Midtreatment Flare Ups In Endodontics Notes
The flare-up is described as the occurrence of pain, swelling, or a combination of these during the course of root canal therapy, which results in unscheduled visits by the patient.
Table of Contents
American Association of Endodontics defies a flare-up “as an acute exacerbation of periradicular pathosis after initiation or in continuation of root canal treatment”
Etiology
Causative Factors
- There can be mechanical, chemical, and/or microbial injury to the pulp or periapical tissues resulting in the release of a myriad of inflammatory mediators.
- Pain occurs due to the direct stimulation of the nerve fiers by these mediators or edema resulting in an increase in the hydrostatic pressure with consequent compression of nerve endings.
Mechanical Injury:
The mechanical injury occurs due to
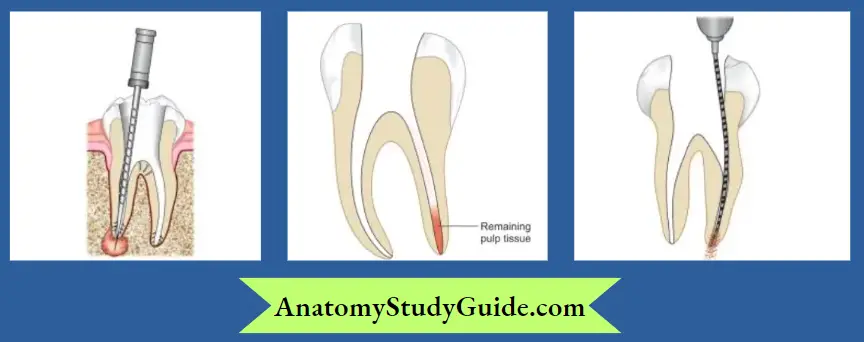
- Overinstrumentation (a most common cause of mistreatment flare-ups)
- Inadequate debridement or incomplete removal of pulp tissue
- Periapical extrusion of debris
Read And Learn More: Endodontics Notes
Chemical Injury:
Chemical injury to periapical tissue is caused by
- Irrigants
- Intracanal medicaments
- Overextended filling materials

Microbial Induced Injury:
Microbial factors in combination with iatrogenic errors cause interappointment pain.
Contributing Factors for Flare-ups:
- Age of the Patient: Patients aged 40–59 years experience more flare-ups than younger ones.
- Gender: Females show more pain incidences than males.
- Systemic Conditions: Patients with allergies to various substances (sulfa medication, pollen, dust, and foodstuff) have a higher frequency of interappointment pain.
- Tooth Type: Mandibular teeth show more interappointment emergencies than maxillary teeth.
- Anxiety: Anxious patients are likely to have more pain during the course of treatment.
- Presence of Preoperative Pain and/or Swelling: Patients taking analgesics and anti-inflammatory drugs to prevent preoperative pain have shown a higher incidence of flare-ups.
- Pulpal/Periapical Status: Teeth with vital pulps show a lower incidence of flare-ups as compared to teeth with necrotic pulp. Periradicular status of the tooth can also predict the flare-up rates, with an incidence of 3.4% in chronic apical periodontitis, 4.8% in acute apical periodontitis, and 13.1% in the case of the acute apical abscess. The presence of a sinus tract is not associated with the development of a fire-up.

- Number of Visits: If proper case selection is not done, more flare-ups occur after the multi-visit approach compared to single-visit endodontics.
- Retreatment Cases: Chances of flare-ups are 10-fold higher in retreatment cases because of the extrusion of infected debris or solvents into periapical tissues.
Mechanisms For Flare Ups
Microbiological and Immunological Factors
The following microbiological and immunological factors are responsible for flare-ups (Seltzer et al., 2004):
- Alteration of local adaptation syndrome
- Changes in periapical tissue pressure
- Microbial factors
- Chemical mediators
- Changes in cyclic nucleotides
- Immunological responses
- Psychological factors
Alteration of Local Adaptation Syndrome:
- Selye showed that when a new irritant is introduced in chronically inflamed tissue, a violent reaction may occur because of disturbance in local tissue adaptation to applied irritants.
- For example, in the case of chronic pulpal diseases, the inflammatory lesion is adapted to irritants but during root canal therapy, a new irritant in the form of medicament gets introduced in the lesion leading to flare-up.
Changes in Periapical Tissue Pressure:
In teeth with increased periapical pressure, exudate creates pain by causing pressure on nerve endings. In these cases, pain is relieved when a tooth is kept open to drain the exudate but in teeth with less periapical pressure, if kept open, microorganisms and other irritants get aspirated into the periapical area resulting in pain.
Microbial Factors:
- Gram-negative anaerobes like Prevotella and Porphyromonas species release endotoxins which are neurotoxic. These organisms also activate the Hageman factor to release bradykinin, a potent pain mediator.
- Teichoic acid, present in the cell wall and plasma membranes of Gram-positive bacteria produces humoral antibodies IgM, IgG, and IgA, and releases various chemical mediators that cause pain.
Microbial Mechanisms in the Induction of Flare-ups
- Apical extrusion of infected debris: Extrusion of microorganisms and their products during the endodontic procedures may disrupt the balance between microbial aggression and host defense leading to acute periapical inflammation

- Changes in the endodontic microflora and/or in environmental conditions: Incomplete chemomechanical preparation disrupts the balance between different microbial communities within the root canal system resulting in fire-up

- Secondary intraarticular infection: Penetration of new microbial species, microbial cells, and substrate from saliva into the root canal system during treatment may lead to a secondary infection and can be a cause of fire-up.

- Increase of oxidation–reduction potential: Alteration of oxidation–reduction potential during endodontic treatment may favor the overgrowth of facultative bacteria that resist chemomechanical procedures resulting in flare-ups.

Effect of Chemical Mediators:
- Chemical mediators are in the form of cell mediators, plasma mediators, and neutrophil products. Cell mediators include histamine, serotonin, prostaglandins, platelet-activating factor, etc. which cause pain. Plasma mediators are present in the circulation in inactive precursor form and get activated on coming in contact with irritants.
- For example, the Hageman factor when gets activated after coming in contact with irritants produces multiple effects like the production of bradykinin and activation of the clotting cascade, which may cause vascular leakage.


Changes in Cyclic Nucleotides:
Bourne et al. showed that the character and intensity of the inflammatory and immune response is regulated by hormones and mediators. In flare-up cases, there is= an increase in cGMP which stimulates mast cell degranulation and a decrease in cAMP which inhibits mast cell degranulation
Immunological Response:
- In chronic pulpitis and periapical disease, the presence of macrophages, and lymphocytes indicates both cell-mediated and humoral response.
- Despite their protective effect, the immunologic response also contributes to the destructive phase of the reaction, which causes perpetuation and aggravation of the inflammatory process.
Psychological Factor:
Anxiety, apprehension, fear, and previous history of dental experience play a contributory role in mid-treatment flare-ups.
Clinical Conditions Related To Flare Up
Flare-ups in endodontics may be grouped as
- Interappointment flare-ups
- Postobturation flare-ups
Interappointment Flare-ups:
The following conditions can be seen during the course of endodontic treatment.
Apical Periodontitis Secondary to Treatment:
An asymptomatic tooth before initiation of endodontic treatment becomes sensitive to percussion during treatment which can be due to
- Overinstrumentation
- Overmedication
- Forcing debris into periapical tissues
- Confirmatory test: Apply the rubber clamp and use a sterile paper point. Access and mark the working length. Then, place the paper print in the canal. In case of overinstrumentation, the paper point will go beyond working length without obstruction. On withdrawal, the tip of the paper point shows a reddish or brownish color indicating inflamed tissue in the periapical region and the absence of a stop in apical preparation.
- Management: An intracanal corticosteroid–antibiotic medication is given to the patient for symptomatic relief. Medication is carried on a paper point and applied with a pumping action so as to reach the inflamed periapical tissues. Routine endodontic therapy may be continued after 2–5 days after readjusting the working length.

Incomplete Removal of the Pulp Tissue:
- Incomplete removal of inflamed pulp tissue can cause pain.Confirmatory test: Apply rubber dam and place a sterile paper point; on removal, it shows brownish discoloration indicative of inflamed seeping tissue.
- Management: Re-establish the working length and remove the remaining pulp tissue.
Recrudescence of Chronic Apical Periodontitis (Phoenix Abscess):
This condition occurs in teeth with necrotic pulps and asymptomatic apical lesions. The reason for pain in these cases is the alteration of the internal environment of the root canal space during instrumentation which activates the bacterial flra.
- Management: Apply the rubber dam and allow it to drain. Drainage is allowed until exudation ceases or a slightly clear serum drains. Irrigate the canal using sodium hypochlorite, dry it with paper points, place an appropriate intracanal medicament, and seal it with a dry cotton pellet and a temporary restoration.
Recurrent Periapical Abscess:
It is a condition where a tooth with an acute periapical abscess is relieved by emergency treatment after which the acute symptoms return. In some cases, the abscess may recur more than once due to microorganisms of high virulence or it results in resistance.
- Management: Management is the same as discussed above for Phoenix’s abscess.
Flare-ups Related to Necrotic Pulp:
- Teeth with necrotic pulp often develop as acute apical abscesses after the initial appointment. As the lesion is confined to the bone, there occurs severe pain.
- Management: Th drainage is established, canal copiously irrigated and the tooth sealed after placing an intracanal medicament of calcium hydroxide. Increasing the appointment time allows more exposure of the bacteria to irritants like hydrogen peroxide and sodium hypochlorite, thus reducing the chances of flare-ups.
Postobturation Flare-ups:
- Postobturation flare-ups are relatively infrequent as compared to interappointment flare-ups. Only one-third of endodontic patients experience some pain after obturation.A mild pain is usually present which may resolve spontaneously.
- Patients experiencing preoperative pain are more likely to suffer from post-obturation flare-ups. Another cause of post-obturation flare-ups may be overextended root canal filings.
- Management: Mild-to-moderate pain may be controlled with analgesics. For severe pain, retreatment is indicated. When nonsurgical retreatment is not possible, surgical intervention is required.
Management Of Flare-Ups
As the etiology of flare-ups is multifactorial, many treatment options have been advocated for the prevention and alleviation of symptoms during root canal therapy.
Management of flare-ups can be categorized as
- Preventive management
- Definitive management.
Preventive Management:
- Accurate Diagnosis: An accurate diagnosis of the condition should be made to prevent incorrect treatment that may cause pain/swelling to the patient.
- Long-Acting Local Anesthetics: Long-acting anesthetics, for example, bupivacaine, provide an increased period of analgesia for up to 8 h during the immediate postoperative period.
- Determination of Proper Working Length: Inaccurate measurement of working length may cause under or overinstrumentation and extrusion of debris, irrigants, medicaments, or obturating materials beyond the apex.
- Complete Debridement: Through cleaning and shaping of root canal system by crown-down preparation and maintaining apical patency reduce the incidence of flare-ups.
- Occlusal Reduction: Pain relief provided by occlusal reduction is due to the reduction of mechanical stimulation of sensitized nociceptors.

Placement of Intracanal Medicament in Multivisit Root Canal Treatment
Calcium hydroxide is used as an intracanal medicament for the prevention or treatment of flare-ups. It serves the following purposes:
- Antimicrobial action: Calcium hydroxide hydroxylates the lipid moiety of bacterial lipopolysaccharide, rendering it incapable of producing biological effects and complement activation. It absorbs carbon dioxide thus nutritionally depriving the capnophilic bacteria in the root canal system. The antimicrobial effect of calcium hydroxide remains in the canal for one week
- It obliterates the root canal space which minimizes the ingress of tissue exudates, a potential source of nourishment for remaining bacteria
- Extrusion of calcium hydroxide periapical reduces inflammatory reaction by reducing substrate adherence capacity of macrophages
- Calcium hydroxide has soft tissue dissolving properties because of its high pH. Its denaturing effect on the necrotic tissue allows sodium hypochlorite to dissolve the remaining tissue more easily
Chlorhexidine gluconate, iodine, and potassium iodide are other primary medicaments that can be considered. The use of phenolic medicaments that have an immunologic potential should be avoided to prevent the occurrence of flare-ups.

Medications:
- Systemic antibiotics: These is not indicated in the prevention of flare-ups for healthy patients with localized infections. Antibiotics are recommended only in cases of medically compromised patients at high-risk levels and in cases of spreading infection that indicates failure of local host responses to control bacterial irritants. Commonly prescribed antibiotics are penicillin, erythromycin, or cephalosporin. Metronidazole, tinidazole, ornidazole, and clindamycin are also used because of their efficacy against anaerobic bacteria
- Analgesics: Nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen are the most commonly used drugs to reduce pain. Treatment with an NSAID before a procedure has been shown to reduce postoperative pain. The most commonly used drugs include ibuprofen, diclofenac sodium, and ketorolac
Closed Dressing:
Leaving a tooth open for drainage is contraindicated as it can cause contaminations from the oral cavity and lead to flare-ups. The tooth is allowed to drain under a rubber dam and closed immediately to prevent secondary infection.
Behavioral Management:
Providing information about the procedure is an important step in reducing patient anxiety.
Definitive Treatment:
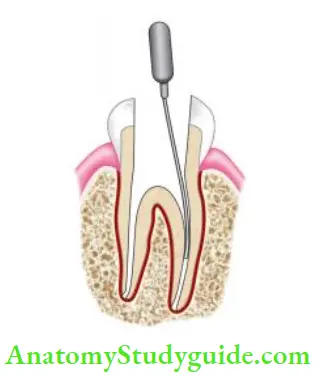
Drainage through Coronal Access Opening:
- The first step in relieving pain is to establish drainage through a root canal. Sometimes apical trephination may be needed to establish drainage.
- In patients with periradicular abscess but no drainage through the canal, penetration of the apical foramen with small files may establish drainage that helps in reducing the periapical pressure, thus alleviating the symptoms.
Incision and Drainage:
- Occasionally, more than one abscess is present in relation to the tooth. One communicates with the apex, while the other is present in the vestibule.
- As they do not communicate with one another, flare-ups can be best managed through a combination of canal instrumentation and incision and drainage.
Complete Cleaning and Shaping:
- Under profound local anesthesia, working length should be re-established, apical patency is obtained and thorough chemomechanical preparation is done.
- This removes the necrotic tissue, microorganisms, and toxic products responsible for causing pain.
Trephination:
- When drainage through the canal is not possible due to restorative issues, or in case of certain conditions like failing treatments or necessary correction of procedural accidents, surgical trephination can be used as a palliative measure.
- It involves the surgical perforation of the alveolar cortical plate over the root end to release the accumulated exudates to release pain. However, it is not the first line of treatment because of additional trauma, invasiveness, and questionable beneficial result.
Intracanal Medicaments:
Use of corticosteroid–an antibiotic combination as an intracanal medicament is recommended to reduce pain, especially in cases of overinstrumentation.
Analgesics and Antibiotics
- For most patients, NSAIDs are sufficient to control pain. However, if pain can’t be controlled with NSAIDs, opioid analgesics can be used as a supplement to NSAIDs. Commonly used opioids include morphine, codeine, meperidine, tramadol, and propoxyphene.
- Antibiotics are prescribed for the treatment of flare-ups only when indicated, as discussed before. The use of antihistaminics for the treatment of flare-ups has also been suggested
.
Midtreatment Flare-Ups In Endodontics Conclusion
- The development of flare-ups during endodontic treatment appointments is an extremely undesirable and challenging problem.
- Despite judicious and careful treatment procedures, severe pain, swelling, or both may occur.
- Clinicians should employ proper measures and follow appropriate guidelines to prevent these undesirable occurrences.
- Psychological preparation of the patient, thorough cleaning and shaping of the root canal system, and use of long-acting anesthetic solutions and analgesics may decrease the incidence of flare-ups.
- Prompt and effctive treatment of flare-ups is essential to alleviate the patient’s symptoms and prevent their recurrence.
Leave a Reply