Interceptive Orthodontics Introduction
Interceptive orthodontics is described as the art and science of orthodontics employed to recognise and eliminate potential irregularities and malpositions of the developing dentofacial complex.
Table of Contents
Paediatric dental surgeons have excellent opportunities to detect these minor irregularities in the dentition as they walk the child from deciduous dentition through mixed dentition to permanent dentition.
The irregularities in the developing dentition can be broadly classified as inter-arch discrepancies and intra-arch discrepancies.
Inter-arch discrepancies involve a mismatch of the maxillary and mandibular arches, while intra-arch discrepancies are problems that exist within one arch.
Early detection and intervention of such discrepancies solve many complexities of the erupting dentition.
Read And Learn More: Paediatric Dentistry Notes
The procedures that detect and interrupt the developing minor irregularities of the erupting dentition are called interceptive orthodontic procedures.
These procedures guide a tooth into an ideal position as and when the tooth erupts and moves towards the occlusal plane.
Interceptive measures are corrective procedures performed upon witnessing any faint symptom or sign of deviation.
On the other hand, preventive orthodontic procedures, are indicated before actual damage occurs.
These interceptive orthodontic procedures are a continuation of preventive orthodontic procedures.
The complications are reduced to a large extent, if not eliminated.
A need for future orthodontic mechanotherapy is however not to be ruled out.
Orthodontic mechanotherapy involving removable appliances for simple correction and fixed appliances for precise positioning of crowns/roots may be indicated later.
Inter-Arch Discrepancy
A harmonious relationship exists between the maxilla and mandible only when their sizes, shapes and spatial positioning are coordinated.
Inter-archmalrelationships are the discrepancies between maxillary and mandibular counterparts.
They include crossbites and developing skeletal class II or class III malocclusions.
Crossbite
The maxillary arch is normally larger than the mandibular arch. So, the facial or buccal surface of the maxillary teeth lies outside when compared to their mandibular counterparts.
The buccal cusps of mandibular posterior teeth occlude in the central groove of the maxillary posterior teeth.
A crossbite is said to occur when the maxillary teeth are inside or more palatal to the mandibular teeth.
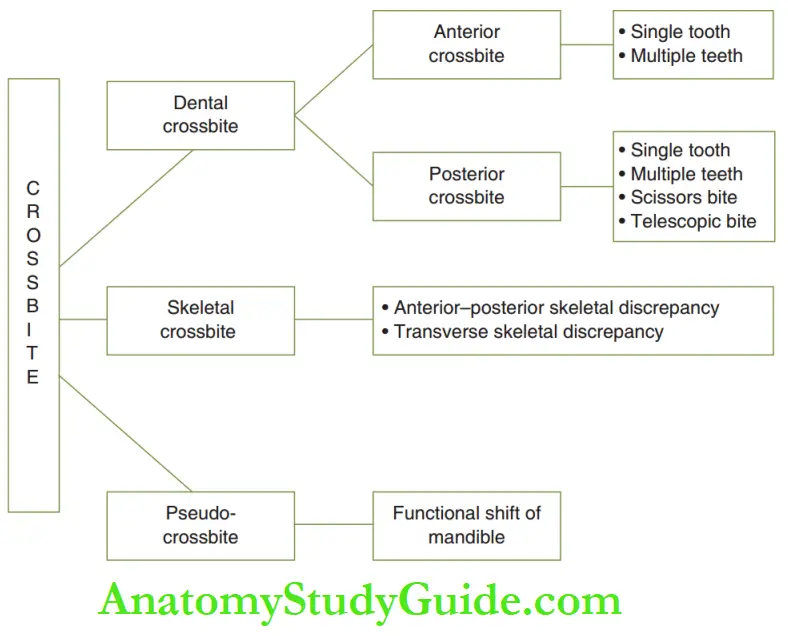
Crossbites can be classified, according to aetiology, such as dental crossbite, skeletal crossbite and pseudo-crossbite.
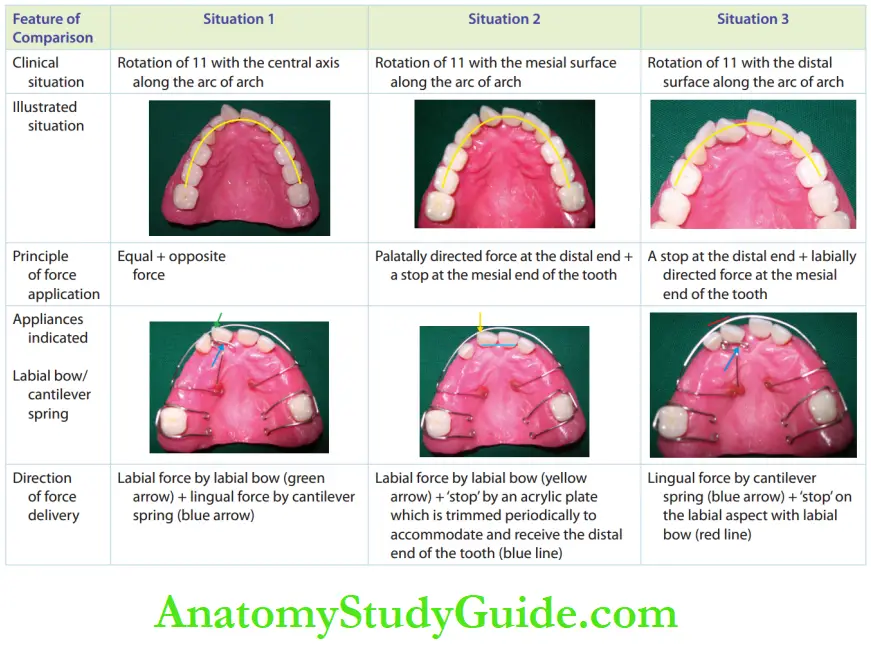
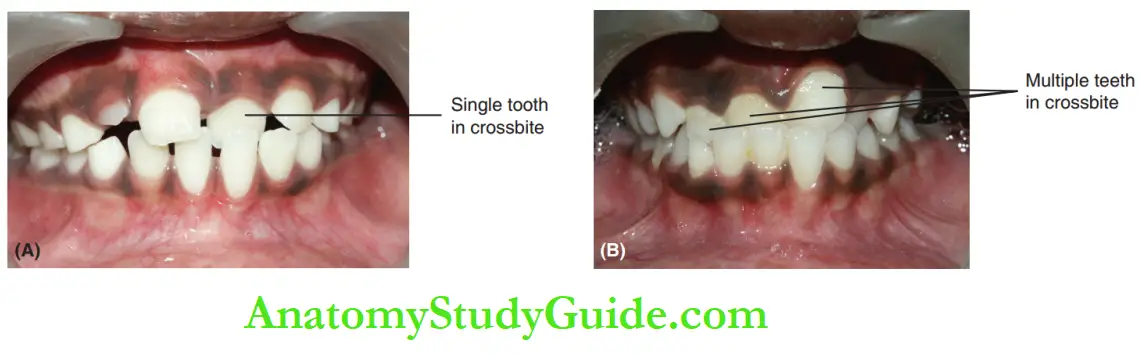
Dental crossbites can be further divided into anterior and posterior crossbites. The classituation of crossbite.
Dental Anterior Crossbite
The maxillary anterior teeth vertically overlap the mandibular anterior teeth by about 2–4 mm in normal occlusion.
This is described as an overbite. Dental anterior crossbite is a condition where the maxillary anterior teeth are locked behind the mandibular anterior teeth.
A reverse overbite exists as the mandibular anterior teeth overlap the maxillary anterior teeth.
There is no discrepancy in the size and position of the maxilla and mandible.
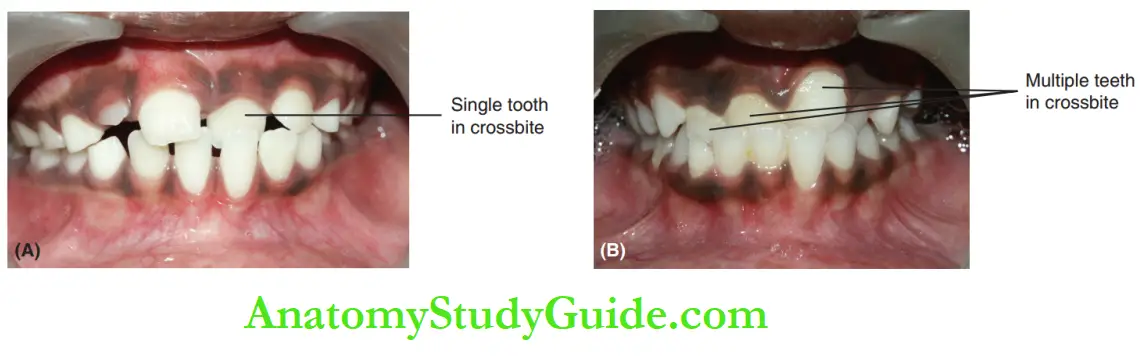
Dental anterior crossbite occurs due to the altered eruption path of teeth, over-retained primary teeth, lack of space for the eruption of permanent teeth ectopic eruption associated with supernumerary teeth. It may involve a single tooth or multiple teeth.
Dental Anterior Crossbite Management
Pre-correction evaluation is required to identify the aetiology of the crossbite and eliminate the same.
The level of the eruption of the tooth in question is assessed. This denotes the extent of overbite to be corrected to allow movement of the maxillary tooth locked behind the mandibular tooth.
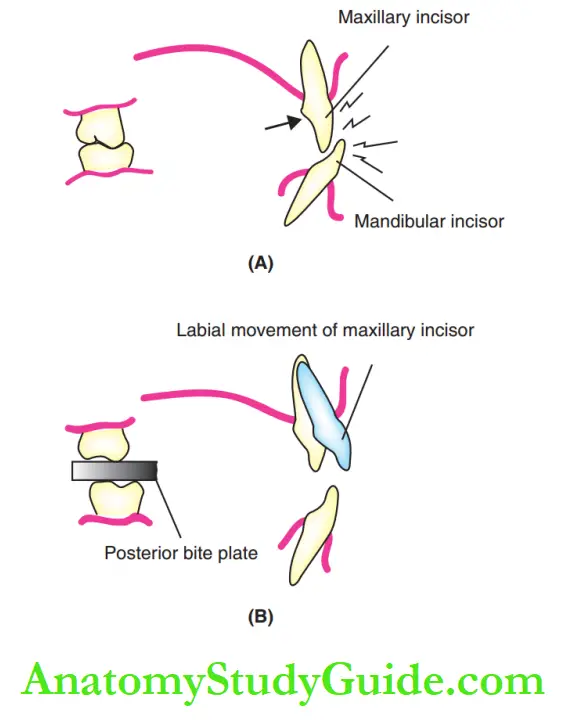
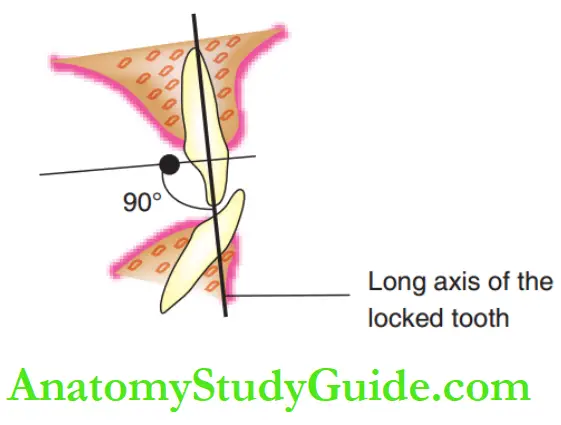
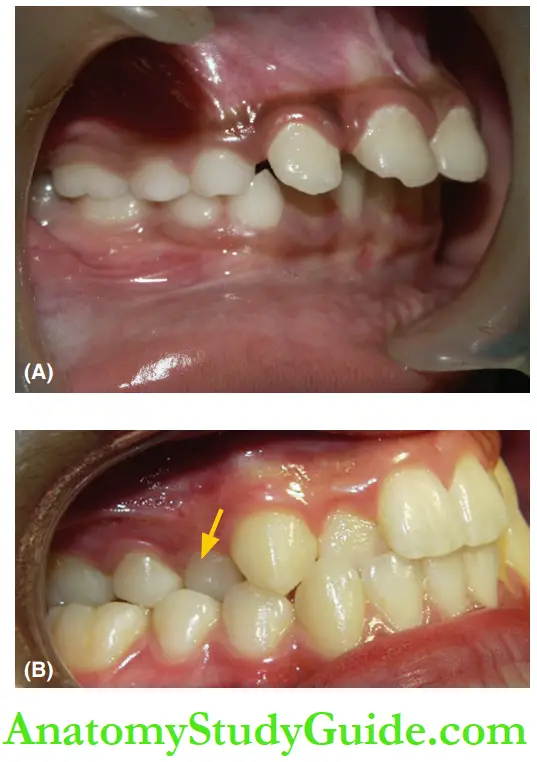
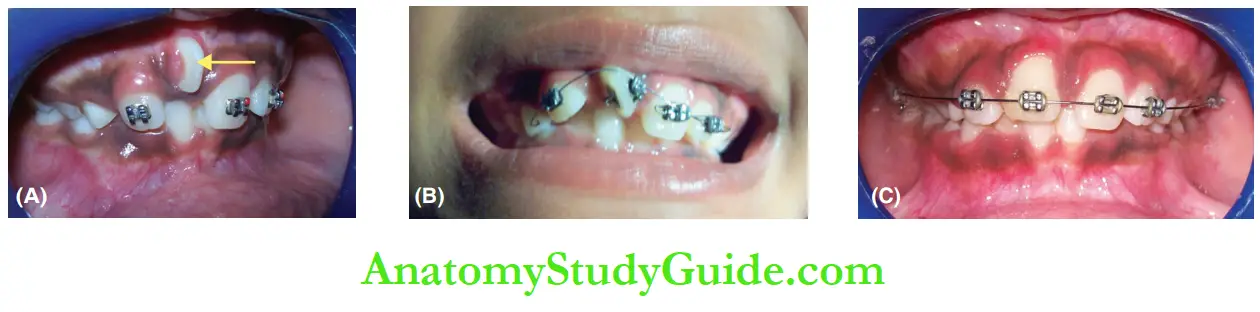
illustrates a typical case of anterior crossbite where the maxillary incisor is locked behind the mandibular incisor.
Attempts made to move the locked incisor will injure the upper and lower incisors.
In such a case, a posterior bite plate is incorporated temporarily to open the bite.
This allows the labial movement of the locked maxillary incisor.
Two modes of force may be applied for the correction of anterior crossbite.
A push type of force can be exerted from behind the locked tooth. The vector of this force is directed, forwards.
An inclined plane principle is beneficial when the resultant vector is preferred in a downward and forward direction.
The appliance is indicated according to the desired displacement for correction.
1. Push type of force: This is ideally applied perpendicular to the long axis of the locked tooth by active components such as screws or springs.
The point of application of force should be constant. The active components are incorporated into an acrylic plate to deliver the pushing force.
It is important that the appliance is anchored fim, to withstand reactive forces.
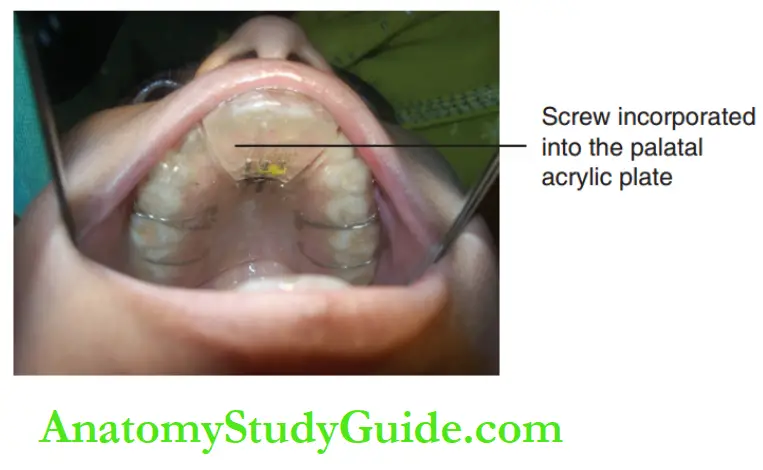
Screws: A slow expansion screw is used for the correction of anterior crossbite.
The manufacturer supplies a Key along with the screw. The screw is incorporated into a palatal acrylic plate and activated periodically using the provided key.
When activated, the screw expands and pushes the locked teeth outwards to correct the crossbite.
Posterior bite plates are often required to release the lock of occlusion and allow anterior teeth to move forwards.
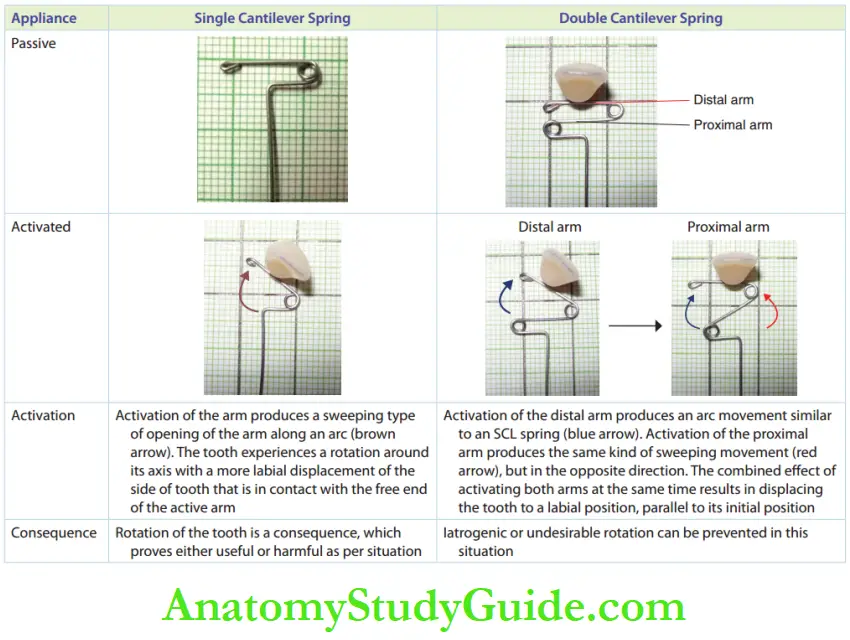
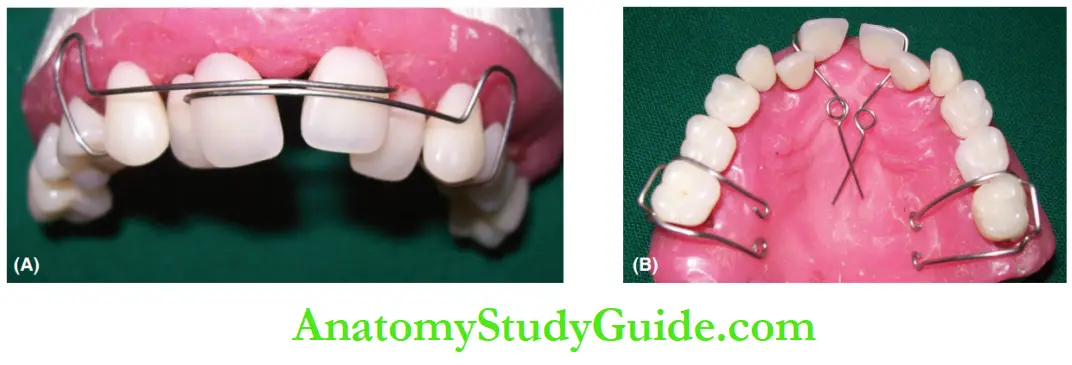
Springs: Springs such as single cantilever springs (SCL) and double cantilever springs (DCL) are used to exert force on the palatal surface of the tooth in crossbite.
On activation of the spring, the tooth is pushed outwards to correct the crossbit the mechanism of activation of the SCL and DCL.
The duration of wear of the springs or screws depends on the severity of the problem and the patient’s cooperation.
Two or three weeks of appliance wear is sufficient for the correction of anterior crossbite in a cooperative patient.
No special appliance is required to retain the changes achieved on the correction of crossbite.
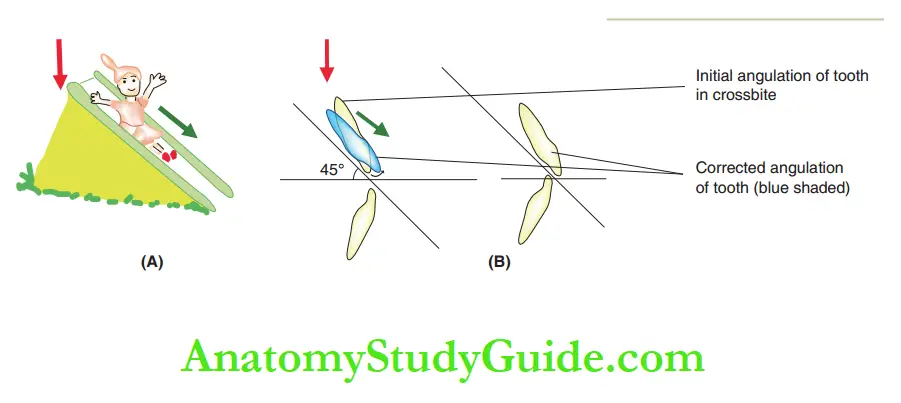
2. Inclined plane principle: Force applied vertically down on an inclined plane gets redirected to vertical and horizontal planes.
The Steepness of the inclined plane decides the magnitude of the vertical or horizontal component of the vector.
In the same principle, an inclined plane appliance slides the tooth downwards and forwards, thus correcting the anterior crossbite.
The inclined plane concept can be applied by tongue blade therapy and Catalan’s appliance.
Other designs suggested are steel crowns with occlusal extension or composite build-up on the incisal aspect.
Tongue blade therapy: This is indicated for a single anterior tooth that can possibly erupt in crossbite.
The therapy has to be initiated when one-fourth of the tooth has erupted and is yet to be locked behind the lower incisor.
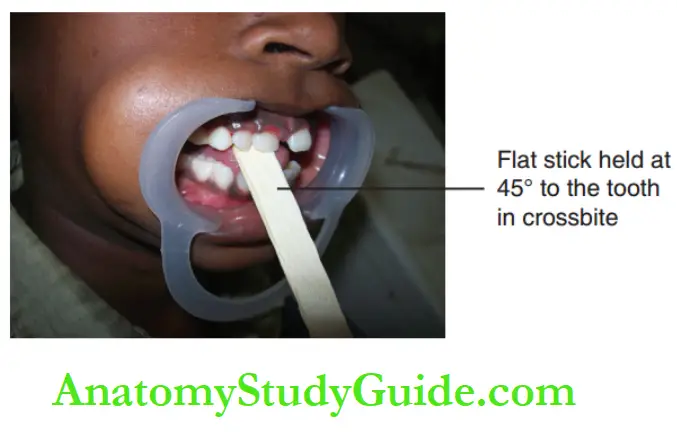
The tongue blade is a flat stick held at 45° to the tooth in crossbite.
The child is instructed to gently bite on it. The stick is tipped outwards with the lower incisors as a fulcrum.
The action is performed 20–30 times, twice per day for 2–3 weeks.
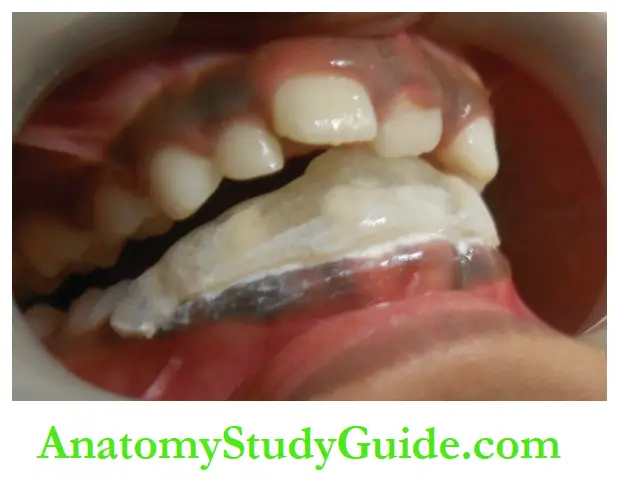
Catalan’s appliance/inclined plane appliance: This is indicated in the same situation as the previous appliance.
The difference is that the therapy is initiated when nearly half of the tooth has erupted and is yet to be locked behind the lower incisor.
An acrylic cap-like covering is provided on all the lower incisors with an incline extending occlusal and lingually at 45° to the occlusal plane.
This delivers a forward and downward force on the tooth in crossbite.
The load is distributed to all the capped teeth so that the appliance does not injure any tooth or ginger va.
It involves full-time wear as it is cemented. Demonstrable change is noted within 7–10 days.
Apart from the types of forces and appliances discussed earlier, the following points have to be remembered in the management of anterior crossbite:
- Patient cooperation and motivation are the starting lines of treatment.
- Mesiodistal space availability in the arch is essential for correction.
- Bite opening has to be done to allow forward movement.
- Lower teeth should be healthy to withstand fulcrum load.
- Too early movement of the tooth in question can shorten root development.
- Excessive force has to be avoided as it damages the young permanent teeth.
- Holding the appliance longer than necessary creates an iatrogenic anterior open bite.
- Future torquing of the concerned tooth may be necessary.
- No retention appliance is required to maintain a corrected crossbite.
Dental Posterior Crossbite
Dentalposteriorcrossbiteis a condition where maxillary posterior teeth are located palatal to their mandibular counterparts.
A posterior crossbite occurs due to lack of space, over-retained deciduous teeth or premature loss of primary teeth.
A posterior crossbite can be unilateral or bilateral.
A scissors bite is a variant of posterior crossbite that reveals a severe transverse deficiency of the lower arch.
The blades of scissors move in close proximity to each other. Yet they never come into direct contact.
Similarly, the upper posterior teeth lie entirely outside the lower posterior teeth.
The palatal surfaces of all the upper posterior teeth are positioned buccally to the buccal surfaces of all the lower posterior teeth.
Such a relationship is called ‘scissors bite’.
Telescopic bite is a rare condition that reveals a more severe transverse deficiency than a scissors bite.
The upper arch completely surrounds and overlaps the lower arch and slides like the rings of the telescope.
Management
Posterior crossbite may involve a single tooth or multiple teeth. Appliances indicated for management depend on the tooth or teeth involved.
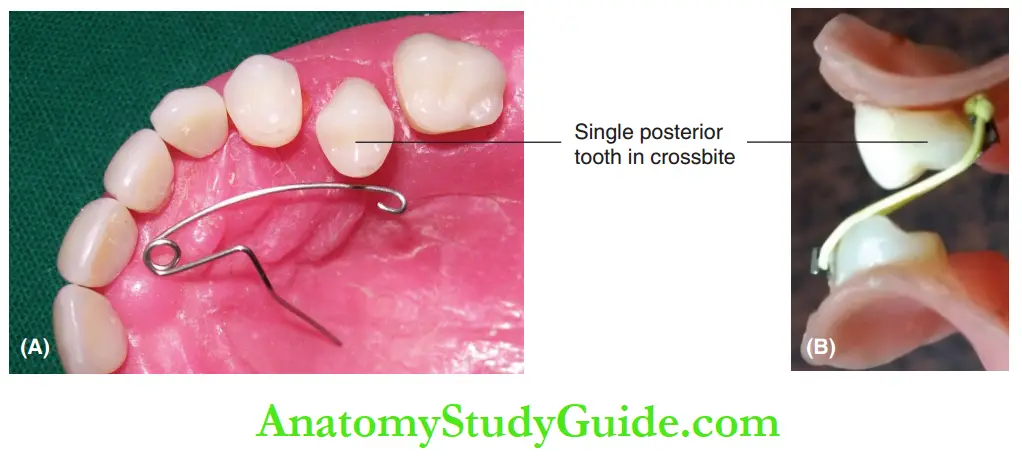
1. Appliances indicated for the correction of single tooth posterior crossbite is as follows:
Whiplash spring: It is a cantilever spring with a long arm.
Expansion screw appliance: It exerts a force on the posterior tooth in crossbite.
Elastics: Thy are engaged to find appliances on the palatal surface of the upper and the buccal surface of the lower teeth.
They produce tipping movement of the tooth in crossbite. Unwanted movement of the rightly placed tooth must be avoided.
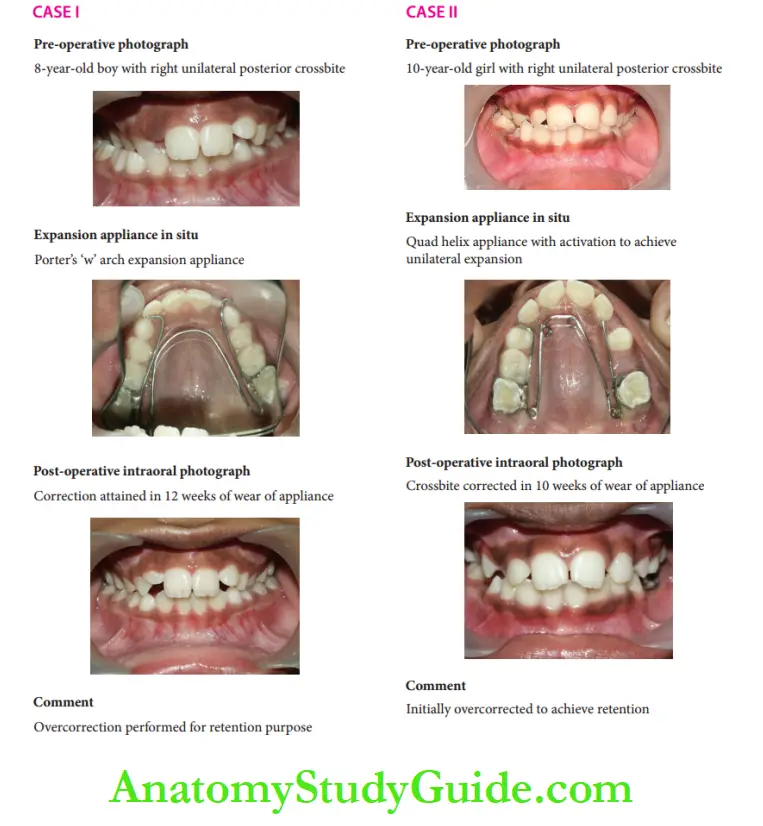
2. Appliances used for correction of multiple teeth posterior crossbite are as follows:
Rapid maxillary expansion screw: Th appliance is preferred in case of multiple teeth posterior crossbite when rapid skeletal expansion is also necessary.
The rate of expansion is 1 mm per day. It has acrylic bite planes cemented on posterior teeth.
The treatment duration is short and the appliance is held in place passively for retention purposes.
It is important to check the adequacy of the root length of the teeth on which the screws are anchored.
Hyrax screw: This is preferred when skeletal expansion is also needed.
Quad helix appliance: This is a slow expansion device producing dental expansion.
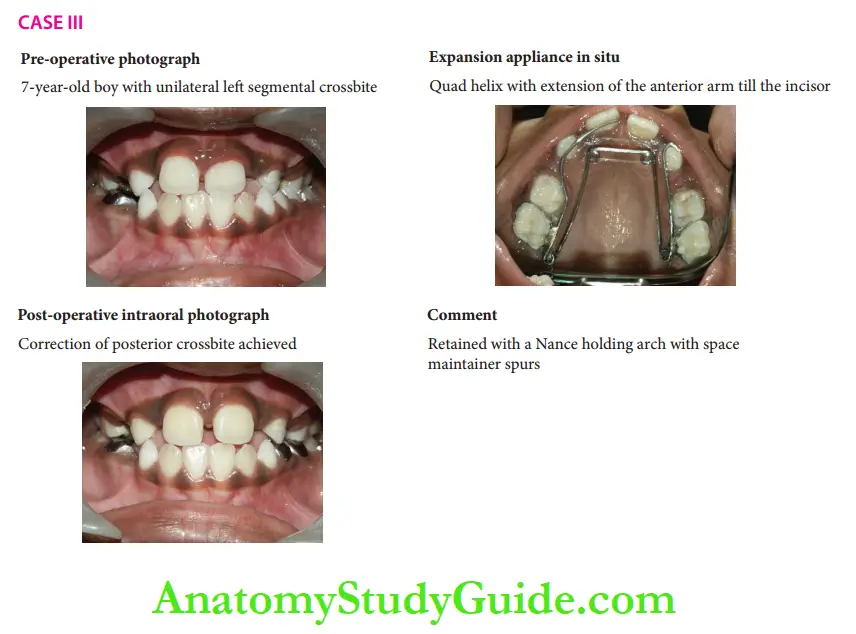
There are cases of unilateral posterior crossbite and Scissors bite. mode of correction with banded expansion appliances.
Skeletal Anterior and Posterior Crossbite
Unfavourable angulation of maxillary and mandibular teeth in their respective jaw bases is the reason for dental crossbites.
A skeletal crossbite results when disparity exists in the size/position between maxillary and mandibular jaw bases in anteroposterior/transverse planes.
The mandibular bone may be positioned anterior to the maxillary bone causing skeletal anterior crossbite.
Skeletal posterior crossbite occurs when the mandibular bone is wider than the maxillary bone in the transverse dimension.
Differentiation between dental crossbite and skeletal crossbite is essential to manage the conditions appropriately.
Both conditions present a similar clinical picture.
The inclination of maxillary and mandibular anterior teeth and anterior-posterior position of their respective skeletal bases have to be assessed to identify the skeletal or dental origin of the condition.
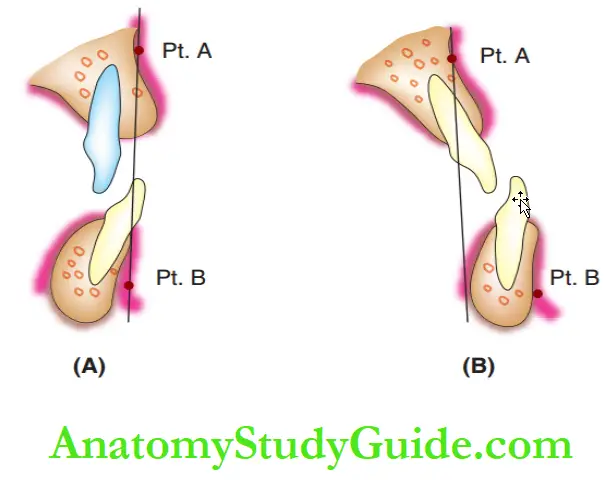
This can be checked with a lateral cephalogram by comparing the position of point A and point B on the jaw bases.
Point A (Pt. A) represents the anterior end of the maxilla and point B (Pt. B) represents the anterior end of the mandible.
The normal maxilla is positioned anterior to the mandible with Pt. A positioned 0–2 mm ahead of Pt.
B in the lateral cephalogram. An abnormality in this alignment leads to a skeletal discrepancy, discussed in the following pages.
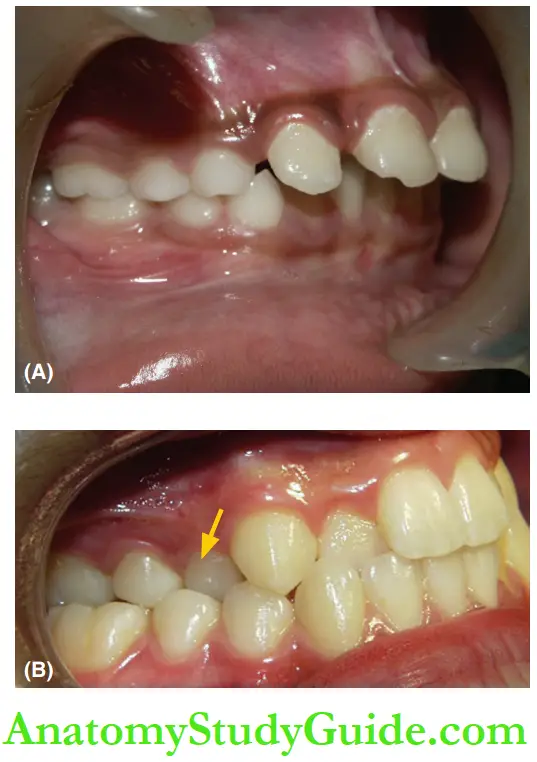
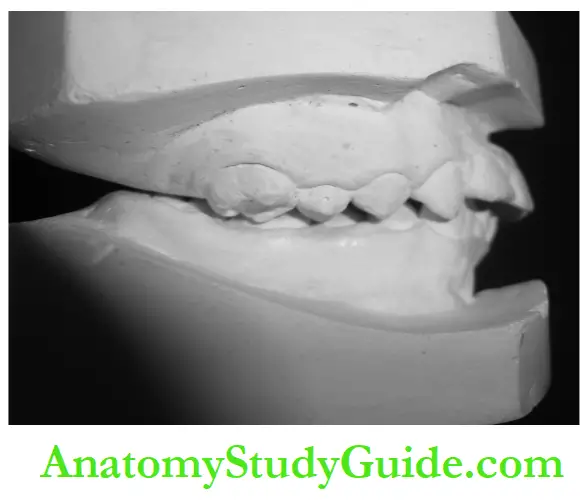
shows the difference between dental and skeletal crossbite with respect to Pt. A and Pt. B. shows a dental crossbite condition where Pt. A and Pt.
B is in normal relationship to each other B shows a skeletal crossbite condition where Pt. B is ahead of Pt. A.
Skeletal malocclusion is discussed in detail in the next section Developing Skeletal Class II and III Malocclusion.
Pseudo-Crossbite
In certain conditions, the mandible may deviate during closure from the rest position.
The deviation that occurs during this function is called functional deviation.
The crossbite that occurs due to functional deviation is called pseudo-crossbite.
For instance, a premature occlusal contact between the maxillary and mandibular teeth may guide the mandible to slide forward.
This leads to an anterior crossbite through the position and angulation of skeletal bases and the teeth are normal.
Early identification of premature contact and eliminating the same alleviates crossbites.
If left unattended, there is every possibility for a skeletal malocclusion to set in.
Developing Skeletal Class II And III Malocclusion
A discrepancy of size/shape/spatial position between the maxilla and mandible results in skeletal malocclusion.
Discrepancies between their skeletal bases occur due to restriction of growth or disproportion in the magnitude of growth between the jaws.
Inheritance of a disproportionate jaw size from either of the parents or unsynchronised growth of the maxilla and mandible also results in a skeletal mal relationship.
Functional deviation, discussed earlier, may misdirect the expression of jaw growth and initiate a skeletal discrepancy.
Developing skeletal discrepancies can occur in anteroposterior, transverse and vertical dimensions.
Discrepancies occurring in the anteroposterior dimension can present as a skeletal class II or class III condition.
Correction of skeletal discrepancies is possible by modulation of growth with interceptive orthodontic procedures.
Skeletal Discrepancy in the Anteroposterior Dimension
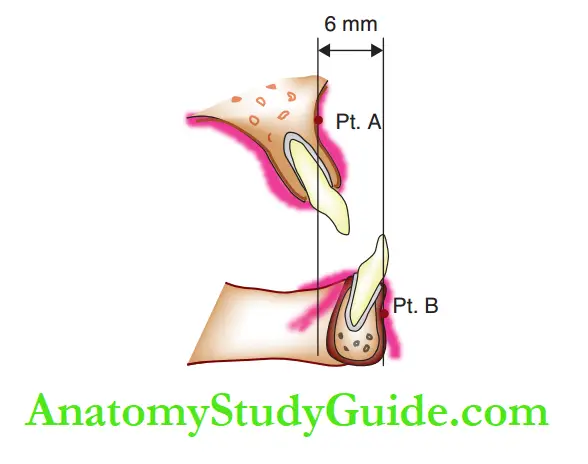
A discrepancy in the anteroposterior dimensions of the maxilla and mandible can lead to skeletal class II and skeletal class III conditions.
In normal conditions, the maxilla (Pt. A) lies slightly ahead of the mandible (Pt. B).
Skeletal malocclusion occurs when points A and B do not lie in an acceptable relationship with each other. depicts a skeletal class II condition where Pt. A of the maxilla is positioned much ahead of Pt.
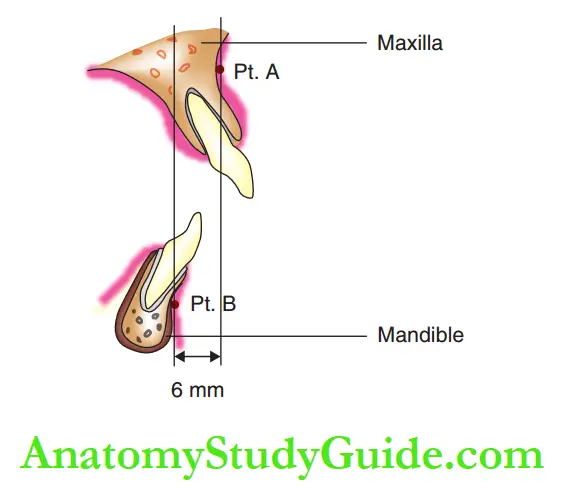
B of the mandible. This can occur in the following three situations:
- Prognathic maxilla and normal mandible
- Normal maxilla and retrognathic mandible
- Prognathic maxilla and retrognathic mandible
- depicts a skeletal class III condition where Pt. B of the mandible is positioned much ahead of Pt.
- A of maxilla. Ths can occur in the following three situations:
- Normal maxilla and prognathic mandible
- Retrognathic maxilla and normal mandible
- Retrognathic maxilla and prognathic mandible
Clinical Features
Certain clinical parameters and the patient’s history of pernicious oral habits may indicate a possibility of skeletal malocclusion.
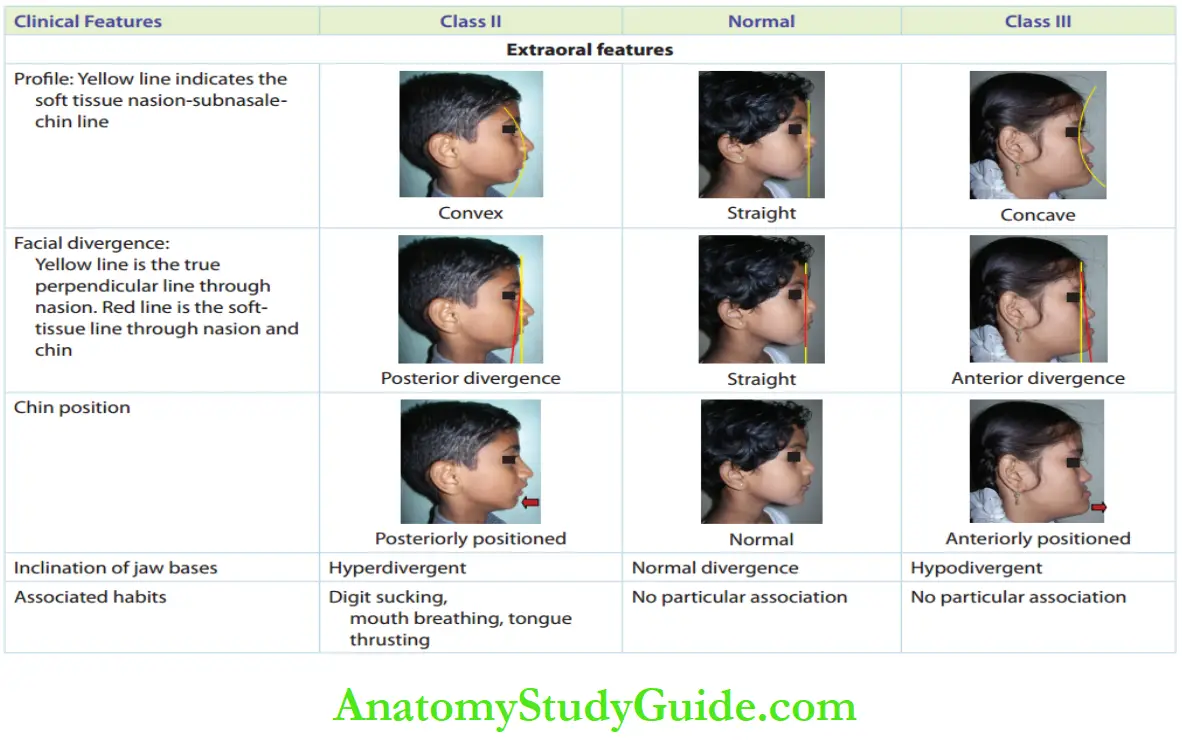
compares the extraoral and intraoral features in normal,
skeletal class II and skeletal class III situations with the help of clinical pictures.
The extraoral features of skeletal class II and class III malocclusion are as follows:
1. Profile: A line connecting the soft tissue nasion, sub nasale and chin indicates the profile of the individual.
It is straight in normal individuals, convex in class II and concave in class III conditions.
2. Facial divergence: A line connecting the soft tissue nasion and chin is compared with the true perpendicular line passing through nasion.
Both the lines superimpose in normal individuals.
The tissue nasion to the chin line diverging posteriorly to the true perpendicular line indicates a class II condition and when the line diverges anteriorly, it indicates a class III condition.
3. Chin position: The position of the chin with reference to the face as a whole is an indicator of skeletal malocclusion.
A retruded or backwardly placed chin indicates a class II condition and a prominent chin indicates a class III condition.
4. Inclination of jaw bases: The lower border of the mandible indicates whether the mandible is rotated backwards or forwards.
In most situations, backward rotation indicates class II condition and forward rotation indicates class III condition.
In most cases, the intraoral features of the permanent dentition coincide with a similar skeletal relationship of their jaw bases.
Hence, the following intraoral features may indicate a probable underlying skeletal malocclusion:
1. Angle’s molar relationship: Class I relationship where the mesiobuccal cusp of the maxillary first permanent molar occludes in the mesial groove of the mandibular first permanent molar is considered ideal.
When the mandibular molar is distal or mesial to the ideal position, it indicates a class II or class III condition, respectively.
2. Canine relationship: The mid-axis of the maxillary canine tangents the distal surface of the mandibular canine in an ideal relationship.
When the mandibular canine is distal or mesial to the ideal position, it indicates a class II or class III condition, respectively.
3. Incisor relationship: Class I relationship is where the incisal edge of the mandibular incisor is below the cingulum plateau or the mid-cingular slope region of the maxillary incisor.
When the mandibular incisor is behind or ahead of this position, it is said to be in a class II or class III relationship, respectively.
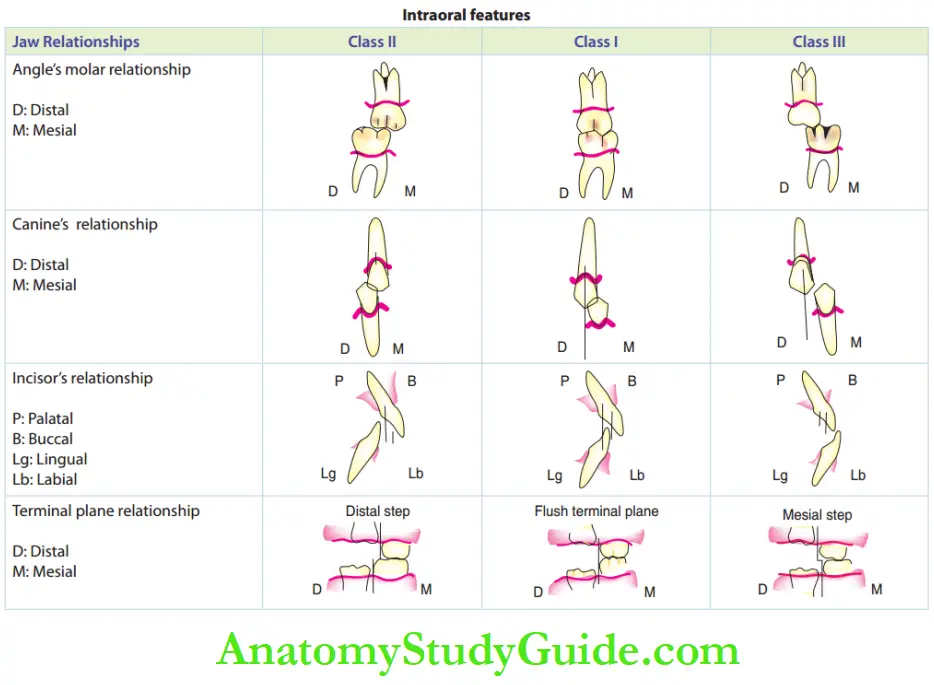
4. Terminal plane relationship: This relationship is given more importance than the permanent molar relationship during the mixed dentition stage, as the latter changes with the utilisation of leeway space.
The flush terminal plane is likely to lead to a class I molar relationship, while the distal step and mesial step relationships later lead to class II and class III permanent molar relationships, respectively.
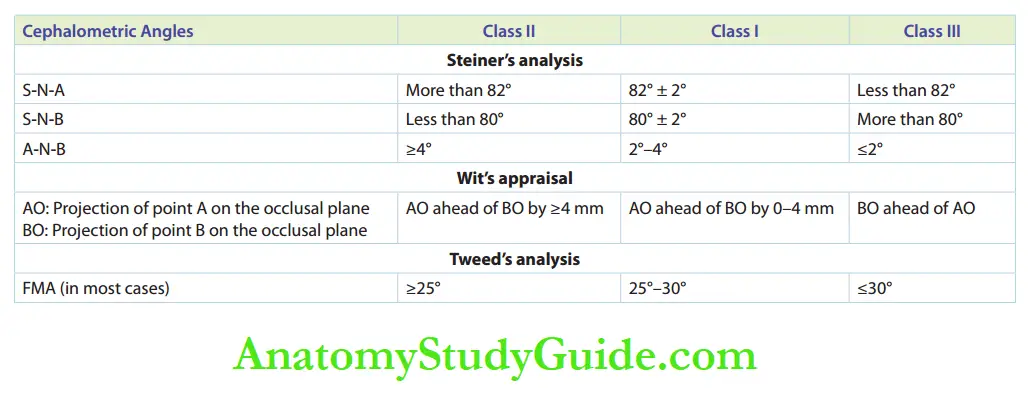
Apart from the intraoral and extraoral features, some basic cephalometric parameters are referred to in locating the positions of Pt. A and Pt. B.
Steiner’s analysis, Wit’s appraisal and Tweed’s analysis are most commonly used for this purpose. Gives a comparison between the cephalometric parameters of class I, II and III skeletal conditions.
The reader is advised to refer to books on cephalometric analysis, for more information.
Management
Every effort to treat discrepancies should be taken during the pre-pubertal period.
Active growth happens during this period and growth modification is feasible.
Growth modification is attempted to fulfil the following requirements:
- Restrict, enhance and redirect the expression of growth within genetic potentials.
- Regulate functional matrices, when disturbed The first step in managing a skeletal discrepancy is to identify the aetiology and locate the jaw causing the discrepancy.
The oral habit or the functional shift causing the skeletal discrepancy has to be eliminated and corrected, respectively.
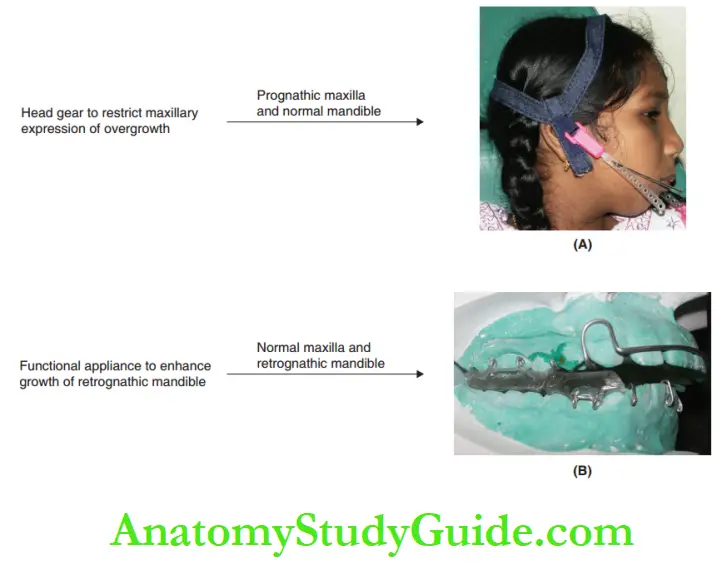
The next step is to choose an appropriate appliance to bring about the desired results.
An appliance acts by either delivering force or shielding the restricting effect of a force, depending upon the condition.
A prognathic jaw has to be restricted from expressing growth in the direction it proves unfavourable.
A retrognathic jaw is encouraged and enhanced to fully express its potential for growth or made to increase the magnitude of its growth by delivering a programmed force system through appliances.
Appliances indicated in skeletal class II conditions.
Restriction of prognathic maxilla–headgears
Enhance the growth of retrognathic mandible-functional appliances such as twin block, activator and Frankel’s functional regulators
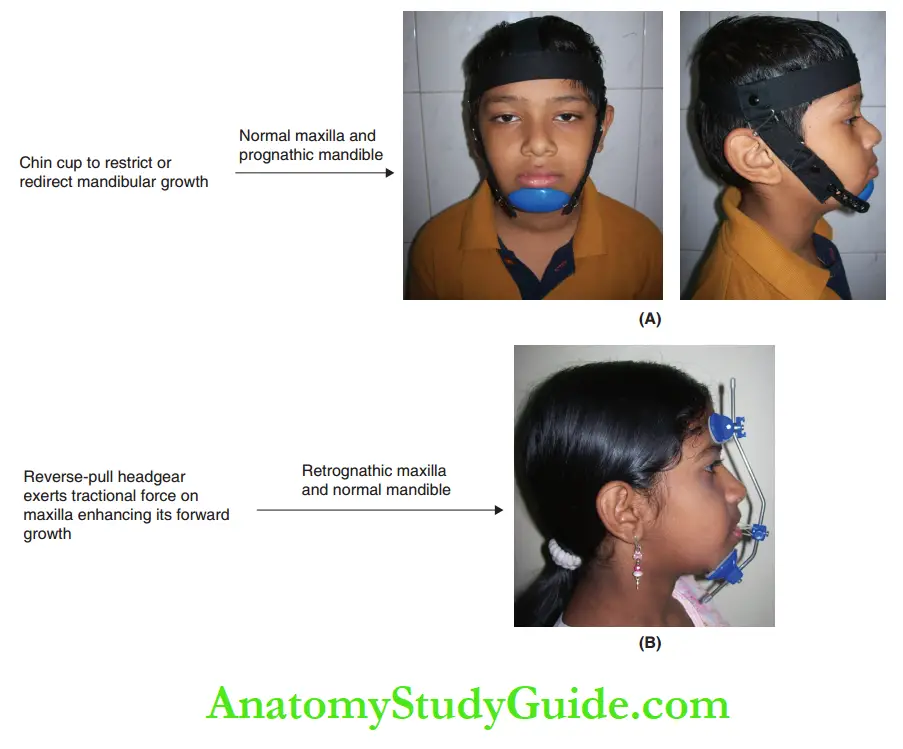
Appliances indicated in skeletal class III condition are shown in.
- Restriction of prognathic mandible – chin cup
- Enhance the growth of retrognathic maxilla – reverse-pull facemasks
Skeletal Discrepancy In the Transverse Dimension
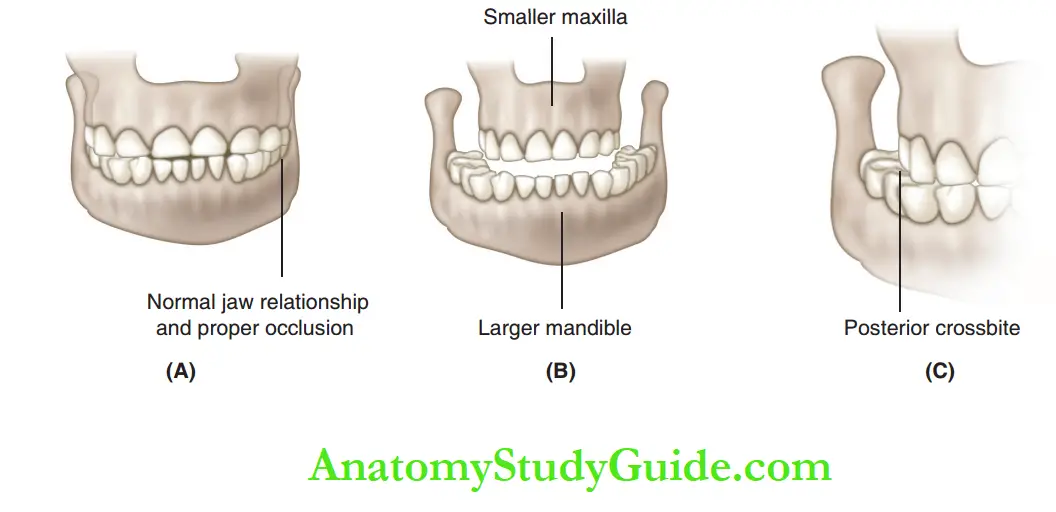
A transverse skeletal discrepancy occurs due to disproportionate transverse dimensions between the skeletal bases of the maxilla and mandible.
The maxillary and mandibular jaw bases are incompatible with each other.
There can be a smaller maxillary base for a larger mandibular base or vice versa.
In such a condition, even when teeth are in the correct position on their respective jaw bases, posterior crossbite occurs when upper and lower teeth occlude.
In most cases, the maxilla is constricted with a posterior crossbite on one or both sides.
Pernicious oral habits alter the neutral zone by disturbing the buccinator mechanism.
This causes constriction of the maxilla.
Management
The following appliances are indicated to correct skeletal discrepancies in the transverse dimension.
Established transverse skeletal discrepancies have been shown to complicate treatment modalities and the stability of results.
1. Rapid maxillary expansion with Hyrax screw: Th appliance can be used after the eruption of the premolar.
Th mid-palatal suture is split upon activation of the screw. This causes movement of the two halves of the maxilla away from each other.
Rapid expansion occurs in approximately 21 days.
This appliance is not indicated in mixed dentition as the resorbing roots of primary molars do not withstand the force of this screw.
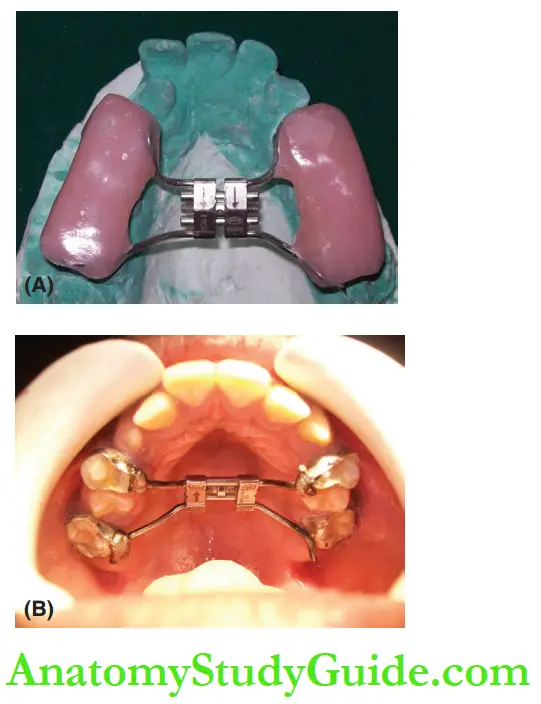
2. Quad helix: This appliance brings about a slower dental expansion as the force delivered is lesser than that in a Hyrax screw.
Quad helix is versatile, as it can cause a selective expansion in anterior/posterior/both regions.
Quad helix can be used in mixed dentition cases where an adequate root length of primary molars is evident.
Fortunately, constriction of the mandible is uncommon. Appliances are ineffective in expanding the mandibular basal structure.
As a midline suture does not exist in the mandible, Hyrax screws cannot be indicated in such cases.
Fabrication of appliances such as quad helix also proves difficult due to the presence of the tongue.
Surgical intervention is indicated for increasing the mandibular transverse dimension.
Skeletal Discrepancy In Vertical Dimension
Growth of the maxilla and mandible ideally occurs in a downward and forward direction.
When there is more growth in the vertical direction than in the horizontal direction, the lower facial height is increased.
The lower facial height appears highly disproportionate to the upper facial height.
Lips become incompetent to cover the vertical increase of the jaw bones.
This causes increased teeth show and a gummy smile.
Management
High-pull headgear is indicated in the case of vertical maxillary excess as it exerts a restrictive force on the expression of maxillar growth.
Chin cup and functional appliances indicated for transverse skeletal discrepancy address the mandibular vertical discrepancies simultaneously.
show the appliances indicated for the skeletal discrepancy in transverse dimension.
The same appliances can be modified appropriately for discrepancies in vertical dimensions also.
Intra-Arch Discrepancy
Arch size–tooth size discrepancies within one dental arch are called intra-arch discrepancies.
Proper interception can prevent or reduce the future need for elaborate orthodontic mechanotherapy.
The three important intra-arch discrepancies discussed in this chapter are as follows:
- Developing crowding
- Arch perimeter loss by migration of teeth
- Median diastema
Developing Crowding
A dental arch containing well-aligned teeth with proper mesiodistal contacts is considered to be the most functionally efficient and aesthetically pleasing.
Crowding of teeth occurs due to inadequacy of available space in the arch.
Apart from unaesthetic appearance, crowding causes the accumulation of food remnants and deposits leading to periodontal problems.
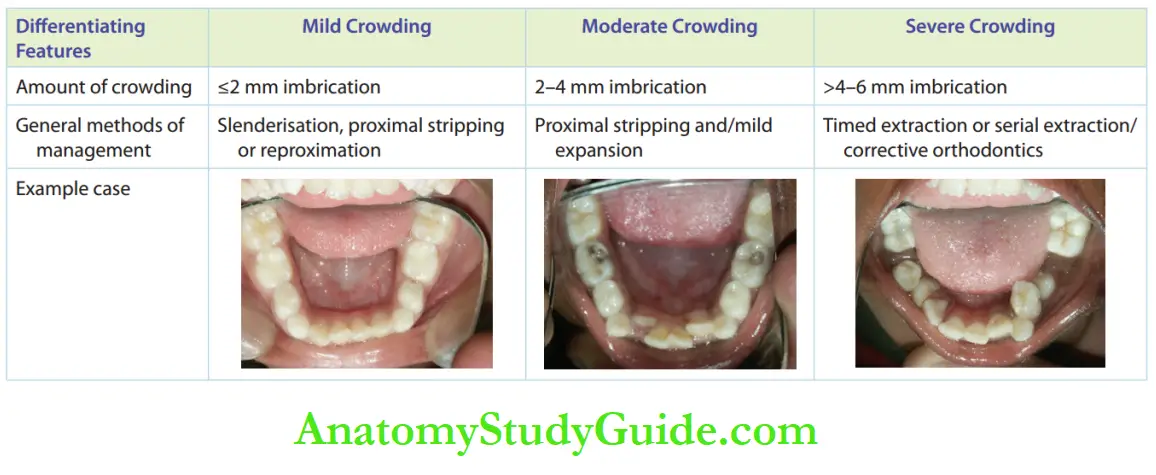
Crowding can be mild (up to 2 mm), moderate (2–4 mm) or severe (>4 mm), depending on the lack of space.
Aetiology
The potential conditions that cause crowding within a dental arch are as follows:
- The absence of spaces between the primary anterior teeth leads to a closed deciduous dentition. This is likely to result in a crowded permanent dentition.
- Tooth size–arch length discrepancies like larger-sized teeth for smaller-search can lead to crowding.
- This condition can be inherited from either of the parents. Larger-sized permanent teeth may not have space if there is inadequate growth of jaws. The incisal liability may not be nullified and causes crowding.
- Over-retained primary incisors do not provide adequate space for the erupting permanent teeth. This leads to crowding of the permanent dentition.
- Supernumerary teeth such as mesiodens or paramours occupy arch space and cause crowding of the other neighbouring teeth.
Management
Preventive and interceptive orthodontic procedures aim to correct crowding as and when it develops.
mentions the appropriate management techniques for different situations of crowding.
Mild crowding, that is less than or equal to 2 mm, can be relieved by decreasing the mesiodistal size of teeth in the arch.
This can be done by grinding the proximal surfaces of teeth by a maximum of 0.5 mm on either side.
Safe-sided discs or slender burs are used for this procedure, which is called tenderization.
This technique can also be called proximal stripping or approximation.
Moderate and severe crowding is managed by arch expansion, timed extraction and serial extraction.
For a detailed description of serial extraction and timed extraction.
Premature Loss Of Teeth
When there is premature loss of deciduous teeth or loss of permanent teeth due to either caries or injury, the neighbouring teeth gradually migrate into space occupied by them.
The situation becomes critical when permanent teeth of that region erupt only to find inadequate space, resulting in crowding.
An interceptive orthodontic procedure to avoid crowding is to regain this space, lost due to migration.
Appliances that regain lost spaces are called space regainers.
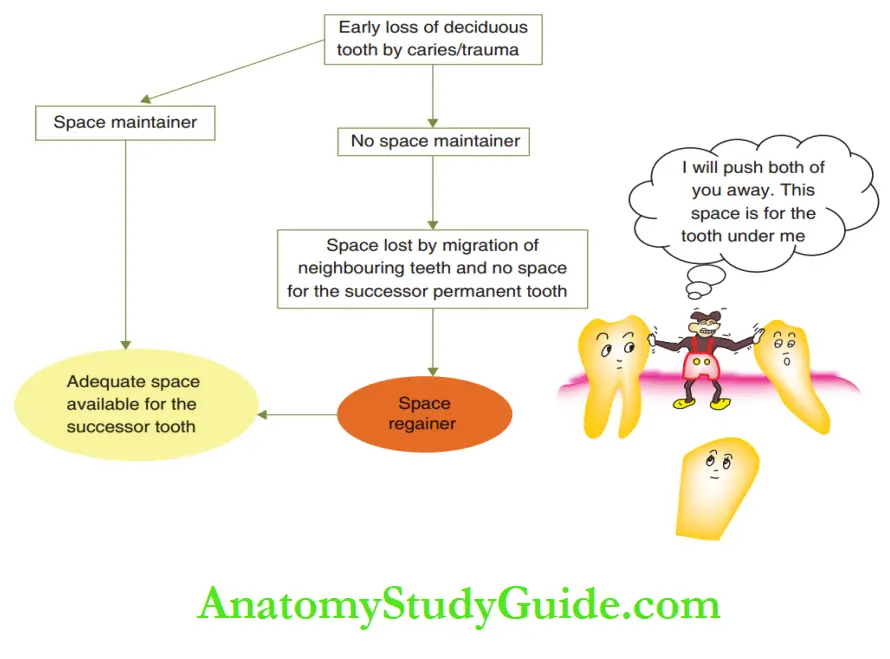
Space regainers are active appliances, unlike passive space maintainers.
They try to push the migrating neighbours until the required space is regained.
In contrast, space maintainers do not exert any force.
Ideal Requirements
A space regainer should have all the features of a space maintainer in addition to the following requirements:
- Light and continuous force should be exerted by the appliance.
- The force should not displace the migrated tooth or teeth out of the arch.
- Self-limiting force – the appliance should be active until a required amount of space is recovered and then remain passive.
Designs
The design of a space regainer is decided according to the situation.
The space regainer appliance can be fixed/removable and anterior/ posterior.
Space regainers are incorporated with active components such as springs, screws and coil springs to exert force.
Certain passive appliances such as lip bumpers are indicated to move the migrated molar teeth back to their position.
Lip bumper works by redirecting the force generated while peri-oral muscles function.
Space regainers are only capable of tipping teeth back to their position.
If bodily migration of the tooth has occurred, corrective orthodontics with field mechanotherapy has to be employed for correction.
The patient has to be referred to an orthodontist for the same.
Anterior Space Regainer
Anterior space regainers are used for mesiodistal movement of migrated anterior teeth.
Finger springs or split labial bows are indicated in these cases. These appliances have to be anchored properly with suitable clasps.
Certain assumed situations of anterior space loss and the appliances indicated to correct them are listed.
Posterior Space Regainer
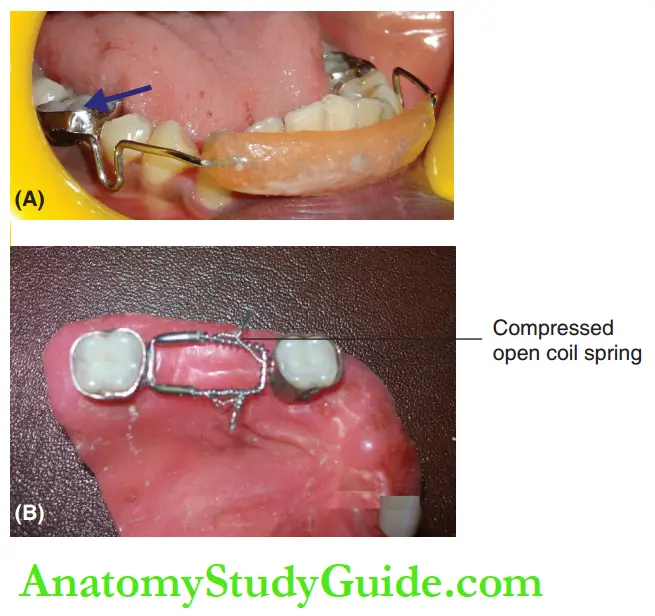
Posterior space regainers are indicated for mesially migrated molars.
A field appliance serves better when the child’s cooperation is discouraging.
A few fixed and removable types of posterior space regainers are given below:
1. Lip bumper: It applies destabilising force to the mesially migrated molars.
The lip bumper pushes the molars distally to regain lost space. The appliance is placed about 5–6 mm away from the anterior teeth.
The ‘U’ loop of the buccal wire segment is either in contact with the molar tube or soldered to the molar band.
The pressure of the lip, during its function, is transmitted to the acrylic bumper and then to the molars through the wire.
This force pushes the molars distally and space is regained.
2. Looped lingual holding arch: A lingual holding arch is a passive ‘U’-shaped wire running from one molar to the other on the lingual aspect of the lower arch.
Hotz lingual arch appliance has adjustable U loops on either side to enable activation.
The loop is activated by opening it and inserting it into the molar tube present on the lingual side of the molar band.
This exerts a destabilising force on the molar to regain lost space.
3. Appliance with screws: Expansion screws incorporated in acrylic removable appliances can be used for visualising upper and lower posterior teeth.
Expansion screws are positioned perpendicular to the midline for transverse expansion of the arch.
They are positioned parallel to the midline to produce an anteroposterior expansion.
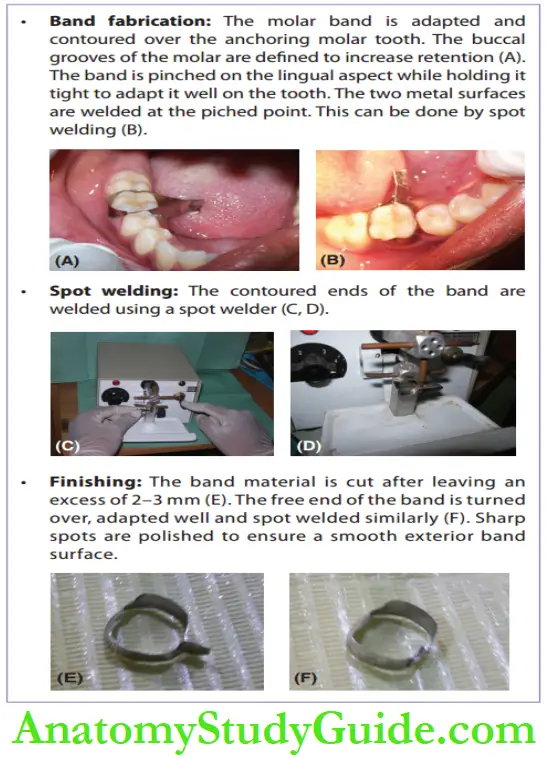
4. Gerber’s space regainer: This space regainer requires bands fabricated on teeth on either side of the space.
An open coil spring is used to deliver the force to push the teeth away from each other.
Description of band fabrication. While the migrated molar is being pushed back with the appliance, the tooth anchoring the appliance also experiences a reactionary force.
It is necessary to ensure that the anchor tooth withstands the displacing force.
Median Diastema
The midline space between central incisors is called median diastema.
The space affects function, aesthetics, phonation and arch alignment.
It also initiates certain oral habits such as frenum-sucking
Aetiology
Midline diastema occurs due to the following reasons:
- Mesiodens/supernumerary tooth
- Midline pathologies such as median cysts, cement toma and odontoma.
- The prominent and bulky labial frenum
- Peg laterals or congenitally absent lateral incisor
Management
It is important to eliminate the aetiology before advocating any appliance for median diastema.
Missing lateral incisors and peg laterals are managed by providing suitable prostheses or restorations.
Midline pathologies such as median cysts, cementoma or odontoma are removed before managing the space.
Radiographs help in identifying these midline pathologies. Frenectomy is indicated for a highly attached frenum that blanches upon lifting the lip.
Orthodontic closure median diastema is achieved with a removable or fixed appliance.
The appliance is selected according to the position of the teeth and their inclination.
Removable appliances such as split labial bows and finger springs are indicated for minor corrections.
They deliver tipping force to move the central incisors towards each other.
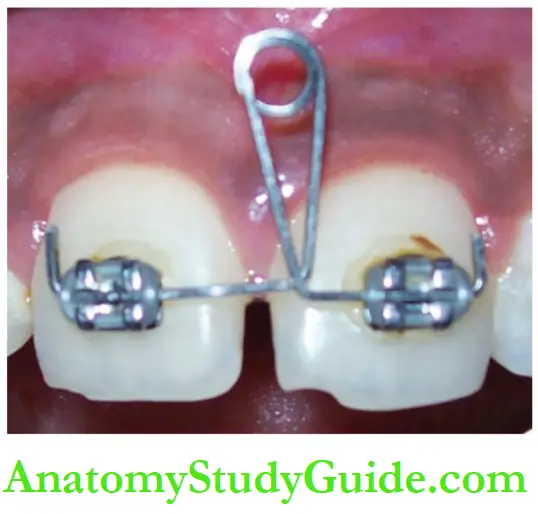
Fixed appliances are very effective for correcting wide midline diastema.
They deliver controlled force capable of causing bodily movement of the teeth.
A2 × 4 sectional fixed appliance offers good results. It has failed appendages located on the two fist molars and the four incisors.
Rectangular looped wires in an edgewise bracket slot placed on the two central incisors can close in median diastema.
Other Minor Intra-Arch Irregularities
Irregularities in individual tooth positioning disturb the alignment of teeth in the arch.
Such irregularities have to be prudently corrected at the earliest notice.
This will avoid the development of further malocclusion in the arch.
The minor intra-arch irregularities include the following:
- Rotations
- Abnormal eruption
- The altered inclination of anterior teeth
- Impacted tooth
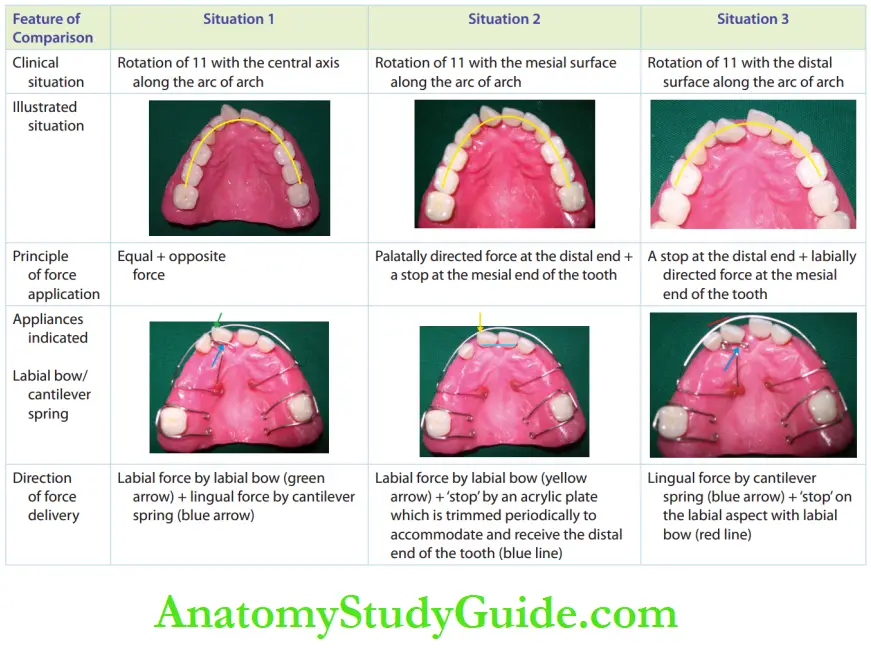
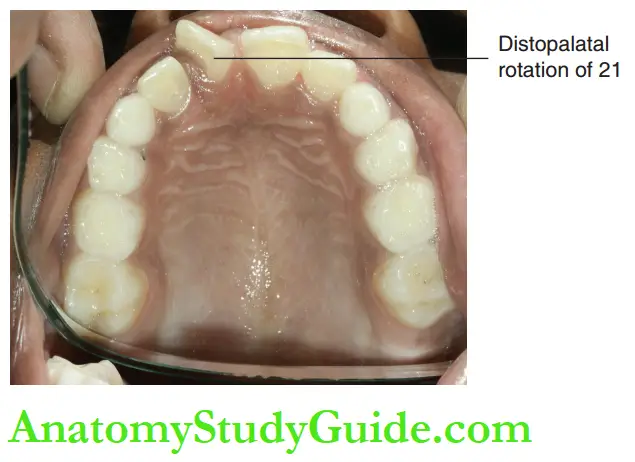
Rotation
A tooth may be rotated around its central axis with its proximal side on the facial or palatal aspect of the arc of the arch.
This can affect the integrity of the arch and the position of the adjacent teeth.
It also affects the aesthetics, function and phonation.
Management
Derotation of the tooth requires adequate space in the arch.
If the available space is inadequate, creating adequate space is a prerequisite before attempting correction.
Assessment of the type of rotation of the tooth and the extent of derotation required is necessary for designing the type of active component of the appliance indicated.
A combination of the labial bow with a cantilever spring can be of use, provided the clinician is well aware of the vectors of force delivery.
Clinicians should design the appliance after acquiring a thorough knowledge of the action and reactions of springs upon activation.
A clear prescription has to be sent to the technician to fabricate the custom-designed appliance.
The different clinical situations of rotation are appropriate management is suggested.
Abnormal Eruption
A tooth erupting away from its normal position is an ectopically erupting tooth.
An ectopic tooth also causes derangement of the arch and affects function, aesthetics and phonation.
Aetiology
A tooth can erupt in an abnormal position due to crowding and inadequate space in the arch.
Alteration in the path of an erupting tooth can occur due to the presence of a supernumerary tooth, retained deciduous tooth, retained root fragment and other physical barriers such as hard and thickened soft tissue.
The trauma of a deciduous tooth can dislocate or dilacerate the permanent successor near its root, thus changing its eruption path.
Management
Tooth erupting out of the arch allows neighbouring teeth to drift into its place.
This disrupts the arch’s intactness. A removable appliance proves futile in most of situations as precise tooth movement is required.
A sectional fied 2 × 4 appliance is recommended for correction.
It involves the two first permanent molars and the four erupted anterior teeth.
Altered Inclinations
When the axis of the tooth is inclined mesially or distally, the space occupied by the tooth in the arch is altered.
The intactness of the arch is disturbed.
An inclined or over-riding anterior tooth occupies a lesser space in the arch.
This allows neighbouring teeth to drift into the space, leading to crowding or midline shift.
Management
Early correction of an inclined tooth is desirable with fixed appliances, as removable appliances have their limitations because they only deliver tipping force.
Space availability in the arch is a prerequisite for such correction.
The correction obtained with a removable appliance may seem to be sufficient temporarily but controlled uprighting may be required later with a fixed appliance.
Impacted Tooth
Impaction of primary teeth is generally not noted. An anterior tooth may get intruded due to trauma and fail to re-emerge or re-erapt later.
Impaction of the permanent tooth may occur due to hard tissue or
soft-tissue hindrances in the path of eruption.
Hard tissue hindrances are over-retained deciduous teeth, supernumerary teeth, odontomas, etc.
Soft-tissue hindrances are mucosal thickenings around the crown of the erupting tooth.
Aetiology
Apart from the hindrances in the path of eruption, other causes may lead to impaction. They are as follows:
- Premature loss of primary teeth and migration of neighbouring teeth into that space results in loss of arch space.
- The permanent successor is blocked as there is no space for eruption. The tooth may remain impacted.
- Prolonged retention of primary teeth impedes the eruption of permanent successor teeth.
- Abnormal eruption path of the permanent tooth Certain abnormal oral habits such as constant tongue thrusting at the site of eruption may delay the eruption of the tooth.
- Systemic diseases such as cleidocranial dysostosis or endocrine disturbances such as hypoparathyroidism may be suspected if multiple impacted teeth are evident.
Sequelae:
The absence of a tooth disrupts the alignment of the arch and the integrity of occlusion, leading to the migration of neighbouring teeth into the edentulous space created.
The presence of space initiates pernicious oral habits such as posturing the tongue in the available space.
The impacted tooth may also resorb the root of the adjacent tooth. In the long term, there is a possibility of cystic changes around the impacted tooth.
Early interception is therefore necessary.
Management:
The aetiology has to be identified and eliminated. Radiographs such as orthophoto monogram, intraoral periapical view or occlusal view radiographs are used for this purpose.
Soft tissue
hindrances such as mucosal thickening are removed by oper culectomy.
Hard-tissue hindrances are eliminated surgically.
Space regainers are employed to regain the space lost due to the migration of adjacent teeth.
When a favourable environment is created, the impacted teeth do erupt without any further intervention, requiring only periodic follow-up.
However, active orthodontic intervention is called for when the tooth shows no sign of eruption.
Attachments are bonded to the tooth and active eruption is done.
Summary
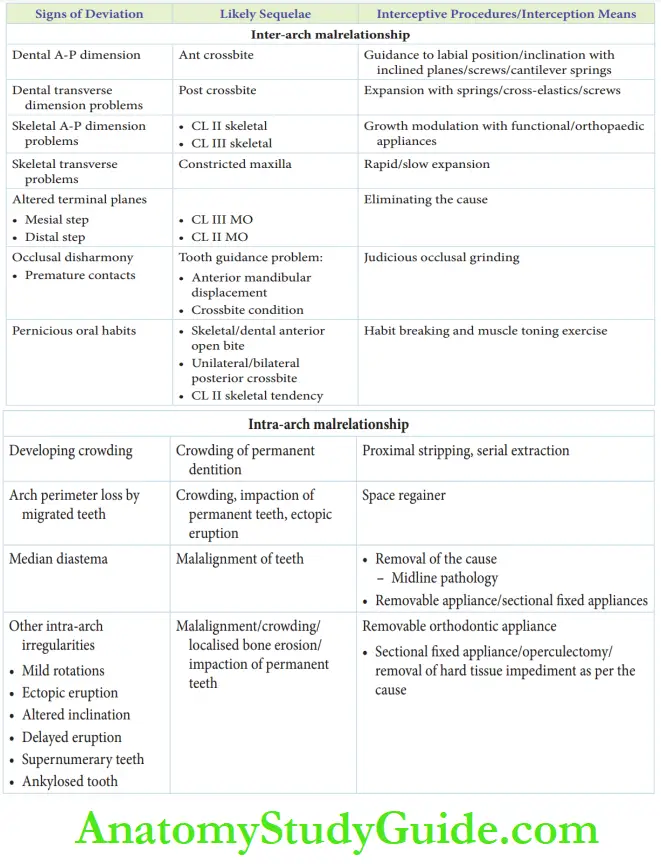
1. Various deviations and interceptive orthodontic procedures
Leave a Reply