Lower Gastrointestinal Bleeding
Lower Gastrointestinal Bleeding Introduction
Lower gastrointestinal (LGI) bleeding refers to bleeding which occurs beyond the ligament of Treitz. Bleeding per rectum may be a manifestation of upper GI bleeding (UGIB), the causes of which have been discussed under haematemesis.
Table of Contents
In this chapter, bleeding per rectum due to lower GI causes will be discussed. LGI bleeding accounts for 1% of acute hospital admissions each year. Severe bleeding is that which continues for 24 hours after hospital admission or that which recurs 24 hours after resolution.
Read And Learn More: Gastrointestinal Surgery Notes
In all, so-called lower GI bleeding—rule out 3 important causes of upper GI bleeding, namely—oesophageal variceal bleeding due to portal hypertension, peptic ulcers—mainly duodenal ulcer bleeds and acute erosive gastritis or acute gastric mucosal lesions (AGML).
Bleeding from these causes can be so massive, they result in fresh bleeding per rectum, thus adding confusion at the diagnosis. A nasogastric tube lavage that yields blood or coffee-ground-like material confirms the diagnosis of upper GI bleeding.
Lower Gastrointestinal Bleeding Definition
Haematochezia: Bloody stools (LGIB or rapid UGIB).
Melaena: Black tarry stools from digested blood. The duration of bleeding is more than 8 hours
Massive GI tract bleeding: The bleeding which requires more than 3 units of blood transfusions in 24 hours or 25% of intravascular blood volume loss.
Obscure: Bleeding which persists or recurs after initial evaluation has failed (with EGD and colonoscopy).
Obscure Two types:
- Obscure occult: Iron deficiency anaemia, faecal occult blood positive, no visible bleeding. More than 80% resolve with no treatment.
- Obscure overt: Recurrent and visible bleeding, e.g. angiodysplasia.
Investigating a case of lower GI bleeding is like investigating a ‘crime’ by CBI officer. One should not jump to conclusions as soon as one cause of bleeding is found. There are innumerable examples of ‘piles’ being treated for bleeding, totally missing a growth above in the rectum.
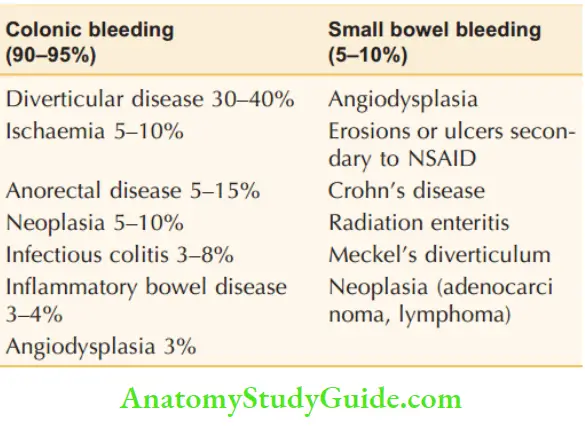
Differential Diagnosis of lower GI bleeding incidence:
Lower GI Bleeding Common Causes
- Most originate in the colon or rectum—haemorrhoids, polyps, carcinoma, and inflammatory bowel diseases are common causes.
- 10% from the upper intestinal tract.
- Small intestinal haemorrhage is usually due to arteriovenous malformations (angiodysplasia), accounting for 70–80%.
- Jejunal diverticula, Meckel’s diverticula, neoplasia,
- Crohn’s disease, and aorto-enteric fistula following a previous aortic graft are other causes of bleeding from small intestines.
Lower GI Bleeding Types
- Depending upon the source:
- Small bowel bleed—5%
- Colonic bleed—95%
- Depending upon the clinical manifestation:
- Melaena: Passage of black tarry stools (altered blood) due to slow bleeding or a more proximal source of the bleed.
- Haematochezia: Passage of bright red stools with or without clots.
Bleeding Per Rectum with Acute Abdomen
- Mesenteric ischaemia
- Intussusception
- Ischaemic colitis
- Necrotising enterocolitis
Lower Gastrointestinal Bleeding Causes
Depending on Aetiology
1. Congenital:
- Polyps: Congenital polyp, Peutz-Jeghers syndrome, familial polyposis coli (FPC)
- Meckel’s diverticulum
- Hereditary haemorrhagic telangiectasia (HHT)
2. Inflammatory:
- Tubercular ulcers
- Enteric ulcers
- Crohn’s ileocolitis
- Ulcerative colitis
- Necrotising enterocolitis
- Dysentery—amoebic, bacillary, Strongyloides infestation
3. Neoplastic:
- Papilloma of rectum
- Carcinoma colon, rectum
- GIST
- Lymphoma
- Carcinoma small bowel
4. Vascular:
- Angiodysplasia
- Ischaemic colitis
- Vasculitis—polyarteritis nodosa
- Haemangioma
5. Clotting disorders:
- Haemophilia
- Thrombocytopaenia
- Leukaemia
- Warfarin therapy
- Disseminated intravascular coagulopathy
6. Miscellaneous:
- Piles, anal fissure
- Prolapse
- Injury to the rectum
- Diverticular disease
Depending on Site of Bleeding
1. Small intestine:
- Peutz-Jeghers polyps
- Meckel’s diverticulum
- Tubercular ulcers
- Crohn’s ulcers
- Leiomyoma
2. Large bowel:
- Angiodysplasia right colon
- Carcinoma colon
- Ulcerative colitis
- Dysentery
- Diverticular disease
3. Anorectal conditions:
- Piles
- Prolapse rectum
- Fissure in ano
- Anorectal conditions
- Piles
- Prolapse rectum
- Fissure in ano
- Fistula in ano (rare)
- Injuries to the rectum
Lower Gastrointestinal Bleeding Clinical Examination
1. Age of the patient:
- Children and young boys: Polyps, Meckel’s diverticulum, necrotising enterocolitis.
- Young age group: Piles, tuberculosis, Crohn’s, dysentery.
- Middle and old age: Carcinoma, piles, prolapse, diverticular disease.
2. Colour of blood:
- Bright red: Piles, fissures, polyp.
- Altered blood: Carcinoma, tubercular ulcer, Crohn’s colitis, dysentery.
- Maroon colour: Meckel’s diverticulum.
3. Blood with mucus:
- Intussusception
- Dysentery
- Inflammatory bowel diseases
- Carcinoma
4. Other special features:
- Severe pain with bleeding: Anal fissure
- Splash in the pan: Piles
- Red currant jelly stools: Intussusception
- Streaks of blood: Anal fissure
- Bloody slime: Carcinoma rectum
- Blood with cherry-red mass coming out: Piles, polyps.
5. Palpable mass abdomen:
- Hard mass in the colon: Carcinoma colon.
- Firm to hard mass in the right iliac fossa: Ileocaecal tuberculosis.
- Contracting mass: Intussusception.
6. Rectal examination:
- Very painful: Anal fissure
- Pedunculated mass: Rectal polyp (juvenile polyps)
- Ulcerations in the rectum: Solitary rectal ulcer
- Indurated ulcer or growth: Carcinoma rectum
7. Evidence of bleeding tendencies”
- Purpuric spots
- Haematoma
Lower Gastrointestinal Bleeding Investigations
1. Proctoscopy:
- Cherry red to pink mucosal bulges: Haemorrhoids
- Bleeding ulcer or a growth: Cancer of the rectum
- Single anterior ulcer: Solitary ulcer rectum.
2. Sigmoidoscopy:
- Multiple small pinpoint ulcers: Ulcerative colitis
- Large deep flask-shaped ulcer: Amoebic ulcers
- Multiple small polyps: Hereditary polyposis coli.
3. Colonoscopy:
- It is the gold standard investigation for lower GI bleeding. It can detect 3 important diseases:
- Carcinoma, inflammatory bowel diseases (IBDs) and diverticular diseases. It can also detect ischaemic colitis, polyps and angiodysplasia. It needs to be repeated.
- In massive bleeding, it can really tax an expert colonoscopist also.
- Colonoscopic adrenaline injections, snaring and coagulation (argon plasma coagulation) are therapeutic advantages.
4. Barium enema:
- Irregular filling defect in the colon: Cancer colon.
- Contracted pipe-stem colon: Ulcerative colitis.
- Pincer ending: Intussusception.
- Saw-tooth appearance: Diverticular disease




5. Stool examination:
- Amoebiasis, bacillary dysentery
- Hookworm infestations.
6. Small bowel enema (enteroclysis) :
- The diverticulum in the terminal ileum is Meckel’s diverticulum. Multiple ulcers and stricture terminal ileum can be due to tuberculous ulcer.
- Barium studies have little value in the presence of acute haemorrhage. They can be used in intermittent or chronic bleeding wherein endoscopy has failed to detect the cause.
Differential Diagnosis Of Lower GI Bleeding














Special Investigations
They are indicated when the diagnosis of lower GI bleeding cannot be made out. They are more useful where there is active bleeding or obscure bleeding.
1. Radionuclear Scanning:
- 99mTc-labelled sulphur colloid or autologous red cells with 99mTc may be given which can detect the bleeding site. It is extremely sensitive, can detect as little as 0.1 ml/min of bleeding.
- Less precise but less invasive with the least complications. If a 99mTc-tagged RBC scan is positive, then an angiogram is used to localise the bleeding site.
2. Visceral Angiography:
- All three vessels—coeliac, superior mesenteric and inferior mesenteric arteries are used.
- Extravasation of contrast into the bowel lumen is suggestive of a ‘lesion’.
- Bleeding rate should be at least 0.5 ml/minute.
- Thus, Meckel’s diverticulum, angiodysplasia, small bowel tumours, vasculitis, etc. can be diagnosed.
3. Capsule Endoscopy:
Capsule Endoscopy Definition:
- It is an investigation wherein a small camera pill is swallowed to study the entire GI tract, in particular, small intestines. This ‘camera pill’ that is swallowed is disposable.
- It weighs 4 grams and is 26 mm × 11 mm in size. Parts: Video camera, lens, colour camera chip, 6 light emitting diodes. As it passes through the entire gastrointestinal tract, images are taken.
- Capsule endoscopy is useful to detect (observe) small intestinal bleeds that are missed by routine upper GI scope and colonoscopy. The procedure takes a very long time for detection of the lesions
- Such bleeds are called ‘obscure’ bleeds. These are very difficult problems to treat because they tend to recur.

Capsule Endoscopy Procedure:
- Patient should be fasting overnight.
- The patient swallows the pill.
- Capsule camera sends signals and pictures—2 pictures/second are taken.
- The capsule gets deactivated in 8 hours and is passed out in stools.
- The receiver tied over the patient’s waist receives signals and ‘endo’ pictures. This is connected to computer software and pictures are obtained.
Capsule Endoscopy Drawbacks:
- Biopsy of the lesion cannot be taken.
- It cannot detect motility disorders which are very important in GIT.
- Expensive, not available in many centres.
- Capsule retention resulting in obstruction can occur
Capsule Endoscopy Conclusion:
- Thus it can detect polyps, inflammatory bowel disease (Crohn’s disease), ulcers and tumours of the small intestine.
- Capsule endoscopy is an excellent tool in the patient who is haemodynamically stable but continues to bleed. Reported success rates as high as 90% in identifying small bowel pathology.
- It is usually well tolerated, although it is contraindicated in patients with obstruction or a motility disorder.
4. Push Enteroscopy
- It employs a 400 cm scope which is ‘pushed’ (hence push enteroscopy) through the duodenum, through DJ flexure into the intestines. It needs lots of skill and expertise.
- It can detect leiomyoma of the jejunum, small intestinal diverticular bleeds causing chronic anaemia, etc.
- Extended enteroscopy is the same as enteroscopy but may take 6–8 hours till the scope travels distally with peristalsis. Up to 70% small intestine can be visualise
Role Of Colonoscopt /Enteroscopy










Massive Lower GI Bleeding
Massive lower GI bleeding is defined as a haemorrhage distal to the ligament of Treitz that requires more than 3 units of blood in 24 hours
Lower GI bleeding Common Causes
Diverticular disease, inflammatory bowel diseases, angiodysplasia, Meckel’s diverticulum, haemobilia, etc.
Signs of hypovolemia:
- Mild to moderate hypovolemia: Resting tachycardia.
- Blood volume loss of at least 15%: Orthostatic hypotension (a decrease in the systolic blood pressure of more than 20 mmHg or decrease in diastolic pressure of more than 10 mmHg when moving from recumbency to standing).
- Blood volume loss of at least 40%: Supine hypotension.
Lower GI bleeding Diagnosis:
Diagnosis is established by colonoscopy, RBC-tagged scan and angiography in most of cases.
Lower GI bleeding Treatment
- Initial aggressive resuscitation by fluids, blood transfusion and treatment of shock.
- Emergency colonoscopy and vascular malformations, if detected, can be treated by argon plasma coagulation or by cauterisation.
- Therapeutic vasopressin infusion 0.2 units/minute via angiographic catheter with or without embolization will stop or arrest the lower GI bleeds in more than 85% of cases.
- Unstable patient should be subjected to urgent laparotomy.

A Few Important Tips at Exploratory Laparotomy:
- A midline incision is preferred. Careful inspection and palpation of entire small and large bowel.
- Empty small bowel. Then palpate for hidden lesions.
- Intraoperative enteroscopy, if no obvious lesion is found.
- Endoscopic evaluation of transilluminated gut wall.
- On-table colonoscopy via appendiceal opening after appendicectomy.
- Rarely, blind right hemicolectomy/subtotal colectomy or blind resection of proximal jejunum may be necessary in obscure bleeding (keeping in mind angiodysplasia).
Lower Gastrointestinal Bleeding Differential Diagnosis
All the topics related to GI bleeding have been discussed in the respective chapters. Summary and important causes of the GI bleeding are given here.
1. From the Colon
1. Haemorrhoids:
- These are the common causes. They cause a splash in the pan. It is painless, fresh bleeding. It is one of the differential diagnoses for anaemia.
- Diagnosis is by proctoscopy—as cherry red spongy masses.
- Sigmoidoscopy is done to rule out proximal carcinoma. Treated by haemorrhoidectomy.
2. Fissure in ano:
- A severe painful condition of the anal canal, results in constipation, hard pellet-like stools and drop of blood.
- Treated by lateral sphincterotomy.
3. Carcinoma rectum/colon:
- Fresh bleeding per rectum, bloody slime, loss of weight, anaemia, mass abdomen in an elderly patient suggests it could be carcinoma rectum/colon.
- Diagnosis is by colonoscopy and biopsy. Treated by colectomy.
4. Haemobilia:
- Rare cause of UGI or LGI bleeding
- Triad of Sandblom: Melaena, biliary colic and obstructive jaundice
- External trauma
- Latrogenic :
- Transhepatic puncture (PTC, stenting)
- Surgery on biliary tree or pancreas
- After dilatation of biliary strictures, etc.
- Endoscopy: Blood emerging from the ampulla of Vater
5. Diverticular disease of the sigmoid colon:
- Common in Western patients, a diet poor in fibre is mostly the cause.
- The diverticuli are acquired herniation of the mucosa, hence thin. Bleeding can be occult/ intermittent or massive.
- Diagnosis is by colonoscopy. To visualise the bleeders, endotherapy can be done by injecting adrenaline into the bleeding vessel. In emergency situations, with massive lower GI bleeding, emergency colectomy is required.
6. Inflammatory bowel diseases:
- Commonly ulcerative colitis and less commonly Crohn’s disease produces lower GI bleeding. Bleeding is intermittent with mucous diarrhoea, weight loss and malnutrition.
- Often patients are young. Diagnosis is by colonoscopy and biopsy.
- Initial treatment is always conservative—salazopyrines, steroids, etc.
- In massive bleeding to save the life—emergency total colectomy with or without pouch may be required. In Crohn’s disease, the aim is always to conserve the segment of the intestine.
- Resection is required, only if massive bleeding is present. This is rare in Crohn’s disease.
7. Angiodysplasia:
Vascular ectasia also called angioma, haemangiomas and arteriovenous malformations are collectively grouped under angiodysplasia. Commonly right side colon, i.e.,caecum and ascending colon are affected. In the small intestines, jejunum is the most common site.
- They are acquired lesions, seen in elderly patients.
- Less rapid, but recurrent.
- The caecum and right colon are common sites—the caecum is the most common site.
- The small bowel (proximal) is the second common site.
- Small red mucosal lesions between 2 and 10 mm, flat or raised lesions—dilated tortuous submucosal veins.
- Recurrent painless and self-limiting bleeding often associated with aortic stenosis—Heyde’s syndrome.
- Colonoscopy is the investigation of choice.
- They can be treated endoscopically—coagulation with heat probe, bipolar electrode or laser, etc. but recurrence or failure can occur.
- Surgery by resecting the segment is a definitive procedure.
- Angiography is rarely positive.
- Enteroscopy, capsule endoscopy and intraoperative
- endoscopy are useful investigation.
- These lesions are seen in acute renal failure, von
- Willebrand’s disease, HHT.
- Hormone treatment.
- Endoscopy-directed resection.
Typically, elderly patients present with intermittent bleeding is the cause of anaemia. Usual causes of lower GI bleeding are ruled out by colonoscopy and other investigations. Suspect angiodysplasia. A few cases present with massive bleeding—a difficult problem to treat. Repeat colonoscopy, capsule endoscopy, angiography, and on-table enteroscopy are taxing investigations—all may provide no results— emergency colectomy or intestinal resection of the suspicious segment may be required.
8. Ischaemic colitis:
- Elderly, hypertensive patients present with diffuse abdominal pain, severe in nature, with blood in stools—it is often massive, sometimes moderate.
- On examination, tenderness may be present on the left side of the colon. Plain X-ray abdomen supine will show thumb printing sign due to mucosal oedema and submucosal haemorrhage.
- CT scan—colonic wall thickening with posterior fat shadowing. A colonoscopy may reveal ulcers or a few changes in the splenic flexure region. If conservative measures fail such as blood transfusion, segmental colectomy may be required.
9. Dysentery:
- Various dysenteries such as amoebic, bacillary, Shigella, HIV related—all produce ulcerations in the colon resulting in blood and mucus in the stools.
- Gripping pain, acute in nature with or without fever and tenderness over the colon—in the right iliac fossa and in the left iliac fossa are suggestive.
- Diagnosis is by stool examination and colonoscopy. Treated with antiamoebic drugs or antibiotics.
9. Irradiation proctitis or telangiectasia:
- Usually occurs with pelvic radiotherapy, for example—radiation is given to treat carcinoma cervix. The most common site is the rectum. Tenesmus, mucus and blood in stool are common.
- Proctoscopy reveals ulceration.
- Treated with stool softening agents, 5-ASA (aminosalicylic acid) topical or steroid enema. Acute irradiation injury occurs within six weeks of therapy.
- Chronic radiation procto-sigmoiditis has a more delayed onset.
- The first signs often occur at approximately 9 to 14 months following radiation exposure but may develop after more than two years in some patients
10. Adenoma, polyps, familial polyposis coli:
- They are common in the colon. All are precursors for carcinoma colon. Often patients are young with lower gastrointestinal bleeding.
- Diagnosis is by colonoscopy and biopsy. Villous adenomas, polyps can be snared or excised. Always histological examination is a must.
2. From the Small Intestines
1. Tubercular ulcers:
- They are never massive bleeders.
- Patients are between 20 and 40 years old with blood and mucus in the stools, loss of weight, crampy abdominal pain, and evening rise of temperature with or without pulmonary tuberculosis.
- On examination, the mass may be palpable, if the caecum is also involved (ileocaecal tuberculosis). Visible step ladder peristalsis indicates obstruction from a tubercular stricture or obstruction due to mass.
- A colonoscopy with visualisation of the terminal ileum and biopsy is the key to the diagnosis.
- Obstructed cases can be treated with stricturoplasty in a single stricture or resection in appropriate cases. Cases without obstruction are treated with antitubercular treatment.
2. Crohn’s ulcers:
- The ileum is the commonest site—rest of the bowel can also be affected.
- Transmural inflammation, multiple ulcers, and skip lesions are other features.
- Diagnosis is by CT scan, push enteroscopy and biopsy. Treatment is as for ulcerative colitis
3. Enteric ulcers:
- High grade fever—enteric fever patient who has bleeding after 15 days of fever may be having enteric ulceration of the Peyer’s patches with bleeding.
- In majority of the cases, bleeding is occult and usually stops once the disease is treated, rarely exploration and resection of the segment may be required in cases of massive bleeding cases.
4. Meckel’s diverticulum:
- Children or young patients, often bleeds are intermittent, maroon coloured with or without abdominal pain. Peptic ulceration in the ectopic mucosal site in the Meckel’s diverticulum causes bleeding.
- Colonoscopy is normal. RBC-tagged technetium scan is the investigation of choice. It can pick up as little as 0.1 ml/min of bleeding. Exploration and excision of the Meckel’s diverticulum is the treatment of choice.
5. Angiodysplasias:
- Small intestines are the most common sites of angiodysplasia.
- They are the differential diagnoses for obscure bleeds.
- Angiogram and small bowel push enteroscopy, capsule endoscopy are the investigations. Diagnosis is by exclusion.
6. Small bowel tumours:
- They are uncommon causes of lower GI bleeding. They have to be kept in mind when the common causes described above are ruled out one by one.
- Adenocarcinoma, lymphoma and stromal tumours (GIST—gastrointestinal stromal tumours) are a few examples. GIST can affect the small intestine.
- The mucosal ulcerations cause GI blood loss. Bleeding is not massive—can be intermittent and result in anaemia. Palpable mass sometimes massive which is bosselated, anaemia and bleeding are the triad of GIST.
- CT scan is the investigation of choice.
- Resection almost cures the disease. The degree of malignancy is decided by the mitotic figures in pathology.
- Imatinib is the drug used in recurrent cases of GIST or GIST with metastasis. Patients with liver metastasis will live beyond 5–10 years with imatinib.
Lower Gastrointestinal Bleeding Miscellaneous
Ischaemic Colitis
- Ischaemic colitis is a non-inflammatory condition affecting splenic flexure region resulting in ischaemia and lower GI tract bleeding.
- Elderly hypertensive patients are commonly affected.
- Often they are males.
- The splenic flexure region can have relative vascularity.
- The exact point is called Griffith’s point.
- It is defined as the site of (1) communication of the ascending left colic artery with the marginal artery of Drummond, and (2) anastomotic bridging between the right and left terminal branches of the ascending left colic artery at the splenic flexure of the colon.
- Anastomosis at Griffith’s point is present in 48%, poor or tenuous in 9%, and absent in 43%. Thus, it is important that in cases of ligation of the inferior mesenteric artery, there is a possibility of ischaemia developing in that region.
- It can also be affected in “nonocclusive” ischaemic colitis.

Three types have been classified—called Marston’s classification:
- Gangrenous type
- Stricture type
- Transient type
Clinical Notes:
- A 28-year-old male patient had an urgency to pass stools early morning. He collapsed while passing stools, with massive bleeding. He was brought to the hospital in a state of shock. He was resuscitated and blood transfusions were given. All investigations were normal.
- He had another bout of massive bleeding the next day, during which time, even an angiography could not detect the cause. Urgent laparotomy was done.
- A 4 cm small bowel tumour (haemorrhagic) was excised from jejunum and histology confirmed it as leiomyoma. Leiomyoma is called a bleeding tumour of the small bowel. The case history highlights the importance of exploratory laparotomy. Leiomyomas are included under GIST
Lower Gastrointestinal Bleeding Multiple Questions And Answers
Question 1. Lower GI tract bleeding refers to bleeding
- Below ligament of Treitz
- Below ampulla of Vater
- Below Meckel’s diverticulum
- Distal to ileocaecal junction
Answer: 4. Distal to ileocaecal junction
Question 2. The most important inherited anomaly which produces bleeding is
- Juvenile polyp
- Meckel’s diverticulum
- Familial polyposis coli
- Hereditary haemorrhagic telangiectasia
Answer: 4. Hereditary haemorrhagic telangiectasia
Question 3. The ideal investigation for bleeding Meckel’s diverticulum is
- CT scan
- Colonoscopy
- 99mTc-tagged RBC scan
- Push enteroscopy
Answer: 4. Push enteroscopy
Question 4. The following facts are true for angiodysplasia, except
- They are congenital lesions
- The right colon is the common site
- It is one of the causes of obscure bleeding
- The small bowel is the second common site
Answer: 1. They are congenital lesions
Question 5. The following are true about capsule endoscopy, except
- It is a disposable pill
- Ideal for small intestinal bleeds
- Biopsy can be taken
- Capsule retention can occur
Answer: 3. Biopsy can be taken
Question 6. The following are true for jejunal bleeding lesions, except
- Carcinoma
- Meckel’s diverticulum
- Angiodysplasia
- Hamartomatous polyp
Answer: 2. Meckel’s diverticulum
Question 7. The following are true for haemobilia, except
- It causes melaena
- It causes biliary colic
- Obstructive jaundice
- Splenomegaly
Answer: 4. Splenomegaly
Question 8. Which one of the following is the cause for massive lower GI bleeding?
- Carcinoma rectum
- Crohn’s colitis
- Typhoid colitis
- Diverticulitis of the colon
Answer: 4. Diverticulitis of the colon
Question 9. Which one of these causes bleeding with septic shock?
- Carcinoma colon
- Ulcerative colitis
- Mesenteric ischaemia
- Angiodysplasia
Answer: 3. Mesenteric ischaemia
Question 10. Which one of these causes painless and massive bleeding per rectum?
- Angiodysplasia
- Sigmoid volvulus
- Necrotising enterocolitis
- Mesenteric ischaemia
Answer: 1. Angiodysplasia
Leave a Reply