Lower Limb Ischaemia And Popliteal Aneurysm
Describe the etiopathogenesis, clinical features, investigations and principles of treatment of occlusive arterial disease.
Table of Contents
Lower Limb Ischaemia And Popliteal Aneurysm Introduction
Walking is a fundamental human requirement. Peripheral arterial disease (PAD) is a main cause of disability. Many individuals are conscious of chest pain caused by myocardial ischaemia and arrive at a hospital early.
However, patients present relatively late to the hospital with lower limb ischaemia. The disease, though benign, is not totally curable, causing financial, social, and psychological burdens to the patient and his or her relatives.
Read And Learn More: General Surgery Notes


Causes Of Lower Limb Ischaemia
Occlusion refers to obstruction to the lumen of blood vessels. Examples are atheromatous plaques or a blood clot, etc. Stenosis refers to the abnormal narrowing of the vessel.
- Other rare causes of lower limb ischaemia include popliteal entrapment syndrome and cystic medial degeneration.
- One should not forget that diabetes mellitus is also a common cause of peripheral vascular disease in elderly patients. While treating a patient with atherosclerotic disease, care of diabetes is equally important.
Causes Of Lower Limb Ischaemia

Risk Factors For Peripheral Arterial Disease (Pad)
- Smoking: Smoking in any form increases the risk by almost tenfold. It is proportional to ‘pack-years’ smoked.
- Male (gender): Men are affected 10 years earlier than women.
- Other risk factors: These include hypercholesterolemia (>200 mg/dl), hypertriglyceridaemia, hypercoagulable state (polycythaemia), and hyperhomocysteinaemia.
- Known diabetes: Type 2 diabetes mellitus—increases the risk by two to fourfold.
- Elderly patients between 60 and 70 years are vulnerable.
- Raised blood pressure—hypertension.
- You can remember as SMOKER
Hyperhomocysteinaemia
- It increases the risk of developing PAD by 7%
- Homocysteine levels >15 mmol/L
- Increased levels cause endothelial injury and lead to vascular inflammation
- Defective gene for methylene tetrahydrofolate reductase (MTHFR)
- Prevention is by eating foods containing B6 , B9, B12 and folate, such as potatoes, green vegetables, fish, etc.
- It is also a strong risk for myocardial infarction in young patients.
Collateral Circulation
Collateral circulation is present in most organs. Hence, even if a major vessel is occluded, the organ may still survive provided collaterals are well-developed.
- In acute ischaemia caused by thrombus or embolism, there is no time for collaterals to develop. This results in gangrene of the limb in untreated cases.
- Chronic ischaemia caused by TAO or atherosclerosis allows sufficient time for collaterals to develop. Hence, necrosis or gangrene that occurs is minimised and the limb often survives.


Collateral Circulation Symptoms
1. Pain in the limb is the chief symptom of lower limb ischaemia. It is a severe, cramp-like pain due to ischaemia of the muscles that is brought on mainly by exertion, relieved by rest, and reproducible. It is called intermittent claudication.
Symptoms Grades of intermittent Claudication—Boyd’s classification
- Grade 1: The patient walks for a distance, gets the pain, continues to walk and the pain disappears. As a result of ischaemia, anaerobic metabolism takes place, which produces substance P, lactic acid, etc. These produce vasodilatation and the pain disappears.
- Grade 2: The patient walks for a distance, gets the pain and continues to walk with the pain. He has a limp.
- Grade 3: The patient walks and gets the pain. He has to take a rest. This grade indicates severe muscle ischaemia.
- In late stages: Pain at rest is due to ischaemia of nerves in addition to ischaemia of the muscles.
- Cry of the dying nerves, due to involvement of vasa nervosum Pain is due to ischaemic neuropathy involving small unmyelinated A, delta and C sensory fibres.
The most common site of obstruction is the superficial femoral artery which results in classical calf muscle claudication.
- Blood supply to the great toe comes from the dorsal pedal artery and a branch from the medial plantar artery, a branch of the posterior tibial artery.
- When these are affected, it results in instep claudication. The muscle affected is the extensor hallucis longus.
Symptoms Superficial Femoral Artery Stenosis or Occlusion
- It is the most common cause of intermittent claudication
- Usually, calf muscles are affected
- Does not produce life-threatening ischaemia unless profunda femoris is involved.
- Single stenosis less than 3 cm is treated by Percutaneous Transluminal Angiography (PTA)
- Rest pain: It is an intractable type of pain usually felt in the foot (instep), toes, etc. It is an indication of severe ischaemia of the foot with impending gangrene. Rest pain is increased in the night because of reduced sympathetic drive, which in turn results in decreased cardiac output and tissue perfusion.
- Typically, a patient with rest pain sits on the bed, holds his foot with both hands or hangs his foot off the bed. This gives him some kind of relief. Rest pain is worse at night. It may lead to suicidal tendencies.
- Claudication distance refers to the distance a patient is able to walk before the onset of pain. A patient with severe claudication may not be able to walk even a few yards.
The site of claudication depends on the level of arterial occlusion.
Site Of Occlusion And Claudication

list other causes of pain in the leg.
Important causes of pain in the leg

Symptoms Pain in the leg—other causes

Intermittent claudication in a young patient may be due to some rare causes such as:
- Popliteal artery entrapment due to the abnormal origin of the gastrocnemius muscle
- Cyst in the media of the popliteal artery
- Hyperhomocysteinaemia
2. Nonhealing ulcer is the next commonly presenting symptom. It is usually precipitated by minor trauma and occurs in the most distal part of the body, such as the tip of the toes. Ischaemic ulcers are deep and very painful.
3. Some patients present with gangrenous patches of skin or subcutaneous tissue. Gangrene affects distal parts such as the toes. However, gangrene is minimal because of collaterals.

4. A history of bilateral gluteal claudication with impotence may occur in a young patient due to a saddle thrombus at the bifurcation of the aorta. This is called Leriche’s syndrome, which presents as a triad of claudication, erectile dysfunction, and decreased distal pulses.
- Impotence is due to failure to achieve an erection due to paralysis of the L1 nerve. Gluteal claudication is confused for sciatica and many patients are referred to the orthopaedic department.
- Sciatica causes neurogenic claudication, which is present even at rest and is aggravated by movements of the spine. Causes of neurogenic claudication include slipped discs, fractured vertebrae, tuberculosis of the spine, etc.
5. Coldness, numbness, paraesthesia, and colour changes indicate chronic ischaemia.
6. The majority of patients with peripheral vascular disease are smokers. TAO occurs exclusively in male smokers.
Chronic Lower Limb Ischaemia Classification
Fontaine and Rutherford also categorised chronic lower limb ischaemia into 6 different categories ranging from asymptomatic to major tissue loss.
Clinical Classification Of PAOD

Claudication is classified as either mild, moderate, or severe based on treadmill response and ankle pressure (AP).
- Mild: Completes treadmill test. AP is >50 mmHg after exercise.
- Moderate: Cannot complete treadmill test. AP after exercise is <50 mmHg.
- Severe: Resting AP <40 mmHg (cannot complete treadmill test).
- Normal segmental systolic arterial pressures (mmHg)
- Arm – 120
- Upper thigh – 160
- Above knee – 150
- Below knee – 140
- Ankle – 130
Classification Diagnostic criteria of TAO: = Shionoya criteria
- Age at onset <50 years
- Smoking history +
- Distal extremity ischaemia, upper limb involvement, phlebitis migrants
- Typically, infrapopliteal occlusions
Chronic Ischaemia Clinical Examination Inspection
The findings are appreciated better if a comparison is made with the opposite limb. Evidence of chronic ischaemia of the leg includes:
- Attitude of the limb: Very often, the patient holds the calf muscles or dorsum of the foot.

Commonly asked question—why does the patient hold his legs and hang them off the bed?
- Venous stasis and reflex vasodilatation.
- He compresses the muscles with his hands which may also help in venous return.
- The warmth of the hands is transferred to the limb. These are explanations given by many experienced senior examiners and teachers. I request the student to verify these explanations.
- Gravity-assisted blood flow.
- Flattening of the terminal pulp spaces of toes
- Fissures and cracks between the toes
- Ulceration of toes, interdigital ulcers
- Brittle, flat, and ridged nails, shiny skin
- Loss of hair and subcutaneous fat
- The limb may appear more dark in dark-skinned patients or markedly pale in fair-skinned patients with vasospastic diseases such as TAO.
- Gangrene is usually dry with a clear line of demarcation. It indicates the junction of dead and living tissue. Since the blood supply to the muscle is better, usually the line of demarcation involves skin and subcutaneous tissue.
- The line of demarcation is very well appreciated in senile gangrene, where it may be skin, muscle, or bone-deep.
- The limb may show muscle atrophy.
- Multiple toes and finger involvement suggest vasculitis.

Clinical Examination Palpation
1. Ulcer: Examination should be done as described. Ischaemic ulcers are very tender.
2. Gangrene: It is described according to its size, shape, and extent. In dry gangrene, the part is dry and mummified or shrunken. Features of dry gangrene are summarised.
Clinical Examination Gangrene
- Loss of temperature
- Loss of pulsation
- Loss of sensation
- Loss of colour
- Loss of function
3. Limb above
- Ischaemic limb is cold: Careful palpation from above downwards will reveal the change in temperature from warm to cold. Temperature changes are better appreciated with the dorsum of the hand because it has many cutaneous nerve endings.
- Tenderness: It is tender due to the presence of inflammation.
- Sensation: Ischaemic limb is hypersensitive, due to irritation of the nerve endings.
- Pitting oedema may be due to thrombophlebitis or due to nonfunctioning of the limb.
- Feel pulses in all four limbs and in the head and neck region.
4. Palpation of pulses
Examination Of Peripheral Vessels

After examining the pulses, results are interpreted in a pulse chart as shown.

In a similar manner, upper limb pulses and head and neck pulses are also recorded in the pulse chart.
Clinical Examination Disappearing pulse: When collateral circulation is very good, peripheral pulses may be normal.
- However, when the patient is asked to exercise, the pulse may disappear.
- Exercise produces vasodilatation below the obstruction and arterial inflow cannot keep pace with the increasing vascular space. Hence, the pressure falls and the pulse
disappears.
Clinical Examination Other Tests Of Minor Importance
1. Buerger’s postural test is relevant in fair-skinned patients. The patient (supine) is asked to raise his legs vertically upwards keeping the knees straight. In cases of chronic ischaemia, marked pallor develops within 2–3 minutes.
The angle at which pallor develops is Buerger’s angle of circulatory insufficiency. In an ischaemic limb, pallor develops even on the elevation of the leg by 15–30°.
2. Capillary refill test: Apply pressure over the tip of the terminal pulp space for a few seconds and release the pressure. Rapid return of circulation is observed in normal persons (<2 seconds).
- The test may also be done on the ischaemic foot by asking the patient to sit up and hang his legs down and observing for colour changes.
- The time taken for the ischaemic foot to become pink is described as the capillary filling time. This is prolonged in an ischaemic foot.
Clinical Examination Auscultation
- Systolic bruit over the femoral artery may be heard in atherosclerotic occlusion of the iliofemoral segment due to turbulence created by the blood flow.
- Auscultation of the heart to rule out mitral stenosis (mid-diastolic murmur, loud S1).


Lower Limb Ischaemia Differential Diagnosis
Even though there are many causes of lower limb ischaemia, thromboangiitis obliterans (TAO) and atherosclerotic vascular disease are the most common causes.
- Hence, they should be considered before giving other diagnoses.
- TAO is also called Buerger’s disease. The details are given.
- Atherosclerotic vascular disease is the most common cause of lower limb ischaemia. It may manifest from a simple ulcer to massive gangrene.
Differential Diagnosis

Differential Diagnosis Checklist of Features of Chronic Lower Limb Arterial Occlusion
- Cold and numbness
- Limb elevation: Slow venous refilling. The line of demarcation present
- Altered/diminished sensation
- Ulcerations
- Dead toe—gangrene—dried and mummified
- Intractable pain—rest pain
- Cracks, fissure—interdigital
- Arterial pulsations decreased or absent
- Thrill/bruit may be present
- Intermittent claudication
- Oedema—if thrombophlebitis or cellulitis occurs
- Narrow calf muscle girth—muscle atrophy
- Remember as CLAUDICATION
Differential Diagnosis Classification of Buerger’s Disease
- Type 1: Upper extremity
- Type 2: Crural (leg and foot)
- Type 3: Femoral type—femoropopliteal
- Type 4: Aortoiliac
- Type 5: Generalised type
Differential Diagnosis Buerger’s Disease—Summary
- Male smoker
- Progressive, nonatherosclerotic, segmental, occlusive, inflammatory condition
- Occlusion of small- and medium-sized vessels, superficial thrombophlebitis and Raynaud’s phenomenon constitute the ‘triad’ of TAO.
- Microabscesses, polymorphs, and giant cells (pathology) are found.
- Distal, infrapopliteal, segmental occlusion with skip lesions and corkscrew collaterals in the angiogram.
- Stop smoking
- Start analgesics
- Lumbar sympathectomy is of some value
- Keywords can be remembered as PRISON
- Progressive, I inflammatory, Segmental, Occlusive, Nonatherosclerotic
Chronic Lower Limb Ischaemia Management
Management Investigations
1. Complete blood picture: Anaemia delays wound healing and decreases tissue perfusion. A high total count indicates secondary infection.
- Elevated platelet count suggests a risk of thrombosis.
- Fasting blood glucose and glycosylated haemoglobin. HbA1c is an important test as it reflects the duration of diabetes.
- Increased creatinine indicates renal disease.
2. Lipids: Fasting total cholesterol, high-density lipoprotein, low-density lipoprotein, and triglyceride concentration—hyperlipidaemia should be controlled to prevent the progression of peripheral arterial disease and death from coronary artery diseases.
3. Hypercoagulable status:
Protein C deficiency is identified as a risk factor for arterial thrombosis, especially in patients who will be treated with heparin.
- Heparin-induced platelet aggregation and heparin-induced thrombocytopenia.
- Antiphospholipid antibody (APLA) syndrome (APLS) is also called Hughes syndrome. It is an autoimmune hypercoagulable state resulting in thrombosis of veins (deep vein thrombosis), thrombosis of the artery (stroke), and pregnancy-related complications. It is treated with aspirin and heparin.
- Homocysteine levels (4 to 15—normal, >15 mmol/L can be dangerous).
4. Hand-held Doppler ultrasound blood flow detector: This is an extension of clinical examination. This test is based on the Doppler principle. An ultrasound signal is beamed at an artery and the reflected beam is picked up by a receiver.
- Frequency changes of the beam due to moving blood are converted into audio signals which may be heard by a probe. Thus, a Doppler probe may be used to detect the pulse even when the pulse is clinically not palpable.
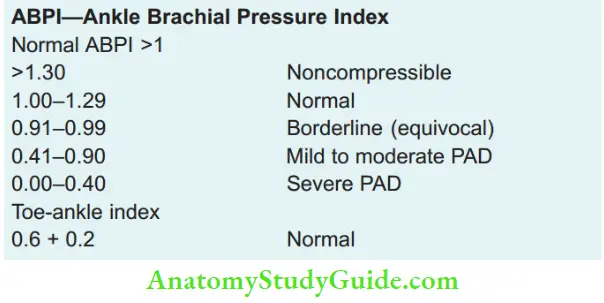
- Using a sphygmomanometer, systolic blood pressure (SBP) of the limb can be measured by positioning the cuff at a suitable level and the pressure index can be calculated. This is called the ankle-brachial index (ABPI).

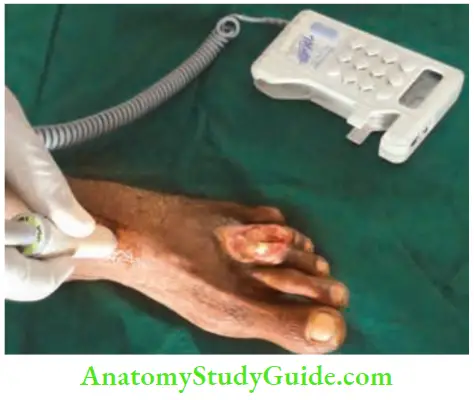



Normal values are >1. However, in patients with peripheral vascular disease of the lower limb, the values are <1 (indicative of vascular obstruction).
- In diabetic patients, ABPI may be increased due to arteriosclerosis. In such patients, the pressure is measured. If toes are not available (postoperative status), transcutaneous oxygen tension (TcPO2) should be measured instead.
- Normal toe pressure is 20–40 mmHg less than ankle pressure.
- <30 mmHg of toe pressure is associated with ischaemic symptoms.
- Foot ulcers heal only if the pressure is >30–40 mmHg.
- When ankle pressure is <30 mmHg, gangrene may be imminent.
Management Uses Of Doppler Probe
- To detect normal pulses in operation theatres
- To detect a clinically nondetectable pulse in peripheral vascular disease
- To measure BP (blood pressure) in ischaemic limbs
- To remeasure BP in the lower limb after exercise to differentiate ischaemic claudication from neurogenic claudication
5. Duplex scan
Duplex ultrasound involves using high-frequency sound waves to look at the speed of blood flow. This is the investigation of choice today. Duplex scan is a combination of Doppler and B-mode ultrasound.
- B-mode ultrasound is used to obtain the image of the vessel, and Doppler is used to evaluate the direction and velocity of the blood flow of the vessel. Colour Duplex allows for the assessment of blood flow direction.
- Red colour indicates that the direction of blood flow is towards the transducer, whereas blue colour indicates that the direction of blood flow is away.

Management Duplex Imaging Scan
- It yields both anatomic and blood flow information
- No nephrotoxic contrast agent is used
- It gives a triphasic wave pattern systolic, diastolic and elastic recoil
- Elastic recoil is absent in calcified arteries
- Thus biphasic and monophasic wave patterns indicate ‘PAD’
- Overall sensitivity of 92% and specificity of 99% in occlusive cases
- Limiting factors are extensive ulcers, calcification and oedema of the leg
6. Computed tomography angiography (CTA)
For all patients with chronic limb ischaemia, if revascularisation is planned by surgical or interventional methods, CTA is done. Here, 4 contrast–iodine about 300–400 mg/mL is used. An average of about 130 mL of contrast is used.
- Interpretation of CTA is always based on the axial images. Hydration of the patient should be adequate, and creatinine should be normal, or else renal failure may occur.
- Advantages of CTA: It gives the vascular anatomy, collaterals, variations (if any), and reformation of the vessels. The most important advantage of CTA over duplex scan is to get the exact information of the level of the block, length of occluded segment stenosed or segment, and distal runoff.
- This forms the basis of revascularisation procedures.
- CTA is the choice of investigation to assess intrathoracic vessels.
- Because of these advantages and the ease of the procedure, conventional angiogram using Seldinger’s technique (details given below) is not done for limb ischaemia.
- Catheter angiography—a catheter is inserted into an artery and advanced to the area of the probable blockade, contrast is injected and using DSA, vessels are visualised. This is used more for the therapeutic purpose of thrombolysis or dilatation of stenosed segments of the arteries.


7. Seldinger’s technique: Today it is done to assess cerebral circulation (percutaneous transfemoral method). An incision is made in the upper thigh to expose the femoral artery on the normal side.
- A Seldinger needle and guidewire are used to introduce the arterial catheter, and a radiopaque dye is introduced after placing the catheter into the aorta. It visualises the entire aortoiliac segment and below.
- Since the catheter is passed from the femoral artery into the aorta, it is also called the retrograde method. When a conventional angiogram is done, subtracting soft tissues bones etc., improves the quality of the images.
- This is called digital subtraction angiography (DSA). DSA gives excellent pictures of the carotid and large central vessels.
- Complications of Angiography
-
- Contrast allergy, and anaphylaxis, which can be avoided by a trial injection.
- Paraplegia due to spasms of spinal arteries.
- Infection
- Renal failure
Management Complications of Angiography
- Thrombus
- Rarely paraplegia
- Arterial dissection
- Unexpected infection/sepsis
- Massive bleeding
- Anaphylaxis
- Remember as TRAUMA
8. Magnetic resonance angiography (MRA)
It is more popular than arteriography because of no arterial puncture and no contrast-induced nephropathy.
- It also has no radiation exposure.
- Unlike CTA, MRA is not affected by arterial calcification.
- Gadolinium-enhanced MRA may visualise the entire arterial tree and pattern, including small pedal vessels.
- Patients with newly placed metallic implants are advised to avoid undergoing MRA.
- MRA may overestimate the degree of stenosis because of turbulence, and metal clips may cause artefacts that mimic vessel occlusions.




Treatment Of Peripheral Arterial Disease (Tao And Atherosclerosis)
In all patients with peripheral vascular disease, the following general measures must be taken which will help in better perfusion of the lower limb tissues.
- Anaemia must be treated with haematinics and, if necessary, blood transfusion. If the ejection fraction is low, drugs are given to improve cardiac output.
- Lifestyle modification of decreasing weight, avoiding fat-rich food and control of diabetes.
Treatment Of Peripheral Arterial Disease Principles of Treatment
-
- To relieve the pain
- To arrest the progression of the disease
- Medical treatment
- Surgical methods
1. To Relieve the Pain
As already discussed, the pain is very severe and distressing. Some amount of pain relief may be obtained with:
- Analgesics: Simple analgesics may not help these patients. Paracetamol 650 mg 1 tablet 2–3 times a day, Tramadol (50 mg) one tablet, 3 times a day.
- Narcotic analgesics (used judiciously) in cases with rest pain. Buerger’s position, by elevating the head-end of the bed, causes venous congestion and reflex vasodilatation.
- Buerger exercises by elevation and dependency of the limb for a few minutes. Heel raise by 1–2 cm, to increase claudication distance by decreasing the workload on the calf muscles.
2. To Arrest the Progression of the Disease
- Stop smoking: This is more beneficial in TAO patients than in atherosclerotic patients.
- Supervised walking on a treadmill for 1 hour or more three times a week as an exercise program for 3 months with control of diabetes and cessation of smoking will improve claudication.
- Diet: Avoid fatty foods to reduce serum cholesterol. This is more useful in patients with hyperlipidaemia.
- Avoid injuries.
3. Medical Management
- Cilostazol
- Is the drug of choice in atherosclerotic occlusive disease.
- It is an antiplatelet drug and a vasodilator.
- It helps improve claudication symptoms.
- It helps stabilise atherosclerotic plaques.
- It is a selective inhibitor of phosphodiesterase type 3.
- Aspirin or clopidogrel
- 75 mg/day of clopidogrel or 75 mg of aspirin is advised for all these patients as an antiplatelet.
- It has been shown to reduce the mortality rate due to cardiac events in these patients.
Medical Management Of Peripheral Vascular Disease Drugs, Dosage And Their Role

4. Surgical Procedures
- In TAO: Lumbar sympathectomy and amputations.
- In atherosclerotic arterial disease (aortoiliac disease and femoropopliteal disease): Percutaneous transluminal angioplasty and bypass grafts.
1. Lumbar sympathectomy is the indirect surgery [done for TAO patients since direct arterial surgery is not possible.
- Salient Features of Lumbar Sympathectomy
- Transverse loin incision
- Extraperitoneal approach and it is a preganglionic sympathectomy.
- The Lumbar sympathetic trunk is identified in the paravertebral gutter lateral to the psoas muscle as a cordlike structure.
- 2nd lumbar ganglion is large and has white rami joining it.
- The sympathetic trunk is divided below the first lumbar vertebra and removed up to the 4th lumbar vertebra.
- This is a preganglionic sympathectomy because fibres supplying the vessels of the limb have their cell stations in the sacral ganglia which are not disturbed.
- Indications: Cutaneous ulcer and rest pain.
- Structures which may be confused for the lumbar sympathetic trunk include:
- The genitofemoral nerve
- Tendon strip of the psoas muscle
- The lymphatic chain and fatty tissue
By depriving sympathetic nerve supply to the lower limb blood vessels, vasomotor tone is reduced, which in turn reduces some amount of vasospasm.
- Thus, rest pain improves and minor ulcerations heal due to cutaneous vasodilatation. However, the duration of the effect of lumbar sympathectomy is not clear.
- Both sides may be done in one sitting. However, during bilateral operation, the 1st lumbar ganglion on one side should be spared since removal of both ganglia may cause sterility due to paralysis of the ejaculatory mechanism.
- One should be careful not to damage lumbar veins which join the inferior vena cava.
- Conservative amputations should be done if the toes are gangrenous.
- Below-knee amputation is the last resort. It is indicated in severe rest pain cases in which all other modalities of treatment have failed. The risk of amputation after ten years of the disease is around 10%. The risk of amputation is higher with patients having an ABPI of less than 0.5.
2. Surgery in atherosclerotic vascular disease:
- Avoid or treat risk factors.
- Major Risk Factors for Atherosclerosis
-
- Lipids: Dyslipidaemia
- Inhalation of tobacco: Smoking
- Pressure: Hypertension
- Insulin deficiency: Diabetes
- Disordered metabolism: Hyperhomocysteinemia
- Remember as LIPID
The decision to revascularise the limb is taken after an angiography. The success of reconstruction depends on a number of factors.
- Prognostic Factors for Limb Revascularisation
-
- Severity of the disease
- Site of occlusion
- Presence of collaterals
- Age of the patient
- Presence of diabetes
- Angina pectoris
- Chronic smoking
- Fitness for anaesthesia
- Intermittent claudication alone is not an indication for surgery. Rest pain and gangrenous changes in the limb are definite indications for reconstruction with acceptable mortality and morbidity.
- Surgery can be classified as surgery for aortoiliac disease, ileofemoral disease and femoropopliteal disease.
- Principle of reconstruction: Wide exposure to allow safe control of vessels, proximal and distal control inflow (proximal) and outflow (distal) anastomosis in disease-free area, careful selection of graft depending upon the site of surgery.
- Dacron and ePTFE perform equally well in aortoiliac bypass, but the saphenous vein has superior patency in infrainguinal bypass.
Aortoiliac Disease
It is treated by bypass grafts or endarterectomy.
1. Bypass Grafts
- Usually, it is bilateral and is treated with an aortobifemoral graft to bypass the stenosis. The graft is made from either Teflon or Dacron. It is also called a Y-graft or trouser graft.
- It commonly has a 16 mm trunk and two 8 mm limbs. In unilateral cases, a unilateral graft is applied.
- The aorta is approached from a midline incision. The posterior peritoneum is opened to expose the aorta with 2 vertical incisions, and the common femorals are exposed in the groin.
- Before clamping the vessels, heparin 5000 U is administered intravenously. End-to-side of the graft to the aorta above and femoral artery below is done.
- Extra-anatomical bypass refers to any bypass graft, autologous or otherwise, that is placed in a site different to that of the arterial segment that is being bypassed.
- For example, axilla-bifemoral bypass in a case of hostile abdomen (previous surgeries, mycotic aneurysms, aortoenteric fistulae), obturator bypass (hostile groin after radiation or previous surgery), femoral-femoral bypass.

2. Aortoiliac Endarterectomy
They are usually not done.
Indications: Short segment, large artery such as aorta and single artery.
Aortoiliac Endarterectomy Types:
- Open endarterectomy: An arteriotomy is done first and the diseased intima, atheromatous plaque, and thrombus are removed. An arteriotomy incision can either be closed directly or with a vein patch graft to close the defect to avoid narrowing.
- Closed endarterectomy is indicated in a longer diseased segment. In this procedure, after an arteriotomy, a wire loop is used to strip out a core of atheroma by introducing it through the lower arteriotomy.
- And removing the atheromatous plaque from the upper end. However, the results of bypass grafts are better than endarterectomy. The modern tendency is to do bypass graft.
ILiofemoral Stenotic Disease
1. Transluminal angioplasty: Any arterial stenosis can be dilated in angioplasty. The technique can be repeated if stenosis recurs. The procedure is done under local anaesthesia and is indicated in poor-risk patients.
- Ideally suitable for the iliofemoral segment, but not suitable for stenosed vessels below the knee. A balloon catheter is inserted into the artery under local anaesthesia and is inflated at high pressure for around 30 seconds and deflated.
- By inflation and dilatation 2–3 times, the stenosed segment can be dilated. Complications include internal dissection, distal embolisation, thrombosis, and even rupture of the vessel.
2. Ilio-femoral bypass grafts: Generally recommended when the diseased segment is beyond 15 cm in length. The technique is similar to what is mentioned above.
- This can be repaired by a bypass graft which is sutured to the normal common iliac artery above and to the normal femoral artery below.
- In this procedure, a balloon catheter is inserted into the artery and inflated. Its correct position is confirmed by radiopaque markers which are present in the balloon.
- A summary of revascularisation surgery is given.
ILiofemoral Stenotic Disease Summary of the Revascularisation Surgery
- Aortoiliac disease – Aortobifemoral or aortofemoral moral graft and endarterectomy
- Iliofemoral disease – Iliofemoral bypass graft Balloon angioplasty
- Femoropopliteal disease – A bypass graft
- Profunda artery stenosis – Profundoplasty

Femoropopliteal Occlusion
This is the most common site of obstruction in atherosclerotic patients. This is treated with a graft extending from the femoral artery above to the popliteal artery below.
- Reversed autologous long saphenous vein is better than other grafts because it is less thrombogenic. If it is not reversed, the valves have to be disrupted using a valvulotome. If the LSV is not available, try the SSV. When no vein is available, try for synthetic grafts.
- Dacron graft and polytetrafluoroethylene graft (PTFE) are commonly used grafts.
- On a few other occasions, small vessel bypasses like femorotibial artery bypass may also be done if the diameter of the distal vessels is ≥3 mm.
- Success in the immediate post-operative period is around 90%, but the 5-year patency is around 50%.
Balloon Angioplasty In Atherosclerotic Arterial Disease







Balloon Angioplasty In Atherosclerotic Arterial Disease Profunda Artery Stenosis
Significant occlusion of the profunda is demonstrated by oblique views in an arteriography. If there are no significant vessels available below the stenosis for reconstruction, profundoplasty is considered. It is done using a patch of Dacron or vein to widen the origin of the vessel after endarterectomy.
Balloon Angioplasty In Atherosclerotic Arterial Disease Complication of Surgery
- Early
- Hemorrhage
- Limb ischemia
- Renal failure
- Intestinal ischemia
- Spinal cord ischemia
- Ureteric injury
- Late
- Graft thrombosis
- Anastomotic pseudoaneurysm
- Sexual dysfunction
- Infection
- Aortoenteric fistula
Acute Arterial Occlusion
Sudden occlusion of an artery commonly occurs due to an embolus. The source of the embolus is from the heart or from an atheroma.
- Increased incidence of road traffic accidents, falls, or war injuries are other causes. Trauma to the artery also produces occlusion.
- Emboli from atheromatous plaques are called atheroemboli. In most of these patients, collaterals would have developed, hence limb ischaemia may not be very critical.
Embolic Occlusion
This commonly occurs in the peripheral arteries (for example. common iliac, femoral, and popliteal).
- An embolus is a foreign body to the bloodstream. It gets lodged in a vessel and produces obstruction, clinically manifesting as severe ischaemia or gangrene and resulting in critical limb ischaemia (CLI).
- Atherosclerotic vascular disease, thromboangiitis obliterans, acute embolic ischaemia, and even diabetes, may present as CLI.
Embolic Occlusion Causes or Risk Factors:
Smokers, cardiac diseases, obesity, recent cardiac surgery
Causes of acute lower limb ischaemia

Embolic Occlusion Pathology
- As a result of sudden occlusion, blood supply to the distal part is cut off resulting in rapid development of tissue death and gangrene.
- Most of such patients also have atherosclerosis. Tissue hypoxia followed by the release of superoxide radicals and thromboxanes results in endothelial damage necrosis and gangrene within a few hours.
Embolic Occlusion Clinical Features
- No previous history is suggestive of intermittent claudication.
- Signs of Acute Lower Limb Ischaemia
- Peripheries are cold
- The pallor of the limb
- Poor capillary return
- Positive Buerger’s test
- Progressive paralysis
- Pulses are absent
- Pulse at the ankle by Doppler—undetectable
- Observe 7 Ps
- Sudden dramatic symptoms are described in the form of the 5Ps-Pain, Pallor, Paresis, Pulselessness, and Paraesthesia.
- Pain is severe, unbearable, and of a burning or bursting type.
- The limb is pale and cold, and superficial veins are collapsed.
- Paresis: Depending on the level of occlusion, the function of the limb is lost. Movement of the toes becomes difficult, followed by total paralysis.
- Pulselessness: Characteristically, peripheral pulses below the level of the embolism are not palpable.
- Paraesthesia: Altered sensation in the limb.
- If left untreated, necrosis of the muscles followed by gangrene of the limb may occur within a few hours (6–24 hours).
- A cardiac examination may reveal signs of valvular heart disease.
Look also for evidence of emboli in other arteries.
Emboli in various arteries symptoms, signs and effects

Acute Arterial Occlusion Critical Limb Ischaemia (CLI)
It is defined as persistently recurring ischaemic rest pain requiring regular, adequate analgesia for >2 weeks or ulceration or gangrene of the foot or toes with an ankle pressure <50 mmHg or a toe systolic pressure <30 mmHg.
Acute Arterial Occlusion Investigations
- Peripheral circulation should be assessed by Doppler ultrasound, which is an excellent noninvasive investigation to judge the severity, level, position, and length of superficial femoral artery stenosis.
- Urgent duplex scan
- CT angiogram


Acute Arterial Occlusion Treatment
1. Angioplasty: Percutaneous transluminal angioplasty (PTA) is indicated in short stenotic lesions in a large vessel (for example. iliac and femoropopliteal lesions).
- First, the balloon catheter is introduced percutaneously over a guidewire across the lesion. Under fluoroscopic control, the balloon is dilated until satisfactory widening of the lumen is achieved.
- It is a relatively safe and simple procedure.
- Immediate intravenous infusion of heparin (10,000 IU) is necessary to reduce the extension of the thromboembolism.
2. Emergency embolectomy is done under GA or local anaesthesia either by a direct arteriotomy incision and removal of the clot or by using a Fogarty balloon catheter to remove the embolus remotely.





- Embolectomy: Under local or general anaesthesia, a transverse incision is given over the common femoral artery. A Fogarty catheter is introduced through the incision for about 1–2 cm and the balloon is inflated.
- The catheter is then withdrawn, and the emboli are removed. The procedure is repeated until bleeding occurs. The catheter can be passed by the ankle to remove distal emboli as well. Postoperatively, anticoagulants are continued.
3. Intra-arterial thrombolysis:
- It is indicated in acute or acute chronic ischaemia where ischaemia is not so severe.
- Intra-arterial thrombolysis: A catheter is passed into the ‘clot’ after performing arteriography and t-PA (tissue plasminogen activator) is infused through the catheter. Repeat angiogram check films are taken to see the results, such as clot lysis, revascularisation, etc.
- It will reopen the occluded lumen within 24 hours.
- The Procedure should be abandoned if the clot does not undergo dissolution.
- A repeat angiogram is necessary to check for patency.
Acute Arterial Occlusion Contraindications for thrombolytic therapy:
- Contraindications to Thrombolytic Therapy
- Absolute
- Recent major bleeding
- Recent major surgery
- Recent ophthalmologic procedure
- Recent stroke
- Relative
- Active peptic ulcer disease
- Pregnancy
- Uncontrolled hypertension
- Coagulation abnormalities
Recent advances: Trans-Atlantic inter-Society Consensus: TASC guidelines

Reperfusion Injuries Or Syndrome
This dangerous event follows the revascularisation of the limbs, resulting in acute compartment syndrome with compartmental pressure exceeding capillary pressure (30 mmHg).
- Most of the injury is believed to be due to O2 derived free radicals. The most important ones include superoxide radicals, hydrogen peroxide, and hydroxyl radicals.
- These radicals attach unsaturated bonds of fatty acids within the phospholipid membranes, resulting in damage.
- Oedema and swelling of the muscles take place.

Reperfusion Injuries Or Syndrome Management
- Diagnosis is clinical, as suggested by severe pain in the limb, oedema of the leg, and muscle tenderness.
- Raised intra-compartmental pressure measured by a transducer cannula will help in the diagnosis.
- Creatinine is elevated (renal failure).
- Creatine kinase is elevated (rhabdomyolysis).
- Treated by urgent multiple fasciotomy and decompression, followed by debridement of dead tissues.
- Supportive treatment such as antibiotics and hydration, is given.
Peripheral Aneurysms
These can affect the popliteal artery, femoral artery, iliac artery, etc.
- 70% of peripheral aneurysms affect the popliteal artery, and two-thirds of them are bilateral.
- However, students should realise that aneurysms are uncommon (rare) causes of lower limb ischaemia.
- Early diagnosis and effective treatment are essential to save the limb. Aortic aneurysms are discussed under abdominal mass.
Popliteal Aneurysms
They are the most common peripheral aneurysms because of the following reasons:
- Turbulence beyond stenosis at the adductor magnus hiatus.
- Repeated flexion at the knee.
Peripheral Aneurysms Clinical Features
- They affect elderly patients and are caused by atherosclerosis. The age at presentation is 65 years.
- One-third of the cases are associated with aortic aneurysms.
- Striking preponderance in males. Male: female ratio is 20–30: 1.
- Presents as a swelling behind the knee.
- Dull aching pain is common. Severe bursting pain indicates rapid expansion and impending rupture.
- Pulsatile, tense, cystic, fluctuant swelling behind the knee in the popliteal fossa, in the line of the popliteal artery.
- Its size diminishes on extending the knee as the aneurysm is deep to the popliteal fascia.
- Proximal compression test: On occluding the femoral artery proximally, the swelling may diminish in size.
Peripheral Aneurysms Investigations
Duplex ultrasonography is the investigation of choice, which can measure the diameter and determine the extent of the mural thrombus.
Angiography can demonstrate the extent of the involved segment to look for patency and check the quality of runoff vessels.
Peripheral Aneurysms Complications
- Thrombosis causes severe acute ischaemia of the lower limb (incidence: 40%).
- Embolisation causes ischaemic ulceration of the lower limb.
- Rupture causes pain and haematoma (rare: 2–5%).
- Compression on the popliteal vein causes pain, tenderness, and swelling of the leg.
- Compression on the lateral peroneal nerve causes foot drop, due to paralysis of the peronei and the extensors of the foot.
Peripheral Aneurysms Treatment
- Proximal and distal ligation of the artery followed by reversed saphenous vein bypass graft is the treatment of choice. This results in total obliteration of the sac and revascularisation of the limb.
- Excision of the sac is better avoided because of the risk of injury to the popliteal vein and nerves. Lateral popliteal nerve injury causes foot drop, and tibial (medial popliteal) nerve injury causes thinning of the calf region, loss of plantar flexion, and clawing of the toes due to paralysis of the intrinsic muscles of the foot.
Miscellaneous Ainhum
It affects those who do not use footwear/walk barefoot. It starts as a fissure at the level of the interphalangeal joint of a toe, usually the fifth. Repeated minor trauma may be present.
- The tissue becomes a fibrous band resulting in tight constriction and necrosis. If it continues, it may culminate in autoamputation.
- Division of the band or early Z-plasty may be needed to avoid amputation.
- In early cases—thrombolysis with a catheter in situ.

Frostbite
- It occurs due to excessive exposure to cold weather.
- High altitudes with excessive cold precipitate vasospasm and damage the blood vessel wall. It causes sludging of blood and thrombosis.
- Malnutrition and ageing are the other precipitating factors. Severe burning pain, discolouration of the foot, and development of blisters suggest that gangrene is imminent.
Frostbite Treatment
- Slow warming of the parts and protection with cotton wool.
- Analgesics and antibiotics.
- Paravertebral injection into the sympathetic chain may help in a few patients.
- Elevation of the foot to reduce oedema.
- Frank cases of frostbite with gangrene require conservative amputation.
Fat Embolism
Fat Embolism Definition
Often a potentially lethal condition occurs due to blockage of major arteries by the aggregation of chylomicrons.
Fat Embolism Causes
- Fracture femur (long bones)
- Orthopaedic surgery, multiple fractures
- Liposuction
- Sickle cell disease
- Pancreatitis
- Diabetes mellitus
Fat Embolism Clinical Features
- Pulmonary: Central cyanosis, tachypnoea, right heart failure, and froth in the mouth and nostrils. Respiratory distress is the most common presenting feature.
- CNS: Drowsiness, disorientation, restlessness, constricted pupils, pyrexia, and coma.
- Retinal artery: Striate haemorrhages, fluffy exudates on fundoscopic examination, and cotton wool spots.
- Cutaneous: Petechial rashes in the non-dependent parts of the body—chest, axilla and conjunctiva.
Fat Embolism Pathogenesis
- 50% of cases occur within 72 hours.
- Free fatty acids (FFAs), released at the time of trauma or breakdown of fat in the lung, directly affect pneumocytes resulting in Acute Respiratory Distress Syndrome (ARDS).
- Another theory is that there is blockage by the aggregation of chylomicrons.
Fat Embolism Investigations
- Arterial blood gases—hypoxaemia and respiratory alkalosis from hyperventilation.
- Chest X-ray—bilateral interstitial and alveolar infiltrates in severe cases (‘snowstorm’ pattern).
Fat Embolism Treatment
- Close monitoring with pulse oximetry.
- Supportive therapy with oxygen and mechanical ventilation as required.
- Surgical—early internal fixation of the fracture.
Air Embolism
- Large veins get opened in the neck
- Open heart surgery or if the pulmonary vein is punctured
- Fallopian tube insufflation
- Illegal abortion (through paravertebral veins)
- Paradoxical embolism, reaching coronary artery through patent foramen ovale
Air Embolism Definition
It is a potentially fatal condition that occurs due to blockage of the pulmonary artery by a large volume of air in the venous circulation.
Air Embolism Causes
- Neck surgeries in which a large vein is inadvertently opened and the patient is in a head-elevated position (thyroid surgery) or sitting position (posterior fossa surgery).
- Rapid infusion of intravenous fluids where emptying of the bottle and infusion set may go unnoticed and a fresh bottle is connected and infused without eliminating air from the infusion set.
Air Embolism Effects
Formation of an air lock within the pulmonary artery and right heart failure.
Air Embolism Treatment
- Position the patient head down (Trendelenburg position) so that air entrainment is stopped.
- Turn the patient to his or her left side so that air will float to the ventricular apex, reducing its entry into the pulmonary artery.
- Administer oxygen and resuscitate as necessary.
Intensive Care Unit (Icu) Gangrene
It is a rare clinical entity. It was first described by Jonathan Hutchinson in 1891 as multiple extremity ischaemia and was termed ‘symmetrical peripheral gangrene.’
- Possible aetiological factors include sepsis, DIC, and the use of vasopressor agents.
- The possible responsible drug is noradrenaline.

Patients in the ICU have multiple arterial punctures for securing intra-arterial lines for invasive monitoring.
- These arterial punctures may also be a possible aetiological factor.
- Sepsis in the presence of sluggish blood flow has been described to be responsible for the development of symmetrical peripheral gangrene.

Vasospastic conditions, small vessel obstruction, and very low cardiac output states (perfusion pressure falling to 35–60 mmHg) may also contribute.
- Medical conditions, such as diabetes mellitus, malignancy, protein C or S or antithrombin 3 deficiency are other contributing factors.
- The usual manifestation is pallor or cyanosis, coldness, and pain in the extremities. They become erythematous and there is dusky discolouration of the skin with bullae or blisters, followed by gangrene.
- Pulses may be intact in the early stages. Large vessels are often spared. Low flow states result in occlusion of the microcirculation of the affected parts.
- The first line of management is immediate discontinuation of vasopressors as soon as discolouration is seen.
- Aggressive treatment of sepsis with intravenous antibiotics and anticoagulation for DIC are the suggested measures.
- Local debridement and secondary skin grafting have been unsuccessful.
- Amputation should be considered only after a clear line of demarcation develops. The condition has a high mortality rate of 40%.
Lower Limb Ischaemia And Popliteal Aneurysm Multiple Choice Question And Answers
Question 1. Which of the following is false regarding thromboangiitis obliterans?
- The dorsal pedis and posterior tibial arteries are often affected
- The radial artery may also be affected
- The superficial femoral artery is also affected
- Bruit is present over the femoral artery
Answer: 4. Bruit is present over the femoral artery
Question 2. The following is true for atherosclerotic arterial disease:
- Large-sized arteries are affected
- The upper limb is often affected
- It may be associated with an aortic aneurysm
- A bruit may be present over the artery
Answer: 2. The upper limb is often affected
Question 3. The following are features of thromboangiitis obliterans:
- Raynaud’s phenomenon
- Migrating thrombophlebitis
- Segmental panarteritis
- Polymorphs and giant cells are absent in histopathology
Answer: 4. Polymorphs and giant cells are absent in histopathology
Question 4. The following are the uses of a Doppler probe:
- To feel the nonpalpable pulse
- To look for pressure index
- To measure blood pressure
- To detect a triphasic pattern
Answer: 4. To detect triphasic pattern
Question 5. Lumbar sympathectomy has the following advantages:
- Rest pain improves to a small extent
- Ulcerations heal
- Claudication and claudication distance improve
- The nutritive value of the blood flow improves
Answer: 3. Claudication and claudication distance improve
Question 6. A Fogarty catheter is used in:
- Chronic arterial occlusion
- Acute arterial embolic occlusion
- Vasospastic disease
- Femoral vein thrombosis
Answer: 2. Acute arterial embolic occlusion
Question 7. The characteristic features of critical limb ischaemia are:
- Intermittent claudication
- Ankle pressure <70 mm of Hg
- Toe systolic pressure <30 mmHg
- Absent pulses
Answer: 3. Toe systolic pressure <30 mmHg
Question 8. The triad of fat embolism includes:
- Respiratory failure, confusion, petechial haemorrhages
- Respiratory failure, confusion, large purpuric spots
- Respiratory failure, alertness, petechial haemorrhages
- Cardiac failure, confusion, petechial haemorrhages
Answer: 1. Respiratory failure, confusion, petechial haemorrhages
Question 9. The following is true for popliteal aneurysm:
- It is caused by atherosclerosis
- It is the most common type of peripheral aneurysm
- It is always unilateral
- Foot drop may occur
Answer: 3. It is always unilateral
Question 10. The following are true about lumbar sympathectomy:
- It is a postganglionic sympathectomy
- The sympathetic trunk is divided below the first sympathetic ganglion
- It is a preganglionic sympathectomy
- It is usually done by an extraperitoneal approach
Answer: 1. It is a postganglionic sympathectomy
Question 11. The following is true for infra-inguinal bypass surgery for diabetic ulcers:
- The long saphenous vein is inferior to the PTFE graft
- Preoperative vein marking is helpful
- 2-year patency is around 70%
- The amputation rate after bypass surgery is still high
Answer: 1. Long saphenous vein is inferior to the PTFE graft
Question 12. The following are major risk factors for atherosclerosis:
- Dyslipidaemia
- Tobacco smoking
- Hyperhomocysteinemia
- Alcohol intake
Answer: 4. Alcohol intake
Question 13. The following is true for profundoplasty except:
- It is done using a patch of Dacron
- It is done using a vein graft
- It is done after an endarterectomy
- It is done in TAO patients
Answer: 4. It is done after an endarterectomy
Question 14. The following are true about tissue plasminogen activators:
- It was first purified from melanoma cells
- It is an endogenous enzyme like urokinase
- It is sometimes elevated in carcinoma stomach
- Streptokinase also has plasminogen-activating action
Answer: 3. It is sometimes elevated in carcinoma stomach
Leave a Reply