Paediatric Endodontics Introduction
Paediatric dentistry primarily aims to preserve and restore the integrity of the dental arch by maintaining the dental arch circumference.
Table of Contents
This can be accomplished by keeping the natural space maintainers, that is, the natural teeth, intact.
Despite increased awareness and modern modes of caries prevention, the prevalence of dental caries remains high. We discussed the restorative management of dental caries in detail.
Read And Learn More: Paediatric Dentistry Notes
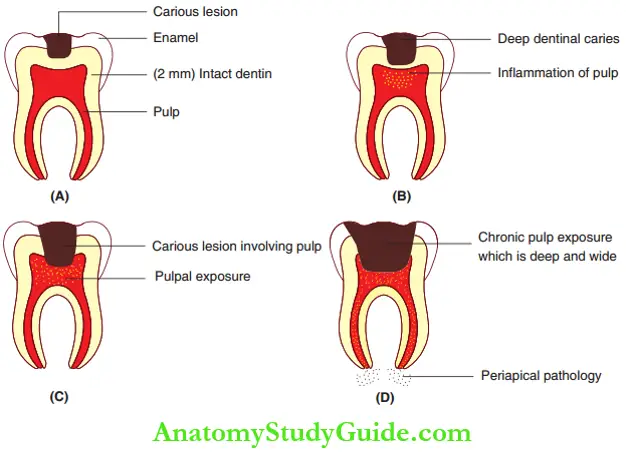
When dental caries involve the enamel and the outer half of the dentin, leaving 2 mm of intact dentin around the pulp, a restorative procedure can re-instil the integrity of the tooth and the arch.
However, with deeper dentinal involvement, frank pulpal exposure or its sequelae, the pulp of the primary tooth requires attention. Rehabilitation of the tooth is necessary to maintain the integrity of the dental arch.
The diagnosis, disease limitation, sepsis elimination and restoration of the health of the pulpodentinal complex constitute endodontic therapy or pulp therapy.
It shows the extent of carious involvement that decides whether the intervention should be a restorative procedure or an endodontic therapy.
Pulpal Inflammation
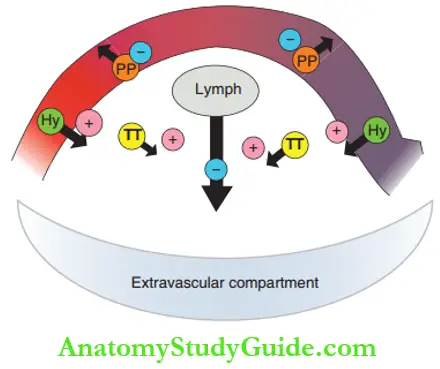
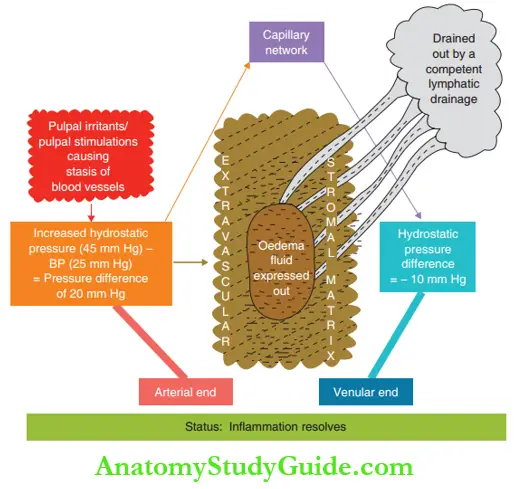
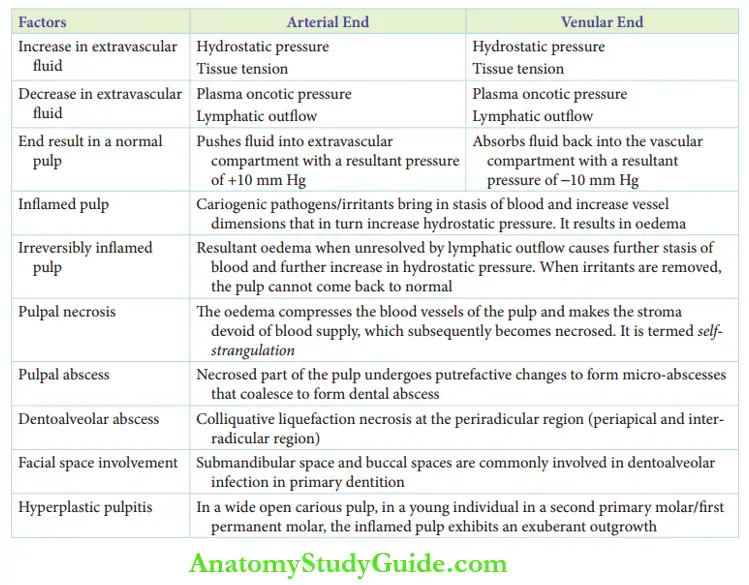
It is essential to know about the blood circulation of the normal pulp to understand the pathology of pulpal involvement. It can be described as arterial ends breaking into capillaries and uniting back to form venular ends on an interstitial stromal matrix.
The stroma represents the extravascular component. Pulpal pathology starts with oedema in the extravascular stroma.
The following four factors influence the rate and quantity of extravascular stromal oedema of the pulp:
- Hydrostatic pressure
- Plasma oncotic pressure
- Tissue tension
- Lymphatic outflow
At the arterial end of normal pulp:
1. Hydrostatic pressure: It is a force that causes the flow of liquid into the extravascular stroma.
2. Plasma oncotic pressure: It is the plasma protein-mediated osmotic pressure that retains the intravascular fluid to decrease extravascular oedema formation.
3. Tissue tension: The tension with which a tissue (extravascular stroma) retains its fluid is called tissue tension.
A lesser quantity of proteins in extravascular stroma has an osmotic pressure that retains the fluid in the extravascular compartment, thus increasing oedema.
4. Lymphatic outflow: The extravascular fluid collected is drained by the lymphatic outflow which decreases oedema.
In the venular end of normal pulp:
- Hydrostatic pressure at the venous end pushes fluid into the extravascular stroma.
- Plasma oncotic pressure retains the fluid to decrease oedema formation.
- Tissue tension retains the flid to increase oedema.
- Lymphatic outflow drains the fluid in the extravascular component to decrease oedema formation.
There is no extravascular fluid accumulation or oedema in a normal uninflamed pulp as the plasma oncotic pressure, tissue tension and lymphatic outflow are the same in the arterial and venular ends.
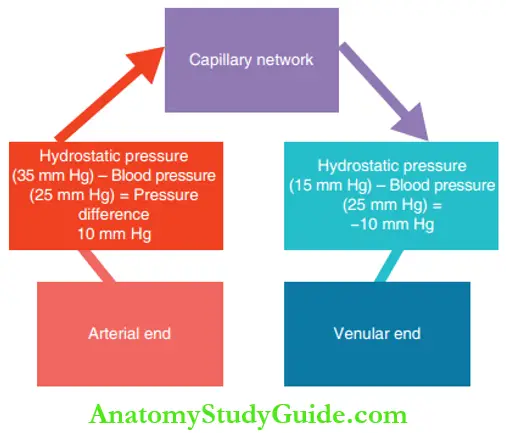
The average (normal) hydrostatic pressure in the blood vessels is 25 mm Hg. The same at the arterial end is 35 mm Hg and at the venular end is 15 mm Hg.
Thus, the amount of fluid collecting in the extravascular compartment is determined by the hydrostatic pressure difference between the arterial and venular ends.
At the arterial end, the hydrostatic pressure difference with tissue pressure is 10 mm Hg (35–25).
Thus, fluid is expressed into the extravascular stroma. Concurrently, there is a negative pressure of 10 mm Hg (15–25) in the venular end.
This sends the fluid back into the vascular component (out of the extravascular component).
Hence, the same quantity of fluid is driven by the same equalised pressure in/out of the extravascular component resulting in no oedema.
Pulpal Inflammation Sequelae Of Pulpal Inflammation
Pulpal inflammation can be acute or chronic. As mentioned earlier, pulpal inflammation begins with extravascular stromal oedema.
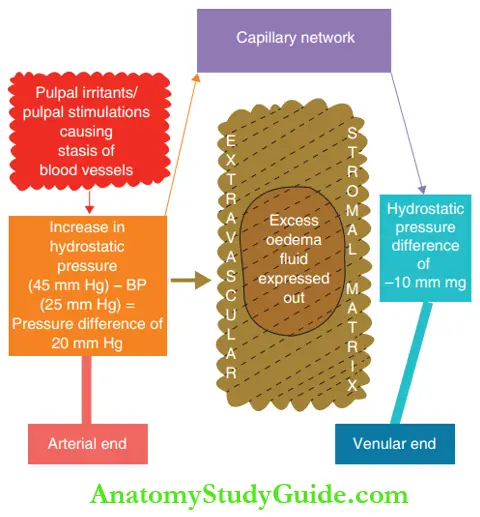
The first reaction of an inflamed pulp is the stasis of the blood. This is due to the products of cariogenic pathogens, cavity preparation or irritants.
The stasis of blood causes an increase in the dimension of the blood vessels.
This in turn increases the hydrostatic pressure at the arterial end than that at the venular end. This results in oedema of the stromal matrix.
1. Reversibly Inflamed Pulp
When the pulp is competent enough to resolve the oedema and restore normal physiology, it is said to be reversibly inflamed.
If the reversible inflammation is momentary, that is, for a very short duration, it is termed transient reversible inflammation.
In a reversibly inflamed pulp tissue, the oedema fluid collected in the extravascular stroma can be absorbed back when the inflammatory aetiology is removed.
The fluid can also be removed from the site by a lymphatic outflow.
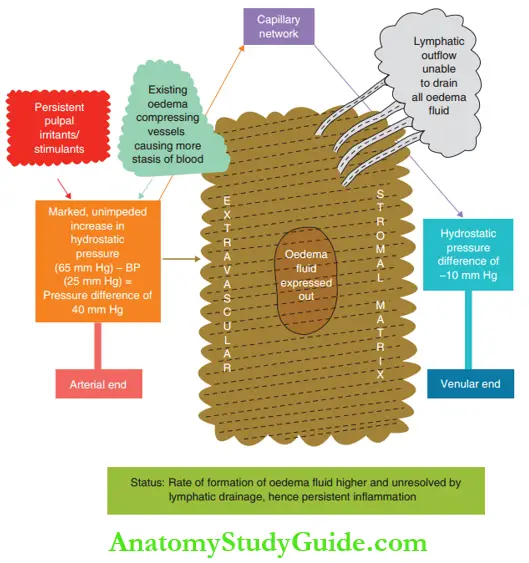
2. Irreversibly Inflamed Pulp
When the pulp reaches a state where it is not competent enough to restore normal physiology even after the inflammatory stimulus is removed, it is said to be irreversibly inflamed.
The lymphatic outflow is unable to resolve the oedema fluid completely and oedema persists. It exerts pressure on the blood vessels that it upholds.
The exertion of pressure on the blood vessels further causes stasis of blood flow.
This increases the hydrostatic pressure differential that increases oedema, thus becoming a vicious cycle.
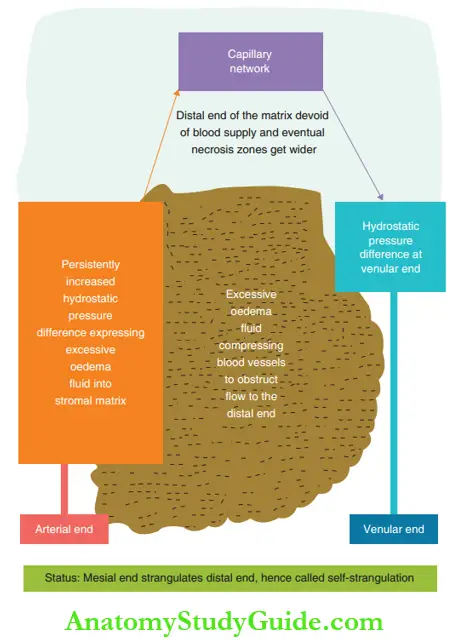
3. Pulpal Necrosis
When the state of irreversible pulpal inflammation persists, the amount of fluid collected in the extravascular component increases.
This tends to compress the blood vessels, thus strangulating and obstructing the blood flow.
As a result, the stromal tissue distal to the site of strangulation is devoid of blood supply. This is described as the self-strangulation of the pulp.
The stromal tissue devoid of blood supply undergoes subsequent necrosis and the pulp becomes non-vital.
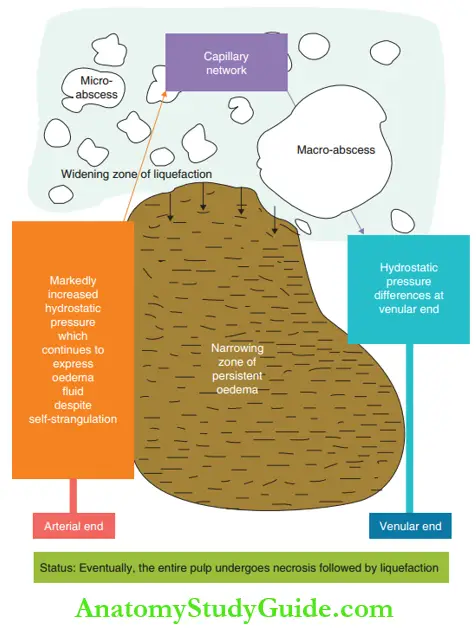
4. Pulpal Abscess
The self-strangulated area of the pulp undergoes colliquative necrosis (liquefaction degeneration) where the entire anatomy is obscured.
These areas subsequently undergo putrefactive degeneration forming micro-abscesses that coalesce to form larger foci. It progresses to form a dental abscess.
The points of the clinical significance of pulpal inflammation are discussed in Box.
Clinical Significance Of Dental Pulp
- Signifiance of pulpal compliance:
The oedema fluid collected in the stroma can be resolved by the ability of the pulp to do so, which is termed as its compliance in handling oedema.
When the compliance mechanism is outwitted, due to a higher rate and quantity of oedema formation, a reversibly inflamed pulp slips into a stage of irreversible inflammation.
The compliance of the pulp in resolving oedema is a measure of its lymphatic outflow.
Contemporary researchers, almost a decade back, have concluded that dental pulp is poorly compliant owing to poor lymphatic outflow.
However, the current perspective has evidence to prove that the lymphatic drainage of the pulp is acceptable, if not efficient, and the dental pulp is an acceptably compliant chamber.
- Painless nature of a chronically inflamed pulp:
When carious lesions are open and extensive, they have a higher number of dentinal tubules that are open and patent.
The fluid collected in the stroma can be continuously expressed through these open patent tubules. This does not induce a stretch response on the free nerve ending to initiate pain.
- Pulpal pain:
When the pulp is gently touched, or when exposed to cold or heat, the only response is pain. The sensory receptors for touch are Merkel’s disc.
The same for heat is Ruffi’s corpuscle, for cold is Krauss fires and for pressure is Pacinian corpuscles. The sensory receptors for pain are free nerve endings. The only predominant sensory receptors in the pulp are free nerve endings.
That is the reason why the pulp can only respond as pain, whatever the stimuli
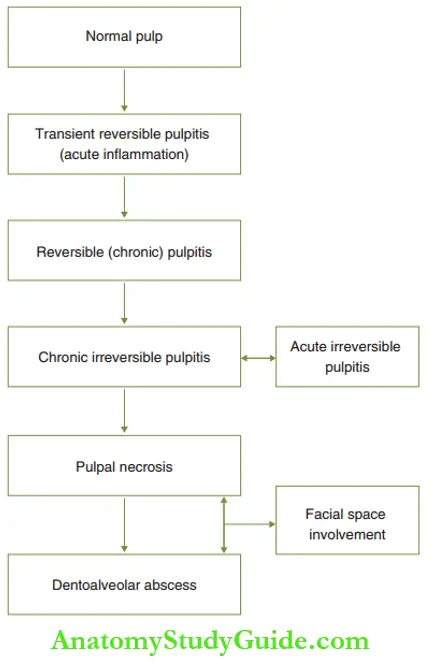
The sequelae of inflammation of the dental pulp are illustrated in depicted.
5. Dentoalveolar Abscess
Pulpal abscess gravitates to involve the periapical region. There is colliquative or liquefaction necrosis at the periarticular region.
The periradicular region includes the periapical region (root tip) and the inter-radicular region (in between roots, below furcation area) in multi-rooted teeth.
This is referred to as a dentoalveolar abscess. The necrosis involves the periodontal ligament and alveolar bone and may involve the cementum also.
In primary molars, the periradicular dentoalveolar abscess is at the inter-radicular region rather than at the periapical region. The reason for this is more lateral canals at the furcation area.
Dentoalveolar abscess undergoes one of the following sequelae: Abscesses become larger and result in enhanced mobility of the tooth. They accentuate the exfoliation of the primary tooth.
The abscess evolves as a sinus tract lined by granulation tissue to drain the pus collected through a punctum in the marginal or attached gingiva.
The abscess gravitates into a space infection by spreading into the soft tissues below the muscle attachment.
6. Facial Space Infection
The facial spaces commonly involved in the dentoalveolar infection of primary dentition are the submandibular space and buccal space.
The parameters that decide whether a dentoalveolar infection culminates into a space involvement are as follows:
- Length of the root and its relation with the muscle attachment: If the length of the root is high, that is, beyond the muscle attachment, the infection perforates the bone to slip into muscle spaces.
- Virulence of the micro-organism: If the virulence of micro-organisms is high and the micro-organisms have the potential to produce hyaluronidase as their product.
- The infection can decent the tissue attachments allowing the infection to pass into tissue spaces.
- Immunity of the individual: If the general immunity of the individual is relatively low, the dental volar infection can gravitate into a space infection.
7. Chronic Hyperplastic Pulpitis
Inflammation is the attempt of the tissue to heal. However, pulpal inflammation, almost always, ends in pulpal degeneration. On the contrary, a chronically irreversibly inflamed pulp can also exhibit an exuberant outgrowth.
This lesion is termed chronic hyperplastic pulpitis. The occurrence of this lesion is more common in the following cases:
- In the second primary molars and first permanent molars of children
- When the carious lesion is open and pulpal exposure is wide
- The microbiota involved are of a relatively low virulent category and the host (child) expresses a good immune response.
The exuberant growth is a clear outgrowth of the pulp and bleeds excessively on manipulation. It has to be excised with the pulp stump for a complete pulpectomy.
Chronic Hyperplastic Pulpitis Management
The success of endodontic therapy depends upon two important parameters.
One is the diagnosis of the extent of pulpal inflammation and the other is the prognosis and choice of endodontic treatment. The various diagnostic procedures and appropriate choice of treatment methods are discussed.
Paediatric endodontic therapy can be indicated for primary teeth and young permanent teeth. The mode of therapy can be conservative or radical depending upon the extent of pulpal inflammation.
The reversibly inflamed pulp can be treated by conservative methods such as pulpotomy or pulp capping. The irreversible inflammation of pulp and sequelae have to be treated by radical modes such as pulpectomy and obturation.
Summary
1. Natural teeth are the best space maintainers. Dental caries is highly prevalent that necessitates the following:
- Restorative procedures: When the dental pulp is not involved, primarily to restore the integrity of the tooth
- Endodontic procedure: Deeper layers of dentin and/or pulp are involved
2. Pulpal pathology starts with oedema in the extravascular stroma. The factors influencing oedema formation are as follows:
3. Reversible inflamed pulp becomes irreversibly inflamed when the ability of the pulp to resolve oedema (by lymphatic outflow) is outwitted by the rate and quantity of oedema formation.
4. The lymphatic drainage of the pulp is acceptably compliant to resolve oedema to a certain degree.
5. Chronically inflamed pulp associated with open pulp or wide carious lesions is usually painless.
6. The predominant nerve receptor in pulp is the ‘free nerve ending’, which senses pain, whatever the stimulus.
7. The pathophysiologic sequelae of the pulp are illustrated.
Leave a Reply