Intestinal Amoebae: Entamoeba Histolytica
Habitat: Large intestine of man
Table of Contents
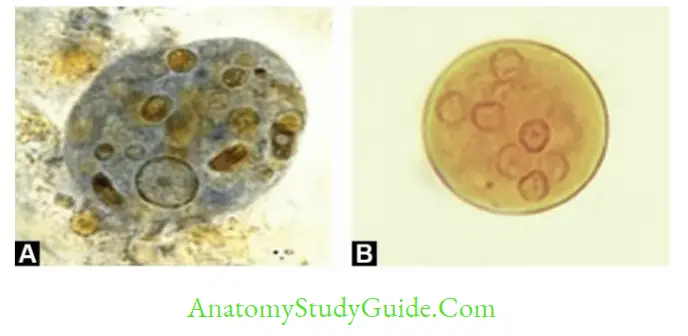
Morphology-3 stages: Trophozoites, Pre-cyst, and cyst.
Life cycle:
- Host: Humans are the only host
- Infective form: Mature quadrinucleate cyst. Cysts can resist chlorination, gastric acidity, and desiccation and can survive in a moist environment for several weeks
- Mode of transmission: Fa eco-oral route and rarely sexual transmission (especially in developed countries among homosexual males). excystation occurs in the small intestine → four small meta cystic trophozoites are released and carried to the large intestine → Trophozoites colonize the GIT mucosa → depending on nutritional status and host immunity, there may have different courses
Read And Learn More: Micro Biology And Immunology Notes
- Asymptomatic cyst passers
- Amoebic dysentery: Trophozoites of E. histolytica secrete proteolytic enzymes that cause destruction and necrosis of intestinal tissue, flask-shaped ulcer formation, and release of large numbers of trophozoites along with blood and mucus in stool
producing amoebic dysentery. Trophozoites usually degenerate within minutes. - Amoebic liver abscess: In a few cases, trophozoites gain entrance into the radicals of portal veins; where they multiply and produce an amoebic liver abscess.
- Ency station: Occurs in the large intestine → first precyst → immature cysts and later mature quadrinucleated cysts are released in the feces (diagnostic form). Cyst formation can be induced by food deprivation, overcrowding, desiccation, accumulation of waste products, and cold temperatures.

Virulence Factors
- Amoebic Lectin antigen: It is a 260 kDa galactose and N-acetylgalactosamine inhabitable surface protein (Gal/NAG lectin) that helps in adhesion
- Cysteine proteinase, Amebapore, Hydrolytic enzymes, Neuraminidase and metallocollagenase, and Thioredox in reductase system
Intestinal Amoebiasis
- Males and females are affected equally with a ratio of 1:1
- Amoebic ulcer:
- Flask-shaped (broad base with a narrow neck)
- Most common site: Ileocecal region
- Complications of intestinal amoebiasis:
- Fulminant amoebic colitis (occurs more commonly in immunocompromised patients and in pregnancy)
- Amoebic appendicitis
- Intestinal perforation and amoebic peritonitis
- Toxic megacolon and Intussusception
- Perianal skin ulcers (Amoebiasis cuts)
- Amoeba (Amoebic granuloma): Diffuse pseudotumor-like mass found in the rectosigmoid region, seen in chronic amoebiasis.
Amoebic Liver Abscess
- MC site involved: Posterior superior surface of the right lobe of the liver
- Sex: Male: female ratio is 9:1
- Anchovy sauce pus: Liver abscess pus is a thick chocolate brown color
- Complications of amoebic liver abscess: Granuloma cutis (amoebiasis cutis), amoebic pleuritic, subphrenic abscess and generalized peritonitis, amoebic pericarditis, the homogenous spread can occur from liver causing brain abscess and secondary amoebic encephalitis, lung abscess, splenic abscess, and painful genital ulcers.
Laboratory Diagnosis
- Minimum of three stool samples on consecutive days: As amoebae are shed intermittently.
- Stool Microscopy-done to demonstrate:
- Trophozoites: Demonstration of hematophagous (RBC ingested) motile trophozoite in freshly-passed stool is considered as gold standard microscopic test. It indicates active infection
- Quadrinucleated cysts: Indicates carrier state. The iodine mount clearly demonstrates the internal structures of the cyst. When the amoeba load in stool is less (as in chronic amoebiasis or convalescent stage), stool samples can be examined after concentration
by formalin ether sedimentation method. - Cyst and trophozoites of E. histolytica should be differentiated from E. coli, which is communal in the stool.
- Stool culture: Two types—(1) Polyenic culture and (2) Axenic culture.
- Polyenic culture:
- Contains bacterial supplements providing nourishment to amoeba.
- Used in chronic and asymptomatic carriers passing less number of cysts.
- 50–70% sensitivity and 100% specificity (gold standard).
- Various cultural media used are:
- National Institute of Health (NIH) media
- Boeck and Drbohlav egg serum medium containing Locke’s solution
- Balamuth’s medium, Nelson’s medium, and Robinson’s medium.
- Axenic culture: It lacks bacterial supplement, e.g. Diamond’s medium. Axenic culture is useful when the bacterial flora interferes with the test results such as:
- Studying pathogenicity of amoeba
- Testing antiamoebic drug susceptibility
- Preparation of amoebic antigen in mass for serological tests
- For harvesting the parasite to determine the zymodeme pattern.
- Stool antigen detection (copra-antigen):
- By ELISA detecting 170 kDa of lectin antigen (has more than 95%
- Immunochromatographic test (ICT): It helps in the simultaneous detection of antigens specific for Giardia lamblia (alpha-1 giardin antigen), E. histolytica (29 kDa surface antigen), and Cryptosporidium parvum from stool.
- Amoebic antigen in serum indicates recent and active infection. ELISA is done for lectin antigen.
- Amoebic antibody: Serum antibodies appear only in the later stages of intestinal amebiasis,e.g. ELISA, IFA, and indirect hem agglutination test (IHA).
- Zymodeme Analysis: Detecting isoenzyme markers like palate dehydrogenase, hexokinase, glucophosphate isomerase, and phosphoglucomutase.
- Molecular diagnosis: (1) Nested multiplex PCR, (2) real-time PCR, and (3) BioFire
Film Array (Its gastrointestinal panel is used to detect common bacterial, viral, parasitic (Cryptosporidium sp, - Cyclospora, E. histolytica, Giardia) diarrheal pathogens.
Charcot Leyden crystal in stool and moderate leukocytosis in blood.


Laboratory Diagnosis of Amoebic Liver Abscess
- Microscopy and Histopathology of liver pus shows trophozoites but never cyst. This is specific but of low sensitivity (< 25%)
- Stool microscopy and culture is not useful
- Lectin antigen by ELISA (170-kDA of lectin Ag), is usually absent in stool but can be demonstrated in serum (70% sensitive in late stage, 100% sensitive when tested before treatment), liver pus (100% sensitive when tested before treatment) and saliva (70%
sensitive). - Antibody detection: Antibodies are often elevated and can be detected by ELISA, IHA, and IFA (titer of ≥1:256 and 1:200 respectively are considered as significant). However,antibodies persist even after the cure, so it cannot differentiate between recent and old infections.
- Molecular diagnosis by Nested multiplex PCR and real-time PCR (detecting 18S rRNA) with a sensitivity of 100% and specificity of 90–100%.
- USG of the liver shows the site of the abscess and its extension.

Amoebae Morphologically Resembling with E. histolytica
- E. dispar, E. moshkovskii and E. Bangladeshi are the amoebae that are morphologically similar to of E. histolytica (both cyst and trophozoite).
- Cysts and trophozoites of all three subspecies are morphologically identical.
- All colonize the large intestine, however, only E. histolytica causes invasive disease
- Differentiated by:
- Lectin antigen (found only in E. histolytica)
- RBC inside trophozoites (sign of invasion, found only in E. histolytica)
- PCR
- Distinct isoenzyme markers by zymodeme study.
Treatment

Free-Living Amoebae
Free-living amoebae are small, freely living, widely distributed in soil and water and can cause opportunistic infections in humans. Human pathogens are:
- Naegleria fowleri is a causative agent of primary amoebic meningoencephalitis (PAM).
- Acanthamoeba species causes granulomatous amoebic encephalitis (GAE) and amoebic keratitis in contact lens wearers.
- Balamuthia mandrillaris causes GAE.
- Sappinia species: causes encephalitis.

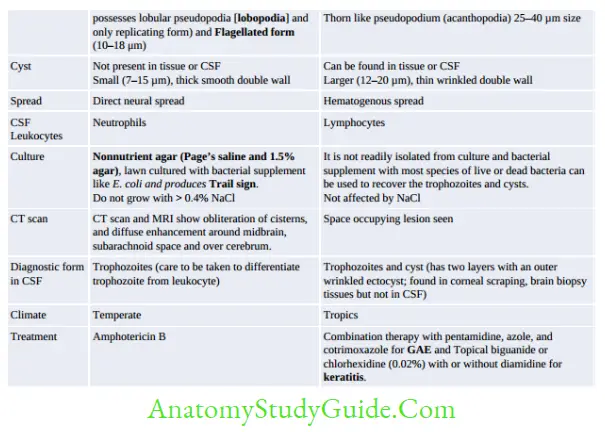

- A multiplex real-time PCR is available targeting Acanthamoeba species, Balamuthia, and N. fowleri. It is a rapid, sensitive,
and specific assay; results can be reported within 4 to 5 hours. - Approximately 20–24% of clinical and environmental isolates of Acanthamoeba harbor bacterial pathogens such as
Legionella species, Mycobacterium avium, and Listeria, and may serve as a potential reservoir and act as Trojan horses of the microbial world.

Balantidium Coli
- Only ciliate parasite of humans: Trophozoite is ciliated
- Largest protozoa invading the human intestine
- Site involved: Large intestine
- Infective form: Cysts in contaminated food or drink
- Both trophozoite and cyst are bi-nucleated: Macro nucleus and Micronucleus
- Trophozoites divide by both binary fission and conjugation
- Dysentery: Ulcers mimic amoebic ulcers but never invade the muscular layer
- Diagnosis: Detection cyst, rarely trophozoites
- Treatment: Tetracycline – DOC.
Leave a Reply