Dental Anomalies Dental Caries Pulp Periapical And Periodontal Lesions Essay Questions
Question 1. Discuss in detail the radiodiagnosis of periapical lesions.
Answer: Periapical lesions are classified into periapical radiolucencies and radiopacities.
Table of Contents
Peripaical Radiolucencies:
- Periapical periodontitis
- Periapical granuloma
- Periapical abscess
- Periapical cyst
- Residual cyst
- Periapical scar
- Surgical defect.
Read And Learn More: Oral Medicine and Radiology Question And Answers

Periapical Periodontitis: Inflammation of periodontal ligament space due to the exit of toxic products from the necrotic pulp. Discontinuity of lamina dura at the root apex and widened periodontal ligament space are the findings.
Periapical Granuloma: Granulation tissue formation in the periapical region to neutralize the toxic products from the root canal. It is the most common periapical radiolucency. Seen as a mixed radiopaque and radiolucent but predominantly radiolucent lesion measuring less than 1 cm in size.
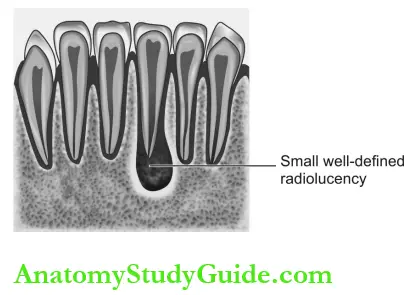
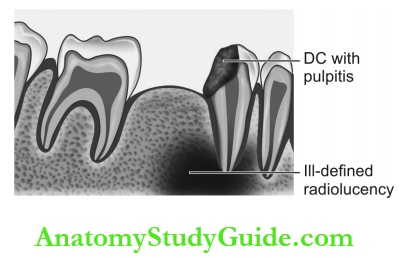
Periapical Abscess: Localized collection of pus in the periapical region as a result of pulpal death results in ill-defined periapical radiolucency.
Periapical Cyst/Radicular Cyst/Dental Cyst:
- Inflammatory odontogenic cyst, resulting from periapical granuloma.
- It is the second most common periapi¬cal infection. Well-defined radiolucency is measuring more than 2.5 cm in diameter surrounded by a thin radiopaque border.

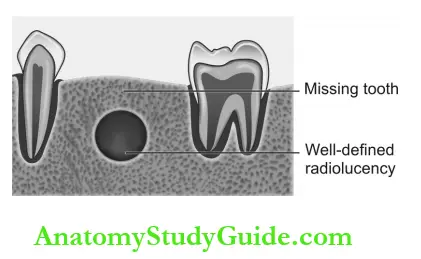
Residual Cyst:
- Cyst develops after incomplete removal of the infected materials in the periapical region of a tooth. The body reacts to the remnant infection by forming granulation tissue.
- When there is more proliferation of granulation tissues, the central region will be devoid of nutrient supply and undergoes liquefaction necrosis. It appears as a well-defined radiolucency surrounded by a thin radiopaque border.
Periapical Scar:
- A thick fibrous tissue mass in the apex of the root canal treated tooth.
- Appear as a well-circumscribed radiolucency resembling periapical granuloma or cyst (smaller than both). The anterior region of the maxilla is the common site.

Surgical Defect: Following surgery, there is a defect in the normal healing process by bone deposition. The surgical site is devoid of bone following a sufficient period of healing. It is seen as a round radiolucent lesion with a well-defined corticated border.

Periapical Radiopacities:
- True radiopacities: Radiopaque structures present in the periapical region.
- Condensing osteitis
- Periapical idiopathic osteosclerosis
- Periapical cement osseous dysplasia
- Hypercementosis
- Odontome
- Foreign bodies
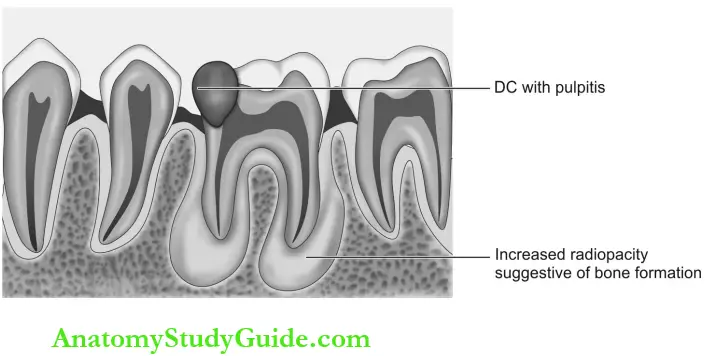
Condensing Osteitis (Focal Sclerosing Osteomyelitis): Sclerosis of bone induced by inflammation or infection. It is seen in the mandibular first molar region as a dense diffuse radiopacity near the periapical region.
Periapical Idiopathic Osteosclerosis (Enostosis): Localized growth of the cortical bone. Few mm to-2 cm diameters in size. Appear as dense, small, isolated, well-defined radiopacities, not contacting the tooth and there is no radiolucent halo at the periphery.

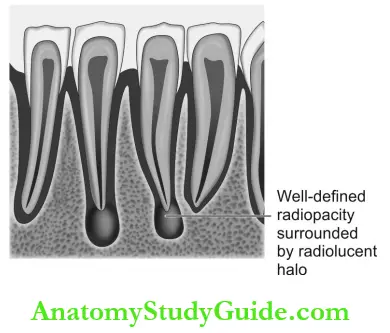
Periapical Cementosseous Dysplasia: Reactive fibro-osseous lesion derived from periodontal ligament. The mature stage reveals dense radiopacity surrounded by a radiolucent halo in the mandibular anterior region. The associated teeth are vital.
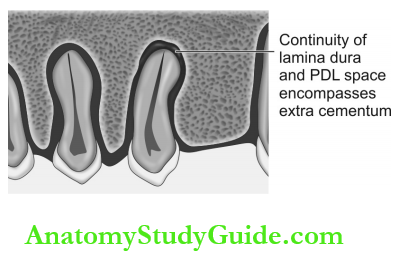
Hypercementosis: Excessive cementum deposition occurs at the entire root or the root apex because of periapical inflammation. It appears as a bulbous root with intact periodontal ligament space and lamina dura.
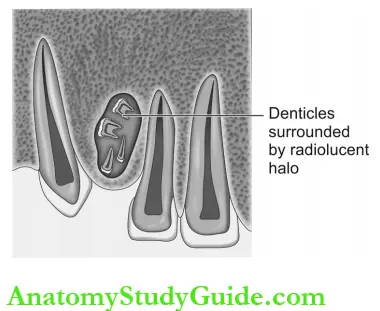
Odontome:
- Developmental hamartoma.
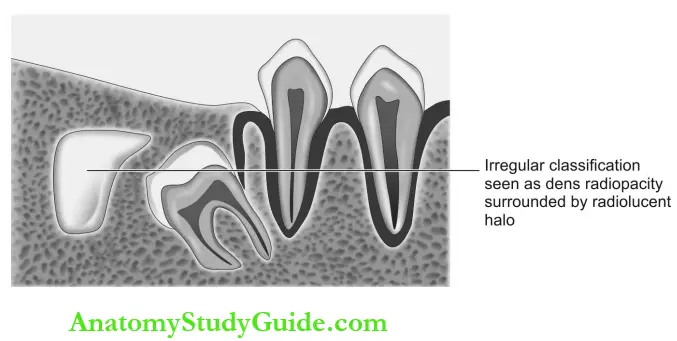
- Compound composite odontoma present as many small teeth-like structures surrounded by a radiolucent halo. It has a preference for the maxillary anterior region.
- A complex composite odontoma is seen as an irregular calcified mass. It is seen as dense radiopacity surrounded by a radiolucent halo in the mandibular posterior region. Do not resemble the tooth.

Foreign Bodies: Restorative materials extruded from the root canal-treated teeth are seen as radiopaque specks.
False Periapical Radiopacities: Structures not present in the periapical region of the teeth but the image is projected in the periapical region.
Unerupted, Impacted, Supernumerary Teeth: Cause radiopacity with central radiolucency representing the pulp chamber.
- Exostosis: Cortical bone protrusion appears as a dense radiopaque shadow.
- Torus palatines: Bony protuberance super-imposed over the apical area of roots of maxillary molar teeth.
- Torus mandibularis: Superimposed bilaterally over the apical area of roots of mandibular canines, premolars teeth.
Question 2. Mixed radiolucent and radiopaque periapical lesion.
Answer:
- Retained roots: Linear-shaped radiopacity with radiolucency in the center representing the root canal can be seen in the periapical region.
- Rarefying osteitis and condensing osteitis:
- It is associated with the pulp periapical lesion and is seen as coronal radiolucency involving the pulp. Chronic inflammation from pulp serves as an irritating factor for bone resorption seen as diffuse periapical radiolucency (rarefying osteitis) and bone deposition in response to destruction seen as radiopacity surrounding the radiolucency (condensing osteitis).
- An intermediate stage of periapical cemental dysplasia: Reactive fibro-osseous lesion derived from periodontal ligament. Three stages with different radiographic appearances:
- Radiolucency suggestive of osteolytic stage
- Mixed radiolucent radiopaque stage
- The radiopaque stage represents bone deposition.
- Cemento-ossifying fibroma: It is a benign fibro-osseous neoplasm. Three stages are seen as the same as periapical cemental dysplasia. Mixed radiolucent and radiopaque lesions were seen in the intermediate stage.
- Intermediate stage of Paget’s disease and fibrous dysplasia: Paget’s disease also called osteitis deformans is an osteodystrophy of unknown cause where physiological bone remodeling is affected due to excess bone deposition and resorption.
- Fibrous dysplasia is a localized developmental disturbance in bone-forming mesenchyme in which the fibrous tissue fails to produce bone matrix and fails to calcify. There is attempted bone formation in the fibrous tissue hence it is a fibro-osseous lesion.
- Three stages of radiographic appearances in both Paget’s disease and fibrous dys¬plasia are:
- Fibrous dysplasia is a localized developmental disturbance in bone-forming mesenchyme in which the fibrous tissue fails to produce bone matrix and fails to calcify. There is attempted bone formation in the fibrous tissue hence it is a fibro-osseous lesion.
-
-
-
- Radiolucency suggestive of osteolytic stage
- Mixed radiolucent radiopaque stage
- Radiopaque stage represents the bone deposition
-
-
Pyogenic osteomyelitis: Moth-eaten radiographic appearance representing bone resorption (sequestrum) seen as radiolucency and involucrum (new bone) seen as radiopacity.

Dental Anomalies Dental Caries Pulp Periapical And Periodontal Lesions Short Notes
Question 1. Enumerate the various conditions causing radiolucencies involving the pulp.
Answer:
- Dental caries involving the pulp.
- Fractures with pulp exposure
- Attrition with pulp exposure
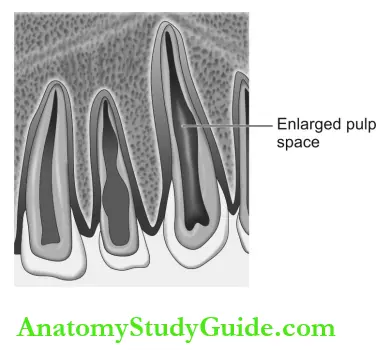
- Internal resorption—Round or ovoid radio-lucency in the pulp canal.
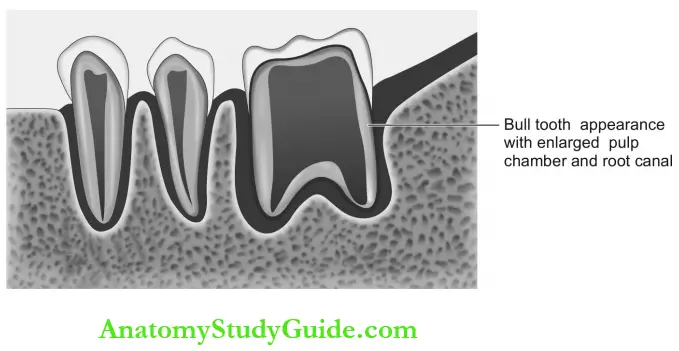
- A developmental disturbance like taur- Odontism causes enlargement of the pulp chamber appearing as a larger radiolucent pulp cavity.
- Recurrent caries—Increased radiolucency at the margin of restoration.
- Radiation caries—Dark radiolucency is seen near the necks of the teeth following radio therapy.
- Root caries—Ill-defined saucer-shaped defect on a mesial and distal aspect of the root.
- Few restorative materials like composite, plastic, and silicate without radiopaque materials like barium, lead or zinc.

Question 2. Enumerate the various conditions causing radiopacities involving the pulp.
Answer:
- Pulp stone: Foci of calcification in the pulp chamber seen as round or ovoid radiopacity occupying the pulp chamber.
- Restorative materials which appear radiopaque:
- Silver amalgam
- Gutta-percha
- Gold
- Stainless steel pins
- Silver points
- Calcium hydroxide
- Orthodontic appliances.

Talon’s cusp: Hyperplasia of cingulum of maxillary or mandibular incisors. Radi-opaque image of Talon’s cusp is superimposed on the crown of the involved incisor.
Question 3. Role of radiographs in the diagnosis of periodontal lesions.
Answer:
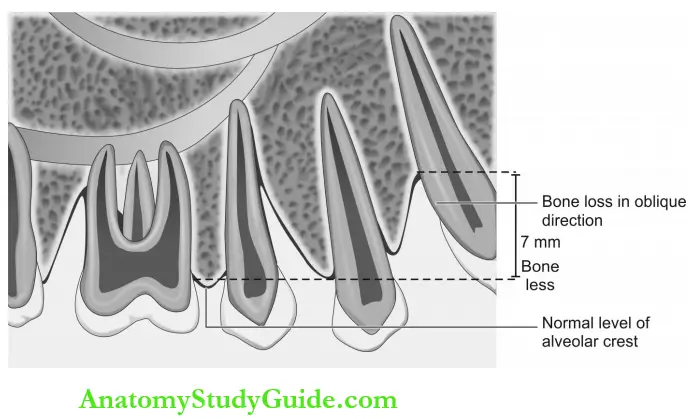
Intraoral Periapical Radiographs Horizontal bone loss:
- Alveolar bone height is reduced
- The bone margin remains perpendicular to the tooth surface
- The most common pattern of bone loss is: Bone loss may be mild, moderate or severe.
- Mild: 1-2 mm loss
- Moderate: 2-3 mm loss
- Severe: Greater than 3 mm.
- Interdental radiolucency is suggestive of the resorption of buccal and lingual cortical plates.

Vertical bone loss:
- Angular bone defect
- Bone loss occurs in an oblique direction along the side of the root.
Furcation involvement:
- Bone destruction is seen as radiolucency of the bifurcation or trifurcation of multirooted teeth
- Based on the severity it is graded from 1 to 4
Periodontal abscess:
- Localized pus collection in the periodontium is associated with a deep pocket and severe bone loss.
- Radiolucent lesion surrounding the root portion of teeth.
Bitewing radiographs:
- To detect the height of the alveolar crest
- Early periodontitis—rounding of the alveolar crest
- Open contact points.
Orthopantomogram: Generalized crestal bone loss.
Question 4. Radiographic assessment of periodontal lesions.
Answer:
- Reveals the amount of bone present.
- The height of the alveolar crest.
- Generalized widening of the periodontal ligament space around the tooth.
- Bone loss in furcation area.
- Calculus or overhanging restorations are evident as radiopacity helps in the identification of cause for periodontal lesions.
- Open contact areas between the teeth are revealed better in bitewing radiographs
- Root resorption.
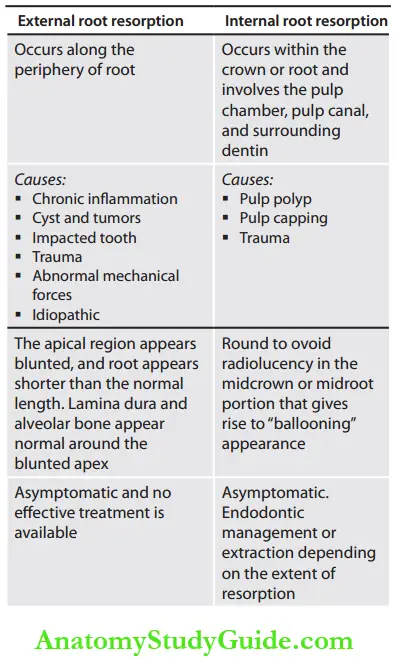
Question 5. Differentiate external and internal root resorption based on the radiographic image.
Answer:
Question 6. Enumerate the steps to overcome the limitation of radiodiagnosis of periodon¬tal lesions.
Answer:
SLOB technique: To assess whether cortical plate destruction has occurred in the buccal or lingual aspect. Fine wire grids of 1mm square size can be superimposed in radiographs during exposing radiographs to get the quantitative assessment of alveolar bone.
Digital subtraction radiography:
- Two images of the same object are recorded at different times, and then the intensities of the resultant pixels are deduced to obtain a new image.
- This method is used to evaluate dental caries and periodontal changes in the radiographs over time.
- It is not possible for the routine dental radio¬graph to predict a difference of 0.85 mm in cortical bone thickness but the subtraction technique can detect as small as 0.12 mm difference.
Question 7. Describe the radiographic diagnosis of amelogenesis imperfecta.
Answer:
Three types of amelogenesis imperfecta are:
- Hypoplasia
- Hypomaturation
- Hypocalcification.
1. Radiographic appearance of hypoplasia type:
- Square shape crown
- Thin opaque enamel
- Absence of faint cuspal outline
- The enamel density is normal except for the pitted crown in which well-defined mottled opacity appears.
2. Radiographic appearance of hypomaniaration type: Enamel appears normal in thickness but cannot be distinguished from dentin as its density is almost equal to that of dentin.
3. Radiographic appearance of hypocalcemiafication type: Enamel appears normal in thickness but more radiolucent.
Question 8. Describe the radiographic diagnosis of dentinogenesis imperfecta.
Answer:
There are 2 types:
- Type 1: Dentinogenesis imperfecta with osteogenesis imperfect.
- Type 2: Dentinogenesis imperfecta without skeletal deformities. The dental radiographic findings in both types include:
- Partial or complete obliteration of pulp chambers
- Absence or “threadlike” root canals
- Periapical radiolucencies without pulpal involvement.
- The normal alveolar bone pattern in both types.
Dental Anomalies Dental Caries Pulp Periapical And Periodontal Lesions Multiple Choice Questions
Question 1. The most common periapical radiolucency is.
- Periapical cyst
- Periapical abscess
- Periapical scar
- Periapical granuloma
Answer: 4. Periapical granuloma
Question 2. Well-defined periapical radiolucency with opaque boundary measuring above 2 cm associated with the nonvital tooth is.
- Radicular cyst
- Periapical abscess
- Periapical scar
- Periapical granuloma
(Note: Radicular cyst (or) periapical cyst).
Answer: 1. Radicular cyst
Question 3. Well-defined, round radiolucency seen over the apex of the resected root of endodontic- cally treated teeth is.
- Periapical cyst
- Periapical abscess
- Periapical scar
- Periapical granuloma
Answer: 3. Periapical scar
Question 4. Bone disease associated with distinct or denser lamina dura is.
- Paget’s disease
- Osteopetrosis
- Osteomalacia
- Myelosclerosis
(Note: Osteopetrosis/marble bone disease/ Albers-Schonberg disease).
Answer: 2. Osteopetrosis
Question 5. Dental caries in the first molar with pain on percussion clinically and associated with diffuse periapical radiolucency in an intraoral periapical radiograph is more likely to be a.
- Periapical cyst
- Periapical abscess
- Periapical scar
- Periapical granuloma
Answer: 2. Periapical abscess
Question 6. Well-circumscribed periapical radiolucency surrounded by a radiopaque border seen in the periapical radiograph of the edentulous region is more likely to be .
- Radicular cyst
- Periapical abscess
- Periapical scar
- Periapical granuloma
Answer: 1. Radicular cyst
Question 7. Dental anomaly is most commonly associated with a pulpoperiapical lesion in.
- Microdontia/peg laterals
- Supernumerary tooth/mesiodent
- Dens in dente/dens invaginatus
- Pulp stones/denticles
Answer: 3. Dens in dente/dens invaginatus
Question 8. Enostosis is otherwise called.
- Hypercementosis
- Peripheral idiopathic osteosclerosis
- Condensing osteitis
- Periapical cemental dysplasia
(Note: Dense bone island/peripheral idi¬opathic osteosclerosis).
Answer: 2. Peripheral idiopathic osteosclerosis
Question 9. The most common site for enostosis is.
- Mandibular incisor
- Maxillary canine
- Mandibular first molar
- Maxillary third molar
Answer: 3. Mandibular first molar
Question 10. Dense radiopacity seen in the periapical region of a tooth associated with a coronal radiolucency involving the pulp is most likely to be a.
- Hypercementosis
- Peripheral idiopathic osteosclerosis
- Condensing osteitis
- Periapical cemental dysplasia
Answer: 3. Condensing osteitis
Question 11. Cyst-like radiolucency of the mandible below the inferior dental canal is.
- Traumatic bone cyst
- Stafne’s bone cavity
- Klestadt cyst
- Idiopathic bone cavity
Answer: 2. Stafne’s bone cavity
Question 12. Cyst-like radiolucency measuring above 2 cm present at the apex of a vital maxillary incisor is.
- Midpalatine cyst
- Nasolabial cyst
- Incisive canal cyst
- Globulomaxillary cyst
(Note: Incisive canal cyst moves away from the apex when the horizontal angulation is changed).
Answer: 3. Incisive canal cyst
Question 13. Cyst-like radiolucency seen in the periapical region of a vital maxillary first molar is most likely a.
- Midpalatine cyst
- Nasolabial cyst
- Pseudo cyst
- Globulomaxillary cyst
Answer: 1. Midpalatine cyst
Question 14. Well-defined round or ovoid radiolucency seen above the mandibular canal with scallo¬ped margins is most likely a.
- Traumatic bone cyst
- Stafne’s bone cavity
- Klestadt cyst
- Idiopathic bone cavity
Answer: 1. Traumatic bone cyst
Question 15. Well-defined periapical radiolucency at the apex of the mandibular canine tooth with no pathology is.
- Hemorrhagic bone cyst
- Canine depression
- Y line of Ennis
- Anterior lingual mandibular bony cavity
Answer: 4. Anterior lingual mandibular bony cavity
Question 16. Any abnormal displacement of the tooth is called as.
- Luxation
- Intrusion
- Extrusion
- Avulsion
Answer: 1. Luxation
Question 17. Abnormal displacement of teeth into bone is called as.
- Luxation
- Intrusion
- Extrusion
- Avulsion
Answer: 2. Intrusion
Question 18. Abnormal displacement of teeth out of bone is called as.
- Luxation
- Intrusion
- Extrusion
- Avulsion
Answer: 3. Extrusion
Question 19. An ideal image is used to examine the interdental bone loss is.
- Vertical bitewing image
- Horizontal bitewing
- Periapical view
- Orthopantomogram
Answer: 1. Vertical bitewing image
Question 20. The radiographic diagnosis of enamel carriers is possible when the demineralization is.
- 100%
- 70-80%
- 30-40%
- 10%
Answer: 3. 30-40%
Question 21. The radiographic depth of the proximal carious lesion is.
- More than the actual clinical depth
- Less than the actual clinical depth
- As the same as the actual clinical depth
- Always magnified and distorted
Answer: 2. Less than the actual clinical depth
Question 22. In germination, the pulp chamber appears as.
- Single and enlarged
- Two separate pulp chambers of normal size
- Two separate pulp chambers of smaller size
- Single and normal size
Answer: 1. Single and enlarged
Question 23. Root dilaceration is most common in.
- Maxillary incisors
- Maxillary premolars
- Mandibular canines
- Mandibular molars
Answer: 2. Maxillary premolars
Question 24. Leong’s premolar is the synonym for.
- Dens invaginatous
- Dilated odontome
- Gestant premolar
- Dens evaginatus
Answer: 4. Dens evaginatus
Question 25. The common cause for open apical foramen is .
- Root resorption
- Trauma and crown fracture before root completion
- Cessation of root development
- Pulpotomy done in young permanent tooth
(Note: Pulpal death leads to the cessation of root development).
Answer: 3. Cessation of root development
Question 26. Flame-shaped pulp chamber present in.
- Dentin dysplasia
- Odontodysplasia
- Turner’s hypoplasia
- Syphilis
Answer: 1. Dentin dysplasia
Question 27. Multiple pulp stones is a feature of.
- Dens invaginatous
- Dens evaginatous
- Dentin dysplasia
- Odontodyspalsia
Answer: 3. Dentin dysplasia
Question 28. The semilunar radiolucency in the cervico proximal region of a tooth denotes.
- Toothbrush injury
- Dental floss injury
- Abrasion
- Erosion
Answer: 2. Dental floss injury
Dental Anomalies Dental Caries Pulp Periapical And Periodontal Lesions Viva Voce
Question 1. Anatomical radiolucent-radiopaque [mixed] lesions.
Answer:
- Developing tooth: The calcifying crown of the developing tooth within the tooth crypt is seen as cyst-like radiolucency with radiopaque foci.
- Normal alveolar bone: Trabeculations seen as radiopaque lines with marrow spaces in between seen as radiolucency.
Question 2. Limitations of radiographic diagnosis of periodontal lesions.
Answer:
- A radiograph does not reveal the total amount of bone destruction.
- Difficult to differentiate between buccal and lingual crestal bone levels.
- The early stage of bone loss is not evident.
- The depth of the pocket cannot be assessed
- Two-dimensional view of three-dimensional structure (bony defects overlapped by higher bony walls).
Question 3. Conditions associated with loss of lamina dura.
Answer:
- Fibrous dysplasia
- Vitamin D deficiency: Rickets in children and osteomalacia in adults
- Hyperparathyroidism
- Osteoporosis.
Question 4. Name the lesions with well-defined periapical radiopacity surrounded by a radiolucent halo.
Answer:
- Odontome (compound and complex)
- Mature stage of periapical cemental dysplasia
- The mature stage of cemento-ossifying fibroma
- Benign cementoblastoma.
Question 5. Name the lesions with noncorticated well-defined periapical radiopacity and not surrounded by a radiolucent halo.
Answer:
- Enostosis
- Condensing osteitis
- Exostosis.
Question 6. Mention the names of rare periapical radiolucencies.
Answer:
- Giant cell granuloma
- Ameloblastoma
- Langerhans cell disease
- Multiple myeloma.
Question 7. Name few malignant peripical radiolucent lesions.
Answer: Radiolucency with diffused margins and band-like widening of periodontal ligament space.
- Chondrosarcoma
- Osteosarcoma
- Metastatic carcinoma
- Adenoid cystic carcinoma (posterior hard palate)
- Hemangiosarcoma.
Question 8. What is horizontal and vertical bone loss?
Answer:
- The alveolar bone loss that occurs in a plane parallel to the cementoenamel junction (CEJ) of adjacent teeth is called as horizontal bone loss.
- If the crystal bone loss is not parallel to the plane of CEJ, it is called as vertical or angular bone loss.
Question 9. Describe the radiographic appearance of calculus.
Answer: Calculus appears radiopaque in a dental mage. It may be:
- Pointed or irregular radiopaque projections extending from proximal root surfaces.
- Ringlike radiopacity encircling the cervical region.
- Nodular or smooth radiopaque projection from the root.
Question 10. What is the false positive outcome in the radiograph?
Answer: False positive outcome is the appearance of a lesion on the radiograph when the object of interest is not really affected.
False positive outcome Example: Hypoplastic tooth surface and wear facet concavities resemble the appearance of the carious lesion on the radiograph.
Question 11. What is the false negative outcome in a radiograph?
Answer: False negative outcome is the radiographically unpredictable lesions whereas it is clinically predictable.
False negative outcome Example: Proximal enamel caries are unpredictable in radiographs until the demineralization reaches 30-40%.
Question 12. What is the mach band effect?
Answer: The mach band effect denotes the optical illu¬sion (false positive) in a radiograph due to a difference in density between two adjacent structures like enamel and dentin or between cementum and interdental alveolar crest.
Question 13. What is the cervical burnout phenomenon?
Answer:
- Cervical burnout is the optical phenomenon occurring as a radiolucent lesion in the cervical margin of the tooth resembling proximal caries.
- The cervical burnout occurs near the cervical margin of the tooth whereas the proximal caries occurs near the contact point. They occur more frequently in maxillary radiographs.
Types of cervical burnout: Circular type, wedge type, trapezoid type, and diffused type.
Question 14. What is the ghost-like appearance of the tooth?
Answer:
- The ghost-like tooth is the radiographic appearance of odontodysplasia or osteogenesis imperfecta. This is because both enamel and dentin are hypoplastic and hypocalcified.
- The tooth contains larger pulp chambers, wide root canals, short and poorly outlined roots, absence of enamel or thin, less dense enamel, and the overall appearance is a thin shell of enamel and dentin.
Question 15. How to differentiate internal and external root resorption?
Answer:
Internal Root Resorption: Irregular widening of the pulp chamber and canals that appears homogeneously radiolucent, either round, ovoid or elongated in shape with a smooth or slight scalloped outline.
External Root Resorption: If the resorption starts at the root apex:
- The apex appears blunted.
- The lamina dura and the alveolar bone track the resorption and appear normal surrounding the shortened root. The loss of lamina dura is common if periapical inflammation is associated with resorption.
- The pulp canal is abnormally widened in the apex
- If the resorption starts at the lateral root surface:
- The buccal and/or the lateral surface of the tooth reveals sharply defined radiolucencies confined to the root surface.
- Alveolar bone sometimes may replace the resorbed lateral surface of the tooth and the condition is known as “synostosis”.
Dental Anomalies Dental Caries Pulp Periapical And Periodontal Lesions Highlights
- Radiographic examination of the tooth and their supporting structures are essential to confirm the clinical diagnosis and precede the treatment plan. In some conditions, radiographs may serve as the only tool to diagnose the problem involving pulpal, periapical, and periodontal tissues.
- Complete knowledge about various radiopaque and radiolucent lesions involving these structures is essential for a successful dental practice.
Leave a Reply