Lasers In Endodontics
Lasers in dentistry are considered to be a new technology that is being used in clinical dentistry to overcome some of the drawbacks posed by conventional dental procedures.
Table of Contents
This technology was first used for dental application in 1960 but its use has rapidly increased in the last few decades.
Laser is an acronym for “ Light Amplification by Stimulated Emission of Radiation.”
The application of lasers is almost in every field of human endeavor from medicine, science, and technology to business and entertainment over the past few years.
Read And Learn More: Endodontics Notes
Lasers In Endodontics History
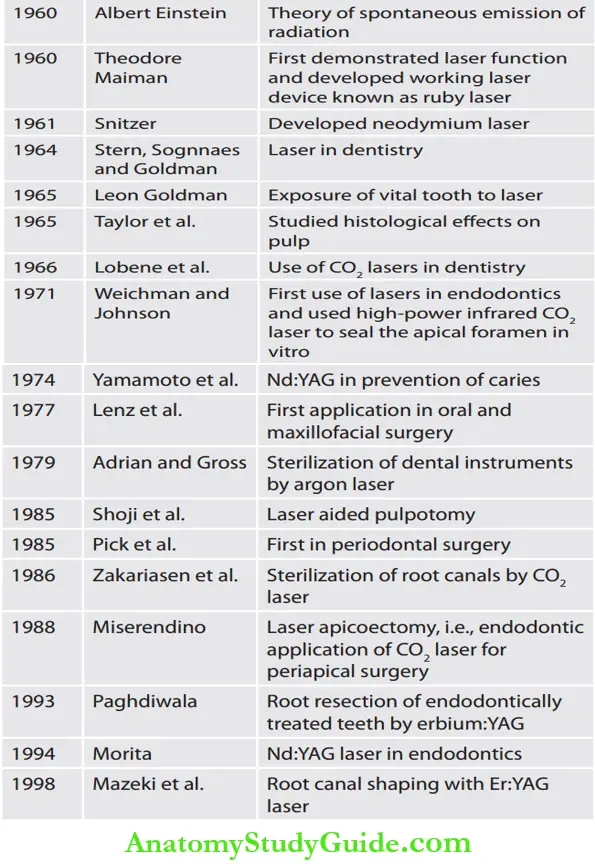
- The first laser or maser as it was initially called, was developed by Theodore H Maiman in 1960. Maser-like laser is an acronym for “Microwave amplification by stimulated emission of radiation.”
- This laser constructed by Maiman was a pulsed ruby laser. The second laser to be developed was the neodymium laser by Snitzer in 1961.
- The first report of laser exposure to a vital human tooth was given in 1965 by Leon Goldman.
- In 1965, Taylor and associates reported the histologic effect of ruby laser on dental pulp. From the 1960s to the early 1980s, dental researchers continued to search for other types of lasers.
- Lobene et al. in 1966 researched the CO2 laser which has a wavelength of 10.6 µm and can be well absorbed by enamel, so considered suitable for sealing of pits and fissures, welding of ceramics to enamel, or prevention of dental caries.
- The advantages of CO2 laser was first applied to periodontal surgery by Pick et al. in 1985. Sufficient research exists to predict that current laser systems such as erbium: YAG, holmium: YAG, Nd: YAG, and excimer have the potential to replace the dental drill for a number of cases.
Classifiation of Laser
- According to ANSI and OHSA standards, lasers are classified as:
- Class 1: These are low-powered lasers that are safe to use, for example, laser beam pointer
- Class 2a: Low-powered visible lasers that are hazardous only when viewed directly for longer than 1,000 s, for example, He–Ne lasers
- Class 2b: Low-powered visible lasers that are hazardous when viewed for >0.25 s
- Class 3a: Medium-powered lasers that are normally hazardous if viewed for <0.25 s without magnifying optics
- Class 3b: Medium-powered lasers that can be hazardous if viewed directly
- Class 4: High-powered lasers (0.5 W), can cause ocular, skin, and fie hazards.
- Based on the wavelength of the beam:
- Ultraviolet rays: 140–400 nm
- Visible light: 400–700 nm
- Infrared: 700 to microwave spectrum.
- Based on the penetration power of the beam:
- Hard: Increased penetration power For example, Nd: YAG, argon
- Soft lasers: Decreased penetration power For example, diode, GA–Sa, He–Ne lasers.
- Based on pulsing:
- Pulsed: The beam is not continuous, i.e., it is of short duration
- Nonpulsed: The beam is continuous and is of fixed duration.
- According to the type of laser material used:
- Gas lasers: CO2 lasers, argon lasers, He–Ne lasers
- Liquid lasers: Ions of rare earth or organic fluorescent dyes are dissolved in a liquid, for example, dye lasers
- Solid state lasers: Ruby lasers, Nd: YAG lasers
- Semiconductor lasers: Gallium, Arsenide.
Principles of Laser Beam
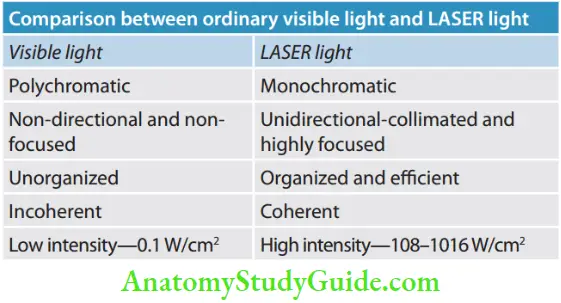
The common principle on which all lasers work is the generation of monochromatic, coherent, and collimated radiation by a suitable laser medium in an optical resonator.
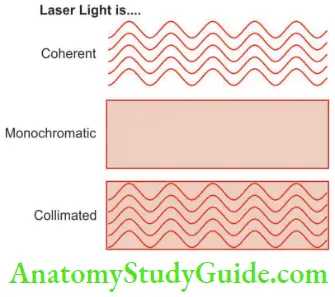
- Monochromatic: Light produced by a particular laser is of a characteristic wavelength. If the light produced is in the visible spectrum (400–750 nm), it will be seen as a beam of intense color.
- It is important to have this property to attain high spectral power density of the laser.
- Coherence: A laser produces light waves that are physically identical. They are all in phase with one another, that is, they have identical amplitude and identical frequency.
- In an ordinary light source, much of the energy is lost as out-of-phase waves cancel each other. Coherency is a property unique to lasers. The light waves produced by a laser are a specific form of electromagnetic energy.
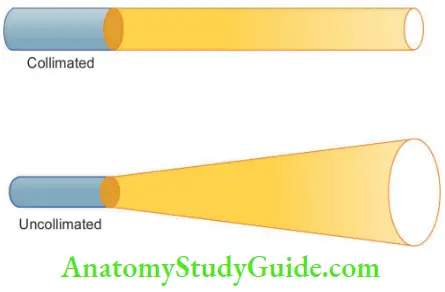
- Collimation: Collimation refers to the beam having specific spatial boundaries. These boundaries ensure that there is a constant beam size and shape that is emitted from the laser unit.
- The main differentiating characteristic of lasers is the wavelength which depends on the laser medium and excitation diode, i.e., continuous wave or pulsed mode.
- The main differentiating characteristic of lasers is the wavelength which depends on the laser medium and excitation diode, i.e., continuous wave or pulsed mode.
Laser is classified in three groups according to the wavelength spectrum under which it falls:
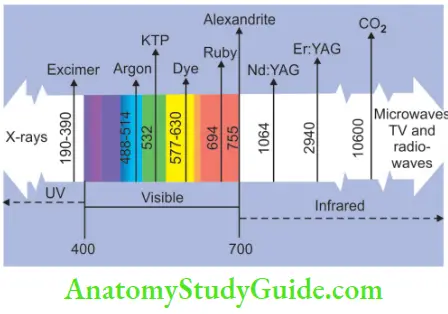
- Ultraviolet (UV range) approx 140–400 nm
- Visible light (VIS range) approx 400–700 nm
- Infrared (IR range) approx 700–microwave spectrum
The shorter the wavelength, the more energetic is the light.
Laser Physics
The basic units or quanta of light are called photons.
- Photons behave like tiny wavelets similar to sound wave pulses. If a photon is absorbed, its energy is not destroyed but rather used to increase the energy level of the absorbing atom.
- The photon then ceases to exist and an electron within the atom jumps to a higher energy level. This atom is thus pumped up to an excited state from the resting ground state.
- In the excited state, the atom is unstable and will soon spontaneously decay back to the ground state, releasing stored energy in the form of an emitted photon.
- This process is called spontaneous emission. The spontaneously emitted photon has a longer wavelength and less energy than the absorbed photon.
The difference in energy is usually turned into heat.
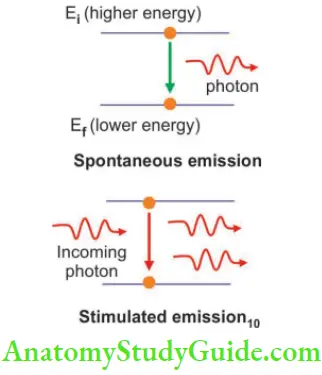
- The process of lasing occurs when an excited atom can be stimulated to emit a photon before the process occurs spontaneously.
- When an atom in the excited state becomes irradiated with a photon of light energy of the same wavelength and frequency that was previously absorbed, as it returns to its resting state, it will emit two photons of light energy of the same direction in the spatial and temporal phase.
- This is the stimulated emission of radiation.
- If a collection of atoms is more that are pumped up into the excited state then remain in the resting state, the spontaneous emission of a photon of one atom will stimulate the release of a second photon in a second atom and these two photons will trigger the release of two more photons.
- These four then yield eight, eight yields sixteen and the cascading reaction follows to produce a brief intense flash of a monochromatic and coherent light.
Basic Components of Laser
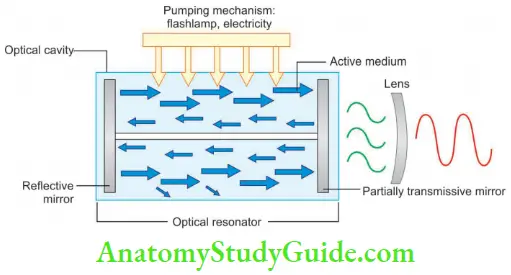
- Laser medium or active medium—This consists of chemicals that are used to fil the optical cavity. The active medium contains atoms that can emit light by stimulated emission. The active medium can be solid-liquid, gas, or plasma. Lasers are generally named for material of active medium which can be a container of gas, a crystal, or a solid-state semiconductor.
- Excitation mechanism—Pump energy into active medium by one or more of three basic methods: optical, electrical, or chemical.
- Optical resonator—Lasers reflect the laser beam through the active medium for amplification. It also helps to prevent the scattering of radiation in the optical cavity.
- Optical cavity—In this, all the other components of the laser are housed. An optical cavity is at the center of the device. The core of the cavity is comprised of chemical elements, molecules, or compounds and is called the active medium.
- Optical mirror—These are totally reflective and partially transmissive mirrors placed parallel to each other. These act as optical resonators reflecting the waves back and forth and help to collimate and amplify the laser beam.
- Lens—It helps in the convergence of light to a focal point. The size and shape of the lens determine the focal length and spot size. Spot size measures the surface area on which the laser is concentrated. It is directly related to efficiency. A smaller spot size is ideal for incisions and a bigger one for ablation and hemostatic procedures. The laser beam can be focused through a lens to achieve a converging beam that has high intensity to form a focal spot. When the laser is moved away from the tissue and away from the focal point, the beam is defocused,
becomes more divergent, and therefore delivers less energy to the surgical site.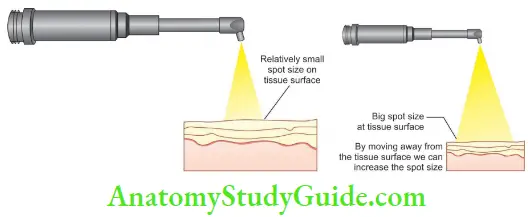
Power Density
Power density is simply the concentration of photons in a unit area. Photons concentration is measured in watts and area in square cm.
Threfore, PD = W/cm2
= W/pr2 (r = beam diameter/2)
- From the beam profile, we know that the power density in the center of the spot is higher and that at the edge of the spot approaches zero.
- Power density can be increased significantly by placing a lens in the beam path because the light is monochromatic and collimated.
- Power density can be increased by the wattage but increasing the power by 10 changes the power density by 10. But decreasing the area by 10 increases the power density by 100.
Type of Lasers
- Carbon Dioxide Lasers
- Developed by Patel et al. in 1964
- Wavelength—10.6 µm
- Highly absorbed by soft and hard tissues with shallow depth of penetration
- Ideal laser for soft tissues
- Limited penetration depth (0.2–0.3 mm)
- Focused beam—fie dissection
- Defocused beam—ablates the tissue.
- Carbon Dioxide Lasers Uses
- It has been used successfully in soft tissue surgery such as:
- Gingivectomy
- Soft tissue surgery
- Frenectomy
- Removal of benign and malignant lesions
- Excisional biopsy
- Incisional biopsy.
- Neodymium:Yttrium Aluminum-Garnet Lasers
- Developed by Geusic in 1964
- Wavelength—1.06 µm
- Penetration depth—0.5–4 mm
- First laser exclusively for dentistry
- Affinity for pigmented tissues
- Penetrates wet tissues more rapidly
- Ideal for root canal sterilization and soft tissue procedures.
- Neodymium Uses
- Nd: YAG laser is used for
- Vaporizing carious tissue
- Sterilizing tooth surfaces
- Cutting and coagulation of dental soft tissue
- Sulcular debridement
- Treat dentinal hypersensitivity
- Remove extrinsic stains
- Prepare pits and fissures for sealants
- Argon Lasers
- Two emission wavelengths used in dentistry
- Delivered through the firo-optic system
- Blue wavelength—488 nm—mainly used for composite curing
- Green wavelength—510 nm—used for soft tissue procedure and coagulation
- Absorbed by hemoglobin tissue and melanin cells.
- Argon Lasers Uses
-
- Composite curing
- Acute inflammatory periodontal lesion
- Hemangioma
- Caries detection.
Emission Modes Of Laser
- Continuous: Th beam is transmitted at one power continuously as long the device is active, for example, CO2 and diode lasers
- Gated pulse mode: Th periodic alteration of laser being on or of like blinking of an eye. It is activated by opening or closing of shutter in front of the beam path
- Free running pulse mode: Here a large peak energy of laser light is emitted for a short time followed by a long time when laser is off, for example, Nd: YAG, Er: YAG lasers.
Laser Interaction with Biological Tissues
When laser interacts with the tissues, it can be absorbed, reflected, scattered, or transmitted.
The type of interaction between a laser beam and any tissue is determined by the wavelength of the laser beam, the operation mode of the laser, the amount of energy applied, and tissue characteristics.
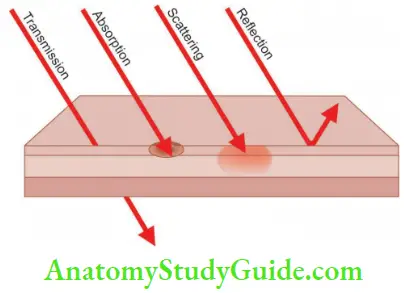
Absorption
Here specific molecules in the tissue known as chromophores absorb photons and produce photochemical, photothermal, photomechanical, and photoelectrical effects.
- Photochemical Effects
- The basis of the photochemical effect is the absorption of the laser light without any thermal effect leading to a change in the chemical and physical properties of atoms and molecules.
- Photochemical effects include biostimulation, that is, the stimulatory effect of lasers on biochemical and molecular processes that normally occur in the tissues such as healing and repair.
- Photothermal Interaction
- In this interaction, laser light energy absorbed by tissue substances and molecules becomes transformed into heat energy which produces the tissue effect. The amount of laser light absorbed into the tissue depends on:
- The wavelength of radiant energy from the laser
- Power density
- Pulse duration
- Spot size
- Composition of target tissue: High water content of most oral tissue is responsible for the absorption of radiant energy in the target region.
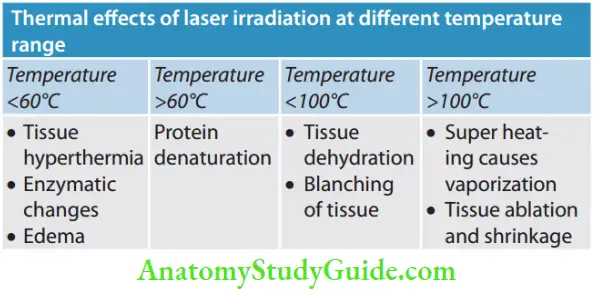
- In this interaction, laser light energy absorbed by tissue substances and molecules becomes transformed into heat energy which produces the tissue effect. The amount of laser light absorbed into the tissue depends on:
- Photomechanical Interaction
- Laser energy can be converted into acoustical energy which upon impact, creates a shock wave that disrupts the target tissue.
- This mechanical disruption occurs whenever the photon energy of the beam exceeds the target tissues. It has three interrelated phases, i.e. ionization, plasma formation, and shockwave generation.
- Photoelectrical Interaction
- This includes photo plasmolysis which explains how tissue is removed by the formation of electrically charged ions that exist in a semi-gaseous high-energy state.
Reflection
The laser beam gets reflected back with no absorption and interaction with tissues. This reflected beam results in undesirable effects of the laser.
Transmission
In this laser energy can pass through superficial tissues to interact with deeper tissues. Nd: YAG and diode lasers show deeper penetration due to tissue transmission.
Scattering
Once the laser energy enters the target tissue, it scatters in different directions. This property is not helpful but can help with biostimulation properties sometimes.
Laser Safety in Dental Practice
The surgical lasers currently used in dentistry generally fall category that is considered the most hazardous group of lasers.
The following hazards are seen with lasers in dentistry:
- Ocular hazards: Retinal and corneal injury occurs either by direct emission or from the laser.
- Tissue hazards: A temperature rise of 21°C above normal body temperature can cause the denaturation of cellular enzymes which interrupts basic metabolic processes.
- Environmental hazards: These non-beam hazards can be the production of smoke, toxic gases, and chemicals
- Electrical hazards: These can occur in the form of electric shock, fire, or explosion.
Laser Safety
To avoid an electrical hazard, the operatory must be kept dry.
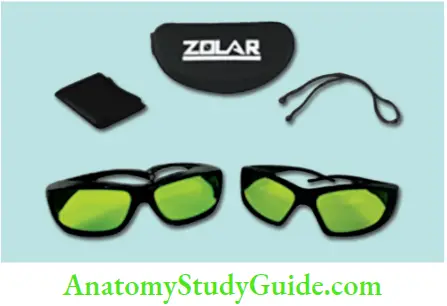
- Use eyewear for protecting the eyes
- Ventilation and evacuation to prevent airborne contamination
- Avoid highly reflctive instruments and mirror surfaces.
Advantages of Lasers
- Less bleeding
- Less pain
- No need for anesthesia
- No noise
- Faster healing
- Less chances of infection
Applications of Lasers
Laser Doppler Flowmetry
Laser Doppler flowmetry (LDF) detects blood circulation in the pulp to check vitality. It is a reliable and comfortable method for the patient.
Diagnodent
It is based on the principle, that is, bacterial metabolites within caries produce fluorescence which is enhanced by laser light.
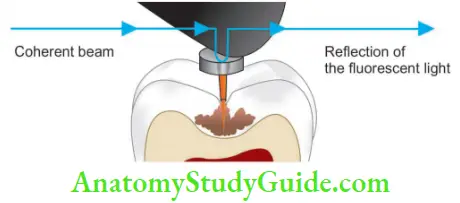
- Advantages of diagnosed
- Easy detection of ICEBERG syndrome—90% of the caries is within the proximal area—they will be detected with diagnosed
- Helps in the early detection of fissure caries and calculus
Thermal Testing
In this pulsed Nd: YAG laser is applied on the tooth. Pain produced by the laser is mild and tolerable when compared to conventional pulp tester.
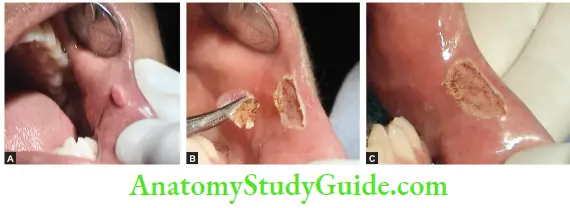
Pulp Capping and Pulpotomy
The first laser pulpotomy was performed by Shoji using CO2 lasers in 1985.
Following this, studies have been done using Nd: YAG, Ga–As semiconductors,s, and Ar lasers.
Lasers have the advantages of less chair-side time, noninvasive and enhanced patient cooperation
1. Indirect pulp capping: Commonly used lasers are Nd: YAG, Ga–As, argon laser, and CO2 lasers
2. Direct pulp capping: Commonly used lasers for direct pulp capping are CO2, Nd: YAG, argon, and Er: YAG laser.
- Advantages of laser-assisted root canal treatment over conventional root canal treatment
-
- Laser-assisted treatment is precise and more accurate
- Causes reduction of ≥99.7% bacterial count from root canals
- It causes better disinfection of the canals
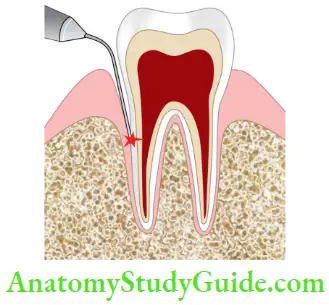
- Laser has the ability to reach and clean the accessory canal, so the sealer can penetrate and can cause a better seal of the root canal
- It is less aggressive than the conventional method, resulting in less bleeding, reduced inflammation, less postoperative discomfort, and less infection
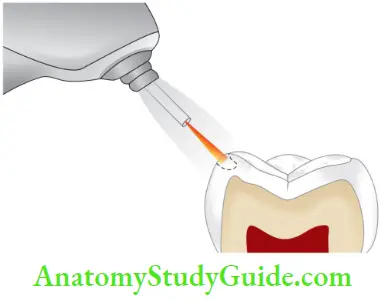
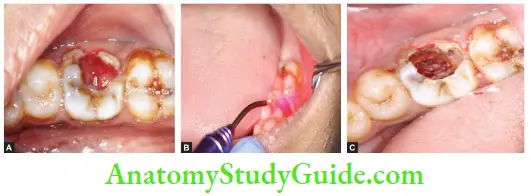
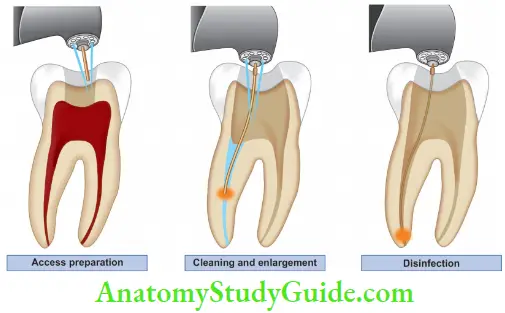
3. Root canal treatment:
- Modification of root canal walls: Laser is used for the removal of the smear layer and its replacement with the uncontaminated chemical sealant or sealing by melting the dentinal surface. The removal of smear layer and debris by lasers is possible; however, it is hard to clean all root canal walls because the laser is emitted straight ahead, making it impossible to irradiate lateral wall
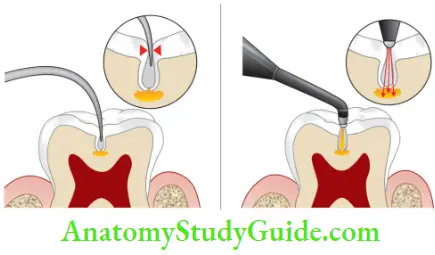
- Sterilization of root canals:
- Traditionally, endodontic techniques use hand and rotary instruments along with irrigants to clean, shape, and disinfect the root canal system.
- Nowadays, laser energy is used to increase cleaning ability, remove the smear layer, and for disinfect of the root canal system.
- Studies have shown that the efficiency of lasers increased in combination with 5.25% sodium hypochlorite and 17% EDTA and 10% citric acid.
- The use of chelating agents facilitates the laser light to penetrate deep into dentinal walls up to 1 mm depth.
- This is known as laser-activated irrigation which is considered to be more effctive than traditional techniques and ultrasonic methods.
- Commonly used lasers for sterilization are Nd: YAG, argon CO2, Er: YAG, and semiconductor diode
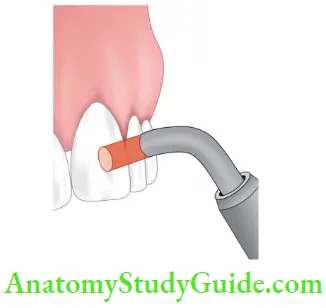
- Photoactivated disinfection (PAD): It uses photodynamic therapy or light-activated therapy. It is a combination of photosensitizing dye and a laser beam which kills bacteria, destroys collagen and carious dentin
- Root canal shaping and obturation: Ar, CO2, and Nd: YAG lasers are used to soften gutta-percha for vertical compaction. Obturation with AH plus and composite resin is activated with argon lasers. Lasers initiate photopolymerization by activation of composite resin.
4. Treatment of incomplete fracture: Lasers are using in repairing incomplete vertical fractures by causing fusion of the fracture.
5. Apicoectomy:
- If laser is used for surgery, a bloodless surgical field is easier to achieve. If the cut surface is irradiated, it gets sterilized and sealed
- Clinically, the use of Er: YAG laser resulted in improved healing and diminished postoperative discomfort.
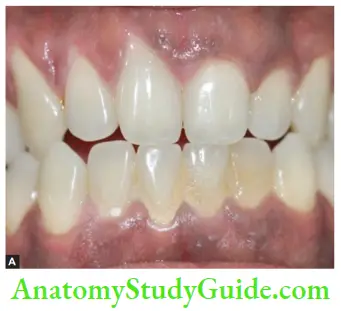
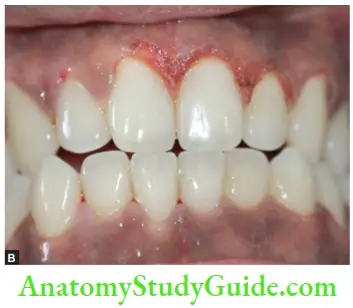
6. In periodontology: It causes a bacterial reduction in gingival pockets before root planning and decontamination of the root canals after root planing, crown lengthening, and depigmentation procedures.
7. Treatment of dental hypersensitivity: Th lasers used for the treatment of dental hypersensitivity are divided into two groups:
- Low output power lasers (He–Ne and Ga, Al, As lasers)
- Middle output power lasers (Nd: YAG and CO2 lasers)
- In case of low-output power lasers, a small fraction of the laser energy is transmitted through enamel or dentin to reach the pulp tissue. He: Ne laser affects the peripheral Ad or C-fier nociceptor
- Laser energy of Nd: YAG is indicating thermally mediated effects and pulpal analgesia. Using CO2 lasers mainly seals the dentinal tubules as well as reduces the permeability.
8. Sterilization of instruments: Argon, CO2, and Nd: YAG lasers have been used successfully to sterilize dental instruments.
9. Teeth whitening: The whitening effect of the laser is achieved by a chemical oxidation process. Once the laser energy is applied, H2O2 breaks down to H2O and free O2 radical which combines with and thus removes stain molecules. The energy of the CO2 laser is emitted in the form of heat. This energy can enhance the effect of the whitening after the initial argon laser process.
Lasers In Endodontics Conclusion
- If used cautiously and ethically, lasers have been an essential tool in many dental treatments. With the introduction of lasers in dentistry, complex procedures have become easier and time-saving.
- This the ability to care for patients has improved. With the development of thinner, more flexible, and durable laser fiers, its applications are increasing in endodontics.
- A further area of future growth is expected to be a combination of diagnostic and therapeutic laser techniques.
- Looking to the future, it is expected that laser technologies will become an indispensable part of dental practice over the next decade.
Leave a Reply