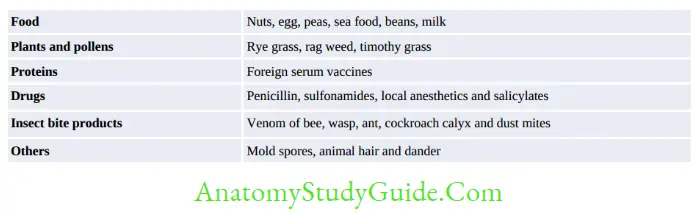
Examples of Type 1 Hypersensitivity Reaction
- Experiments to demonstrate type I hypersensitivity reaction: P-K reaction, Schultz Dale phenomenon and Theobald smith phenomenon
- Systemic anaphylaxis
- Localized anaphylaxis (atopy) such as:
- Allergic rhinitis (or hay fever)
- Asthma
- Food allergy
- Atopic urticarial
- Atopic dermatitis (allergic eczema)
- Drug allergy
- Wheal and flare reaction.
- Parasitic diseases/tests:
- Casoni test (hydatid disease)
- Tropical Pulmonary Eosinophilia (TPE)
- Loeffler’s pneumonia (Ascaris)
- Ground itch (Hookworm)
- Leakage of hydatid fluid
- Cercarial dermatitis/swimmer’s itch (Schistosoma).
Treatment of Type 1 Hypersensitivity Reaction
- Avoidance of contact with known allergens
- Hyposensitization: Repeated exposure to increased subcutaneous doses of allergens can reduce or eliminate the allergic response to the same allergen.
- Humanized Monoclonal anti-IgE-It can bind and block IgE.
- Drugs: Several drugs are useful in suppressing type-1 response such as antihistamines, adrenaline, cortisone, theophylline, and cromolyn sodium.
Type-2 Hypersensitivity Reaction
In type-II reactions, the host injury is mediated by antibodies (IgG or rarely IgM) which interact with various types of antigens such as:
- Host cell surface antigens (e.g. RBC membrane antigens like blood group and Rh antigens)
- Extracellular matrix antigens or
- Exogenous antigens absorbed on host cells (e.g. a drug coating on RBC membrane).
After Ag-Ab binding occurs, the Fc region of antibody initiates the type-II reactions by the following three broad mechanisms:
Antibody (Fc) Activating Complement System
By complement-dependent cytolysis (due to MAC), inflammation (by C5a, C3a), opsonization (by C3b and C4b)
It is seen in following conditions:
- Transfusion reaction (ABO incompatibility)
- Erythroblastosis fetalis
- Autoimmune hemolytic anemia, agranulocytosis, or thrombocytopenia
- Drug-induced hemolytic anemia
- Pemphigus vulgaris
- Hyper acute graft rejection.
Antibody (FC Portion) Interacting with Fc Receptors on Target Cells
- Antibody-dependent cellular cytotoxicity (ADCC)
- Opsonization.
Antibody-Dependent Cellular Dysfunction or ADCD
Autoantibody Mediated:
- Activation of receptor, e.g. Grave’s disease
- Inhibition of receptor, e.g. Myasthenia gravis
- Other examples of ADCD:
- Good pasture syndrome (antibody produced against type IV collagen)
- Pernicious anemia (antibody directed against intrinsic factor)
- Rheumatic fever (antibody against streptococcal antigens cross reacting with heart)
- Myocarditis in Chagas disease.
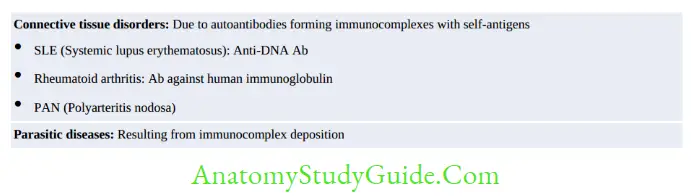
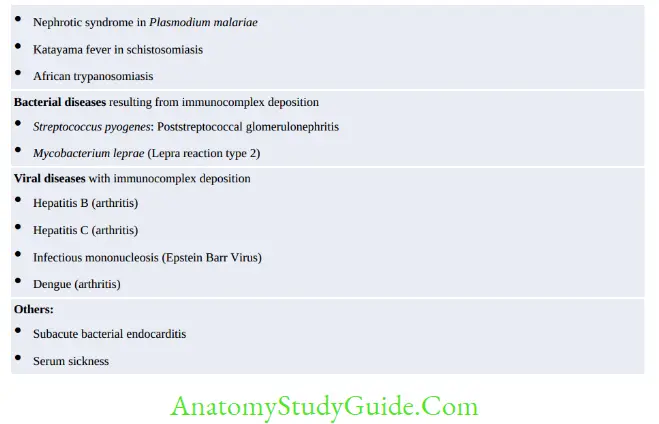
Type-3 Hypersensitivity Reaction
Type-3 hypersensitivity reactions are as a result of excess formation of immune complexes (AgAb complexes) which initiate an inflammatory response through activation of complement
system leading to tissue injury:
- Localized or Arthus reaction
- In skin: (1) following insect bites or (2) during allergic desensitization
- In lungs (1) Farmer’s lung (Saccharopolyspora species), (2) Bird-Fancier’s disease
- Generalized or Systemic type III Reactions, e.g. Serum sickness.
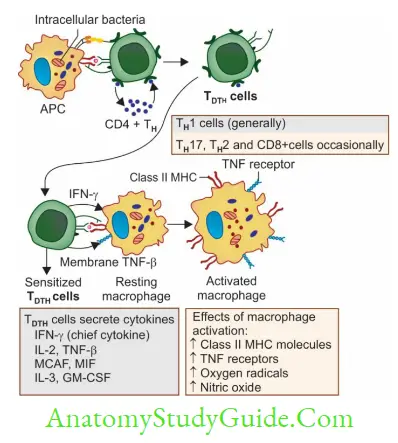
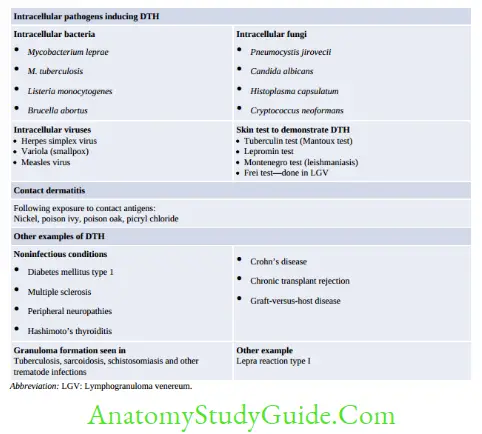
Type-4 Hypersensitivity Reaction
Type-4 hypersensitivity reactions differ from other types in various ways:
- It is delayed-type (occurs after 48–72 hours of antigen exposure)
- Cell-mediated: Characteristic cells called TDTH cells are the principal mediators
- Tissue injury occurs predominantly due to activated macrophages.
Mechanism of Type-IV Reactions
- Sensitization phase (occurs 1–2 weeks following Ag exposure): APCs process and present the antigenic peptides to TH cells.
TH cells are differentiated to TH1 cells which further differentiate to form TDTH cells - Effector phase: The TDTH cells, on subsequent contact with the antigen, secrete variety of cytokines such as:
- Interferon γ
IL-2 - MCAF (Monocyte chemotactic and activating factor)
- TNF-β
- MIF (migration inhibitory factor)
- IL-3
- GM-CSF (granulocyte-monocyte colony-stimulating factor).
- Interferon γ
Cytokines in turn perform various functions which may be either protective type or tissue damage type.
Leave a Reply