Inflammation and Repair
Question 1. Define inflammation. Describe the vascular and cellular changes in acute inflammation. Add a note on defective leukocyte function.
Answer:
Inflammation
- Host response that can get rid of the damaged or necrotic tissues and microbes
- Brought about by phagocytic leukocytes, antibodies, and complement proteins
Read and Learn More Preparatory Manual of Pathology Question and Answers
1. Vascular Changes in Acute Inflammation
- Vasodilation: Mediated by histamine, results in increased blood flow, which causes erythema (heat and redness)
- Vasodilation is followed by increased permeability of microvasculature (occurs due to endothelial retraction or endothelial damage)
- Stasis: Dilatation of small vessels, packed with slowly moving red cells
- Neutrophils accumulate and adhere to the vascular endothelium, followed by movement into the interstitial tissue.
2. Cellular Changes in Acute Inflammation
1. Leukocyte adhesion to endothelium
- Normally, RBCs and leucocytes, flow axially, however, in inflammation, due to stasis, WBCs assume a peripheral position along the endothelial surface.
- This process of leukocyte re-distribution is called margination.
- Leucocytes adhere transiently to the endothelium, detach and bind again, thus rolling on the vessel wall.
- Cells come to rest at some point where they adhere firmly.
- Rolling interactions are mediated by selectins {leukocytes (L-selectin), endothelium (E-selectin), and on platelets and endothelium (P-selectin)}
- Selectins and their ligands are regulated by tumor necrosis factor (TNF), IL-1, and chemokines
- Integrins: Bring firm adhesion of leucocytes on the endothelium
Integrins:
- Vascular cell adhesion molecule-1 (VCAM-1), the ligand for the β1 integrin VLA-4
- Intercellular adhesion molecule-1 (ICAM-1), the ligand for the β2 integrins LFA-1 and Mac-1
2. Leukocyte migration through endothelium
- Transmigration or diapedesis: Migration of the leukocytes through the endothelium
- CD31 or PECAM-1 (platelet endothelial cell adhesion molecule) is involved in the migration of leukocytes
3. Chemotaxis of leukocytes
- Leukocytes migration in the tissues toward the site of injury is called chemotaxis
Chemo attractants
- Exogenous: Bacterial products
- Endogenous: IL-8, C5a and leukotriene B4 (LTB4)
Defective leukocyte function
1. Leukocyte adhesion deficiency type 1:
- Due to a defect in the biosynthesis of the β2 chains shared by the LFA-1 and Mac-1 integrins
2. Leukocyte adhesion deficiency type 2:
- Due to the absence of sialyl-Lewis X, the fucose-containing ligand for E- and P-selectins
Question 2. Write a note on phagocytosis.
Answer:
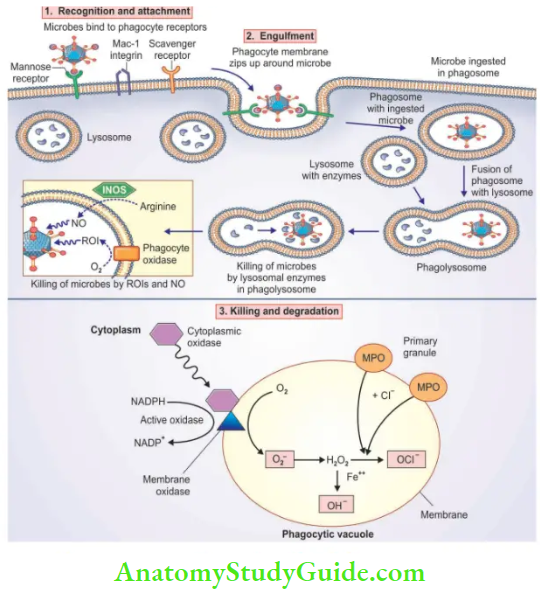
Three steps of phagocytosis
1. Recognition and attachment of the particle to be ingested by the leukocyte
- Is done by phagocytic receptors on the leukocyte surface
2. Engulfment
- Pseudopods (extensions of the cytoplasm) flow around the particle, resulting in the formation of a phagosome, that encloses the particle
- Phagosome fuses with lysosome, resulting in the formation of phagolysosome and there occurs the release of lysosomal enzymes
3. Killing or degradation of ingested material is brought about by
- Lysosomal enzymes, reactive oxygen species (ROS, also called reactive oxygen intermediates), and reactive nitrogen species, derived from nitric oxide (NO). The mechanism by which reactive oxygen species are generated:
- The generation of ROS is due to NADPH oxidase (phagocyte oxidase), which oxidizes NADPH and, in the process, reduces oxygen to superoxide anion (O2–).
- Respiratory burst: Rapid oxidative reaction, in neutrophils
- O2is converted into hydrogen peroxide (H2O2)
- H2O2, in the presence of the enzyme myeloperoxidase (MPO), combines with Cl–, converting H2O2 to hypochlorite (OCl–)
- HOCl is a potent antimicrobial agent that destroys microbes
- H2O2-MPO-halide system: A most efficient bactericidal system of neutrophils
- H2O2 is converted to hydroxyl radical (OH–), another powerful destructive agent
- NO reacts with superoxide (O2) to generate highly reactive free radical peroxynitrite (ONOO–), which brings microbe destruction.
Note:
Reactive oxygen species are neutralized by antioxidants including superoxide dismutase, catalase, glutathione peroxidase, ceruloplasmin, transferrin
Question 3. Write a note on chemical mediators in acute inflammation. Discuss the role of arachidonic acid metabolites in inflammation.
Answer:
Chemical mediators in acute inflammation:
1. Histamine
The release is stimulated by
- Physical injury, such as trauma, cold, or heat
- Binding of antibodies to mast cells (immediate hypersensitivity reactions)
- Products of complement called anaphylatoxins (C3a and C5a)
Actions of histamine
Arteriolar dilation, increased permeability of venules, smooth muscle contraction
2. Serotonin (5-hydroxytryptamine)
Acts as a neurotransmitter in the gastrointestinal tract
Present in platelets
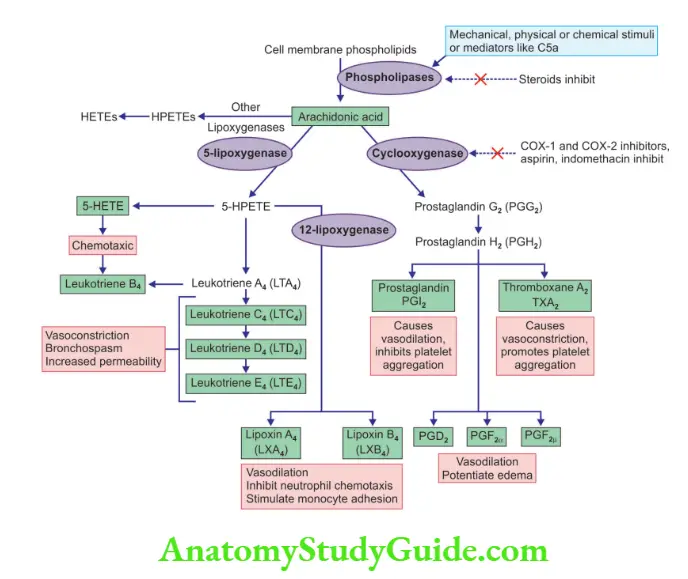
3. Arachidonic acid and its metabolites
Arachidonic acid (AA)
Normally present in membrane phospholipids, and is released by the action phospholipase A2
AA-derived mediators are synthesized by cyclooxygenases (which generate prostaglandins) and lipoxygenases (which produce leukotrienes and lipoxins)
1. Prostaglandins
- Produced by mast cells, macrophages, endothelial cells
- Generated by the action of cyclooxygenase-1 and cyclooxygenase-2
- Includes PGE2, PGD2, PGF2, PGI2 (prostacyclin), and TxA2 (thromboxane A2)
2. Leukotrienes
- Derived by the action of lipoxygenases enzymes
5-lipoxygenase
- Predominantly seen in neutrophils
- Converts arachidonic acid to 5-hydroxyeicosatetraenoic acid, the precursor form of leukotrienes
- LTB4 is a potent chemotactic agent and activator of neutrophils
- LTC4, LTD4, and LTE4 cause intense vasoconstriction, bronchospasm
3. Lipoxins
- Generated from AA by 12-lipoxygenase pathway
- Suppress inflammation by inhibiting the recruitment of leukocytes
Question 4. Write a short note on chemokines.
Answer:
Chemokines
Acts as chemoattractants for leukocytes.
Classified into four major groups
1. C-X-C chemokines (α chemokines)
- Responsible for chemotaxis of neutrophils
- Secreted by activated macrophages, endothelial cells
- IL-8 is typical of this group
2. C-C chemokines (β chemokines)
- Attract monocytes, eosinophils, basophils, and lymphocytes
- Include monocyte chemoattractant protein (MCP-1), eotaxin, macrophage inflammatory protein-1α (MIP-1α), and RANTES
- Eotaxin selectively recruits eosinophils
- 3. C chemokines (γ chemokines)
- Includes lymphotactin which is specific for lymphocytes
4. CX3C chemokines
- For example, fractalkine
- Promotes strong adhesion of monocyte and T-cells
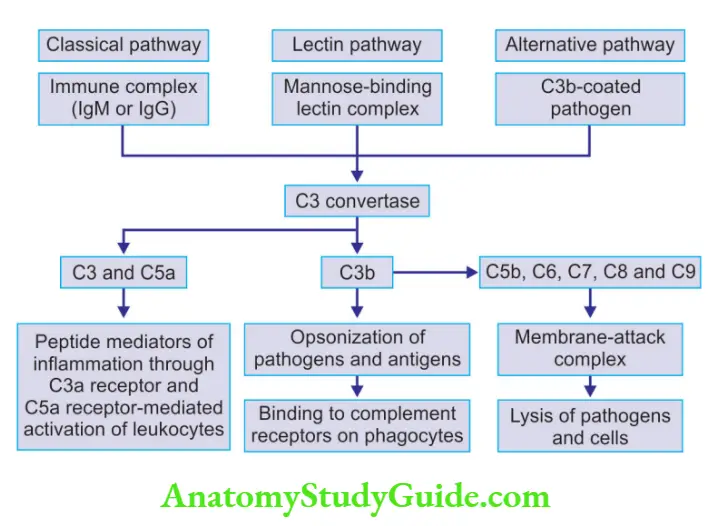
Question 5. Mention functions of the complement pathway system.
Answer:
Functions of the complement system
1. Inflammation
- C3a and C5a are called anaphylatoxins because they stimulate histamine release from mast cells
- Powerful chemotactic agent for neutrophils, monocytes, eosinophils, and basophils
2. Phagocytosis: C3b, acts as opsonins and promotes phagocytosis by neutrophils and macrophages
3. Cell lysis: Deposition of membrane attack complex (MAC) on the cells results in
the death of the image of the cells
Question 6. Write a short note on granulomatous inflammation.
Answer:
Granulomatous inflammation
- Chronic inflammation, characterized by a collection of activated macrophages, T lymphocytes, and central necrosis
- Epithelioid cells: Activated macrophages with abundant cytoplasm
- Multinucleate giant cells: Fusion of activated macrophages
Morphology
- Tuberculous granuloma has an area of central necrosis surrounded by multiple Langhans-type giant cells, epithelioid cells, and lymphocytes
- The central zone of necrosis (caseous necrosis) occurs due to hypoxia and free radical-mediated injury
- Can be seen in tuberculosis, sarcoidosis, cat-scratch disease, lymphogranuloma inguinal, leprosy, brucellosis, syphilis, mycotic infections, Berylliosis, and reactions of irritant lipids.
Question 7. Discuss systemic effects of inflammation. Add a note on acute phase proteins.
Answer:
Acute-phase response
- Systemic changes associated with acute inflammation.
Features of acute-phase response:
1. Fever: TNF and IL-1 stimulate the production of prostaglandin in the hypothalamus.
2. Elevated acute phase proteins:
- For example C-reactive protein (CRP), fibrinogen, serum amyloid A (SAA) protein
- Fibrinogen binds to red cells and causes them to form stacks (rouleaux), that sediment more rapidly and form the basis for measuring erythrocyte sedimentation rate
- Prolonged production of SAA in chronic inflammation causes secondary amyloidosis
- Elevated CRP levels are a marker of increased risk of myocardial infarction in patients with coronary artery disease
- Elevated hepcidin (acute phase reactant) level is responsible for anemia associated with chronic inflammation
3. Leukocytosis:
Neutrophilia—seen in bacterial infections
Lymphocytosis—seen in viral infections (infectious mononucleosis)
Eosinophilia—seen in allergies and parasitic infestations
Leukopenia—seen in typhoid fever, viral, rickettsial, and protozoal infections
Note:
Mediators of an acute-phase reaction include TNF, IL-1, IL-6, type I interferon
Question 8. Describe various stages of repair and healing and their abnormalities.
Answer:
Healing of skin wounds
1. Healing by first intention or primary union:
Occurs in the following circumstances:
- When the injury involves only the epithelial layer, epithelial regeneration is the principal mechanism of repair.
- Healing of a clean, uninfected surgical incision approximated by surgical sutures
Changes brought about in the tissue include:
- Within 24 hours: Neutrophils accumulate at margins
- Between 24–72 hours: Granulation tissue is formed
- Between 48–96 hours: Neutrophils are replaced by macrophages
- End of the first month: Scar formation
2. Healing by the second intention or by the secondary union:
- Seen in large wounds, abscesses, ulceration, and infarction involving parenchymal organs
- The repair process involves a combination of regeneration and scarring
- Much larger granulation tissue is formed
- Wound contraction is brought about by myofibroblasts
Abnormalities in tissue repair include:
- Wound dehiscence and ulceration: Inadequate formation of granulation tissue or a scar
- Hypertrophic scars and keloids: Excessive formation of components of the repair
- Contractures: Seen on palms, soles, and anterior aspect of thorax, after serious burns
- Exuberant granulation tissue (proud flesh)
Question 9. Discuss the factors influencing wound healing.
Answer:
Factors that influence tissue repair
1. Local factors:
- Infection: A most important cause of delay in healing
- Mechanical factors: Early motion of wounds and increased local pressure, delay wound healing
- Foreign bodies: Sutures, steel, glass, and bone can impede healing
- Size, location, and type of wound: Highly vascularized tissues heal faster
2. Systemic factors:
- Diabetes: Results in impaired wound healing
- Nutritional status: Vitamin C deficiency inhibits collagen synthesis
- Glucocorticoids (steroids): Weakens the scar due to inhibition of TGF-β
- Poor perfusion: Due to arteriosclerosis and diabetes, impairs wound healing
Question 10. Discuss the role of vitamin C in wound healing.
Answer:
Vitamin C
- Results in activation of prolyl hydroxylases and lysyl hydroxylases from their inactive precursors, and the resultant hydroxylation of procollagen
- Deficiency results in weak collagen chains
- Weak collagen chains are inadequately cross-linked, lack tensile strength, and are more soluble and vulnerable to enzymatic degradation
- As a result, there occurs impaired collagen formation, which brings about:
- Increased bleeding tendency
- Inadequate synthesis of osteoid
- Impaired wound healing
Leave a Reply