Immunopathogenesis Of Leprosy Notes
Immunology Of Leprosy:
Like in tuberculosis, the immune response in leprosy is also T cell-mediated delayed hypersensitivity (type IV reaction) but the two diseases are quite dissimilar as regards immune reactions and lesions. M. leprae do not produce any toxins but instead the damage to tissues is immune-mediated.
This is due to the following peculiar aspects in immunology of leprosy:
Read And Learn More: General Pathology Notes
1. Antigens of leprosy bacilli:
Lepra bacilli have several antigens. The bacterial cell wall contains large amount of M. leprae-specific phenolic glycolipid (PGL-1) and another surface antigen, lipoarabinomannan (LAM). These antigens of the bacilli determine the immune reaction of host lymphocytes and macrophages. Another unique feature of leprosy bacilli is invasion in peripheral nerves which is due to binding of trisaccharide of M. leprae to basal lamina of Schwann cells (neurotropism).
2. Genotype of the host:
Genetic composition of the host as known by MHC class (or HLA type) determines which antigen of leprosy bacilli shall interact with host immune cells. Accordingly, the host response to the leprosy bacilli in different individuals is variable.
3. T cell response: There is variation in T cell response in two main forms of leprosy:
- Unlike tubercle bacilli, there is not only activation of CD4+ T cells but also of CD8+ T cells.
- CD4+ T cells in lepra bacilli-infected persons act not only as helper and promoter cells but also assume the role of cytotoxicity.
- The two subpopulations of CD4+ T cells (or T helper cells)—TH 1 cells and TH 2 cells, elaborate different types of cytokines in response to stimuli from the lepra bacilli and macrophages.
- In tuberculoid leprosy, the response is largely by CD4+ T cells, while in lepromatous leprosy although there is excess of CD8+ T cells (suppressor T) but the macrophages and suppressor T cells fail to destroy the bacilli due to CD8+ T cell defect.
4. Humoral response:
Though the patients of lepromatous leprosy have humoral immune response such as high levels of immunoglobulins (IgG, IgA, IgM) and antibodies to mycobacterial antigens but these antibodies do not have any protective role against lepra bacilli.
Based on the above unique immunologic features in leprosy, lesions in leprosy are classified into 5 distinct clinico-pathologic types and three forms of reactional leprosy (described below), and an intradermal immunologic test, lepromin test, has been described.
Lepromin Test:
It Is Not A Diagnostic Test But Is Used For Classifying Leprosy On The Basis Of immune response. Intradermal injection of lepromin, an antigenic extract of M. leprae, reveals delayed hypersensitivity reaction in patients of tuberculoid leprosy:
- An early positive reaction appearing as an indurated area in 24-48 hours is called Fernandez
reaction. - A delayed granulomatous lesion appearing after 3-4 weeks is called a Mitsuda reaction.
Patients of lepromatous leprosy are negative by the lepromin test.
The test indicates that cell-mediated immunity is greatly suppressed in lepromatous leprosy while patients of tuberculoid leprosy show good immune response. A delayed type of hypersensitivity is conferred by T helper cells.
The granulomas of tuberculoid leprosy have sufficient T helper cells and fewer T suppressor cells at the periphery while the cellular infiltrates of lepromatous leprosy lack T helper cells.
Classification Ridley And Jopling’S Classification:
Traditionally, two main forms of leprosy are distinguished:
- A lepromatous type representing low resistance; and
- Tuberculoid type represents high resistance.
Salient differences between these two forms of leprosy are summarised in Table
Since both these types of leprosy represent two opposite poles of the host immune response, these are also called polar forms of leprosy. Cases not falling into either of the two poles are classified as borderline and indeterminate types.
Based on clinical, histologic and immunologic features, modified Ridley and Jopling’s classification has been described which divides leprosy into 5 groups as under:
Difference Between Lepromatous And Tuberculoid Leprosy:

- TT — Tuberculoid Polar (High resistance)
- BT — Borderline Tuberculoid
- BB — Mid Borderline (Dimorphic)
- BL — Borderline Lepromatous
- LL — Lepromatous Polar (Low resistance)
Variants Leprosy :
In addition, a few variant forms of leprosy which are not included in RidleyJopling’s classification have been described:
- Indeterminate leprosy This is an initial non-specific stage of any type of leprosy. Pure neural leprosy In these cases, skin lesions which are the cardinal feature of leprosy are absent but instead neurologic involvement is the main feature.
- Histoid leprosy Described by Wade in 1963, this is a variant of LL in which the skin lesions resemble nodules of dermatofibroma and the lesions are highly positive for lepra bacilli.
Reactional Leprosy:
Based on shift in immune status, or in patients of leprosy on treatment, two types of reactional leprosy are distinguished: type I (reversal reactions), and type II (erythema nodosum leprosum).
Type I: Reversal reactions:
The polar forms of leprosy do not undergo any change in the clinical and histopathological picture. The borderline groups are unstable and may move across the spectrum in either direction with upgrading or downgrading of the patient’s immune state.
Accordingly, there may be two types of borderline reactions:
- Upgrading reaction is characterised by increased cell-mediated immunity and occurs in patients of borderline lepromatous (BL) type on treatment who upgrade or shift towards tuberculoid type.
- Downgrading reaction is characterised by lowering of cellular immunity and is seen in borderline tuberculoid (BT) type who downgrade or shift towards lepromatous type.
Type II: Erythema nodosum leprosum (ENL):
ENL occurs in lepromatous patients after treatment. It is characterised by tender cutaneous nodules, fever, iridocyclitis, synovitis and lymph node involvement.
Histopathology Of Leprosy:
Usually, skin biopsy from the margin of lesions is submitted for diagnosis and for classification of leprosy. The histopathologic diagnosis of multibacillary leprosy like LL and BL offers no problem while the indeterminate leprosy and tuberculoid lesions are paucibacillary and their diagnosis is made together with clinical evidence.
In general, for histopathologic evaluation of skin biopsy in all suspected cases of leprosy.
The following general features should be looked for:
- Cell type of granuloma
- Nerve involvement
- Bacterial load
- Presence and absence of lymphocytes
- Relation of granuloma with epidermis and adenexa.
The salient features in major types of leprosy are as follows.
1. Lepromatous leprosy:
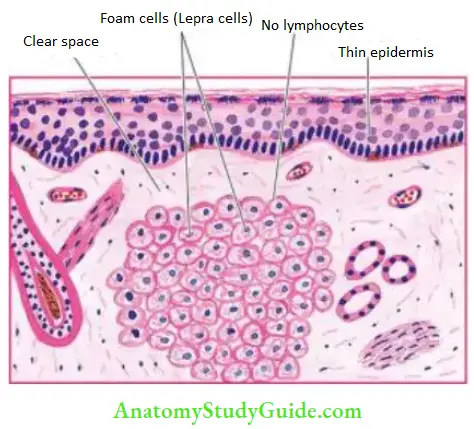
The following features characterise lepromatous polar leprosy:
- In the dermis, there is proliferation of macrophages with foamy change, particularly around the blood vessels, nerves and dermal appendages. The foamy macrophages are called ‘lepra cells’ or Virchow cells.
- The lepra cells are heavily laden with acid-fast bacilli demonstrated with AFB staining.
- The AFB may be seen as compact globular masses (globi) or arranged in parallel fashion like ‘cigarettes-in-pack’.
- The dermal infiltrate of lepra cells characteristically does not encroach upon the basal layer of epidermis and is separated from the epidermis by a subepidermal uninvolved clear zone.
- The epidermis overlying the lesions is thinned out, flat and may even ulcerate.
2. Tuberculoid leprosy:
- The polar tuberculoid form presents the following histological features :
- The dermal lesions show granulomas resembling hard tubercles composed of epithelioid cells, Langhans’ giant cells and peripheral mantle of lymphocytes.
- Lesions of tuberculoid leprosy have a predilection for dermal nerves which may be destroyed and infiltrated by epithelioid cells and lymphocytes.
- Lepromatous leprosy (LL). There is collection of proliferating foam macrophages (lepra cells) in the dermis, sparse lymphocytes and a clear subepidermal zone.
- Tuberculoid leprosy (TT). Granuloma erodes the basal layer of the epidermis. The granuloma is composed of epithelioid cells with sparse Langhans’ giant cells and many lymphocytes.
- The granulomatous infiltrate erodes the basal layer of epidermis i.e. there is no clear zone.
- The lepra bacilli are few and seen in destroyed nerves.



3. Borderline leprosy:
- The histopathologic features of the three forms of borderline leprosy are as under:
- The borderline tuberculoid (BT) form shows epithelioid cells and plentiful lymphocytes.
- There, is a narrow clear subepidermal zone. Lepra bacilli are scanty and found in nerves.
- The borderline lepromatous (BL) form shows a predominance of histiocytes, a few epithelioid cells, and some irregularly dispersed lymphocytes. Numerous lepra bacilli are seen.
- Mid-borderline (BB) or dimorphic form shows sheets of epithelioid cells with no giant cells. Some lymphocytes are seen in the perineurium. Lepra bacilli are present, mostly in nerves.
4. Indeterminate leprosy:
- The histopathologic features are non-specific so the diagnosis of non-specific chronic dermatitis may be made. However, a few features help in suspecting leprosy as:
- Lymphocytic or mononuclear cell infiltrate localized particularly around skin adnexal structures like hair follicles and sweat glands or around blood vessels.
- Nerve involvement, if present, is strongly supportive of diagnosis.
- Confirmation of the diagnosis is made by the finding of lepra bacilli.
- Pure neural leprosy Histopathologic features described in skin lesions of various forms of leprosy may be seen in the nerve biopsy specimens. Pure neural leprosy may be AFB positive or AFB negative.
5. Histoid leprosy:
- The following features characterize these lesions:
- Whorls and fascicles of spindle cells in the upper dermis after a clear subepidermal space.
- On close scrutiny, these cells have foamy cytoplasm.
- The cytoplasm of these cells is laden with lepra bacilli.
6. Reactional leprosy:
Two types of reactional leprosy show the following features:
- Type I reaction: Reversal reactions. These may be upgrading or downgrading types of
reaction: - Upgrading reaction: Shows an increase of lymphocytes, edema of the lesions, necrosis in the center and reduced BI
- Downgrading reaction: Shows dispersal and spread of the granulomas and increased presence
of lepra bacilli. - Type II reaction: ENL The lesions in ENL show infiltration by neutrophils and eosinophils and prominence of vasculitis. Inflammation often extends deep into the subcutaneous fat causing panniculitis. Bacillary load is increased. Secondary amyloidosis may follow repeated attacks of ENL in leprosy.
Leave a Reply