The Musculoskeletal System
History
Table of Contents
The musculoskeletal system determines tire body build, stature, posture, and locomotion. The child should be watched for his gait and stance as he enters the tire examination chamber.
Ask the presenting complaints in chronological order with special emphasis on the mode and type of onset, whether acute or insidious and the evolution of tire disease process.
Identify whether tire symptoms are related to the muscles and other soft tissue structures or tire underlying bones and joints by asking the tired child to point to the tire’s exact site and source of discomfort.
The developmental, chromosomal, and metabolic disorders of bones and muscles are extremely common and likely to have their onset at birth or early in life.
Oligohydramnios may lead to postural defects due to in-utero positioning. Trauma is a leading cause of locomotor disability and may be precog or unreported as a consequence of child abuse.
Post-infectious and autoimmune or connective tissue disorders are primarily limited to tire muscles and joints but are recognized to involve every system of tire body including skin and integuments.
Read and Learn More Pediatric Clinical Methods Notes
Ask for the details regarding the history of discomfort, deformity, pain, and disability.
The degree of disability should be assessed by asking tire child whether he can look after tire “activities of daily living” (ADL), like toilet needs, bathing, dressing, eating, etc. independently or needs the help of the mother.
At times, tire pain in a joint may be referred from another joint or body organ, viz.
pain in the tire knee or above the patella may be referred from the involvement of the hip joint, pain in the sacroiliac joint may be referred to deep in tire buttocks, shoulder pain may occur due to irritation of the diaphragm by basal pneumonia or gallstones, and pain of subluxation of the elbow is often referred to the tire wrist joint.
Spinal pain due to the involvement of intervertebral disks manifests as constriction or girdle pains over the tire chest or abdomen.
Musculoskeletal Disorders List
The distribution of the joints involved, whether the disease is predominantly affecting tire large joints or small joints, and whether it is monoarticular, pauciarticular, or polyarticular in nature should be recorded.
A differentiation should be made between arthralgia (pain alone) and arthritis (pain with signs of inflammation). The monoarticular disease is usually suggestive of a sprain or injury, hemarthrosis, or pyogenic infection.
Migratory or flitting and fleeting joint pains, involvement of 2–3 joints for 2–3 days and then moving on to involve other joints with partial relief to the previously affected joints, is a classical feature of rheumatic fever, but may also occur due to gonococcal arthritis, meningococcal arthritis, inflammatory bowel disease, and acute leukemia.
Early morning stiffness of joints is a recognized feature of acute inflammatory joint disease especially due to rheumatoid arthritis.
Dactylitis, inflammatory spindle-shaped swellings of digits may occur due to juvenile chronic arthritis, tuberculosis, acute lymphoblastic leukemia, congenital syphilis, sickle cell disease, chikungunya, and Reiter’s disease.
Diffuse swelling of the dorsum of hands occurs due to the periosteal reaction of the metacarpals as a consequence of sickle cell disease, acute leukemia, tenosynovitis of flexor tendons, and serum sickness.
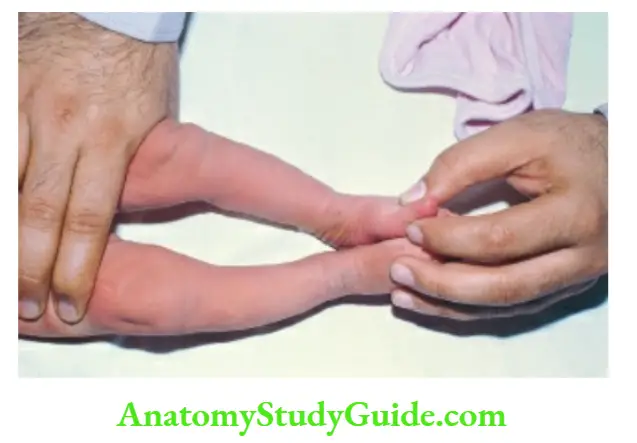
When a toddler is pulled by traction on holding at one or both the wrists or hands, subluxation of the radial head may occur.
The child cries and keeps the elbow slightly flexed and hand pronated while supination is restricted and painful.
The child is unable to lift the hand above the shoulder on the affected side. Preschool children commonly complain of pain in the legs, especially in the evening or night.
The condition is wrongly labeled as “growing pains” because discomfort actually occurs due to fatigue and tiredness in an overactive playful child.
When body pains are present at multiple sites, it is generally suggestive of a psychogenic disorder.
A localized pain in the bone may occur due to subperiosteal bleeding or periostitis or green stick fracture because of trauma, infection, new growth, or avascular necrosis due to sickle cell disease.
Episodic intractable bone pains at multiple sites, especially at night, may occur in children with acute leukemia, metastases, and metabolic bone disease.
Back pain is uncommon in children but may occur due to faulty posture, heavy school bag, sports injury, physical stress,
spinal deformity, localized infection, or tumor.
Ask for associated constitutional symptoms like anorexia, sweating, fever, toxemia, and weight loss.
The family history may give clues to possible genetic disorders, such as congenital syndromes, muscular dystrophy, and skeletal dysplasias.
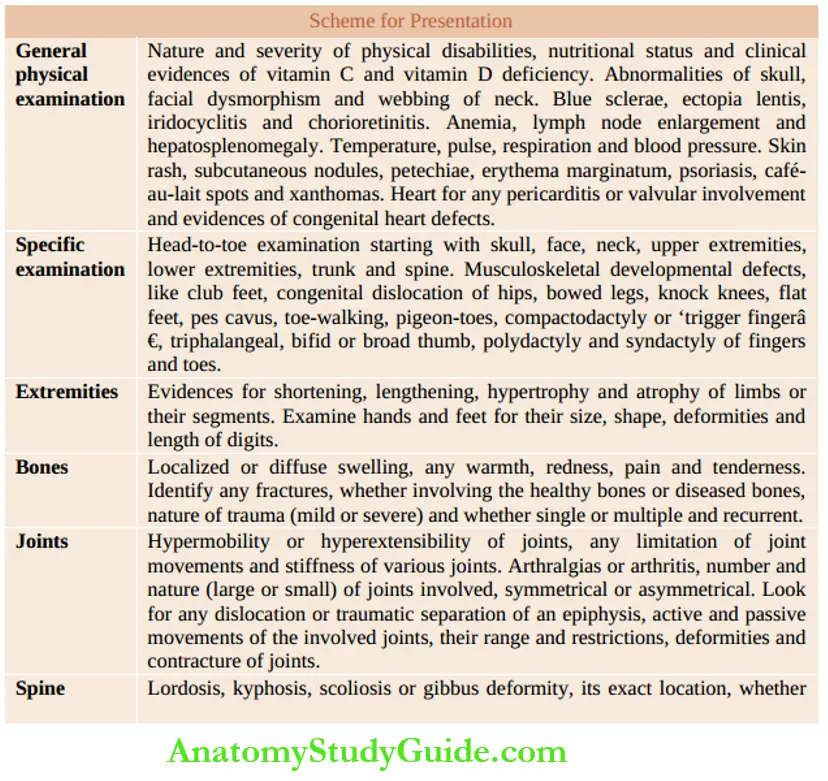
Musculoskeletal Disorders List – General Physical Examination
Observe the gait and posture of the child as he enters the examination chamber. Assess nutritional status and look for any evidence of anemia and deficiencies of vitamins (especially vitamin C and vitamin D) and trace minerals.
Eyes should be examined for blue sclerae as a marker of osteogenesis imperfecta.
Conjunctivitis is commonly associated with patients with Reiter’s syndrome, dry eyes with Sjogren syndrome, and painful iritis in patients with ankylosing spondylitis.
Subluxation of the lens or ectopia lentis may be associated in patients with Marfan syndrome and homocystinuria.
Iridocyclitis may occur in children with pauciarticular rheumatoid arthritis while chorioretinitis is a characteristic feature of TORCH infections.
Look for any obvious swellings, deformities, and functional limitations in the upper and lower extremities.
Look for any abnormalities in the hands and feet, like polydactyly, and syndactyly.
Camptodactyly or flexion deformity of the little finger may occur in association with Down, Carpenter, and Aarskog syndromes or as an isolated anomaly.
A triphalangeal hand or bifid thumb is associated with Holt-Oram syndrome while a broad thumb is a characteristic feature of Rubinstein-Taybi syndrome.
Temperature, pulse rate, respiration rate, and blood pressure should be recorded. Hypertension is commonly associated with patients with connective tissue disorder.
In children with systemic-onset rheumatoid arthritis, high-grade spiking fever with evanescent salmon pink skin rash may precede joint involvement for several days or weeks.
Lymph node enlargement in the draining areas of the disease sites and generalized lymphadenopathy should be looked for.
The skin should be examined for any evanescent macular rash, subcutaneous nodules, petechiae, erythema marginal cafe-au-lait spots, and xanthomas.
Painless, firm, non-tender subcutaneous nodules due to rheumatic fever are characteristically seen over tire pressure and friction sites, such as the olecranon, extensor surfaces of forearms, shins, and spine.
Erythematous maculopapular rash in the shape of a butterfly on the face is diagnostic of systemic lupus erythematosus.
Nonbacterial arthritis and mucosal lesions in the tire mouth and genital area are seen in adolescent children with Reiter’s disease.
Systemic examination, especially cardiovascular assessment is mandatory whenever a connective tissue disease or a metabolic disorder is strongly suspected.
Slipped femoral epiphysis may be associated with an endocrinal disorder and obesity.
Musculoskeletal Disorders Specific Examination
A detailed head-to-toe examination should be conducted starting from the vertex and gradually moving down to the face, jaw, neck, upper extremities, lower extremities, trunk, and spine.
The first aim of clinical assessment of the locomotor system is to determine whether the involvement is of the muscles, bones, joints, or soft tissue structures, such as joint capsules, bursae, tendons, and ligaments.
A great tact and expertise are required for the examination of a painful joint or extremity in children and it should be conducted in the end after completing the rest of the physical examination.
Observe the limb or joint for any swelling, redness, or deformity. Active movements should be assessed before palpation and assessment of the range of passive movements at various joints.
The toddlers should be examined in the comfort of the mother’s lap while older children should be distracted by talking to them while examining the painful joint or limb and they should be handled with utmost gentleness and tact.
Common Musculoskeletal Developmental Defects
Musculoskeletal anomalies account for one-third of all anomalies in newborn babies. Apart from developmental or chromosomal defects, they may develop due to abnormal in-utero posture or because of amniotic constriction bands.
Congenital talipes equinovarus (CTEV or club feet)
There is adduction of the forefoot, inversion of the hindfoot, and an equine position (plantar flexion) of the heel.
It is not possible to fully dorsiflex the foot by touching the dorsum of the foot with the shin, hi isolated forefoot adduction (metatarsus adduct) and abduction (metatarsus varus), it is possible to dorsiflex the foot and correct the abnormality by passive stretching and physiotherapy.
Club feet may be unilateral or bilateral and may be an isolated abnormality or a manifestation of caudal regression syndrome, meningocele, craniocarpotarsal dysplasia, Larson syndrome, dystrophic dwarfism, and spinal tumor.
Equinus position (plantar flexion) may develop due to tightness and shortening of the Achilles tendon because of cerebral palsy and in children with autism and pseudohypertrophic muscular dystrophy.
Toe walking is a characteristic feature of these children.
Musculoskeletal Disorders List Talipes calcaneal
Is less common and is characterized by eversion, abduction, and dorsiflexion of the foot which is exactly the reverse of CTEV.
The toes point upward and the arch of the foot is flat. It may be associated with dysplasia of the hip and external rotation of the tibia.
It should be differentiated from congenital vertical talus or rocker-bottom foot in which the foot is fixed in plantar flexion with reversed or convex arch of the foot.
Congenital dislocation or dysplasia of the hip (CDH)
Is more common in firstborn, breech-delivered female infants. It may be unilateral or bilateral and does not produce any visible abnormalities during the newborn period.
It is diagnosed by detailed physical examination by conducting Ortolani and Barlow tests (see Chapter 15).
When the early diagnosis is missed, it may produce asymmetry of the inguinal or gluteal fold, relative shortening of the femur on the affected side, limitation of hip abduction, delayed walking, limping, or waddling gait (bilateral CDH).
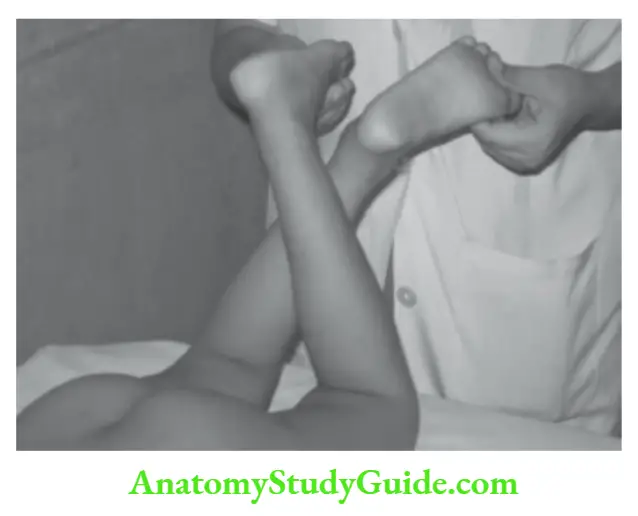
To test for apparent shortening of the femur, both hips and knees are flexed and soles are placed flat on the table.
Because of posterior dislocation of the hip, the knee on the affected side would be at a lower level than the normal side (Galeazzi sign).
Musculoskeletal Disorders List – Bowed legs (genu varum)
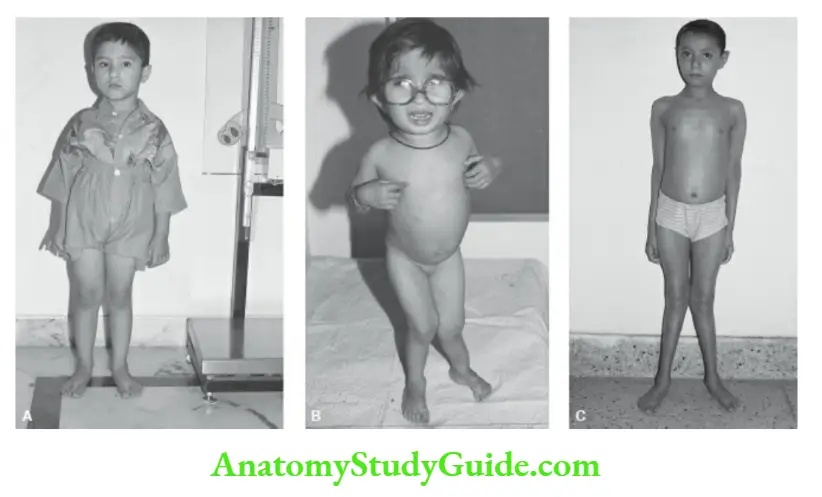
During the first 2 years of life, there is physiologic bowing of the tibia due to rotation at the knees.
When tibial bowing is genuine or marked and persists beyond 2 years, exclude the possibilities of rickets, metaphyseal dysostosis, achondroplasia, trauma, infection, tumor, and osteochondrosis of the medial tibial condyle (Blount disease).
Bloimt disease is characterized by tibia vara because of idiopathic growth disorder of the medial aspect of the proximal tibial epiphysis leading to varus angulation and internal or medial rotation of the tibia.
It is usually bilateral but when unilateral it may cause leg-length discrepancy.
The severity of bowed legs is assessed by measuring the distance between the knees when medial malleoli are closely aligned in a supine infant, hi physiologic bowed legs, the distance between die knees is less than 5 cm.
Knock-knees (genu valgum) Physiologic bowing of legs is gradually replaced by knock-knees during 2–5 years of age.
The severity of knock-knees is assessed by measuring the intermedial malleolar distance between die feet when the child stands erect with knees barely touching each other.
When the severity of genu valgum is more than 5 cm (inter-feet distance) or it persists beyond 5 years, exclude the possibilities of rickets, hypophosphatasia, Morquio disease, Hurler syndrome, and pes valgus.
Musculoskeletal Disorders List
Flat feet (pes planus) During the first 2 to 3 years of life, the arch of die feet is obliterated by a die pad of fat producing physiological dat feet. When a child is asked to stand on tiptoes, the arch of the foot is evident.
Genuine dat feet are associated with pronation or eversion of the forefoot and at times hallux valgus (adduction of the big toe) and prominent medial malleolus.
The children dat feet have generalized relaxation of ligaments and their shoes wear off excessively on die medial surface of die heel. When asked to walk with wet feet, a complete impression of the feet is left on the floor.
Pes cavus There is a high longitudinal arch with excessive plantar curvature of the feet.
It may be an isolated congenital abnormality or may occur as a manifestation or association of Friedreich ataxia, spina bifida, cauda equina lesion, metatarsus varus, diastematomyelia, peroneal muscular atrophy, Hurler syndrome and peripheral neuropathy (Charcot-Marie-Tooth disease).
Toeing-in (pigeon toes) Toeing-in is common in toddlers due to the internal rotation of lower limbs.
The child walks with knees slightly facing each other and toes pointing inwards like a pigeon. The abnormality is self-limiting and usually disappears by the age of 7–8 years.
When toeing-in is marked and persists beyond 10 years of age, surgical correction may be considered. Toe-walking is physiological during the first one to two years of age.
The child can stand on his heels without any difficulty and movements of ankles are normal. The habit disappears as the child learns to walk normally on his heels-to-toes.
Persistent toe walking occurs when tendons-Achill is short and taut with the inability to touch the dorsum of the foot with the shin.
Persistent toe-walking is a recognized feature of cerebral palsy, Duchenne muscular dystrophy, and autism spectrum disorder.
Polydactyly Extra digits may occur in the hand or feet, either on the medial side or preaxial or the lateral side or postaxial.
Musculoskeletal Disorders List
Polydactyly on the ulnar aspects (extra little fingers) of each hand is more common and may occur as an isolated anomaly or in association with chondroectodermal dysplasia (Ellis-van Creveld syndrome), Lawrence-Moon-Biedl syndrome, short-rib polydactyly dwarfism, trisomy-13, and Meckel syndrome.
Syndactyly Fusion or webbing of the toes or fingers may be an isolated anomaly or may be associated with other anomalies, especially the premature fusion of the cranial sutures.
Syndactylism is a recognized feature of Apert syndrome (mitten hand), Carpenter syndrome, Smith-LemliOpitz syndrome, oro-facial-digital syndrome, Poland syndrome, and Pfeiffer syndrome (absence of middle phalanges of all toes).
Trigger thumb or fingers Trigger thumb or flexion of thumb occurs due to idiopathic tightening of the underlying flexor policy long tendon with the inability to fully extend the interphalangeal joint of the thumb.
A palpable nodule may be felt at the base of the thumb. Trigger finger or isolated camptodactyly is uncommon and usually involves the distal interphalangeal joint.
The Extremities
Bony landmarks are used for measuring the length and girth of the upper and lower limbs. Acromion of the scapula, olecranon of the ulna, and lower end of radial condyle are reliable bony landmarks in the upper limbs.
In the lower limbs, the anterior superior iliac spine, upper and lower borders of the patella, and distal edge of the medial malleolus are useful bony landmarks.
Chest circumference is taken at the level of nipples or xiphoid cartilage while abdominal girth is measured at the level of umbilicus.
The waist is measured just above the level of anterior-superior iliac crests. Look for shortening, lengthening, hypertrophy, and atrophy of limbs or their segments.
Hemihypertrophy or hypertrophy of a limb or a localized segment of the limb may occur in cutis marmorated telangiectasia, Beckwith-Wiedemann syndrome, Russell-Silver syndrome, KlippelTrenuanay-Weber syndrome.
Wilms tumor, adrenocortical carcinoma, hepatocellular carcinoma, neurofibromatosis, congenital arterio-venous fistula, lymphangiectasia, and stimulation of epiphyseal growth following osteomyelitis or fracture near an epiphysis.
Shortening of an extremity may occur due to congenitally short femur or tibia, hypoplasia of the femur (infant of a diabetic mother), congenital dislocation of the hip, slipped femoral capital epiphysis, coxa plana, poliomyelitis, hemiplegia, Ollier’s disease and premature arrest of epiphyseal growth due to infection or trauma.
In infantile cortical hyperostosis (Caffey disease) and vitamin A poisoning, there is a diffuse, painful, and localized enlargement of mandibles, clavicles, ribs, scapulae, and some long bones.
Enlargement of ends of long bones or epiphyseal broadening may be seen in children with rickets, hypophosphatasia, chondrodystrophy, Morquio’s disease, and primary hyperparathyroidism.
The ends of long bones may be enlarged and tender and there is associated clubbing of nails in patients with hypertrophic pulmonary osteoarthropathy.
In addition to enlargement of the wrists and ankles, rickets is characterized by frontal bossing, costochondral beading (rachitic rosary), pigeon-shaped (pectus carinatum) or funnel-shaped (pectus excavatum) chest, Harrison’s sulcus, spinal deformities, bowing of legs or knock-knees and coxa vara.
Musculoskeletal Disorders List
The skeletal manifestations of scurvy include subperiosteal hemorrhages in the long bones with marked irritability with pseudoparalysis of extremities with a frog-like posture and scorbutic rosary which is characterized by a bayonet-like angulation at the costochondral junction of ribs due to posterior dislocation of the sternum.
Examine hands and feet for their size, shape, deformities, and length of digits.
Long and thin extremities, hands, feet, fingers, and toes are seen in patients with arachnodactyly (Marfan syndrome), homocystinuria, mucosal neuroma, and Stickler syndrome.
The “thumb sign”, protrusion of the thumb beyond the palm when the hand is fisted, is a characteristic feature of Marfan syndrome.
Small, short, and stubby hands and digits may be seen in patients with Down syndrome, cretinism, Prader-Willi syndrome, Rubinstein-Taybi syndrome (short broad terminal phalanges of thumbs and great toes), and Pfeiffer syndrome (absence of middle phalanges).
Distal hypoplasia of the digits and nails may be seen in fetal phenytoin and alcohol syndrome, chondroectodermal dysplasia, and cleidocranial dysostosis.
Turner syndrome should be considered in every short-stature girl with delayed menarche especially if there is webbing of the neck or cubitus valgus and increased carrying angle of the arm.
Absence or hypoplasia of the radius and thumb may be associated with thrombocytopenia (TAR syndrome), aplastic anemia (Fanconi anemia), and atrial septal defect (Holt-Oram syndrome).
The Bones
It is difficult to examine the deep-seated bones (femur and fibula) as compared to the superficial bones like the tibia and short bones of the hands and feet.
Bone pain is usually continuous (not related to the movement of joint or posture), deep-seated, and penetrating in character, and usually disturbs sleep.
Bone pains may occur without any physical findings in children with leukemia, metastases, and metabolic bone disease.
Exquisitely painful, tense, and slightly warm swelling with erythema and tenderness may occur over one or more long bones due to vaso-occlusive bone involvement in patients with sickle cell anemia.
Localized swelling of long bones may be caused by osteomyelitis, cyst, or tumor. Osteomyelitis is associated with classical signs of inflammation such as redness (rubor), warmth (calor), pain and tenderness (dolor), and swelling (tumor).
Osteochondritis at the distal ends of long bones may occur due to congenital syphilis, and other TORCH infections. Dactylitis is a recognized feature of syphilis, tuberculosis, and choking.
Saber tibiae (anterior angulation or bowing of tibiae) may occur in children with congenital syphilis, neurofibromatosis, fetal malpositioning, and congenital absence of fibula.
Fractures may occur because of trauma to healthy bones or spontaneously in diseased bones (pathological fractures), hr children, trauma may be unrecognized and usually occurs during sports activities or maybe unreported if it is due to child abuse.
The presence of multiple fractures at birth or early in life with deformed thin bones and blue sclerae is suggestive of osteogenesis imperfecta.
When a fracture occurs in a child with multiple cafe-au-lait spots, the possibility of fibrous dysplasia should be excluded.
Due to the presence of soft and pliable bones, children may develop green-stick fractures without break in the continuity of the bone.
Fractures of the clavicle and upper end of the humerus or femur may occur due to difficult extraction of the baby during a breech delivery.
The classical features of closed fracture include pain, tenderness, swelling, deformity of the limb, bony crepitus (abnormal movement with a click at the site of the fracture), and inability to use the limb.
In Colle’s fracture (fracture of the distal end of radius), there is classical “dinner fork deformity” because of dorsal displacement and angulation, shortening, and rotation of the wrist, his open or compound fracture, the soft tissues are damaged, and broken bone ends may protrude out through the damaged skin, his a case of compound fracture, it is important to assess the blood supply, cutaneous sensations, and voluntary movements for any pieces of evidence of nerve injury distal to the site of fracture.
Musculoskeletal Disorders List The Joints
Hypermobility and hyperextensibility of joints are seen his several developmental disorders, like Ehlers-Danlos syndrome, Marfan syndrome, Stickler syndrome, homocystinuria, hyperlysinemia, osteogenesis imperfecta, and primary hyperparathyroidism.
Marked hyperextensibility of fingers and hands may be seen in his children with cartilage-hair hypoplasia, cutis laxa, and fragile-X syndrome.
Joint stiffness and limitation of joint mobility are seen in patients with arthritis, synovitis, osteomyelitis, fasciitis, contractures, dermatomyositis, scleroderma, muscular spasticity, and rigidity.
Several developmental and metabolic disorders like Morquio’s disease, Hurler syndrome, and arthrogryposis congenital multiplex, have generalized stiffness of joints.
Recurrent hemarthrosis of weight-bearing joints (knees and ankles) due to hemophilia may lead to ankylosis, synovial thickening, and atrophy of surrounding muscles (chronic arthropathy).
Subluxation and Dislocation
Developmental dysplasia or congenital dislocation of hip(s) must be ruled out by proper clinical examination his all newborn babies.
Children with hyperextensible joints are more vulnerable to developing dislocation of various joints. Dislocation of multiple joints especially the hip, knee, and elbow is a recognized feature of Larsen syndrome.
Some toddlers are vulnerable to developing recurrent episodes of subluxation of the elbow joint when they are pulled by holding them at their hands.
Traumatic separation of an epiphysis may occur in newborn babies following a traumatic delivery.
It occurs most commonly at the upper humeral epiphysis but may affect any joint causing localized swelling, pain, and limitation of movements.
Arthritis and Arthralgias
The common causes of arthritis and arthralgias in children are listed in.
Arthritis is characterized by local pain, swelling, redness, warmth, restricted and painful movements of joints, deformity, and constitutional and systemic symptoms.
Identify the site (large or small or both), the number of joints involved and whether involvement is symmetrical or asymmetrical in distribution, his superficial joints (especially knee joint), the presence of exudates or pus can be suspected based on pitting edema, fluctuations, and patellar tap.
Neuropathic joint involvement is characterized by recurrent episodes of painless swelling of the foot and any joints with loss of superficial and deep sensations (Charcot’s joints).
In certain children, cracking and creaking sounds may be heard during active and passive movements of certain joints especially metacarpophalangeal and knee joints but it is of no clinical significance.
1. Arthralgias
Reactive or toxic arthritis, chronic active hepatitis, inflammatory bowel disease, toxic shock syndrome, transient synovitis, brucellosis, serum sickness, cystic fibrosis, immunodeficiency disorders, psychogenic pain, and rheumatism
2. Arthritis
Single joint. Pyogenic or septic arthritis, tuberculous arthritis, and acute transient synovitis
Migratory or flitting polyarthritis. Rheumatic fever, gonococcal arthritis, meningococcal arthritis, inflammatory bowel disease, systemic lupus erythematosus, leukemia, or non-Hodgkin lymphoma
Multiple large joints Rheumatic fever, connective tissue disorder (JRA, SLE, Kawasaki disease, polyarteritis nodosa), chikungunya, serum sickness, and Henoch purpura
Multiple small joints of hands and feet Juvenile rheumatoid arthritis, tubercular dactylitis, congenital syphilis, leukemia, sickle cell disease, and psoriatic arthropathy
3. Traumatic arthritis
Hemarthrosis, ruptured cruciate ligament, or torn medial and lateral meniscus of knee joint capsule
4. Miscellaneous causes
Immunodeficiency disorders, disseminated lipogranulomatosis, sarcoidosis, Reiter syndrome, serum sickness, psoriatic arthropathy, sickle cell disease, and pulmonary hypertrophic osteoarthropathy
Arthralgias are characterized by joint pains without any evidence of inflammatory signs.
Musculoskeletal Disorders List Joint Movements
Both active and passive movements of the involved joints should be tested and compared with the normal side. Movements may be limited due to pain, muscle spasms,s and contractures rather than structural damage to the joints.
The movements should be checked after placing the joint in the neutral position. The range of movements can be measured with the help of a transparent goniometer or protractor.
The jaw-jaw movements are tested by opening and closing the mouth, protrusion, and retraction of the jaw and side-to-side movements.
The distance between the incisor teeth on fully opening the mouth is a reliable measure of the severity of ankylosis of temporomandibular joints.
The shoulder The neutral position is with an arm to the side, the elbow flexed to 90 degrees with the forearm pointing forwards.
The scapula should be anchored between the index finger and thumb while testing movements of the shoulder joint.
Test the flexion, extension, abduction, rotation (both in the abduction and neutral position), and elevation of the shoulder. The elbow The neutral position is the forearm in extension.
Test the range of flexion, hyperextension, supination, and pronation. The wrist The neutral position is hand in line with the forearm and palm facing downward.
Test dorsiflexion (extension), palmar flexion, ulnar deviation, and radial deviation. The sacroiliac joints are identified by two dimples on either side over the sacral region.
There are no movements at the sacroiliac joints but their affection can be diagnosed by applying direct pressure over each sacroiliac joint, firm pressure over the sacrum, and inward pressure at both the iliac bones.
The pretzel test is useful to elicit tenderness of sacroiliac joints. The hip The neutral position is the hip in extension with the patella pointing forwards.
The pelvis should be stabilized with one hand while testing the movements of the hip joint.
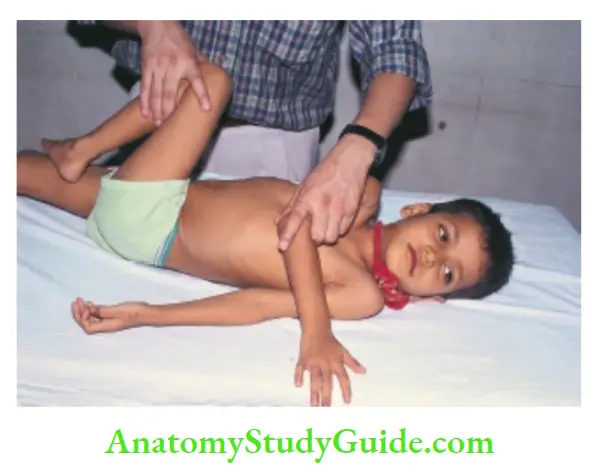
Test hip flexion with knee bent, abduction, adduction, rotation both in extension (prone position) and flexion, and extension while the patient is lying in the lateral position.
Rotation of hip joints is best tested by asking the patient to lie in the prone position with knees in flexion at 90°. Trendelenburg test is done for assessment of the stability of the hip joint.
Observe the patient from behind and ask him to raise one leg.
When the hip joint is normal, the pelvis tilts upwards on the side with the leg raised. When the hip joint is diseased or subluxated, the pelvis sags downwards when the leg is raised.

The knee The neutral position is a complete extension. Test flexion and extension movements. Check for hyperextension of the knee joint (genu recurve).
A patellar tap test is used to check for the presence of effusion in the knee joint. Squeeze all the fluid from the suprapatellar space into the joint with your left hand and tap the patella with the fingers of the right hand.
If the fluid is present, the tire patella will strike the deeper structures and bounce back. The ankle The neutral position is with the outer border of the foot at an angle of 90° with the leg and midway between inversion and eversion.
Test for dorsiflexion and plantar flexion with the knee slightly flexed. Look for the size and tightness of the calf muscles and tendon Achilles.
The foot Test for eversion, inversion, forefoot abduction, adduction, and flexion-extension of metatarsophalangeal and interphalangeal joints.
Look for deformities, like hallux valgus or varus, toeing-in or out, claw toes, hammer toes (fixed flexion of terminal joints), and over-riding of toes.
The spine Examine the child standing and sitting in the erect position. The major landmarks for counting the vertebrae are the spinous process of C7 and the last rib which articulates with the 12th thoracic vertebra.
There is physiological lordosis of cervical and lumbar regions with an S-shaped curve of the thoracolumbar spine.
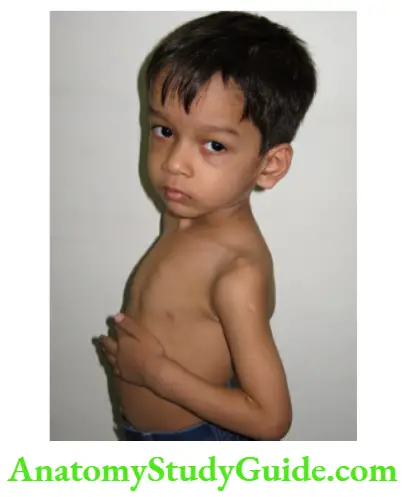
Look for kyphosis (diffuse posterior curvature) and gibbous (localized angular deformity) due to Pott’s disease (spinal tuberculosis) and vertebral disk prolapse.
Lateral curvature is termed as scoliosis and it is always associated with rotation of the bodies of vertebrae.
When scoliosis is caused by inequality of leg length, it disappears in a sitting position.
Examine the cervical and thoracolumbar spine for various movements, like flexion, extension, rotation on both sides and lateral bending towards the right and left.
All movements occur at the cervical spine while the thoracic spine permits mainly rotation and the lumbar spine can flex,
extend and bend laterally.
Assess expansion of the chest which may be reduced due to ankylosing spondylitis even when there is no underlying lung disease.
Pain limitation of straight leg raising (SLR) and sensory loss over the sacral region is suggestive of a prolapsed intervertebral disk.
When the limit of SLR is reached, passive dorsiflexion of the foot further stretches the sciatic nerve causing severe pain.
Musculoskeletal Disorders List The Muscles
Look for muscle tone, power, localized atrophy or hypertrophy, and whether involvement is symmetrical or asymmetrical.
Enlargement or localized hypertrophy of muscles may be seen in patients with Duchenne muscular dystrophy, Becker muscular dystrophy, myotonia congenita, Schwartz-Jampel syndrome, chronic spinal muscular atrophy type 3, and amyloidosis.
Rarely, generalized muscular hypertrophy is observed in patients with hypothyroidism (Kocher-DebreSemelaigne syndrome) and glycogen storage disease associated with acid maltase deficiency.
Generalized hypotonia and floppiness of muscles can occur in children due to a variety of causes. Refer to Chapter 14 for testing muscle strength.
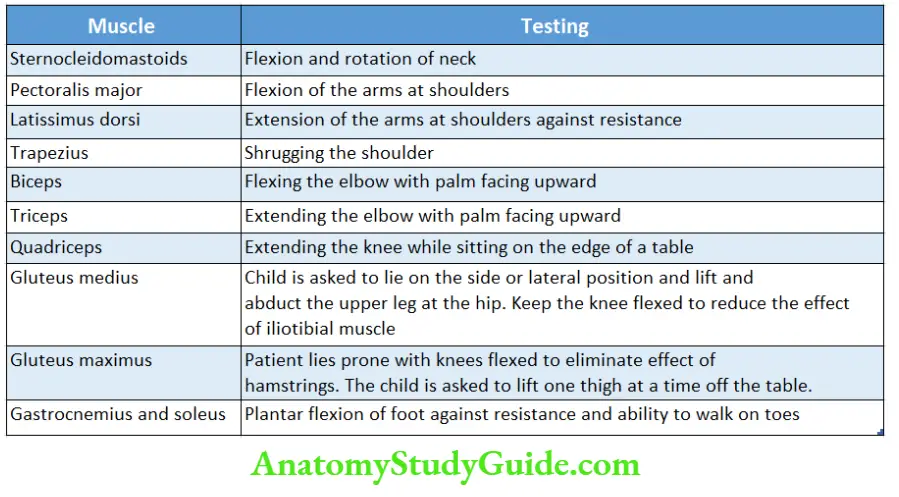
The action of major muscles of the body and various maneuvers for their testing are summarized.
Muscle weakness may be minimal or severe, symmetrical or asymmetrical, and limited to proximal (dermatomyositis) or distal (peripheral neuritis) muscles.
Common causes of muscular hypotonia
Cerebral conditions:
Atonic cerebral palsy, cerebellar tumors, and gliomas
Spinal causes:
Spinal cord transection, and transverse myelitis
Anterior horn cell disorders:
Werdnig-Hoffmann disease, poliomyelitis, Guillain-Barre syndrome, and benign congenital hypotonia
Muscle disorders:
Congenital myopathies Hereditary connective tissue disorders: Ehlers-Danlos syndrome, and Marfan syndrome
Metabolic disorders:
Glycogen storage disease, Zellweger cerebrohepatorenal syndrome, hypothyroidism, myopathic carnitine deficiency, periodic paralysis, myasthenia gravis, primary hypoparathyroidism, and Tay Sachs disease
Musculoskeletal Disorders List Miscellaneous causes:
Protein-energy malnutrition, rickets, Down syndrome, Prader-Willi syndrome, and idiopathic hypercalcemia
Body aches due to muscle pains are common during viral infections and due to fatigue in preschool children which are often labeled as “growing pains”.
Severe myalgias may occur during leptospirosis, dengue fever, Rocky Mountain spotted fever, toxic shock syndrome, and plague.
Staphylococcal infection may produce life-threatening suppurative fasciitis and myositis.
Fibromyalgia in adolescents is characterized by chronic and persistent musculoskeletal aches and pains in at least 3 or more sites with fatigue and morning stiffness.
Musculoskeletal Disorders List The Gait
Gait should be assessed with legs and feet fully exposed and without shoes or sandals. Ask the child to walk away from you, turn around at a given point, and then walk back towards you.
It is best to watch the gait of the child when he is not aware that Iris’s gait is being watched.
The abnormality of gait due to disorders of the central nervous system.
Many children start walking on their toes but persistent toe walking (equine gait) is usually suggestive of spastic diplegia, spinal dysraphism, intraspinal and filum terminal tumors, pseudohypertrophic muscular dystrophy, shortening of tendon-Achilles and an autism spectrum disorder.
In-toeing and out-toeing gait due to torsional variations may occur but often resolve spontaneously.
Medial or internal torsion of the tibia is common during early infancy and is the most common cause of pigeon-toed or toeing-in gait.
When the infant lies supine with knees extended, the lateral malleolus is normally 10–15 degrees posterior to the medial malleolus.
Medial tibial torsion is diagnosed, if the lateral malleolus is at the same plane or anterior to the medial malleolus.
Transient synovitis of the hip joint (“observation hip”) occurs in children below 10 years of age and is an important cause of fever of acute onset with pain in the hip or groin (sometimes referred to as the knee) and limp.
The lower extremity is held in flexion, external rotation, and adduction. Internal rotation and abduction at the hip joint are restricted.
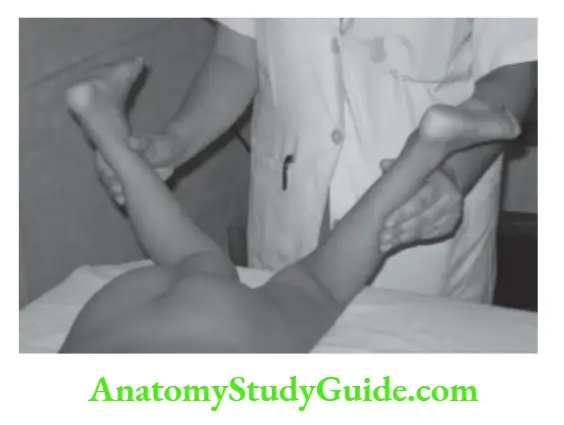
The limitation in abduction is best demonstrated by asking the patient to lie in a supine position with knees flexed and feet resting flat on the examination table.
When the child is asked to let the knees fall apart while keeping the feet together, the limited abduction on the involved side is evident.
Internal rotation of the hip is tested by asking the child to lie in a prone position with knees flexed.
Several clinical conditions should be considered in the differential diagnosis of transient synovitis, septic arthritis, Legg-Calves-Perthes disease (avascular necrosis of femoral capital epiphysis), slipped femoral epiphysis, osteomyelitis, tuberculosis, osteoid osteoma, and rheumatoid arthritis.
Sudden alterations of gait and limping may occur from a variety of painful conditions involving muscles, joints, tendons, and bones. Identify whether limping is painless or associated with pain.
Causes of Limping in Children
Trauma:
- Sprain of the ankle, a splinter in the foot, traumatic periostitis, contusions, tight-fitting shoes, etc.
Osteochondrosis:
- Involvement of femoral capital epiphysis, tibial tubercle, patella, metatarsal, and tarsal bones
Arthritis and osteomyelitis:
- Transient synovitis, slipped femoral epiphysis, arthritis, bursitis, and osteomyelitis involving joints of lower limbs
Neoplastic diseases:
- Leukemia, sarcoma, and metastasis from neuroblastoma
Neurological disorders:
- Peripheral neuropathy, muscle weakness or paralysis, and spinal cord tumor.
Miscellaneous conditions:
- Leg length inequalities, tight tendon-Achilles, inguinal or iliac lymphadenitis, muscular dystrophy, polymyositis, and conversion disorder or hysteria.
Leave a Reply