Management of Developmentally Disabled Special Children Introduction
WHO describes developmentally disabled special children as those who have been infected with either a congenital abnormality or an abnormality in the early years of their childhood which thus prevents them from full participation in the normal activities of their age group.
Table of Contents
These activities may pertain to those of social, educational, recreational, and vocational nature.
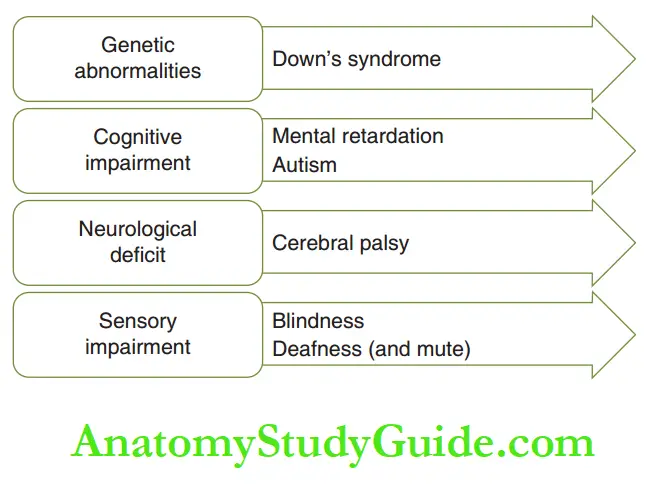
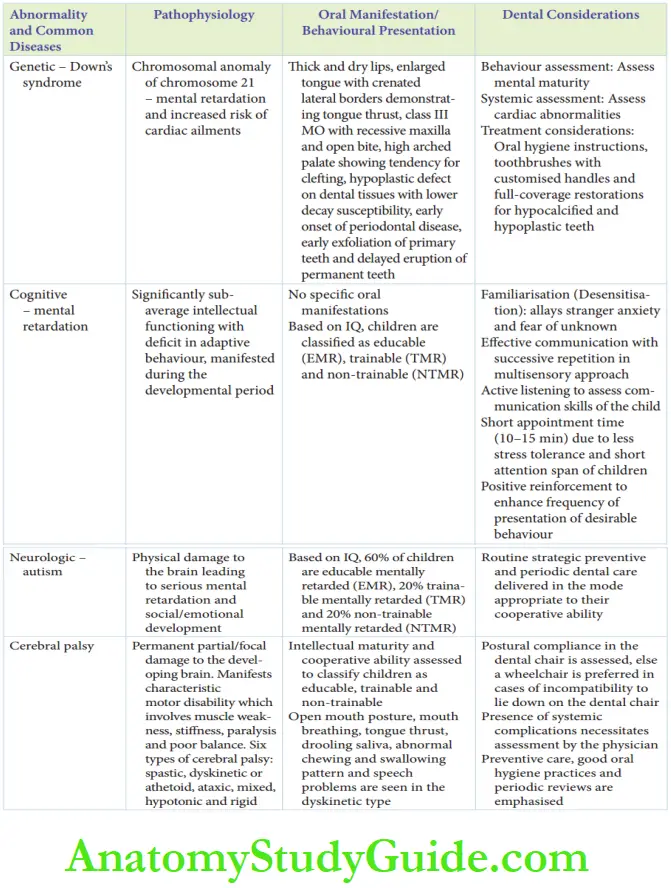
The developmental abnormalities may be classified into genetic abnormalities, cognitive impairment, neurological defects, and sensory impairment.
Read And Learn More: Paediatric Dentistry Notes
Genetic Abnormalities
All the genetic abnormalities may not significantly compromise the development or lifestyle of the child.
Genetic abnormalities that lead to a significant compromise in the development of the child demand a special status.
The most common abnormality encountered is Down’s syndrome.
There are other uncommon genetic abnormalities also, but their dental management is similar to that of Down’s syndrome.
Hence, dental management of Down’s syndrome.
Down’s Syndrome:
Down’s syndrome is a chromosomal anomaly (trisomy, translocation, or mosaicism) of chromosome 21.
The incidence is 1.5 per 1000 live births. It is most commonly associated with an increased maternal age.
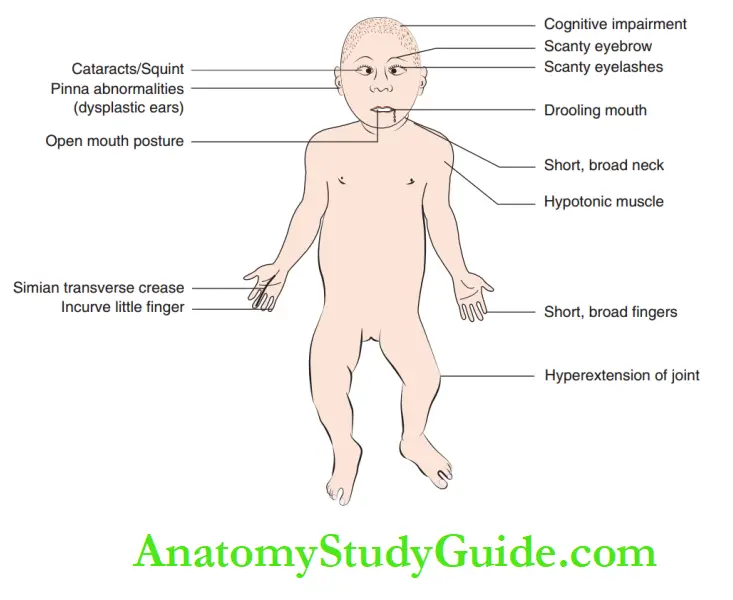
Children infected with Down’s syndrome belong to the category of special children due to the following features:
1. Moderate-to-severe mental retardation
2. Increased risk of medical complications such as cardiac diseases (40% more common), leukemia (10 -20 times higher prevalence), and immunological deficit leading to acute/chronic upper respiratory tract infection Children infected with Down’s syndrome have a characteristic facies.
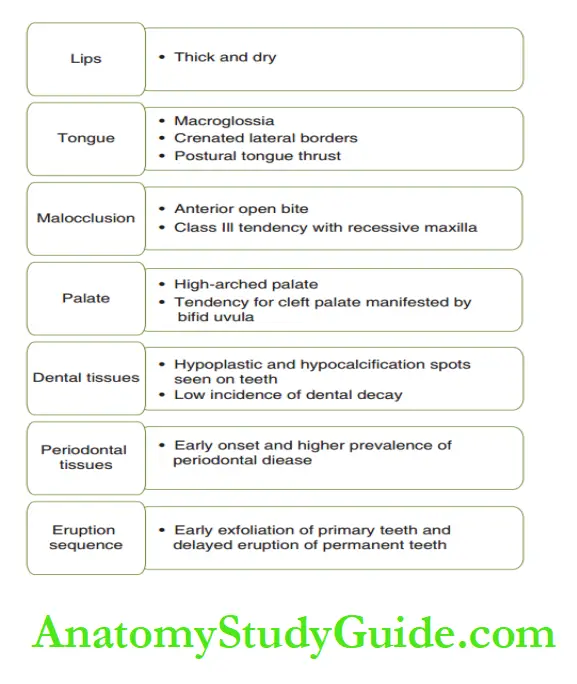
The extraoral and intraoral features, of children with Down’s syndrome, respectively.
Dental Management:
Children suffering from Down’s syndrome require additional dental attention.
Dental management may be discussed under three heads, namely, behavior management mentstrategy, systemic assessment, and dental treatment consideration.
1. Behaviour management: The behavior management technique depends on the level of intellectual maturity/cognitive development and on the severity of mental retardation in the child.
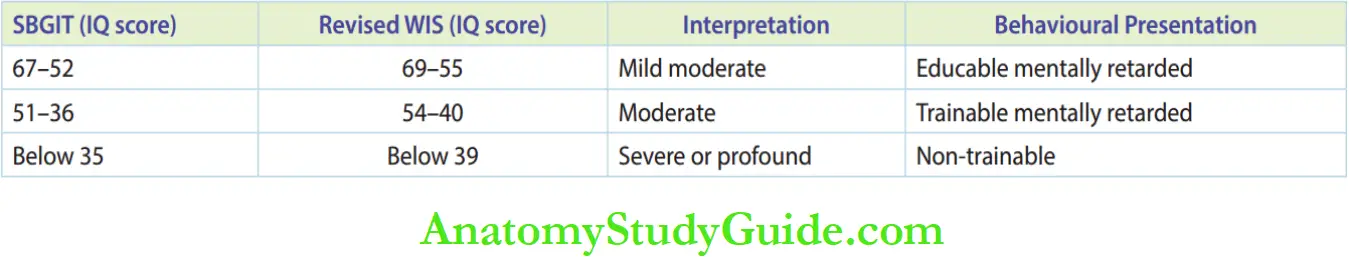
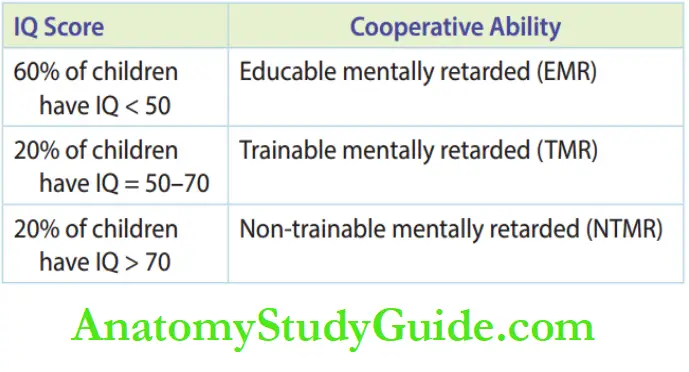
Children are classified as educable, trainable, and non-trainable based on their Intelligence Quotient.
2. Systemic assessment: This is required in the following three risky medical complications commonly encountered in these children:
Children with cardiac abnormalities require a cardiologist’s opinion and advice on fitness before undergoing dental therapy.
Prophylaxis for infective endocarditis is required during sub-gingival scaling, extraction, and endodontic procedures.
Children with leukemia may have an altered immunological response.
They also require a physician’s consent on their fitness to undergo the dental procedure.
Chronic upper respiratory tract infections may contraindicate the child for general anesthetic administration.
3. Dental treatment considerations: The affected child is at an increased risk of periodontal disease due to poor dexterity to perform oral hygiene measures, existing malocclusion, and coexistent systemic immune compromise.
- Oral hygiene instructions should be emphasized to the caretaker.
- Toothbrushes with customized handles (e.g. larger holding end) may be recommended for the child.
- Hypocalcifid and hypoplastic teeth may require full-coverage restorations.
Cognitive Impairment
Intellectual or cognitive impairment due to congenital or developmental conditions causes significant retardation of the development of the child.
Mental retardation and autism are common types of cognitive impairment.
Mental Retardation:
McDonald (1983) applied the term ‘mentally retarded’ to children whose intellectual development was significantly lower than that of normal persons and whose ability to adapt to their environment was consequently limited.
The American Academy of Mental Deficiency (AAMD) describes mental retardation as significantly sub-average intellectual functioning existing concurrently with deficits in adaptive behavior and manifested during the developmental period.
Mental retardation is usually expressed in the unit of Intelligence Quotient (IQ).
IQ is calculated from strategically established intelligence tests.
Two such widely used intelligence tests are as follows:
Stanford Binet General Intelligence Test (SBGIT)
Revised Wechsler’s Intelligence Scale (WIS) for children These scales calculate the mental age of children.
The IQ is then calculated by the following formula:
I.Q. = Mental age/chronological age × 100
IQ scores range from 0 to 210. The various grades of IQ with their corresponding score ranges.
IQ score ranges and their corresponding degree of mental retardation as per the two widely accepted intelligence tests.
An intellectually challenged child is classified not only on the basis of IQ but anyone who manifests both social competence and intellectual deficiency is considered intellectually impaired.
Intellectual impairment can also be classified as mild, moderate, and severe.
Mild Mental Retardation:
Intellectually challenged children are usually expected to communicate purposefully.
They can be educated on the importance of oral hygiene and insist on practicing the same.
The children can understand the proposed dental treatment procedures with the help of euphemisms.
They may be treated as a normal child with some reservations. These children are termed educable mentally retarded (EMR).
Moderate Mental Retardation:
The children’s level of communication is restricted to the basic or primary level.
These children cannot be educated to understand the importance of proceedings of a treatment procedure but can be trained to cooperate for the same.
They are termed trainable mentally retarded (TMR).
For example, the child may not understand the tooth restoration procedure, but he may be trained to keep his mouth open during the procedure.
He will not resist a bite block being placed in his mouth which can help in completing the procedure efficiently.
Severe Mental Retardation:
The children demonstrate very little or mild communication ability.
They either are mute or communicate with inappropriately pronounced words or syllables.
Such children can neither be educated nor be trained effectively for a dental appointment.
These children truly lack cooperative ability. They are termed non-trainable mentally retarded (NTMR).
Dental Management:
Mentally retarded children have a shorter attention span and express restlessness, hypersensitivity, and over-erratic emotional behavior.
They may also present with facial and/or dental anomalies such as hypoplasia of teeth and derangement in sequence or timing of teeth eruption/exfoliation.
The children may demonstrate poor oral hygiene and vulnerability to dental caries and periodontal disease.
The two core objectives to be attained in the delivery of pediatric dental therapy to intellectually impaired children are establishing a dentist-patient-parent rapport and reducing the child’s anxiety.
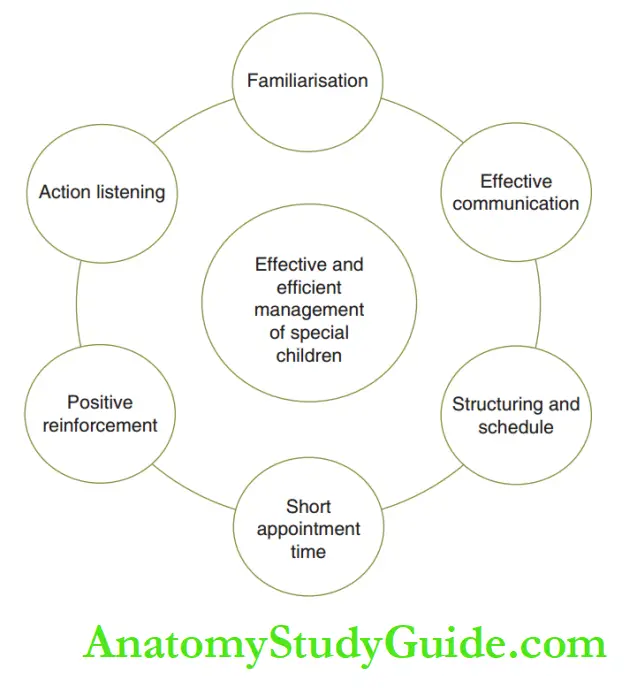
They may be attained by the following methods:
1. Familiarisation (Desensitisation): A brief tour around the dental office and the introduction of assisting personnel and staff at the reception desk family irises the child to the strange environment.
He can be desensitized to his stranger anxiety and fear of the unknown.
2. Effective communication: Simple and brief verbal communication with successive repetition in the multisensory approach is the best strategy to make the child understand the proceedings. This is used in EMR and in some TMR children.
3. Active listening: This can assess the communication skills of the child and also give the comfort of paying attention to the child.
4. Short appointment time: Generally, children have a short attention span. Appointments of 10–15 minutes are predictably uneventful.
5. Structuring and schedule: The treatment may be best scheduled early in the day when the dentist/ assistant/supporting personnel are expected to with the least fatigue.
A structured procedure enables more efficient treatment within the short attention span of the child.
6. Positive reinforcement: The child should be rewarded either by social or a material reinforcer at the successful completion of every small step of the procedure.
This reinforces the presence of desirable behavior throughout the procedure.
The dental treatment for mentally impaired special children should emphasize preventive care and regular review.
Assessment of oral hygiene practice and training of the same is also important.
Neurological Impairment
Neurological impairment is caused due to any insult or trauma to the developing central nervous system of the child.
The causes may be classified as follows:
1. Pre-natal: Maternal rubella infection, radiation damage, and genetic predisposition
2. Natal: Delayed cry and momentary anoxia to the brain during birth.
3. Post-natal: Bacterial or viral meningitis and encephalitis Cerebral palsy and autism are the commonest of neurological impairments seen in children.
Cerebral Palsy:
Cerebral palsy (CP) is a neurologic disorder caused by an insult or trauma to the developing central nervous system.
It results in permanent partial or focal organic damage of the developing brain.
Cerebral palsy occurs in 1 out of every 200 live births.
Organic damage usually develops from a single episode of anoxia to the developing brain tissue.
Perinatal causes such as complications during labor and delayed crying of the newborn may cause significant anoxia to the brain of the newborn.
Post-natal causes leading to CP are meningitis, encephalitis, and heavy metal poisoning.
Cerebral palsy manifests characteristic motor disability with lesser impairment of voluntary muscle control.
It also involves muscle weakness, stiffness, paralysis, and poor balance.
Uncoordinated and involuntary movements with abnormal gait are also evident.
Cerebral palsy is not a distinct entity; it is rather a collection of several neurological manifestations.
The presentation varies from the mildest variety with almost no perceivable symptoms to the most severe form where the individual expresses a very high degree of uncoordinated involuntary movements.
Six types of CP have been described, which are as follows:
1. Spastic cerebral palsy: It represents the majority (70%) of CP-inflicted children.
The major feature is hypermobility of the involved muscle which contracts in an exaggerated fashion.
2. Dyskinetic (athetoid cerebral palsy): 15% of CP cases belong to this type.
Characteristics show twisty or writing involuntary movements (called athetosis) or quick jerky involuntary movements (choreoathetosis).
Open mouth posture, mouth breathing, postural tongue thrust, and excessive salivary drooling are evident.
Abnormal chewing and swallowing patterns and speech problems are also features associated with this type of CP.
3. Ataxic cerebral palsy: This form represents 5% of CP cases.
In this condition, the inability of the involved involuntary muscles to contract completely results in min partially performed voluntary movements.
Poor sense of balance, staggering gait, and difficulty in grasping objects are the symptoms.
4. Mixed cerebral palsy: This variety represents 10% of CP cases.
The characteristics of more than one type of CP are seen.
5. Hypotonic cerebral palsy: In this less common type of CP, the involved muscles are flaccid with a marked loss of tonicity, making it difficult to elicit activity on stimulation.
6. Rigid type of cerebral palsy: This less common type of CP presents inflicted muscle groups in a persistent state of contraction with no stimulation.
Muscle groups lay still and resist any effort towards movement.
The other common manifestations of children suffering from CP are mental retardation (prevalent in almost 60% of individuals), seizure disorder (30–50% of individuals), hearing or visual sensory impairment (25% of individuals), speech disorders, and joint contraction.
Dental Management:
There are no unique intraoral manifestations in CP-infected children.
But the common oral/dental ailments are of a higher frequency due to the following reasons:
1. The prevalence and magnitude of the presentation of periodontal disease are higher. This is because of the following reasons:
- Poor manual dexterity of the child to perform good oral hygiene measures
- Poor intake of fibrous food
- Anti-convulsant medication prescribed induces gingival overgrowth
- The overgrowth clubbed with poor oral hygiene exacerbates the presentation
2. The incidence of dental caries is not higher than what is seen in normal children. The reason is unclear.
3. Malocclusion with conditions such as excessive overbite, overjet, unilateral crossbite, and open bite associated with abnormal oral habits is twice as common.
This is because of the following reasons:
Disharmonious relationship between intraoral and perioral musculature
Uncoordinated movement of jaws, lips, and tongue Mouth open posture with postural tongue thrust and mouth breathing
The treatment consideration involves four points, which are as follows:
1. Intellectual maturity and cooperative ability: Intellectual maturity and proportional cooperative ability are assessed.
Based on this assessment, children are classified as educable, trainable, and non-trainable.
Management of the three categories has been discussed before (see section Mental Retardation).
2. Postural compliance in the dental chair: The manifestation of enhanced muscular rigidity, hypercontractility, jerky and/or uncoordinated movements, and staggering or ataxic gait may compromise the compliance of the child to lie down on a dental chair.
If the child is not able to get onto the dental chair, the examination may be rendered on a chair where the child can be comfortably seated.
If the child is wheelchair-bound, dental examination/ treatment may be carried out as the child is seated in a wheelchair.
3. Systemic complications: The presence of systemic complications necessitates an assessment by the physician.
The physician’s opinion about the fitness of the child to undergo a particular procedure is required.
4. Preventive care: Preventive care comprising good oral hygiene practices, training and awareness of oral hygiene practices to the caretaker, fluoride application, sealant application, and periodic reviews are emphasized.
Autism
Autism is a neurologic condition resulting from a physical disorder of the brain.
It manifests serious retardation of mental, social, and emotional development leading to problems in learning and communication.
The incidence of autism is 5 children out of every 10,000 live births.
Strategic special educational programs parental care and informed guidance can help autistic children acquire basic self-help skills.
Moderate to marked mental retardation is seen in autistic children.
Dental Management:
The IQ of the child is the decisive parameter based upon which dental care is delivered to autistic children
Sensory Impairment
A sensory handicap implies a compromise of the sensual ability and includes visual impairment (blindness), auditory impairment (deafness), and speech impairment (mute).
Usually, auditory impairment and speech impairment are coexistent.
The auditory signals are recorded in the brain, based on which speech signals are incited.
Visual Impairment (Blindness):
Blindness is caused by either pre-natal or post-natal causes, although 35% of blindness relates to an unknown cause.
The common pre-natal causes are developmental in origins such as optic atrophy, cataracts, and microphthalmia, or infectious causes such as congenital syphilis, maternal rubella infections, and tubercular meningitis.
The post-natal causes include trauma, hemorrhagic disease, malignancies, glaucoma, diabetes mellitus, and malignancies around the orbit.
Blindness is a relative term. A child is visually impaired when the visual activity does not exceed
20/200 even with correcting lenses.
A child with visual activity greater than 20/200 but with a visual field of 20° or lesser is also termed visually impaired.
Blindness may not solely exist in a child. It may be associated with congenital syphilis or congenital rubella.
Mental retardation, congenital heart diseases, deafness, and dental defects may coexist in such conditions.
The children may also exhibit slow social development.
Parental attitudes towards the child may vary from overprotection to complete rejection.
These attitude extremes may result in delayed social development and delayed competency in performing self-help skills in affected children.
Such a visually impaired child may resemble a mentally retarded child.
In such a case, counseling is done by the dental care professional to the parent for having a positive attitude and affectionate behavior towards the child.
Visually impaired children may exhibit self-inflicting (sadomasochistic) habits such as eye-pressing or head-banging.
Dental Management:
A clear distinction has to be made between children who are congenitally visually impaired and those who had vision till the early part of life.
The first category needs more emphasis on the explanation of proceedings during treatment.
The explanation is accomplished through touch impulse (feel) and auditory impulse (hear).
Smell and taste impulses are reinforcers. For instance, zinc oxide eugenol cement is used cautiously so that it does not contact the oral soft tissues.
Otherwise, it may become a negative reinforcer. Usually, visually impaired children encounter traumatic dental injuries in anterior teeth prevalently.
They have also been reported to have hypoplastic teeth and gingival inflammation (associated with poor oral hygiene).
While treating a visually impaired, the patient can be addressed directly except in cases where
an interpreter is present.
Expressing sympathy or referring to blindness as a birth defect/curse is strictly avoided.
All the members of the supporting staff are introduced informally to the child.
The patient is allowed to tour around the clinic with the help of a supporting staff This familiarises the child and allays anxiety, and it makes the child feel attended to.
The patient can wear a spectacle if he feels secure with it.
The TSD approach is redefined as Touch-feel-do in the case of a visually impaired child. Sight references are avoided.
A detailed explanation of the proceeding is done and a relaxed atmosphere is maintained throughout the treatment. Adequate positive reinforcement is necessary.
Auditory Impairment (Communication [Speech] Impairment):
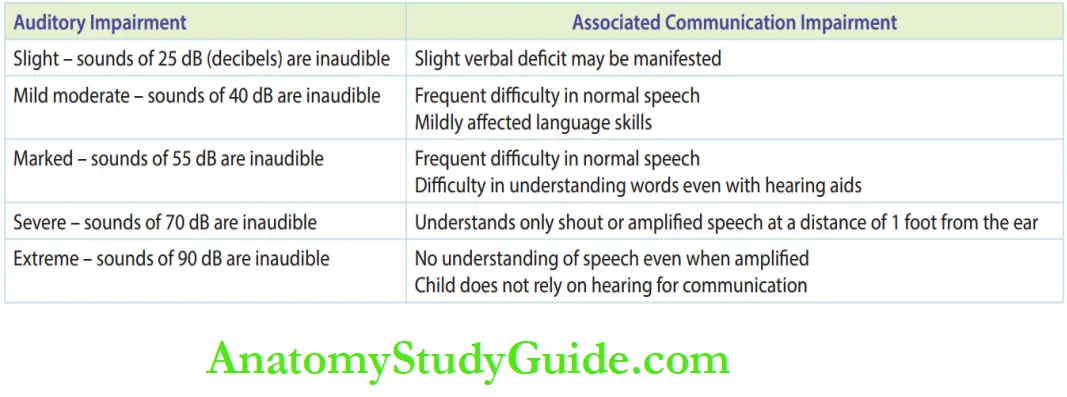
Partial or total loss of hearing ability is a significant sensory handicap as it blocks effective communication. Auditory impairment is associated with varying levels of speech impairment.
It is caused by a multitude of factors, such as follows:
1. Pre-natal factors: Maternal rubella, congenital syphilis, and ototoxic drugs such as streptomycin
2. Perinatal factors: Birth injury, erythroblastosis fetalis, and anoxia
3. Post-natal factors: Injury, ototoxic drugs, and viral infection
The auditory impairment and associated communication impairment are given in Table 62.4.
Dental Management:
Assessment of mutual communicative ability is the primary step in dental management.
Verbal conversation is less effective or ineffective. Hence, the other components of multisensory communication, that is subtle facial expression, maintenance of eye contact, and physical contact, are emphasized during communication.
Loud tones, shouting, or screams should strictly be avoided during the explanation of the procedure.
Words have to be spelled clearly and slowly to give a chance to the affected child to acquire information by lip reading.
The child has to be clearly watched to identify if he has understood what is communicated.
The tell-show-do technique may be modified with emphasis on ‘show’. The child may be allowed to touch and feel the instruments to allay his anxiety.
Hearing aids may be tuned as they may amplify all the sound. The aerator noise may distress the child
when amplified.
Positive reinforcement is necessary for continuous desirable behavior.
Summary
1. Developmentally disabled special children are those who are affected by a congenital/early abnormality that prevents them from participating in the normal activities of their age group.

Leave a Reply