Lung
Question 1. Write a note on Atelectasis.
Answer:
Atelectasis: Defined as the collapse of the lung
Atelectasis Major types:
- Resorption atelectasis: Due to complete obstruction of the airway. Causes include bronchial asthma, chronic bronchitis, bronchiectasis, aspiration of foreign bodies, and fragments of bronchial tumors
- Compression atelectasis: Due to fluid or air in the pleural cavity
- Contraction atelectasis: Pulmonary or pleural fibrosis prevents full lung expansion
Note:
Resorption and compression types are reversible
Question 2. Write about the causes, pathogenesis, and morphology of acute respiratory distress syndrome (ARDS).
Answer:
Acute respiratory distress syndrome (diffuse alveolar damage)
- Characterized by abrupt onset of significant hypoxemia and bilateral pulmonary infiltrates in the absence of cardiac failure
- Acute respiratory distress syndrome (ARDS) is a manifestation of severe acute lung injury (ALI)
- Most common causes: Sepsis, pulmonary infections, gastric aspiration, mechanical trauma
Read and Learn More Preparatory Manual of Pathology Question and Answers
ARDS Pathogenesis
- Following events occur in the sequence leading to alveolar damage:
- Endothelial activation
- Adhesion and extravasation of neutrophils
- Accumulation of intra-alveolar fluid and formation of hyaline membranes
- Resolution of injury with resultant fibrosis of alveolar walls
ARDS Morphology
- Lungs are heavy, firm, red, and boggy and show congestion, interstitial and interalveolar edema, inflammation, fibrin deposition, and diffuse alveolar damage
- Alveolar walls are lined with waxy hyaline membranes
Question 3. Write a note on etiopathogenesis and histological types of emphysema.
Answer:
Emphysema
Characterized by irreversible enlargement of the airspaces distal to the terminal bronchiole, accompanied by destruction of their walls without obvious fibrosis
Emphysema Four major types:
- Centriacinar
- Panacinar
- Paraseptal
- Irregular
1. Centriacinar (centrilobular) emphysema
- Central or proximal parts of the acini, formed by respiratory bronchioles, are affected, whereas distal alveoli are spared
- Lesions are more common and severe in the upper lobes
- Seen in heavy smokers, in association with chronic bronchitis (COPD)
2. Panacinar (pan lobular) emphysema
- Acini are uniformly enlarged and involve the alveolar duct and alveolus
- More common in the lower zones, most severe at the bases
- Associated with α1-antitrypsin deficiency
3. Distal acinar (paraseptal) emphysema
- Distal acinus is involved, severe in the upper half of the lungs
- Multiple, continuous, enlarged airspaces
- Cause of spontaneous pneumothorax in young adults
4. Irregular emphysema
- Acinus is irregularly involved and is associated with scarring
Question 4. Write a short note on chronic bronchitis.
Answer:
Chronic bronchitis Definition:
Persistent cough with sputum production for at least 3 months in at least 2 consecutive years, in the absence of any other identifiable cause
Chronic bronchitis Pathogenesis:
Exposure to tobacco smoke and dust from grain, cotton, and silica leads to:
1. Mucus hypersecretion: Associated with hypertrophy of submucosal glands in the trachea and bronchi
2. Inflammation
3. Infection
Chronic bronchitis Morphology
- Increase in the number of goblet cells and mucus gland layer hyperplasia
- Bronchial epithelium can exhibit squamous metaplasia and dysplasia
- Bronchiolitis obliterans: Marked narrowing of bronchioles due to fibrosis, which results in obliteration (in severe cases)
Reid index: (normal value: 0.4)
- The ratio of the thickness of the mucous gland layer to the thickness of the wall between the epithelium and the cartilage
- Increased in chronic bronchitis
Question 5. Write a short note on the pathogenesis of bronchial asthma.
Answer:
Asthma
Episodic bronchoconstriction due to increased airway sensitivity to a variety of stimuli; inflammation of the bronchial walls; and increased mucus secretion
Asthma Pathogenesis:
1. TH2 responses, IgE, and inflammation
- Early reaction:
- Inhaled allergens (antigens) stimulate TH2 cells and result in IgE production
- IgE results in eosinophil recruitment
- On re-exposure to the antigen, there occurs cross-linking of IgE, bound to the Fc receptors on mast cells resulting in the release of mast cell mediators
- Mast cell mediators bring about bronchospasm, increased vascular permeability, mucus production, and recruitment of leukocytes
- Late reaction: Leukocytes recruited to the site and factors released from eosinophils (for example major basic protein, eosinophil cationic protein), damage the epithelium
2. Genetic susceptibility: Polymorphism in the IL-13 gene and gene encoding ADAM33 increases the risk
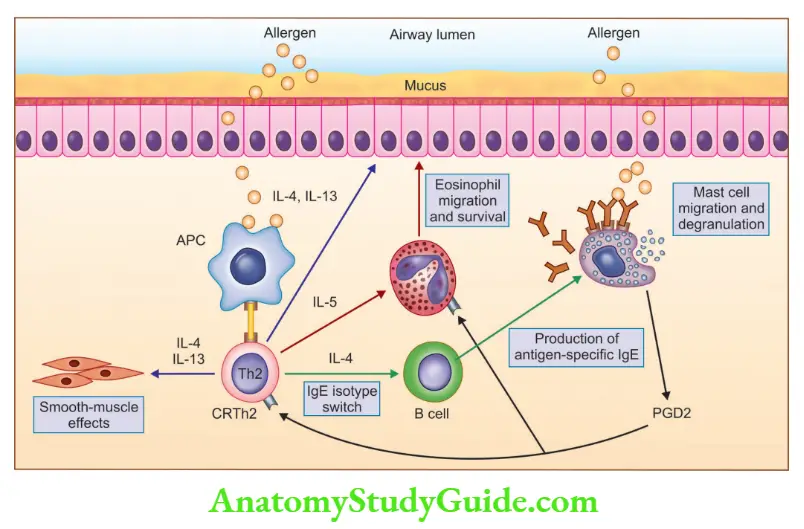
3. Environmental factors: Allergen and smoke acts as induction factors
- Morphology of asthmatic airway
- Accumulation of mucus
- Goblet cell hyperplasia
- Thickened basement membrane
- Intense chronic inflammation (eosinophils, macrophages)
- Hypertrophy and hyperplasia of smooth muscle cells
- Hypertrophy of submucosal glands
Question 6. Discuss the causes and morphology of the lung in bronchiectasis.
Answer:
Lung in bronchiectasis Definition
- Permanent dilation of the bronchi and bronchioles due to the destruction of smooth muscle and elastic tissue by chronic necrotizing infections
Lung in bronchiectasis Causes
- Congenital or hereditary conditions: Cystic fibrosis, primary ciliary dyskinesia, and Kartagener syndromes
- Infections: Pneumonia
- Bronchial obstruction: Tumor, foreign bodies, or mucus impaction
- Rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, COPD
Lung in bronchiectasis Morphology
- Affects bilateral lower lobes, and is most severe in distal bronchi and bronchioles
- Airway dilatation is seen, and dilated bronchioles can be followed almost to the pleural surfaces
- The cut surface of the lung shows dilated bronchi, which appear cystic and are filled with mucopurulent secretions
Question 7. Write a note on pneumoconiosis.
Answer:
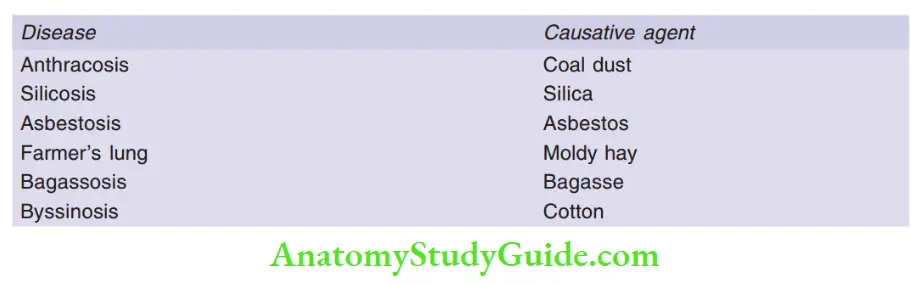
Pneumoconiosis Definition:
Non-neoplastic lung reaction due to the inhalation of mineral clouds of dust encountered in the workplace
Important pneumoconiosis and their implicated causative agent
Question 8. Discuss coal worker pneumoconiosis.
Answer:
Coal workers’ pneumoconiosis
Caused by inhalation of coal particles
Can present as
1. Anthracosis
- Pulmonary lesions were seen in coal miners
- Inhaled carbon pigment is engulfed by alveolar or interstitial macrophages and is deposited along the bronchi
2. Simple coal workers’ pneumoconiosis
- Characterized by coal macules (1 to 2 mm in diameter) and coal nodules
- Sites: Upper lobes and upper zones of the lower lobes
3. Complicated coal workers’ pneumoconiosis (progressive massive fibrosis)
- Characterized by multiple, intensely blackened scars of 1 cm or larger
- Microscopy: Lesions consist of dense collagen and pigment
Question 9. Write salient features of silicosis.
Answer:
Silicosis
Caused by inhalation of crystalline silicon dioxide (silica)
Silicosis Pathogenesis
- Silica occurs in crystalline and amorphous forms
- Crystalline forms (for example quartz) are more fibrogenic
- After inhalation, the particles are phagocytosed by macrophages and activate inflammasome, which releases inflammatory mediators, IL-1 and IL-18.
Silicosis Morphology
- Gross: Nodules in the upper zones of the lungs, which in chronic stages coalesce into hard, collagenous scars
- Fibrotic lesions can also occur in the hilar lymph nodes and pleura
- Eggshell calcification: Thin sheets of calcification in the lymph nodes, seen radiographically
Silicosis Microscopy
- The central area of whorled collagen fibers with a peripheral zone of dust-laden macrophages
- Nodules with polarized microscopy reveal birefringent silica particles
Note:
- Silicosis is associated with increased susceptibility to tuberculosis and lung cancer
Question 10. Mention asbestos-related diseases and their pathogenesis.
Answer:
Asbestos-related diseases include
- Localized fibrous plaques, or rarely, diffuse pleural fibrosis
- Pleural effusions
- Parenchymal interstitial fibrosis (asbestosis)
- Lung carcinoma
- Mesotheliomas (pleural and peritoneal)
- Laryngeal, ovarian, and colon carcinomas
- Increased risk for systemic autoimmune diseases and cardiovascular disease
Asbestos-related Pathogenesis
- Two distinct forms: Serpentine chrysotile (most commonly used) and Amphibole (more pathogenic)
- After inhalation, particles are phagocytosed by macrophages, resulting in the activation of the inflammasome
- Inflammasome activation brings about interstitial inflammation and fibrosis
Asbestos-related Morphology
- Asbestos bodies: Golden brown, fusiform, or beaded rods with a translucent center
- Asbestosis begins in the lower lobes and subpleural
Asbestos-related Pleural plaques
- The most common manifestation of asbestos exposure
- Well-circumscribed plaques of dense collagen
- Sites: Parietal pleura and over the domes of the diaphragm
Question 11. Write a note on sarcoidosis.
Answer:
Sarcoidosis
A systemic granulomatous disease that presents as bilateral hilar lymphadenopathy or lung involvement
Sarcoidosis Pathogenesis
- Intra-alveolar and interstitial accumulation of CD4+ T cells, resulting in CD4/CD8 T cell ratios ranging from 5: 1 to 15: 1
- Association with HLA-A1 and HLA-B8
Sarcoidosis Morphology
- Non-necrotizing granulomas composed of aggregates of tightly clustered epithelioid macrophages, and giant cells
- In giant cells: Schumann bodies (laminated concretions composed of calcium and proteins) and stellate inclusions (asteroid bodies) are found
Question 12. Discuss lobar pneumonia.
Answer:
Lobar pneumonia
Consolidation of a large portion of a lobe or of an entire lobe of the lung
Lobar pneumonia Stages
Four stages of the inflammatory response are seen
1. Congestion
- The lung is heavy, boggy, and red
- Characterized by vascular engorgement, intra-alveolar fluid with a few neutrophils
2. Red hepatization
- Gross: The affected lobe of the lung is red, firm, and airless, with liver-like consistency
- Microscopy: Alveolar spaces with exudates comprising neutrophils, red cells, and fibrin
3. Gray hepatization
- Characterized by the progressive disintegration of red cells and persistence of fibrinous exudate
4. Resolution
- Exudates in the intra-alveolar spaces get broken down and are ingested by macrophages, which are either expectorated or gets organized by fibroblasts
Complications of pneumonia include
- Abscess formation: Due to tissue destruction and necrosis
- Empyema: Spread of infection to the pleural cavity
- Bacteremic dissemination: To the heart valves, pericardium, brain, kidneys, spleen, or joints
Question 13. Discuss the pathogenesis and morphology of the lung in primary pulmonary tuberculosis.
Answer:
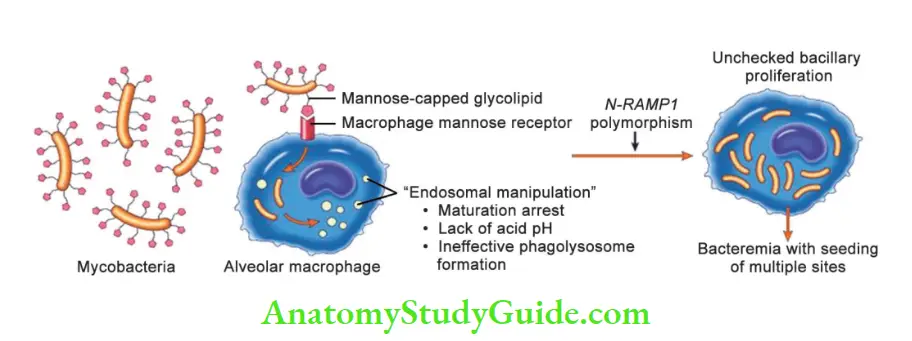
Pathogenesis: Involves the following steps
- Entry of Mycobacterium tuberculosis bacilli into the macrophages
- Replication of tubercle bacilli in the macrophages occurs because tubercle bacilli inhibit maturation of the phagosome and block the formation of phagolysosome
- Th1 response: After 3 weeks of the initial infection, T cells transform into T-helper 1 (Th1) cells, by IL-12
- Th1-mediated macrophage activation and killing of bacteria: Th1 cell mediates IFN- production and thus enables macrophages to contain M. tuberculosis
- Granulomatous inflammation and tissue damage
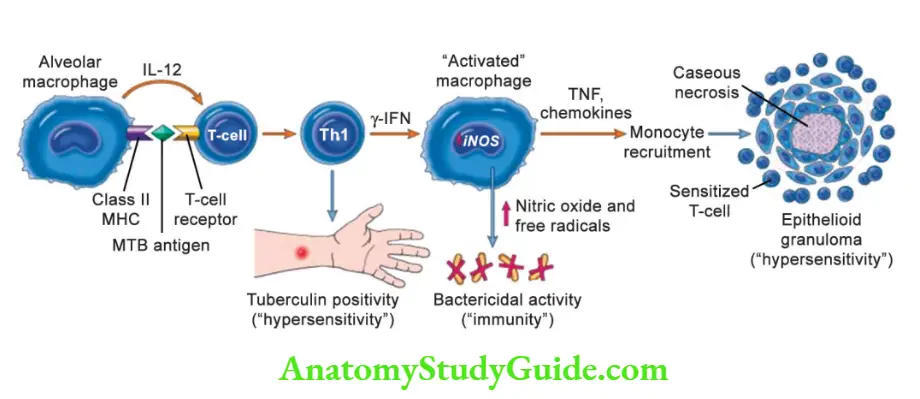
Morphology of lung in primary pulmonary tuberculosis Primary tuberculosis
- Ghon focus: 1 to 1.5 cm area of consolidation, with caseous necrosis in its center
- Ghon complex: Combination of parenchymal lung lesion and nodal involvement
- After cell-mediated immunity controls the infection, Ghon complex undergoes progressive fibrosis, resulting in radiologically detectable calcification (Ranke complex)
Microscopy
Consolidated areas show caseation necrosis with surrounding epithelioid cell granulomas, and multinucleated Langhans giant cells
Question 14. Classify bronchogenic carcinoma. Discuss the etiopathogenesis and morphology of various subtypes.
Answer:
Histologic Classification of malignant epithelial lung tumors
- Squamous cell carcinoma
- Small cell carcinoma
- Adenocarcinoma
- Large cell carcinoma
- Adenosquamous carcinoma
- Carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements
- Carcinoid tumor
Etiology and pathogenesis
- Tobacco smoking
- Industrial hazards: Asbestos, arsenic, chromium, uranium, nickel, vinyl chloride, high-dose ionizing radiation
- Air pollution: Radon gas exposure increases the risk
Molecular Genetics
- Squamous cell carcinoma: Chromosome 3p, 9p and 17p (TP53) deletions, amplification of FGFR1
- Small cell carcinoma: Shows strongest association with smoking, p53 mutations, Rb gene deletions, chromosome 3p deletions
- Adenocarcinoma: Gain-of-function mutations in EGFR, RET receptors, and KRAS gene mutations
Morphology
- Adenocarcinoma arises in the periphery of the lung, whereas squamous cell carcinomas arise in the central/hilar region
1. Adenocarcinoma
- Patterns recognizable on histopathology: Acinar, lepidic, papillary, micropapillary, and solid, with or without mucin production
- Are located peripherally and are smaller
- Shows thyroid transcription factor-1 (TTF-1) positivity
- Microinvasive adenocarcinoma: Tumors with a small invasive component (5 mm)
- Mucinous adenocarcinoma can present as satellite nodules
2. Squamous cell carcinoma
- Most commonly found in men and is strongly associated with smoking
- Presence of keratinization and/or intercellular bridges
- Keratinization may take the form of squamous pearls
- Precursor lesions: Squamous metaplasia, epithelial dysplasia, carcinoma in situ
3. Small cell carcinoma
- Arises in major bronchi or in the periphery of the lung
- Has a strong relationship with cigarette smoking
- Most aggressive lung tumors
- Most commonly associated with ectopic hormone production
Microscopy
- Small cells with scant cytoplasm, ill-defined cell borders, finely granular nuclear chromatin (salt and pepper pattern), and absent or inconspicuous nucleoli
- Tumor cells are round, oval, or spindle-shaped, and nuclear molding is prominent
- Mitotic count is high, with extensive necrosis
- Azzopardi effect: Basophilic staining of vascular walls due to encrustation by DNA from necrotic tumor cells
- IHC: Chromogranin, synaptophysin, CD57 positivity, and high levels of antiapoptotic protein BCL2 are seen in 90% of tumors
Question 15. Mention paraneoplastic syndromes associated with carcinoma lung.
Answer:
Paraneoplastic syndromes
- Hyponatremia: Due to ADH
- Cushing syndrome: Due to ACTH
- Lambert-Eaton syndrome
- Hypercalcemia: Due to parathormone, parathyroid hormone-related peptide, prostaglandin E
- Hypocalcaemia: Due to calcitonin
- Gynecomastia: Due to gonadotropins
- Carcinoid syndrome: Due to serotonin and bradykinin
Question 16. Write a short note on mesothelioma.
Answer:
Malignant mesothelioma
- Associated with heavy exposure to asbestos
Genetics
- Deletion of tumor suppressor gene CDKN2A/INK4a are seen in 80% of mesotheliomas
Morphology
Gross
- Arises from visceral or parietal pleura
- Thick, firm, white pleural tumor tissue ensheathes the lung
Microscopy
1. Epithelioid type
- Consists of cuboidal, columnar, or flattened cells forming tubular or papillary structures resembling adenocarcinoma
- IHC: Positive for calretinin, Wilms’ tumor 1 (WT-1), cytokeratin 5/6, and D2-40
2. Sarcomatoid type
- The mesenchymal type appears as spindle cell sarcoma
3. Mixed (biphasic) type: Contains both epithelioid and sarcomatoid patterns
Note:
- Fifty percent of patients die within 12 months of diagnosis
Leave a Reply