Injuries to the Supporting Bone Introduction
Orofacial trauma can be explained under three main categories, namely injury to the soft tissues, injury to the supporting bone, and injury to teeth.
Table of Contents
Of the three, soft tissue injuries have been while injuries to teeth.
Traumatic injuries to the supporting bone are of four types, which are as follows:
1. Comminution of the alveolar socket
2. Fracture of the alveolar socket wall
- Facial wall involvement
- Lingual wall involvement
Read And Learn More: Paediatric Dentistry Notes
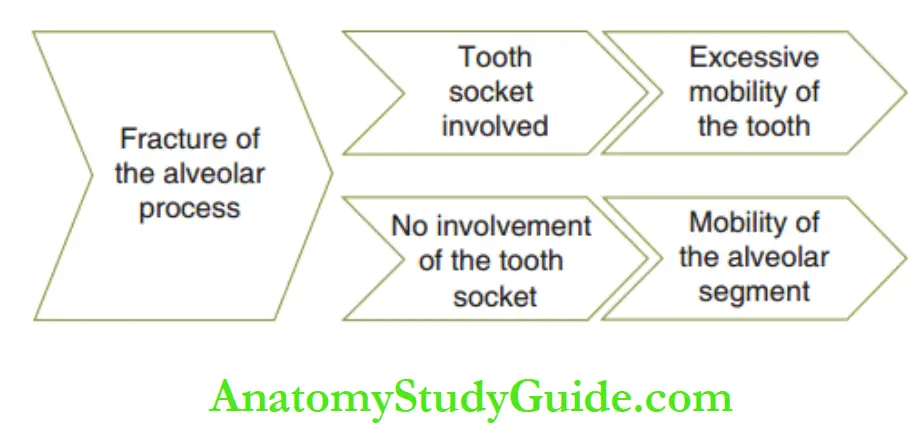
3. Fracture of the alveolar process
- With the involvement of the alveolar socket
- Without the involvement of the alveolar socket
4. Fracture of the basal jaw bone (maxilla or mandible)
- With the involvement of the alveolar socket
- Without the involvement of the alveolar socket
Comminution Of The Alveolar Socket
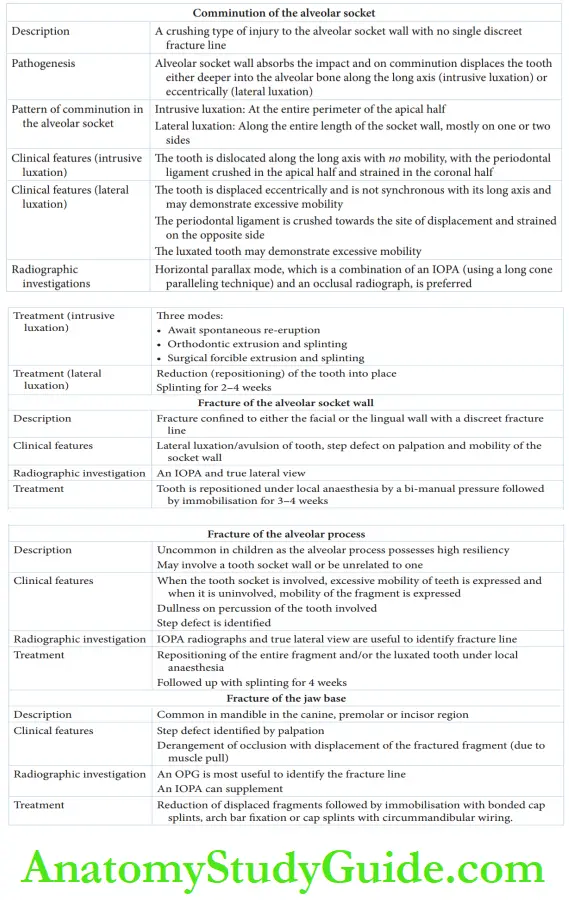
Comminution is a crushing type of injury to the alveolar socket wall with no single discreet fracture line.
The alveolar socket wall absorbs the impact and on comminution displaces the tooth resulting in a luxation injury of the tooth.
Clinical Features
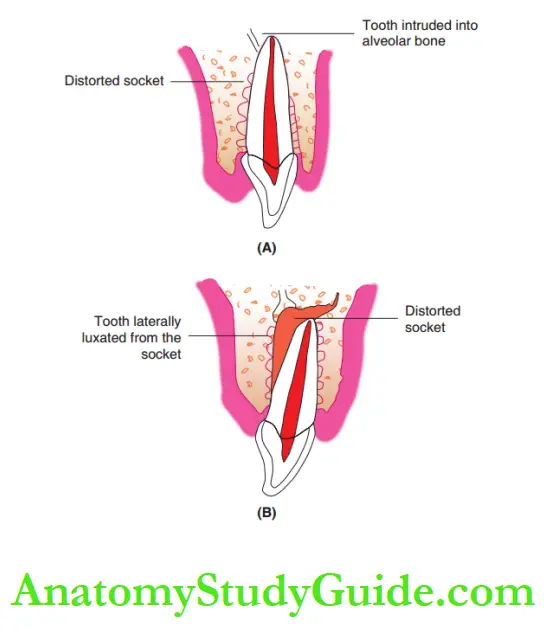
Two patterns of luxation injuries may be noted, namely intrusive luxation and lateral luxation.
The supporting bone is usually not affected in the case of extrusive luxation.
1. Intrusive luxation: Comminution of the alveolar socket involves the entire perimeter of the apical half of the tooth and is associated with the displacement of the tooth deeper into the alveolar bone.
The direction of tooth dislocation is along the long axis of the tooth.
The periodontal ligament is crushed in the apical half and strained in the coronal half. An intruded tooth expresses no mobility.
2. Lateral luxation: Comminution of the alveolar socket is along the entire length of the socket wall, mostly on one or two sides.
The tooth is displaced eccentrically and is not synchronous with its long axis.
For instance, the fracture of the facial and mesial portions of the socket wall involving the entire length of the tooth results in mesiofacial lateral luxation.
The periodontal ligament is crushed towards the site of displacement and strained on the opposite side.
A luxated tooth may demonstrate excessive mobility.
Radiographic Investigation:
An IOPA radiograph can essentially be useful for the localization of displaced teeth.
A parallax method comprising one vertical view and one horizontal view(IOPA and occlusal) can localize the displaced tooth accurately.
Th long-cone paralleling technique with a film holder is preferred as the injured site need not be disturbed by the film.
Treatment:
The treatment is described separately for intrusive luxation and lateral luxation.
Intrusive luxation: Th tooth that has undergone intrusive luxation needs emergency symptomatic treatment comprising relief of any eccentric occlusal contact.
Anti-inflammatory drugs are prescribed to relieve associated periodontal concussions.
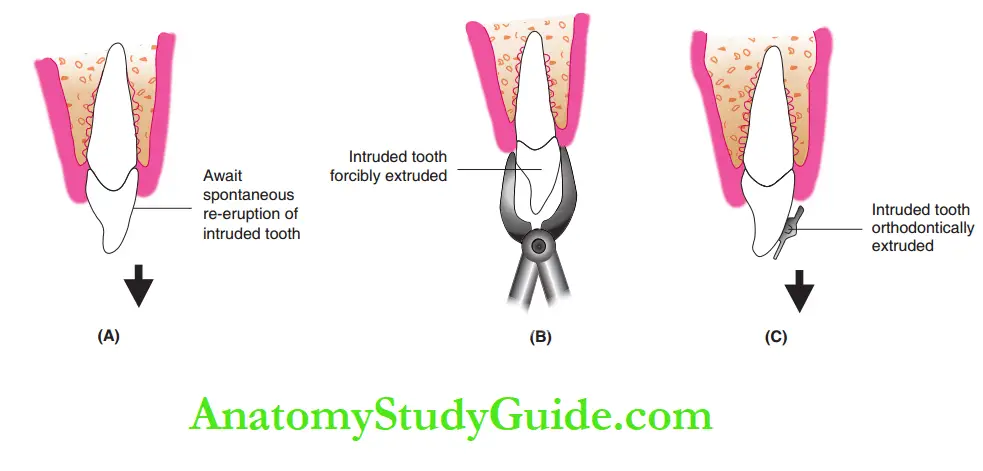
The definitive therapy consists of three modes, which are as follows:
Await spontaneous re-eruption: An intruded tooth may be considered as a quick orthodontic movement with no retention.
Spontaneous re-eruption may be possible with a reorganization of the periodontal ligament fires.
Complete re-eruption may be expected in 6–12 weeks.
Forcible extrusion: The involved tooth may be held with forceps and forcibly extruded to place.
It may then need splinting for 4 weeks. However, forcible extrusion has the risk of iatrogenic extrusion, that is, extraction.
Orthodontic extrusion: It involves the delivery of an orthodontic force of magnitude 75–125 g by the mode of brackets bonded to the intruded tooth.
The most preferable or suggested treatment plan is to await spontaneous re-eruption in 6–12 weeks.
On no demonstrable desired re-eruption, an orthodontic extrusion is performed.
2. Lateral luxation: The treatment of laterally luxated tooth involves two steps:
Repositioning: Reduction of the displaced tooth back to its position is done under local anesthesia by bi-digital pressure application at the apex and at the cervix on opposite sides with the thumb and/or index finger.
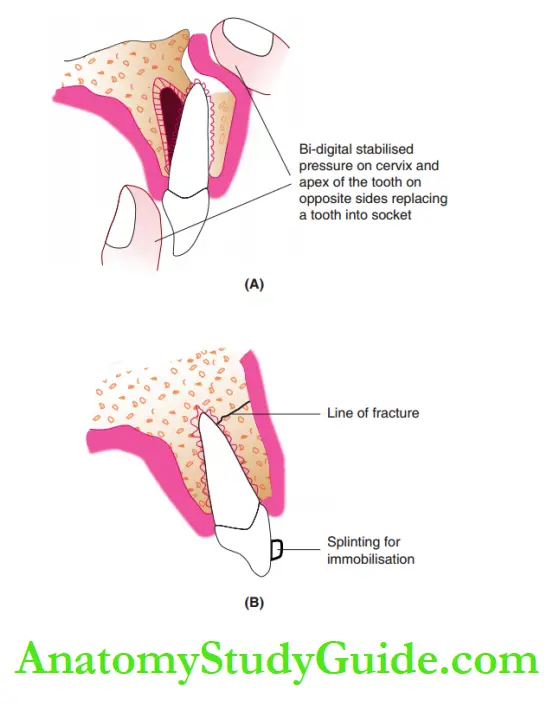
The patient has to be instructed to restrict eating hard/firm food for 2 weeks.
The various splints commonly used for lateral luxation are as follows:
Wire and composite splints: A 19-gauge stainless steel wire is adapted over the repositioned tooth and over at least two non-traumatized teeth on each side.
The wire is then bonded to the teeth with light-cured composite resin.
Glass fire splints: Glass fire cores are more flexible and transparent.
They are adapted over the traumatized as well as over two uninvolved teeth on each side and bonded with light-cured composite resin.
Acrylic cap splints: When sufficient uninvolved teeth are not available to deliver anchorage for splinting, an acrylic cap splint may be preferred.
An impression is made with a thin mix of alginate. The cervical and interdental undercuts are blocked on teeth.
An acrylic cap splint of 2 mm thickness is fabricated.
The splint may be bonded with zinc oxide eugenol zinc polycarboxylate cement.
The barrier to the maintenance of good oral hygiene, occlusal interference, and the inability to note color changes on traumatized teeth are the limitations of a cap splint.

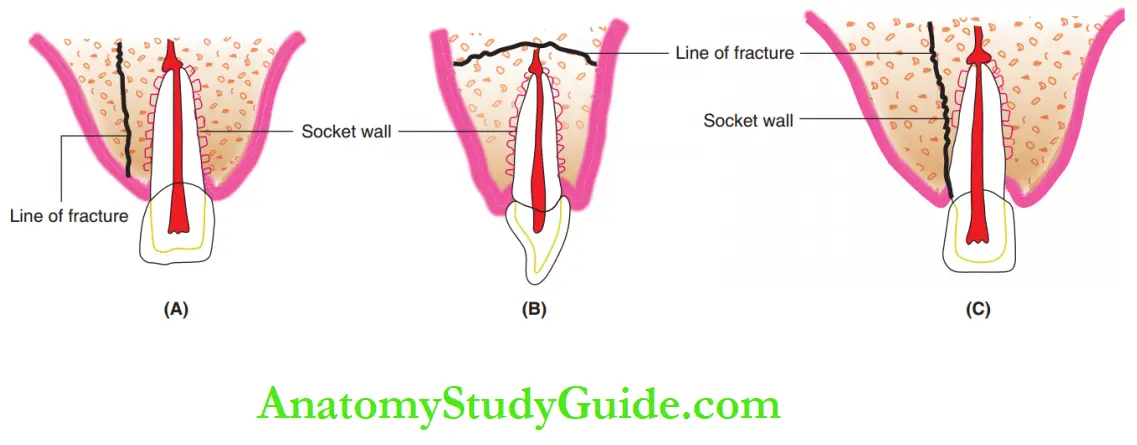
Fracture Of The Alveolar Socket Wall
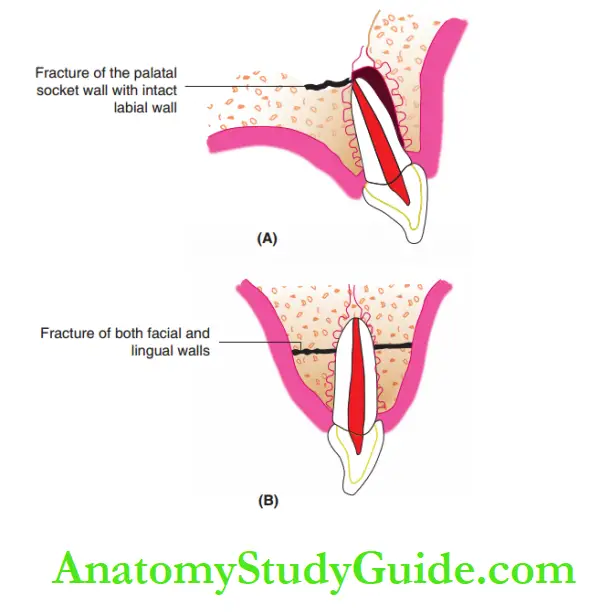
Fractures of the alveolar socket wall may be confined to either the facial (buccal) or the lingual (palatal) wall.
It demonstrates a single discreet fracture line and is commonly observed in the maxillary incisor region.
Clinical Features:
The injury demonstrates a lateral luxation of the tooth or an avulsion injury.
A step defect is identified by palpation at the site of the fracture line.
The mobility of the socket wall is evident. The fracture line may extend to involve several teeth also.
Radiographic Investigations:
The fracture line may not be identified with an IOPA radiograph. An extraoral true lateral view radiograph can disclose the fracture line in the socket wall.
Treatment:
The displaced tooth is reduced (repositioned) under local anesthesia by bi-digital stabilized pressure.
The reduction has to be followed by immobilization through splinting (explained earlier).
Post-operative instruction of restricting hard/firm food for 2 weeks has to be emphasized.
Fracture Of The Alveolar Process
Fracture of the alveolar process is relatively uncommon in children.
It is common in the older age group. The resiliency of the alveolar process decreases with age, making it increasingly susceptible to fracture.
Clinical Features:
When the fracture of the alveolar process involves the tooth socket wall, the tooth may demonstrate lateral or extrusive luxation and excessive mobility.
When the socket wall is uninvolved, the entire fractured alveolar segment expresses mobility.
An effort to move a single tooth in the fragment moves the entire segment.
Percussion of the teeth in the fragment causes a distinctly dull sound.
The fractured fragment is usually displaced with a clear step defect, which is identified on palpation.
Radiographic Investigations:
Fractures of the alveolar process can be identified on both an IOPA radiograph and an extraoral true lateral radiograph.
However, when the fracture line seems to be superimposed on a tooth root, it may be confused with a tooth fracture.
Treatment:
Treatment involves reduction (repositioning) of the displaced fragment under local anesthesia.
When individual teeth are displaced, repositioning is carried out by selective pressure application (as explained earlier).
When the reduced (repositioned) fragment is stable,
immobilization is not necessary.
Else, immobilization can be carried out with wire–composite or acrylic-bonded cap splints.
The period of immobilization is usually 4 weeks. It is reduced to a shorter time in younger children.
Diet is restricted to soft food during this period.
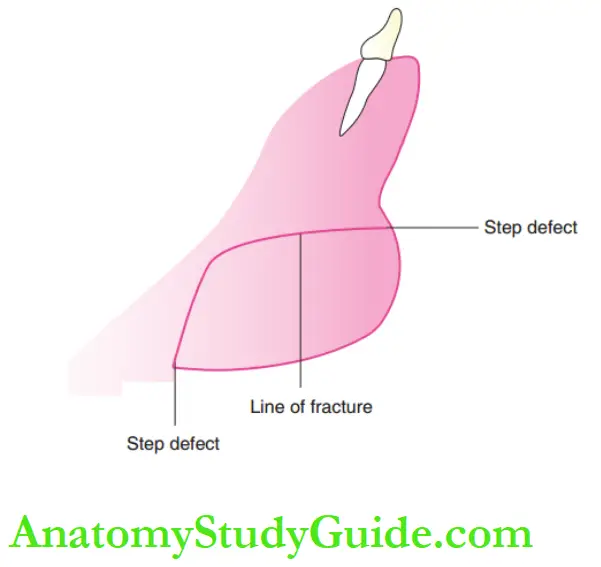
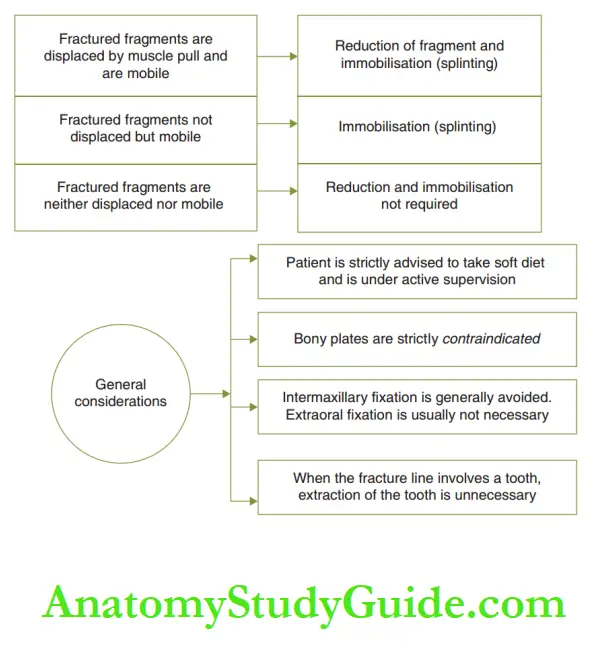
Fracture Of The Basal Jaw Bone (Maxilla/Mandible)
Cortical plates are not distinct in the maxilla as in the mandible, so fracture of the basal jaw bone is only possible in the mandible. It includes the teeth in the line of fracture.
Mandibular canines, premolars, and incisor regions are the commonly associated sites in the order of decreasing frequency.
Clinical Features:
Jaw fractures are associated with derangement of occlusion and displacement of fractured fragments due to muscle pull.
A step defect is clearly demonstrable intraorally as well as extraorally.
Whenastep defect is not evident, bimanual palpation expresses mobility between the fragments, associated with crepitus.
Pain provoked by the movement of the jaw bone or with palpation also confirms a jaw fracture.
Ecchymosis is noted intraorally at the line fracture.
Radiographic Investigations:
An OPG is the most valuable view for the diagnosis of a fracture site.
An IOPA radiograph clearly reveals the position of a tooth involved in the fracture line.
It is more useful than the OPG for a fracture of the maxilla.
In an IOPA, when the central beam is not exactly over the fracture line, it may show as two fracture lines, one line indicating the outer and the other indicating the inner cortical plate.
Treatment:
The treatment protocol When immobilization is required, it is accomplished with an arch bar fixation, bonded cap splints, or cap splints with curcumin and tabular wiring.
Bony plates are strictly contraindicated as they pose a possible risk of damage to the developing tooth buds or to the erupting tooth roots.
Intermaxillary fixation is generally avoided as it is a profound barrier to good oral hygiene maintenance and adequate nutrition.
Extraoral fiction is usually not necessary.
Recent studies point out that when the fracture line involves a tooth, extraction of the tooth becomes unnecessary if prompt reduction and immobilization are carried out.
Outcome And Prognosis:
Injuries to the supporting bone with non-displaced fragments or displaced fragments, which are reduced and immobilized, usually heal uneventfully.
The younger the child, the higher the inflammatory response and the quicker the healing.
The teeth involved with displacement (intrusion, extrusion, and lateral luxation) may undergo pulpal necrosis, pulp canal obliteration, and internal or external root resorption.
The ongoing pathologic sequence exhibits discoloration or increased mobility of teeth and radiographic signs.
The teeth may appropriately be treated by pulpectomy followed by conventional obturation with gutta-percha in a permanent tooth with complete root formation.
Obturation with calcium hydroxide and CMCP mixture or MTA is done in a primary tooth or in a permanent tooth with incomplete root formation.
Odontogenic disturbances are reported on developing teeth that lie in the site/line of fracture.
Summary
1. Traumatic injuries to the supporting bone are four types:
2. Outcome and prognosis: Injuries to the supporting bone usually heal quickly with a higher inflammatory response.
The teeth involved with displacement may undergo pulpal necrosis, pulp canal obliteration, and internal or external
root resorption.
Odontogenic disturbances are reported on developing teeth that lie in the site/line of fracture.
Leave a Reply