Examination Of Newborn Baby
Table of Contents
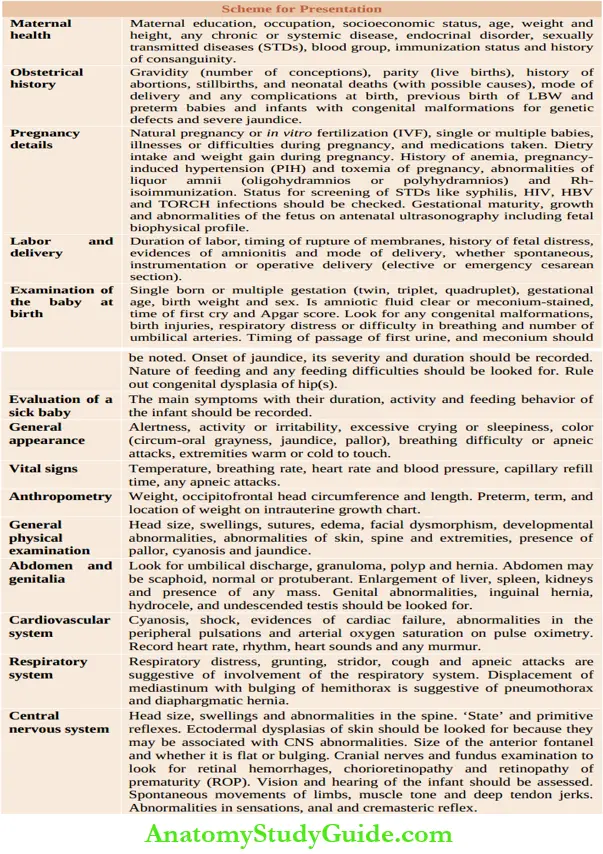
History
It must be remembered that a newborn baby is around 9 months old at birth unless prematurely born. Neonatology is not a system-limited speciality, it deals with all the systems of a newborn baby (up to 28 days of life).
A detailed history regarding diseases suffered by the mother and drugs taken during pregnancy should be elicited
Basic Indicators:
Ask whether it was a natural pregnancy or in-Vitro fertilization (IVF). The date of birth, gestational age and birth weight should be recorded. The gestational age is calculated from the first day of the last menstrual period.The education, occupation, and economic status of parents should be enquired.
Read and Learn More Pediatric Clinical Methods Notes
The age of the mother is important because young mothers (<18 years) are likely to produce low birth weight babies and have an increased risk of delivery hazards while elderly mothers (>35 years) are at an increased risk to have babies with congenital malformations and chromosomal disorders.
Review of maternal and perinatal history:
- Family history: History of hereditary, metabolic, chromosomal, and developmental disorders.
- Maternal history: Duration of marriage, age, blood group, chronic illnesses, like diabetes mellitus, hypertension, renal disease, cardiac disease, lung disease, endocrinal disorder, systemic lupus erythematosus, bleeding disorder, CNS or psychological disorder, sexually transmitted disease including herpes and HIV, TORCH screening, etc.
- Previous obstetrical history: Gravidity, parity, abortions, stillbirths, neonatal deaths (with possible causes), prematurity, LBW or growth retarded babies, obstructed labor, cesarean section, congenital malformations and blood transfusion.
- Current pregnancy: Natural pregnancy or IVF, gestational age, weight gain, excessive vomiting, bleeding, polyhydramnios/oligohydramnios, ultrasound examination, diagnostic and therapeutic procedures done during pregnancy, pregnancy-induced hypertension, pre-eclampsia, infections (UTI, diarrhea/dysentery, malaria and tuberculosis), surgery, drugs of abuse and medications (hormones, glucocorticoids, tocolytic agents and antibiotics).
- Labor and delivery: Fetal distress, presentation, mode of delivery, duration of rupture of membranes, duration of labor, amnionitis, amniotic fluid (volume, clear or meconium-stained), anesthesia/analgesia, Apgar score, resuscitation required and examination of the placenta.
Previous Obstetrical History:
The gravidity (number of all conceptions including abortions, stillbirths, etc. with possible causes) and parity (number of live births) should be recorded.
The interval between successive pregnancies and their outcome should be enquired. History of recurrent abortions and stillbirths is suggestive of incompetent cervical os, diabetes mellitus, syphilis, and Rli-isoimmunization.
Gestational maturity, birth weight, congenital malformations; obstructed labor, and mode of delivery of previous babies should be noted. The neonatal course, unusual manifestations and outcome of previous babies should be ascertained.
Prepregnancy Health Status:
Maternal systemic disorders, like heart disease, hypertension, bronchial asthma, chronic renal failure, tuberculosis and anemia, are associated with increased risk of abortions, stillbirths, intrauterine growth retardation, premature births and increased perinatal mortality rate.
History of maternal endocrinal disorders, such as diabetes mellitus, thyrotoxicosis, myxedema and hyperparathyroidism should be asked. Systemic lupus erythematosus may be associated with complete heart block in the fetus.
Chronic undernutrition of the mother during childhood and adolescence leads to short stature (<145 cm) and low adult weight (<40 kg) which are associated with increased risk of low birth weight babies.
History of sexually transmitted diseases including herpes, syphilis, and HIV should be checked. The Rhesus blood group should be identified because of the potential risk of Rh-isoimmunization if an Rh-negative mother is carrying an Rh-positive fetus. Tetanus toxoid and rubella vaccination status should be assessed.
Course of Pregnancy:
The adequacy and quality of antenatal care received should be checked. The first trimester of pregnancy is characterized by embryogenesis. Diseases and drugs taken during this phase of pregnancy are potentially teratogenic.
Ask for history suggestive of maternal rubella, cytomegalovirus, and toxoplasmosis which are manifested by fever, skin rash, and posterior cervical lymphadenopathy. Ask history of petechiae or thrombocytopenia during pregnancy.
The abnormalities reported on antenatal ultrasound scans should be recorded, hi a malformed or sick baby, a detailed history of medications taken during pregnancy should be recorded because they may produce unusual clinical manifestations in the newborn baby
Maternal ABO and rhesus blood type, indirect Coombs’ titer (if mother is Rh-negative), hemogram, VDRL and whenever indicated, carrier status for hepatitis B virus and HIV and TORCH screening should be checked. The diagnostic and therapeutic procedures undertaken during pregnancy should be recorded.
Dietary intake especially during the second half of pregnancy is crucial to ensure the optimal growth of the fetus. During an uncomplicated pregnancy, most Indian mothers gain between 6 and 10 kg body weight.
History of pregnancy-induced hypertension with or without urinary abnormalities associated with placental dysfunction, intrauterine growth retardation, perinatal hypoxia, and birth asphyxia.
Ask for a history of bleeding during pregnancy whether due to abruptio placentae or placenta previa. The quantity of amniotic fluid should be checked. Oligohydramnios is associated with placental dysfunction, postmaturity, renal agenesis and obstructive uropathy.
Polyhydramnios (amniotic fluid >2 liters) is associated with maternal diabetes mellitus, syphilis,pre-eclamptic toxemia and fetal congenital malformations, such as open neural tube defects, anencephaly, ectopia vesicae, esophageal atresia, duodenal/jejimal atresia, twins and hydrops fetalis.
Meconmm-stained liquor amnii in a vertex-presenting baby is indicative of fetal distress or fetal diarrhea due to listeriosis.
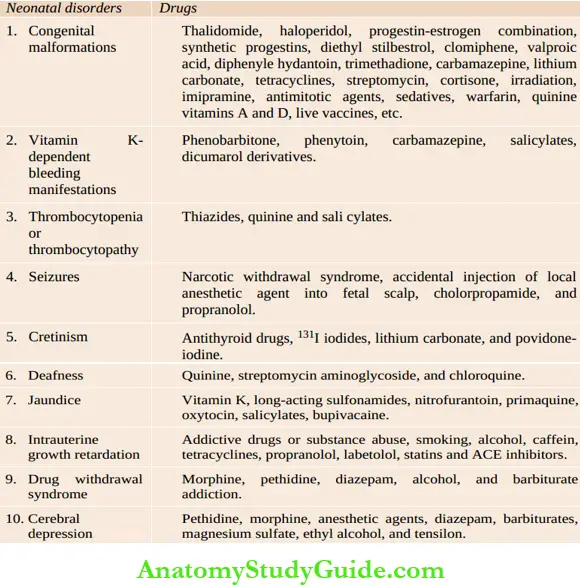
Common neonatal disorders and malformations due to maternal medications during pregnancy:
Labor and Delivery:
History of amnionitis (periportal fever, abdominal tenderness), prolonged rupture of membranes (>24 hours), and unclean or too many vaginal examinations are recognized markers of intrauterine bacterial pneumonia.
Prolonged labor (>18 hr first stage, and >6 hr second stage) and difficult delivery are associated with an increased risk of birth asphyxia and birth trauma.
Determine whether the baby was delivered vaginally following spontaneous labor or after induction/augmentation with oxytocin.
Ask for history of instrumentation or operative delivery (elective or emergency cesarean section). Check whether any pieces of evidence of fetal distress were present during labor.
Evidences of cephalopelvic disproportion, cord around the neck or cord prolapse, etc. should be noted. Analgesics and anesthetics used during labor can adversely affect the fetus.
Neonatal History:
Ask whether baby cried immediately after birth or was asphyxiated. Details regarding Apgar score should be checked in case of institutionilized delivery. If 1-minute Apgar score is low, it should be checked at 5 minutes and 10 minutes.
Determine whether baby was kept in a nursery or roomed in with the mother. General activity and history of feeding during first week should be asked. Ascertain the passage of first urine (upper limit is 48 hours) and stools (upper limit is 24 hours) after birth.
Occasional vomiting on the first day of life is common and is of no significance. Ask for history of severe jaundice, seizures and feeding difficulties during the neonatal period.
History of Present Illness:
Ask and assess the chief complaints as told by the mother or attendant in chronological order. Newborn babies manifest nonspecific symptoms due to a variety of disorders.
They have a limited capacity to produce symptoms. Refusal of feeds, lethargy, and inactivity are a common denominator due to several neonatal disorders. The nature of predisposing or associated conditions is more crucial to make a diagnosis in a newborn baby.
Assess the predisposing factors (maturity, birth weight, birth asphyxia, prolonged rupture of membranes, etc.), age of onset, and evolution of symptoms. The common neonatal conditions include birth asphyxia, respiratory distress syndrome, jaundice, septicemia, bleeding manifestations, inborn errors of metabolism, and congenital malformations.
Preterm babies are vulnerable to develop a variety of disorders including hyaline membrane disease, metabolic disorders, hypothermia, infections, necrotizing enterocolitis, intraventricular hemorrhage, patent ductus arteriosus, retinopathy of prematurity, etc.
Neonates are known to manifest a large number of minor developmental peculiarities and physiological problems which need to be identified to offer reassurance and advice to the mother.
On the other hand, when a neonate is genuinely sick, he cannot be managed on an ambulatory basis and must be admitted in a hospital providing level II neonatal care.
Family History:
Ask for the family history of developmental and metabolic disorder. History of neonatal deaths in sibship or family should be asked. History of a similar disorder in a previous sibling should be ascertained. History of consanguinity among parents should be asked.
Immunizations:
Check whether BCG, Hepatitis B, and oral polio vaccine have been taken or not. The maternal status of tetanus toxoid vaccination should be enquired.
Physical Examination
Examination should be conducted in a warm and comfortable room with the baby completely undressed and placed on a flat surface at a height convenient for the physician.
A good source of light should be available and the examiner’s hands should be clean and warm. The detailed examination is conducted routinely at birth, within 24 hours or next day, and at the time of discharge.
The key timings for examination of newborn babies are shown in The baby should be examined in detail whenever there is any evidence of abnormality or illness. The newborn baby is best examined one hour after the feed.
Before the feed, the baby may be crying or cranky due to hunger and when a baby is examined soon after the feed, it may lead to vomiting and aspiration.
Key timings for examination of newborn babies:
- At birth
- Daily check in the lying-in ward
- Examination at the time of discharge
- Examination of sick babies in the NICU
- Healthy babies for immunizations, follow-up of NICU babies or unwell babies in the ambulatory clinic
Examination at Birth:
The aim of examination of the baby at birth is to ensure and assess that lungs have expanded and that air passages are not obstructed, and to make an early diagnosis of life-threatening congenital malformations and birth injuries.
Apgar Scoring System:
Despite its limitations, the Apgar scoring system is coventionally used to assess the condition of the baby at birth. The most crucial items in the system are breathing and heart rate because muscle tone, response to reflex stimulus and color are dependent upon cardiorespiratory status.
Time taken by the baby to produce the first cry after birth should be noted. Ask whether the amniotic fluid was clear or meconium-stained.
Screening For Congenital Malformations
The maternal history should be screened for any ingestion of teratogenic and goiterogenic drugs, irradiation and viral infections during the first trimester of pregnancy.
The existence of polyhydramnios in the mother should alert the pediatrician to the possibility of obstruction in the upper intestinal tract. About 25 percent cases of esophageal atresia and 75 percent cases of obstruction of the duodenum and upper jejunum are associated with polyhydramnios.
In fact, one out of every seven cases of polyhydramnios are associated with upper intestinal obstruction. Oligohydramnios, on the other hand, maybe associated with bilateral renal agenesis, obstructive uropathy, and Potter facies.
Family history of any developmental anomalies should be enquired. A quick but complete examination should be conducted with the following scheme in mind.
Birth weight and gestational age:
The incidence of anomalies in preterm babies is twice in frequency as compared to term appropriate-for-gestational age babies. In small-for-dates (especially hypoplastic) babies, the incidence of anomalies is 10 to 20 times higher.
A thorough examination and observation of these babies is essential for early diagnosis of anomalies.
Single umbilical artery and palmar crease:
The cut end of the cord should be inspected for a number of the vessels. A single umbilical artery, which has an incidence of around 0.8 percent, is associated with internal congenital malformations in 15 to 20 percent of cases.
The commonly associated malformations include esophageal atresia, imperforate anus, and genitourinary anomalies.
A single palmar crease should alert one to make a thorough search for additional anomalies
Apgar scoring system:
Hypoplasia of the depressor anguli oris muscle:
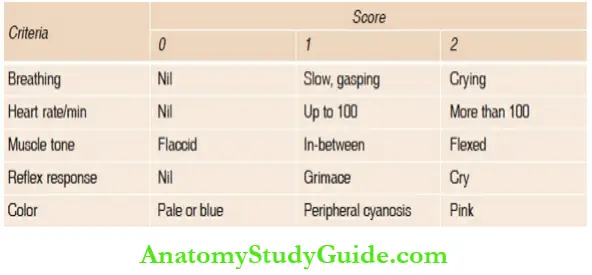
The asymmetric crying facies due to congenital hypoplasia of the depressor anguli oris muscle (DAOM) should be looked for because these infants have additional associated anomalies in over 20 percent of cases.
During crying, angles of the mouth and mandible are pulled down with flattening of the nasolabial fold on the normal side due to the unopposed action of DAOM.
Cardiovascular anomalies and congenital dislocation of hips are most commonly associated.
Orifice counting and their patency:
The anomalies are concentrated around orifices. Look for a cleft palate and ectopic or closed anus. The patency of esophagus should be checked by passing a stiff rubber catheter into the stomach in the situations listed below.
Some pediatricians recommend this procedure routinely in all babies:
- Small-for-dates baby
- Single umbilical artery
- Polyhydramnios
- Maternal diabetes mellitus
- Frothiness and drooling of saliva
When the catheter has reached the stomach, the gastric contents should be aspirated. If gastric aspirate exceeds 20 ml, it is strongly suggestive of high intestinal obstruction.
Evidence of respiratory difficulty:
The surgical causes of respiratory distress should be excluded and an urgent X-ray chest should be asked for.
Midline lesions on the back and front:
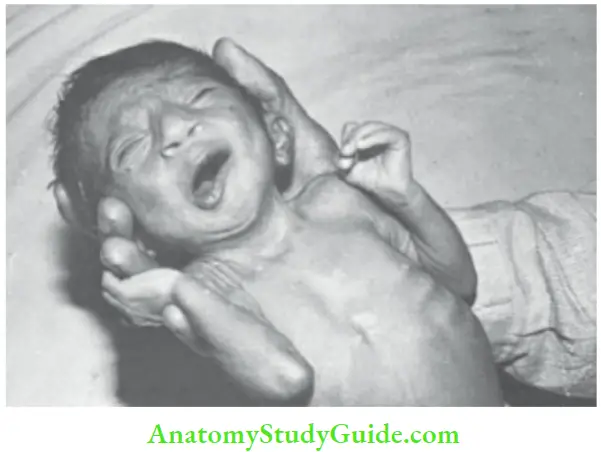
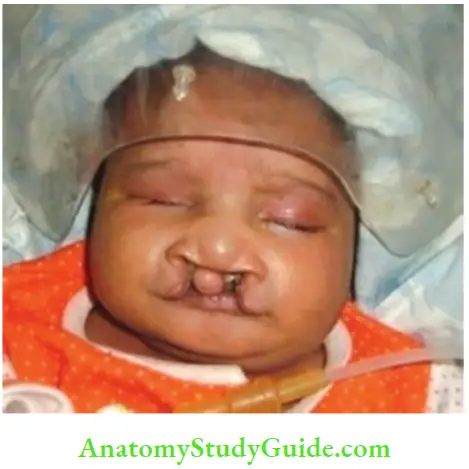
Cleft lip, cleft palate, spina bifida, meningomyelocele, pilonidal sinus, ambiguous genitalia, hypospadias, exomphalos, etc. should be looked for.
Cleft palate may occur as an isolated defect or may occur in association with ventricular septal defect and several syndromes, like trisomy–13, trisomy – 18, mandibulofacial dysostosis, Wolf-Hirschhorn syndrome, velocardiofacial syndrome and Pierre-Robin syndrome.
Submucous cleft of the plate can be missed unless carefully looked for a thin and transparent defect in the palate. A bifid uvula also indicates a submucous cleft of the palate which requires surgery.
Routine systemic examination:
Abdomen should be palpated for any massess and heart examined for its position and murmurs. ‘Dextrocardia’ due to pushing of the heart, in association with respiratory difficulty, is suggestive of left-sided pneumothorax and diaphragmatic hernia.
Look for musculoskeletal anomalies and evidences of congenital amputations due to amniotic bands.
First-day Examination:
The main purpose of the first-day examination is to record anthropometric measurements, to make sure that no anomalies have been overlooked, to enquire about feeding behavior, and to look for onset of jaundice.
History of frothiness, choking, and vomiting after feeds should be asked for and evaluated. Enquiry should be made regarding the time of passage of the first meconium (up to 24 hours) and urine (up to 48 hours).
Some infants may cry due to the unpleasant sensation of a full bladder, become quiet or dazed while passing urine, and resume crying after evacuation due to the discomfort of wet diaper.
This is normal pattern and should not be mistaken with bladder neck obstruction
1. Vital signs:
The vital signs in healthy term babies denote a median heart rate of 140/min, respiratory rate 40/min, blood pressure 60/40 nun Hg, and core body temperature of 36.5°C to 37.0°C.
It is easy and convenient to remember that in a healthy term infant, respiratory and heart rates are twice while blood pressure is one-half of an healthy adult. A persistent heart rate of more than 200 per minute in a quiet baby is suggestive of paroxysmal atrial tachycardia while a heart rate consistently below 80 beats per minute suggests a complete heart block.
Bradycardia in newborn babies is a recognized feature of asphyxia, hypothermia, hypothyroidism, raised intracranial tension, hypertension, and hyperkalemia. Instead of a febrile response, hypothermia is more commonly associated with septicemia, especially in preterm babies.
Fever may occur in term babies having Grampositive infections or meningitis. Skin temperature can be reliably assessed by touch alone with some experience. In a healthy baby, trick should feel warm to touch and soles and feet should be reasonably warm and pink.
When the trick is warm but soles and feet are pale and cold, it suggests that baby is in cold stress and his ambient temperature should be raised. Breathing should be recorded in a quiet baby at least one to two hours after a feed.
Blood pressure may be recorded with the flush method or with the help of a Doppler, hi infants with adequate tissue perfusion, the baby is pink and warm without any mottling of skin, the difference between central and peripheral skin temperature is less than 1.5°C, and capillary refill time over the upper chest is less than 2 sec and urine output is adequate (At least 1.0 ml/kg/hr).
2. General behavior: Look for color, respiration, movements of limbs and their posture, general alertness, and activity of the child. Excessive sleepiness or irritability is indicative of CNS disorder.
Persistent unconsolable high-pitched cry is suggestive of meningitis. Routine neurological examination or even elicitation of Moro response is unnecessary if the baby is active and feeding normally. The onset of jaundice within 24 hours of age is indicative of a serious disorder.
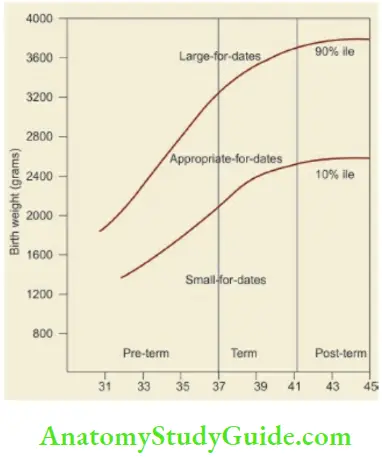
Anthropometry:
Birth weight should be recorded at birth as soon as the baby is stable and preferably during the first 24 hours of life. The birth weight and gestation of the child is plotted on the intrauterine growth chart to identify whether the baby is appropriate-for-dates, small-for-dates, or large-for-dates.
Occipitofrontal head circumference, chest circumference at nipples, and crown heel length on an infantometer are recorded. The head circumference should preferably be taken after 24 hours of birth when caput succedaneum and over-riding of sutures would have disappeared, a term baby, head circumference is around 34–35 cm with a crown-heel length of 48–50 cm.
Ponderal index (weight in grams/(length in cm)3 × 100) should be calculated. The PI is usually less than 2 in asymmetric small-for-dates babies compared to ponderal index of more than 2 in term AGA infant and symmetric SFD babies.
Gestational Assessment:
Assess gestation by physical and neurological examination, if menstrual history is unavailable or uncertain. As gestation proceeds, the baby grows and matures physically and neurologically.
The anthropometric measurements, such as weight, length, head, and chest circumference are unreliable parameters of maturity because they may be adversely affected by intrauterine growth retardation.
Head circumference and length are relatively spared in a baby with intrauterine malnutrition as compared to weight and chest circumference.
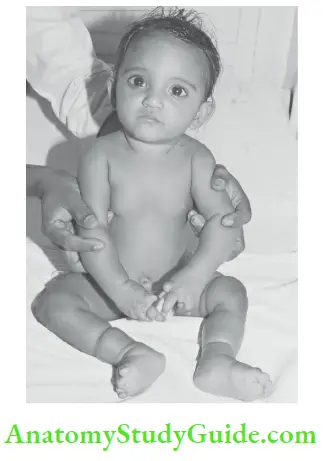
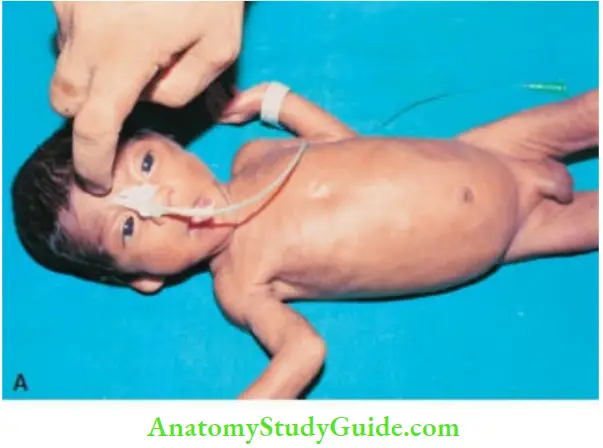
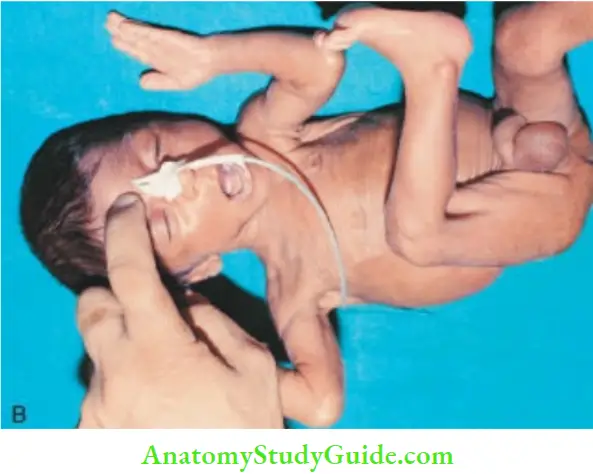
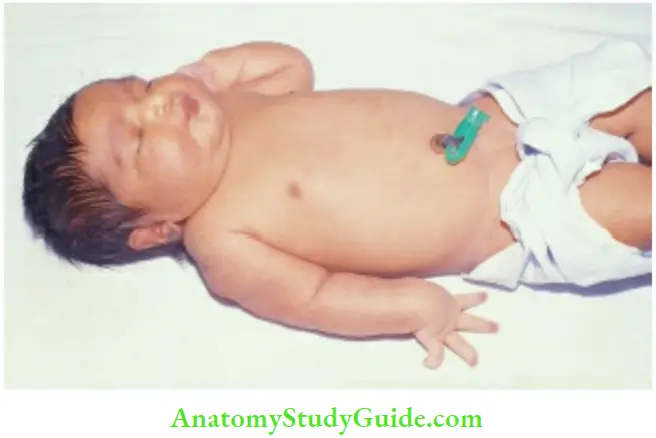
Grouping of Babies into Preterm and Term:
In a baby with unknown gestation, assessment of the maturity of the baby on the basis ofphysical characteristics alone is fair This simple approach helps in deciding whether the baby should be roomed-in wily reliable.
The the mother or kept in the special care nursery. But does not permit classification of the baby on the basis of birth weight and gestational age.
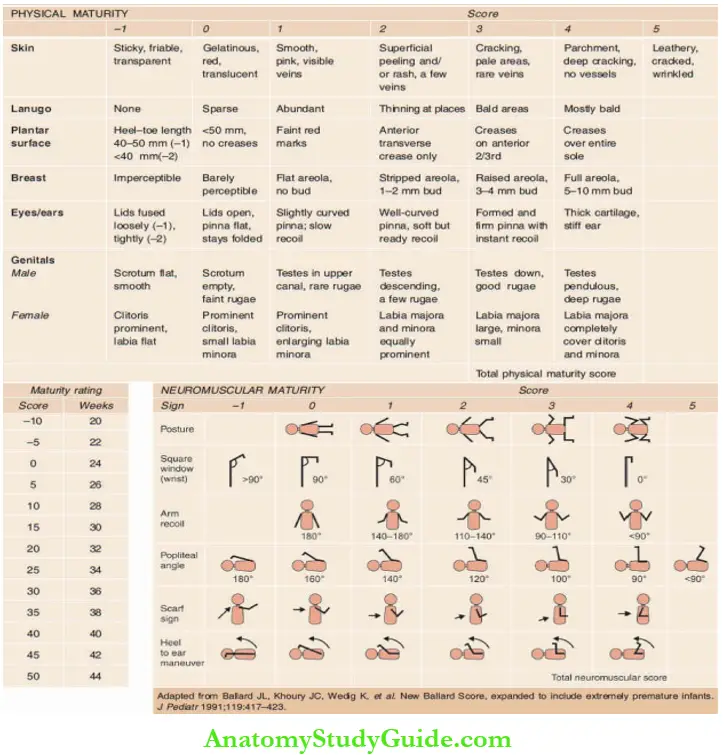
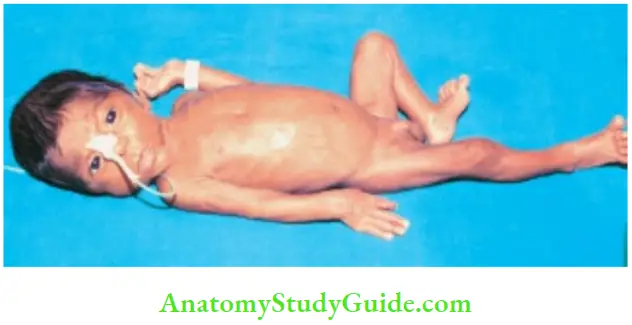
The preterm baby (less than 37 weeks) shows most of the following characteristics:
- Anthropometry: In preterm babies, birth weight is usually less than 2500 g (term small-for dates babies may also be low birth weight), crown heel length <47 cm and head circumference of <33 cm and head size is usually more than 3 cm bigger than chest circumference.
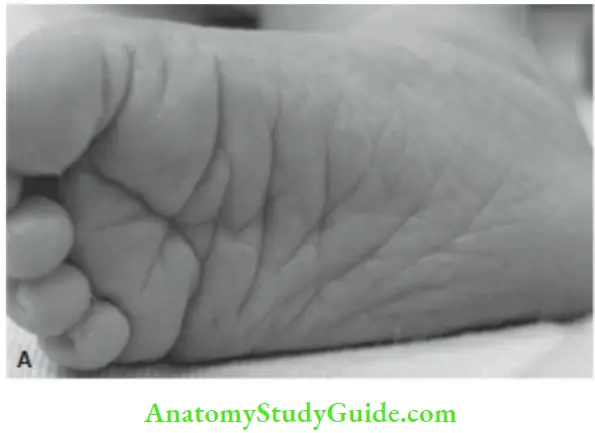
- Sole creases: In a preterm baby, there is a single deep crease over anterior one-third of the sole or no deep crease. The sole may be full of superficial creases
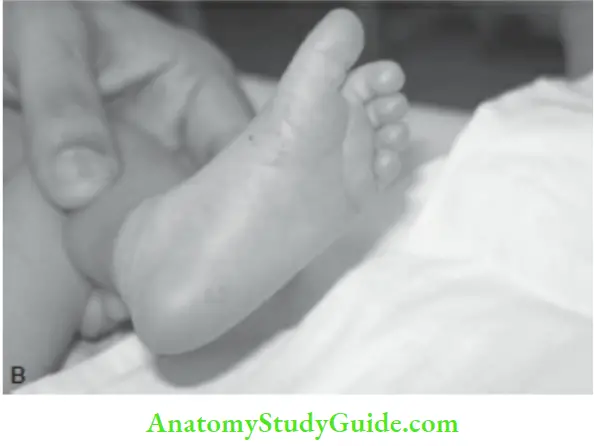
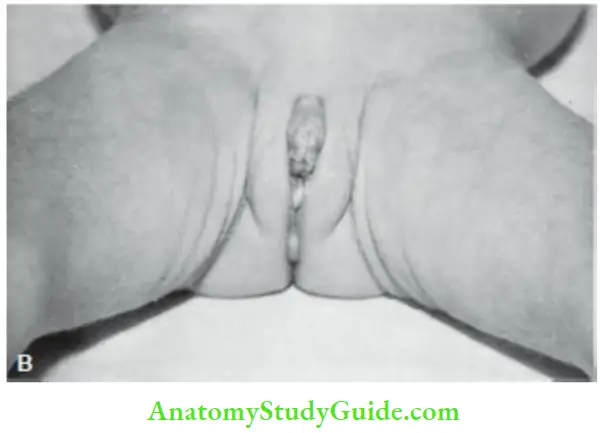
- Genitals: In male babies, both the testes are at the external ring or above and the scrotum is small with scanty rugosities. In girls, labia majora are widely separated with labia minora fully exposed and the clitoris is hypertrophied
- Breast nodule: Breast nodule is less than 5 mm and nipple is small or absent. In small-fordates babies, breast tissue may be deficient or absent even when they are gestationally fully mature.
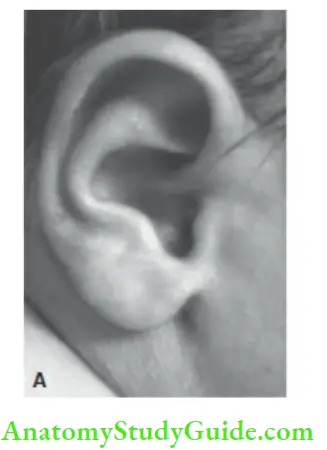
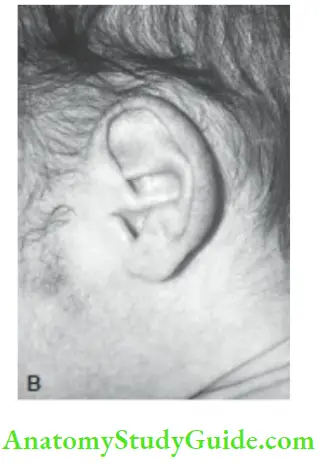
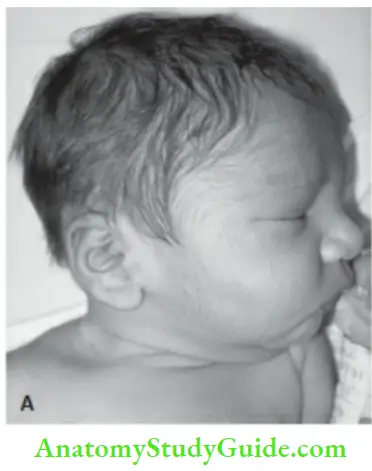
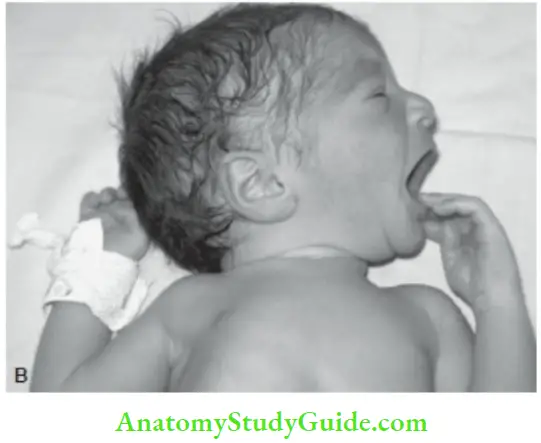
- Ear cartilage: Cartilage is deficient and even absent at places and on folding the external ear, the recoil may be poor.
- Hair: Brownish-black fuzzy or woolly in appearance with no difficulty in identifying the individual hair fibers
Depending upon the degree of immaturity, the preterm babies may have shiny and oily plethoric skin, plenty of lanugo, and edema. Neurologically, they are less alert, hypotonic, and various neonatal reflexes may be absent or incomplete.
Precise Estimation of Gestational Age:
The physical characteristics outlined above are very reliable to differentiate between preterm and term babies but are of limited value to assess the precise gestation of babies of less than 36 weeks of maturity.
On the other hand, neurological parameters are more reliable for precise delineation of gestational maturity of preterm babies, while they are of limited predictive value in relatively mature babies.
The neurological assessment is based on four fundamental observations:


1. Muscle tone: The muscle tone progressively increases in utero as maturity proceeds. The tone in the newborn baby is assessed by three parameters.
- Posture or attitude
- Passive tone is evaluated by assessing popliteal angle and scarf sign and Majora are widely separated and labia minora exposed
- Active tone is assessed by traction response and recoil.
2. Joint mobility: The degree of flexion at ankle and wrist (square-window) is limited in preterm babies because of the relatively greater stiffness of joints in early gestation As term approaches, the joints become more flexible and relaxed to allow for easy molding during delivery.
3. Automatic reflexes: They appear at specific ages of gestational maturity. Moro reflex appears as early as 28 – 30 weeks but lacks a complete adduction phase till 38 weeks of gestation.
Pupillary response to light is present after 30 weeks and the infant may turn his head towards diffuse light during 32 – 36 weeks of gestation. Grasp response makes its appearance around 30 weeks but a strong grasp is elicitable after 36 weeks.
Neck flexors are able to contract in response to traction around 33 weeks of maturity. Rooting and coordinated sucking efforts are present by 34 weeks of gestation.
4. Fundus examination: The disappearance of tire anterior vascular capsule of the lens has been used to assess the gestational age of the infant with a gestation of less than 28 weeks.
After 34 weeks of maturity, anterior capsular vessels are almost completely atrophied with graded changes in babies between 28 and 34 weeks of gestation.
Ophthalmic examination is, however, technically cumbersome in newborn babies due to physiological photophobia andlack of cooperation
In view of a rather wide overlap in the time of appearance and persistence of various physical and neurological criteria, many workers have evolved scoring systems by using the combined maturity score of physical and neurological criteria for the assessment of gestation.
Outlines one such simplified scoring system for the assessment of gestation. The assessment should be made on babies with normal Moro response, because neurologically damaged and severely ill babies would be grossly under-scored on neurological assessment.
Babies with severe intrauterine growth retardation may also be under-scored to some extent due to its adverse effects on the development of breast tissue and muscle tone.
On the basis of combined physical and neurological scores, the expected gestational age of the baby can be read from a predictive error of ± 2 weeks.
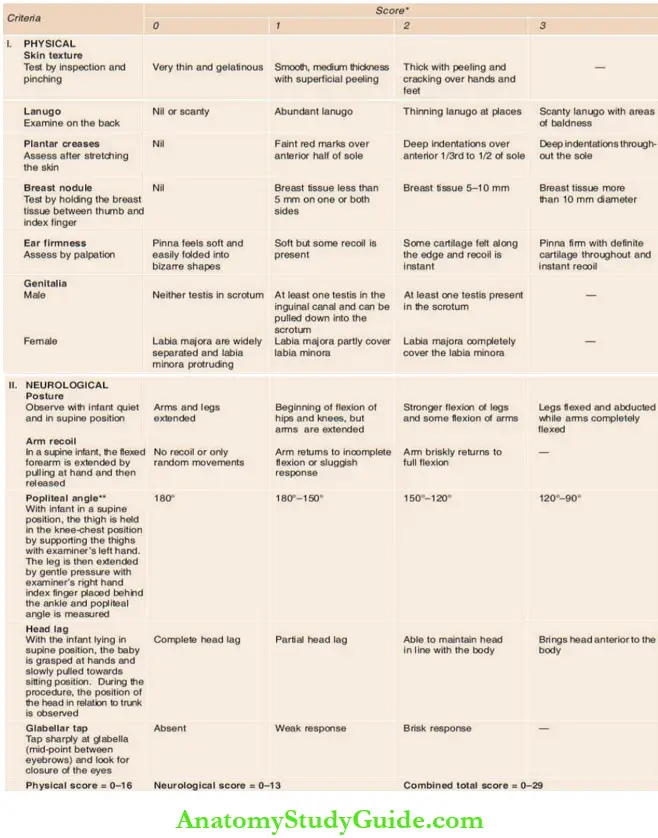
Scoring system for assessment of gestational age:
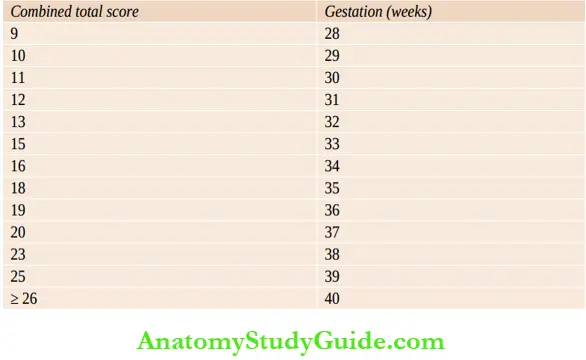
A number of other scoring systems based on physical and neuromotor evaluation are used for gestational assessment. A revised Ballard score is widely used in clinical practice and is credited to have greater accuracy for assessment of gestational age in extremely premature infants
Relationship between combined total score with gestational age:
Systemic Examination
Minor Developmental Peculiarities:
Examine the skin for toxic erythema or urticaria neonatorum, milia (yellow-white papules on the nose), stork bites or salmon patches (capillary ectasia over the upper eyelids, glabella and nape of the neck), capillary hemangiomata, and mongolian blue spots over the butocks and sacral region .
Subconjrmctival hemorrhage over the outer canthus of the eye, Epstein pearls (epithelial inclusion cysts as white papules one on either side of median raphe of hard palpate), and sucking callosity as a rounded cornified plaque at the center of the upper lip are commonly seen in healthy normal infants.
Some infants may be born with incisor teeth which may have to be removed, if they are loose or cause feeding difficulty. Genuine tongue-tie is uncommon and is characterized by tight fibrous frenulum, notch at the tip of the tongue, and inability to protrude the tongue beyond the margins of the lips.
Tongue-tie seldom interferes with sucking or cause delay in the onset of speech. Mastitis neonatorum is characterized by enlargement of breasts in full-term infants of both sexes on third or fourth day of life due to the effect of transplacentally transferred maternal hormones.
Withdrawal type of vaginal bleeding on third or fourth day may be seen in female infants and is of no pathological significance. Hymenal tags and slimy mucoid vaginal discharge are extremely common, hi male infants, foreskin of penis cannot be retracted due to physiological phimosis.
1. Head:
Examine for caput succedaneum, cephalhematoma, forceps marks, encephalo-cele and widely separated or closed sutures. Caput succedaneum is a localized edema of the scalp over the presenting part of the head following vaginal delivery.
It pits on pressure, crosses the suture lines, is non-fluctuant, and disappears within 1 – 2 days. Cephalhematoma is a subperiosteal collection of blood that appears a few hours after birth as a large cystic swelling limited by suture lines.
It tends to resolve slowly over a period of a few days or weeks and may leave a calcified edge. It may aggravate the severity of physiological jaundice. Rarely, a large hematoma may occur under the occipitofrontalis aponeurosis (subgaleal hematoma) leading to periorbital and periauricular edema, anemia, jaundice and hemorrhagic shock.
Unlike subperiosteal or cephalhematoma, subeponeurotic hemorrhage (subgaleal hematoma) is not limited by suture lines.
New Ballard scoring system for assessment of gestation of extremely premature babies:


Anterior fontanel varies in size between 2 and 3 cm while posterior fontanel is small (admits finger tip) and usually closes by 2 months of age. In preterm, small-for-dates, and hydrocephalic babies, head circumference is more than 3 cm bigger than the chest.
The size, shape, and symmetry of the skull may be altered by craniosynostosis. Cradle cap over the scalp is common due to crusting of sebum. Craniotabes or softening of skull bones which can be pressed like a table tennis ball is suggestive of prematurity, hydrocephalis, congenital rickets, congenital syphilis, and osteogenesis imperfecta. It should be looked for some distance away from the sutures.
2. Face:
Yellow-white papules on the nose due to retention of sebum (milia) are present in most term babies and disappear spontaneously. Typical acne-like lesions, may be seen over the forehead, nose, and cheeks at birth in term babies due to transplacental passage of maternal androgens to the fetus.
Salmon patches or stork marks or nevus flammeus are pinkish-gray sparse capillary hemangiomata commonly located at nasal bridge, upper eyelids, and nape of the neck. They invariably disappear after a few months.
Look for abnormal facies or dysmorphism by paying due attention to size, shape, and position of ears, distance between two eyes and their alignment, size of the oral opening and tongue, shape of the nose and its bridge, shape of lips and size of philtrum and chin size in profile.
Recheck for cleft palate. The characteristic constellation of micrognathia, retrognathia, glossoptosis, and cleft palate of Pierre Robin syndrome should be looked for. Eyes should be examined for conjunctivitis, subconjunctival hemorrhage, corneal haziness, cataract, white reflex, and glaucoma.
The watering (epiphora) or persistent wetness of one or both eyes occurs due to obstructed nasolacrimal duct. Hairy pinna is characteristically seen in infants of diabetic mothers.

Look for preauricular skin tag anterior to the auricle which may be associated with renal anomalies. The preauricular pit or sinus is uncommon and is of no significance.
3. Neck:
Short neck with webbing is a recognized feature of Turner syndrome. “Sternomastoid tumor” is a hard swelling over the middle of anterior border of either sternomastoid muscle due to calcified hematoma which may cause torticollis. It usually resolves by passive movements and physiotherapy of the neck.
Look for goiter, cyst or branchial fistula, and lymphangioma. Thyroglossal duct cyst or sinus is located in the midline of the neck while branchial cleft cysts are located at the anterior border of the sternocleidomastoid muscle.
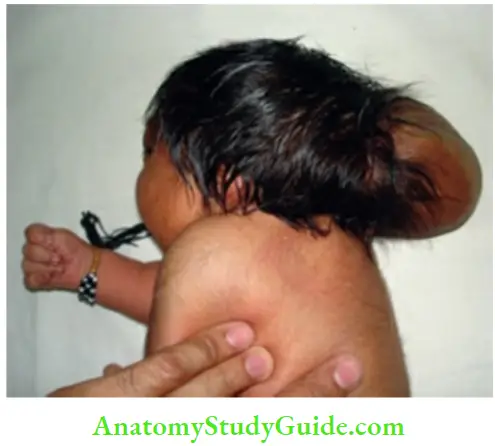
Cystic hygroma is a compressible, spongy transilluminant mass, which may invade the thorax causing respiratory distress. Intertrigo due to fungal infection is common in the neck.
4. Skin:
Examine for jaundice, cyanosis, petechiae, lanugo hair, birth marks, hemangiomata, rashes and evidences of dysmaturity. Toxic erythema or urticaria neonatorum is common in term babies during first week of life.
Erythematous skin rash with central pallor appears on the face on second or third day of life and spreads to the trunk and extremities in next 24 hours.
It disappears spontaneously after 2–3 days without any treatment. The rash should be differentiated from pyoderma, transient pustular melanosis and congenital syphilis.
Congenital syphilis is characterized by maculopapular exfoliative or vesiculobullous skin eruptions involving palms and soles. Perioral ulceration (rhagades) and perianal condylomata should be looked for. Look for evidence of congenital ichthyosis.
Transient neonatal pustular melanosis is rare and is characterized by superficial fragile pustules mainly over the chin, neck, forehead, back and buttocks.
Pustules are formed due to subcorneal collection of neutrophils with a few eosinophils. They are asymptomatic but may persist up to 3 months.
There is cephalopedal progression of yellow discoloration of skin as the level of serum bilirubin rises. The clinical jaundice manifests on the face at a serum bilirubin level of 5 mg/dl.
Tire yellow staining of trunk indicates serum bilirubin of 10–15 mg/dl, but when soles and palms are yellow-stained, the serum bilirubin is likely to be more than 15 mg/dl.
5. Spine:
Spina bifida, meningocele, meningomyelocele, pilonidal sinus and tuft of hair should be looked for. Sacral dimple or pit should not be confused with pilonidal sinus.
6. Extremities:
Club feet and minor varus or valgus deformities should be looked for. Talipes equinovarus is characterized by plantar flexion (equinus) and inversion (varus) of the ankle and adduction of forefoot.
In talipes calcaneovalgus deformity, the ankle is dorsiflexed and foot is abducted and everted. It should be differentiated from congenital vertical talus (rocker-bottom foot), in which foot is fixed in plantar flexion with a reversed arch.
Look for anomalies of digits (oligodactyly, polydactyly, syndactyly), genu recurvatum, and arthrogryposis multiplex congenita. Bowed legs are normal during early infancy. Look for any fracture of clavicle, humerus, and femur.
Abdomen and Genitalia:
Umbilical cord dries and falls between 5 and 10 days after birth. The separation of cord is delayed in preterm babies, infants with cell-mediated immunodeficiency disorder, and due to local infection.
Look for any discharge from the umbilicus, whether it is watery (urine), purulent, or serosanguinous. Umbilical granuloma is characterized by pale irregular granulation tissue while polyp is pedunculated with a bright-red glistening appearance.
Polyp may have a small central opening with watery or fecal discharge due to communication with a urachal cyst or omphalomesenteric duct.
Abdominal examination in a newborn baby is often unsatisfactory unless the baby is quiet or asleep and while taking a feed, otherwise the abdomen becomes tense during palpation.
To relax abdominal wall, the infant is supported with a soft pillow in a semi-reclining position, or a supine infant is slightly lifted off the cot by holding at both the ankles. Liver edge is normally felt 2 cm below the costal margin.
Spleen tip and occasionally lower poles of kidneys, especially tire right, may be palpable by an experienced neonatologist. However, if spleen and kidneys are easily palpable, it is abnormal.
Bimanual palpation for kidneys is attempted with one hand by placing the fingers over the loin while the thumb searches for tire kidney with gentle, steadily increasing pressure subcostal in a posterior and cephalad direction.
Obstructive uropathy is characterized by three abdominal masses (two kidneys and distended bladder) and large over hanging wrinkled skin of the abdominal wall.
Genitals should be examined for any anatomical abnormalities, undescended testes, and hydrocele. In a term infant, the scrotum is large, pendulous, darkly pigmented and testes are easily palpable due to absence of a cremasteric reflex at birth.
Inguinal hernia is more common on the right side because processus vaginalis closes earlier on the left side. As opposed to umbilical hernia, inguinal hernia must be operated within 4 – 6 weeks of diagnosis because of high incidence of incarceration during infancy.
Hydrocele should be looked for but its excision should be delayed till 6 months of age because most of them get resorbed spontaneously. Look for the opening of urethra to exclude epispadias and hypospadias.
Ambiguous genitals with “Salt-losing syndrome” (vomiting, diarrhea, dehydration, and shock) is suggestive of congenital adrenal hyperplasia.

Cardiovascular System:
Developmental cardiac defects are present in about 1.0% of newborn babies and about two-thirds of these manifest in the neonatal period. Auscultate for any cardiac murmur or abnormalities of heart sounds.
It is desirable to use a stethoscope with small-sized chestpiece for auscultation of newborn babies. There is physiological tachycardia and ‘tic tic’ rhythm due to equality of systolic and diastolic phases. Transient cardiac murmur may be heard in 2 to 8% of normal babies during first 48 hours of life.
The significant or pathological cardiac murmur is usually loud, grade III or more, and may be associated with an ejection click and abnormalities of the second heart sound. The presence of a murmur is not essential for the diagnosis of heart disease.
In a severely symptomatic newborn baby, the presence of a soft and insignificant murmur or absence of murmur usually signifies a serious underlying heart disease.
Infact, 20 percent of infants dying of heart disease in the neonatal period may not have a murmur. In infants with leftto-right shunt, murmur may appear after several days or weeks when pulmonary vascular resistance falls and shunt becomes significant.
Therefore, a murmur in the neonatal period does not necessarily indicate the presence of cardiac malformation while absence of a murmur does not rule out congenital heart disease.
Look for evidences of cyanosis and congestive cardiac failure. The cyanosis due to right-toleft shunt becomes worse when the baby cries. Marked cyanosis in the absence of any respiratory difficulty is highly suggestive of cyanotic heart disease.
When arterial oxygen saturation (SaO2) is less than 85% in a stable baby without any respiratory distress, it is suggestive of congenital heart disease which should be ruled out by 2D electrocardiography with color flow Doppler. Clubbing may appear after 3 – 6 weeks in cyanotic babies.
Tachypnea, tachycardia, progressive hepatomegaly, edema (or sudden weight gain), and cardiomegaly are recognized features of cardiac failure in a newborn baby, jugular venous pressure is unreliable and difficult to evaluate in a newborn baby due to short neck. The common causes of cardiac failure on the basis of age at onset are listed in Table
Respiratory System:
In the absence of respiratory difficulty or any other complaints, such as cough or feeding problem, the routine examination of the chest is unnecessary and often non-contributory.
Cough is an uncommon symptom in newborn babies and may occur due to meconium aspiration syndrome and pneumonia especially due to Chlamydia trachomatis.
Look for tachypnea, dyspnea, grunting and retractions of chest. Recessions occur readily especially in preterm babies due to the softness of ribs.
Stridor may occur due to upper respiratory tract obstruction. Over-inflated barrel-shaped chest because of obstructive emphysema is seen in infants with meconium aspiration syndrome.
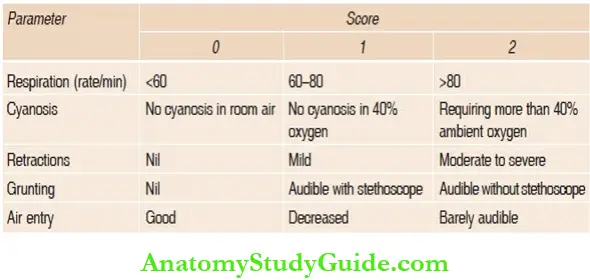
A number of scoring systems are available to clinically assess the severity of respiratory distress.
Common causes of heart failure on the basis of age at onset:
- Fetal causes: Anemia. Erythroblastosis (Rh-isoimmunization), fetomaternal transfusion, parvovirus B19 infection (hydrops fetalis), and hypoplastic anemia. Arrhythmias. Supraventricular tachycardia, ventricular tachycardia, and complete heart block.
- First 48 hours: Premature infants. Fluid overload, patent ductus arteriosus, bronchopulmonary dysplasia, and hypertension.
- Full-term infants: Asphyxial cardiomyopathy, systemic AV fistula, viral myocarditis, polycythemia, sepsis, hypoglycemia, hypocalcemia, complete heart block, congenital thyrotoxicosis, and fluid overload.
- First week of life: Critical aortic/pulmonary stenosis, hypoplastic left heart syndrome, transposition of great vessels with intact ventricular septum, obstructed total anomalous pulmonary venous connection, coarctation of the aorta, and Ebstein anomaly.
- Second week of life: Large ventriculi septal defect, atrioventricular septal defect, large PDA, unobstructed total anomalous pulmonary venous drainage, and truncus arteriosus.
- 1–2 months of life: Large L-R shunts, transposition and malposition complexes, anomalous left coronary artery from the pulmonary artery, and aorta-pulmonary window.
Decreased movements of chest on one side are seen in association with pneumothorax, diaphragmatic hernia, pleural effusion, and hypoplasia of lung. Diaphragmatic hernia is characterized by flat or scaphoid abdomen, reduced chest movements, and/or bowel sounds usually in the left hemithorax with displacement of the mediastinmn and heart to the opposite side.
The auscultation of the chest is not always rewarding in newborn babies due to cross conduction of adventitious sounds, hi infants with respiratory distress due to pulmonary causes, the underlying cause is suspected on the basis of associated or predisposing conditions rather than any specific clinical signs.
All seriously sick neonates, a skiagram of the chest is mandatory irrespective of clinical symptoms and signs referable to the respiratory system.
Scoring system for assessment of severity of respiratory distress:
Central Nervous System:
Brain in newborn babies functions mostly at a subcortical level because babies born without cerebral hemispheres are indistinguishable in behavior from normal babies and cerebral motor defects do not generally manifest in the neonatal period.
Therefore, the neurological examination has a limited localizing value for cerebral lesions in the neonatal period. The lack of cooperation and proper ‘state’ of the baby poses practical difficulties. Therefore, emphasis is laid on thorough observation which is likely to be most informative and least disturbing to the infant.
The neurological examination is best performed about two hours after the last feed when baby is in ‘state’ 3 or 4 but normal babies remain in these ‘states’ only for 10 to 15 percent of the time.
The examination should never be attempted immediately after the feed because some babies may vomit if they are handled or disturbed. Most babies fall asleep after a feed.
Purpose of Neurological Examination:
Routine neurological examination in a healthy term baby is unnecessary. The information regarding activity, behavior and feeding pattern of the baby as reported by the mother, absence of any abnormalities of the skull and spine, and symmetry of spontaneous movements of limbs on the two sides are enough to rule out any significant neurological abnormality.
There is no need to elicit Moro reflex on these apparently normal babies, hi general, a detailed neonatal neurological examination is usually done for the following purposes.
- Diagnosis of acute neurological illness:
- The prognosis for future neurological development following perinatal hazards and neurological illness.
- Assessment of gestational age.
The common symptoms of neurological illness in a newborn baby include irritability, frank or subtle seizurs, high-pitched crying, drowsiness, inability to suck (despite gestational maturity of >34 weeks), bulging anterior fontanel, lack of movements of the limb(s) and seizures. Hypoxic ischemic encephalopathy and metabolic disorders are common causes of seizures in a newborn
baby.
Age at onset of seizures provides useful clue to the underlying cause of seizures
Brazelton’s ‘States’ of wakefulness in a neonate:
- State 1. → Deep sleep with regular respirations, no movements.
- State 2. → Light sleep with eyes closed, occasional movements of eyelids, lips, fingers, etc., and irregular respirations (REM sleep).
- State 3. → Eyes open with no gross movements (quiet wakefulness).
- State 4.→ Eyes open with gross body movements.
- State 5. → Eyes open or closed and crying.
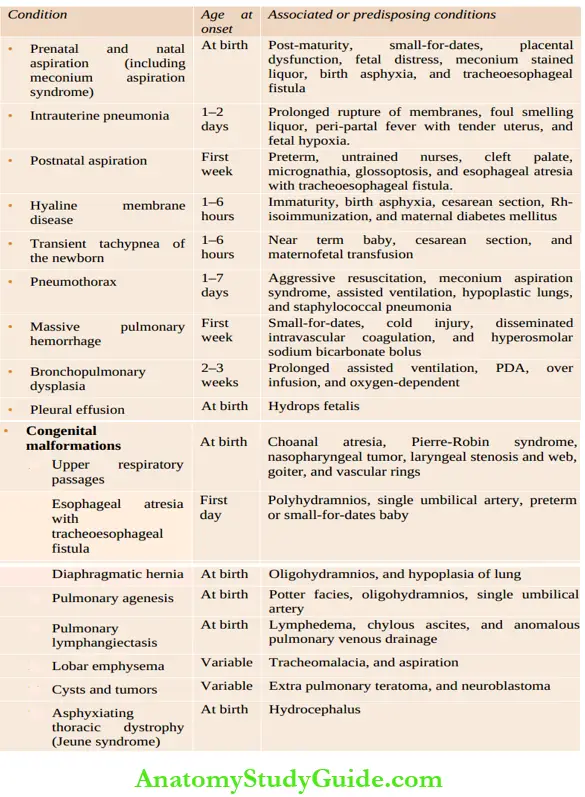
Common causes of respiratory distress due to pulmonary disorders:
Age at onset of convulsions:
- First day: Hypoxic-ischemic encephalopathy, cerebral contusion, ‘first day’ hypocalcemia, pyridoxine dependency, and accidental injection of local anesthetic into the fetal scalp.
- Between 1 and 3 days: Intracranial hemorrhage, hypoglycemia, narcotic withdrawal, and inborn error of metabolism
- 4th to 7th day: Tetany, meningitis, TORCH infections, developmental malformations, kernicterus, and benign neonatal seizures
- 1 – 4 weeks: Late-onset hypocalcemia, sepsis, progressive hydrocephalus, herpes encephalitis, inborn error of metabolism, cerebral dysgenesis, and epileptic syndromes.
General Observations:
The ‘containers’ of the central nervous system (skull and spine) should be carefully examined to exclude any traumatic or developmental defects.
Skin should be examined for any ectodermal dysplasia which may be associated with CNS abnormality. ‘State’ of the baby and cry should be recorded. High-pitched shrill cry may signify the presence of cerebral irritability.
1. Skull:
The occipitofrontal circumference should be measured after 24 hours of birth when molding and over-riding of sutures have disappeared. Abnormalities of shape, symmetry, and swellings (cephalhematoma and encephalocele) should be looked for .
The ‘Setting sun’ sign may be normally seen in some neonates. If persistent and exaggerated, it suggests hydrocephalus and kernicterus. It is suggestive of raised intracranial tension with compression of orbital plate or brainstem irritation.
During the first 48 hours, skull bones overlap each other due to molding. A wide range of normal variations in the size of anterior fontanel and sutural separation makes their interpretation difficult.
Hydrocephalus should be suspected only when the head circumference is more than the 95th percentile for the gestation or postnatal age. The sagittal suture may be separated up to 0.50 to 0.75 cm during the first fortnight due to the rapid growth of the brain outstripping the bony growth of the calvarium.
Generally, squamoparietal sutures are not separated except in hydrocephalus but may be open in preterm and small-for-dates babies without hydrocephalus. A ridge at metopic suture (midline on forehead) is normal while sutural ridges at other places suggest craniosynostosis.
Auscultation of skull may reveal a bruit in infants with arteriovenous fistula or angiomatous malformation.
Transillumination of the skull should be done as a routine in all cases. The torch should be fitted with a circular tightly fitting rubber foam ring over its front end to ensure close contact of the torch to the baby’s scalp. Cold-light transilluminator can be used for assessment of transillumination of the skull.
Normally, the halo of light around the rim of the illuminator extends up to one centimeter in the occipital region and about two centimeters in the frontal region in term babies.
Excessive transilhrmination is seen whenever the abnormal collection of fluid at any intracranial site is within one centimeter of the inner table of skull. In large collections of fluid and in infants with hydrocephaly and porencephaly, the whole skull may glow with light.
2. Spine:
Exclude spina bifida and associated anomalies, tuft of hair, dermal sinus, fracture of the spine, etc.
3. Cranial nerves:
Examination of cranial nerves has limited usefulness in a newborn baby.
For examination of second and eighth cranial nerves, refer below to the section on special senses. For examination of third, fourth and sixth cranial nerves, the baby should be held on the arm by
Supporting the head in your palm in a diffuse light when he is likely to open his eyes spontaneously. Ptosis and inability to close the eye should be looked for. Doll’s eye movements should be tested to detect any ocular palsy.
Nystagmoid movements may be seen normally. For the fifth and seventh cranial nerves, tap the nation. The eyes close. This evaluates movements of the upper face . The rooting reflex gives information regarding the lower half of the face.
Asymmetry of the face on crying is a useful sign of facial palsy. In partial facial palsy or congenital absence of depressor anguli oris muscle, the mandible alone may deviate or is pulled down on the normal side as the baby cries.
Corneal reflex is absent when the trigeminal nerve is affected. Look for nasal regurgitation during feeds and elicit the gag reflex for testing the ninth and tenth cranial nerves. Asymmetry of tongue is seen due to the involvement of the twelfth nerve.
Fasciculations of tongue are characteristically seen in infants with Werdnig-Hoffmann disease.

4. Fundus:
The examination of the fundus is of limited value in a newborn baby. Satisfactory pupillary dilatation can be achieved with a mixture of phenylephrine 0.1% and tropicamide or cyclopentolate 0.2% eye drops. The disk is normally pale and devoid of foveal reflex during the first three months of life.
Papilledema as a sign of raised intracranial tension is rare because rising tension is easily buffered by sutural diastasis. Retinal hemorrhages are commonly encountered but are of no clinical significance.
Large subhyaloid hemorrhages are seen in intracranial bleeding in the subarachnoid and subdural spaces. Choroido-retinopathy is suggestive of certain intrauterine infections. Indirect ophthalmoscopy is recommended for screening of retinopathy of prematurity (ROP).
Special Senses:
They can be tested only during ‘states’ 3 to 4, otherwise the interpretation is unreliable.
1. Vision:
The visual fixation and attention must be assessed with due patience and care because these are the only functions at birth which indicate the integrity of cerebral hemispheres. The visual acuity in a term newborn baby is around 6/45 and it gradually matures to an adult level of 6/6 by the age of 6–7 years.
- The vision can be tested as follows:
- The baby responds to strong light by blinking.
- Head turns towards diffuse light after 32 weeks of gestation.
- The baby shows attention or follows moving red ball after 34 weeks of gestation.
- Opticokinetic nystagmus is present.
2. Pupils:
Their size and reaction to light should be recorded. Pupils do not react to light in babies less than 29–31 weeks of gestation, during raised intracranial tension and posterior fossa compression.
Pupils may be dilated and fixed in infants with optic atrophy or retinal detachment; while in cortical blindness, pupillary responses are preserved.
In a newborn baby, the dilated pupils give poor prediction regarding the side or site of intracranial hemorrhage. Examine pupils with the help of an ophthalmoscope light.
The presence of the “Red reflex” rules out any serious abnormalities in the anterior and posterior chambers of the eye. The presence of a “White pupil” or leukocoria is suggestive of cataract, retinoblastoma, persistent pupillary membrane, vitreous opacity, and retrolental fibroplasia due to ROP.
3. Hearing:
Clinical examination for hearing in tire newborn is not reliable. The baby is watched for tire following responses, after giving a sound stimulus of a bell or 60 db vocal sound: Look for startle response, blinking of eyes, sudden change in tire activity of tire baby with greater alertness, and change in tire heart rate and breathing pattern or rate.
The positive response, both for visual attention and hearing, signifies a lack of any generalized neurological disturbance. A negative response, however, is of little significance because many variables may affect this.
There is a need to do repeated assessments to evaluate the integrity of vision and hearing. A formal hearing test (BERA, OAE) should be done at the tire age of 3 months.
Motor Functions:
1. Spontaneous movements: The range and symmetry of spontaneous movements should be observed. Watch and record in detail any tremors (jitteriness) and convulsions. Subtle seizures are common in preterm babies and may consist of jerking of the eyes, blinking, staring look, sucking or chewing movements. The seizures are usually multifocal dome, tonic, or myoclonic in type.
2. Muscle tone:
The normal term neonate is rather hypertonic while preterm babies are usually hypotonic. Increase or decrease in tone must be significant before it is regarded as abnormal. Differences in muscle tone between the two sides of the body have greater localizing value.
The baby’s head must be kept in the midline, while assessing the muscle tone, otherwise tonic neck posture may influence muscle tone unequally on the two sides. Look for popliteal angle and heel to ear maneuver in tire lower limbs and scarf sign in tire upper limbs, for assessment of muscle tone.
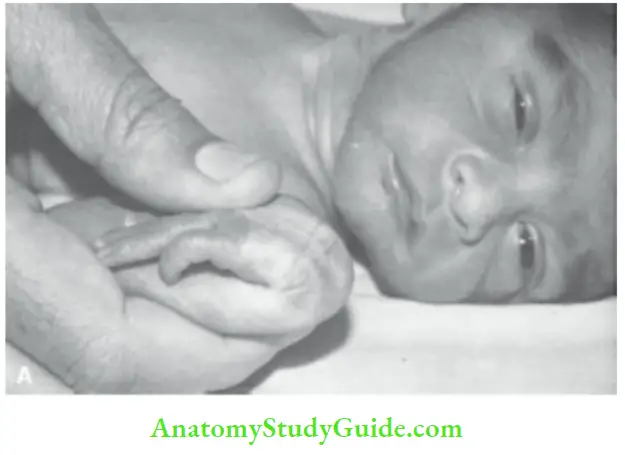
Avulsion of brachial nerve roots may occur during difficult breech extraction or shoulder impaction. In Erb’s palsy (C5, C6), the affected arm hangs limply and kept adducted and internally rotated with elbow extended.
When lower cervical roots are affected (Klumpke’s palsy), there is wrist drop due to flaccid paralysis of hand with absent palmar grasp. The presence of miosis, ptosis, and anhidrosis (Horner’s syndrome) though uncommon is suggestive of associated damage to the cervical sympathetic chain of tire first thoracic root.
3. Tendon jerks: The deep tendon jerks are rather variable in neonates and are generally brisk. The index or middle finger can be used to elicit deep tendon jerks in newborn babies. Knee jerk in tire newborn is normally followed by contraction of the adductors of both hips (crossed adductor spread).
Ankle clonus may elicit up to eight jerks in normal babies, but if 10 to 12 uninterrupted jerks are obtained, it is abnormal. The tendon jerks are of poor diagnostic utility except in infants with peripheral nerve and spinal cord injuries.
Primitive Reflexes:
The newborn babies have a large number of primitive or automatic reflexes. It is time consuming and tiring both for tire baby and the physician to elicit all of these automatic reflexes. The following reflexes are useful for clinical purposes and one should observe whether tire response is sluggish, normal or exaggerated and symmetric or asymmetric.
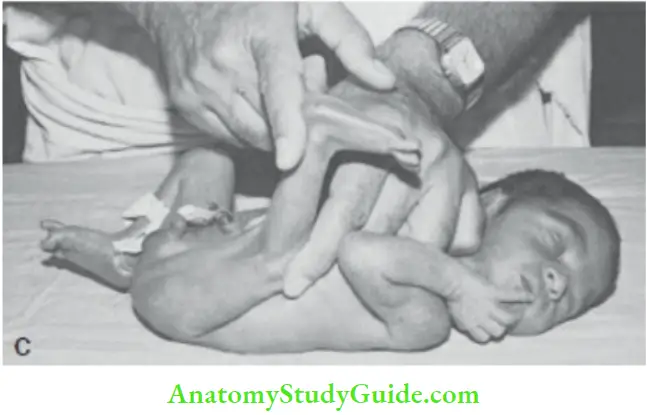
1. Moro reflex:
Moo reflex or startle response is tire most useful. The baby should be held supine over tire right hand and arm. The flexed head is suddenly allowed to drop by about 30°. A positive response consists of rapid abduction and extension of upper limbs and opening of hands followed by slower adduction and flexion or embrace equivalent the infant may cry.
The response can also be elicited by pulling a supine infant by both hands (as in traction response). When angulation occurs between tire head and trunk, tire hands are sharply released to cause sudden extension of the neck.
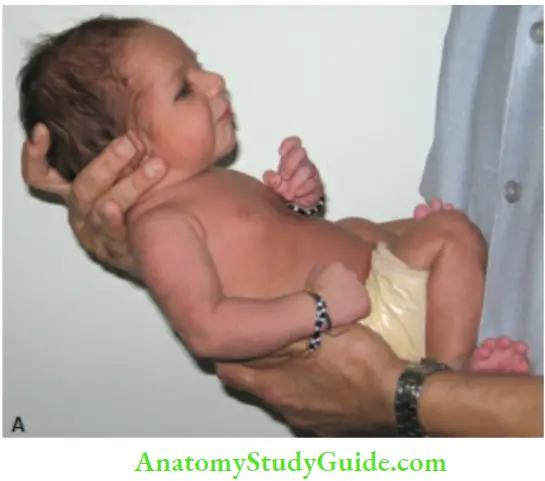
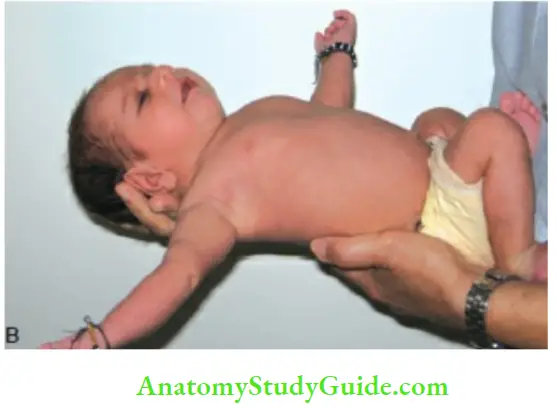
The response may be depressed or absent in infants with cerebral depression. Exaggerated or jumpy response may be obtained in cases of cerebral irritability.
The Moro reflex may be incomplete in babies, with a gestation of less than 35 weeks. Asymmetric Moro response may suggest brachial palsy and fracture of the clavicle or humerus.
In babies with kernicterus, the Moro response is often characteristic. The sudden extension of arms is not followed by a flexion component but is often accompanied by downward rolling of eyeballs (‘setting sun’ sign), lid lag, and a peculiar grin.
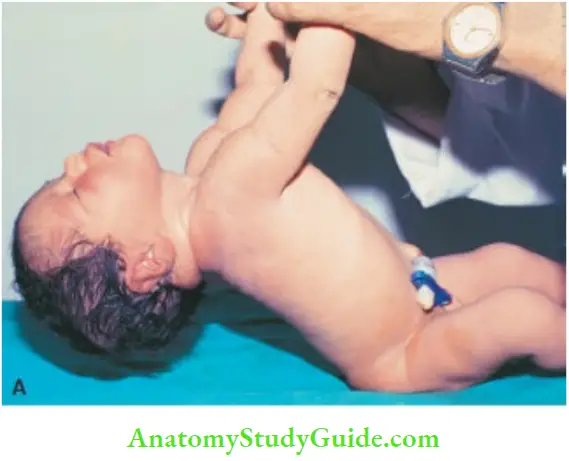
Exaggerated startle reaction to sound is seen in infants with Tay-Sachs disease, GM1 gangliosidosis, Sandhoff disease, progressive cerebral degeneration, and blindness. The supine baby is lifted off the cot by gently holding at the wrists.
2. Glabellar tap: Tapping of nation is followed by closure of eyes in infants above 30 weeks gestation
3. Rooting and sucking responses: Stimulation of the angle of the mouth or lips initiates rooting and sucking in infants above 34 weeks gestation. The mother or nurse’s report regarding the feeding behavior of the baby is more informative.
4. Tonic neck reflex: The baby assumes an asymmetrical posture when the head is turned to one side. The limbs facing the head are extended while the limbs on the opposite side are flexed.
5. Tonic neck reflex: When the baby’s head is turned to one side, the ipsilateral arm and leg get extended while contralateral limbs are flexed. The asymmetric tonic neck reflex disappears after 2 to 3 months. If a baby constantly or persistently maintains the tonic neck posture, it is abnormal and may signify as a marker of the future development of cerebral palsy
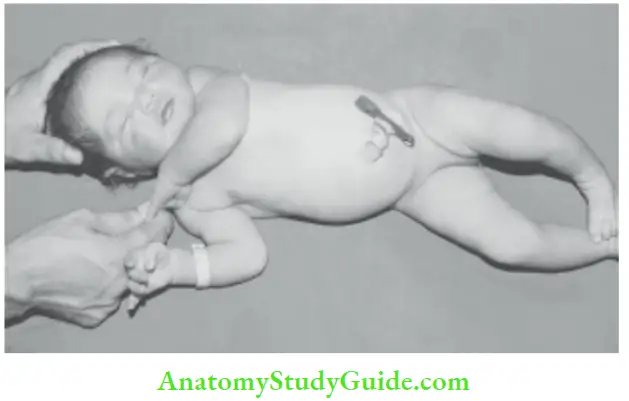
6. Traction reflex: The supine baby when pulled up by holding at the wrists, his ability to flex the arms and neck should be observed.
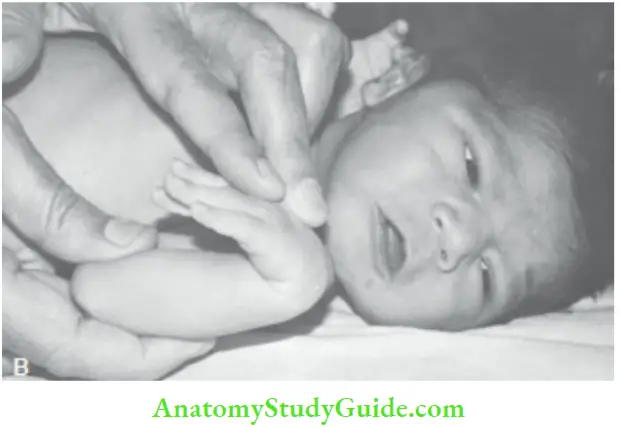
7. Palmar and plantar grasp: The finger is placed on the palmar surface of the fingers or plantar surface of toes of the baby to elicit grasp or flexion of digits. Stroke the dor stun of the hand to persuade the baby to open the fist.
8. Most primitive reflexes: Disappear between 4 and 5 months of age and their persistence is considered as an early sign of cerebral palsy.
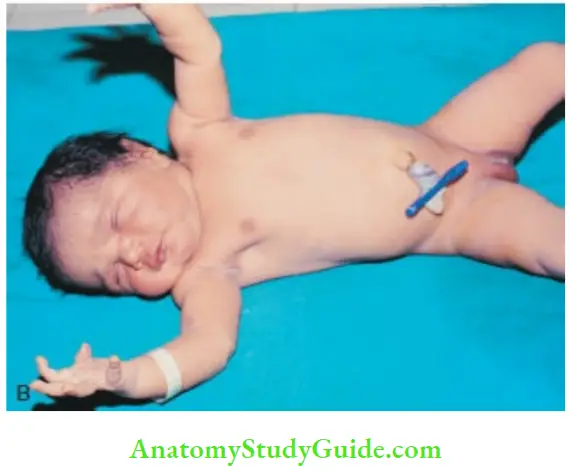
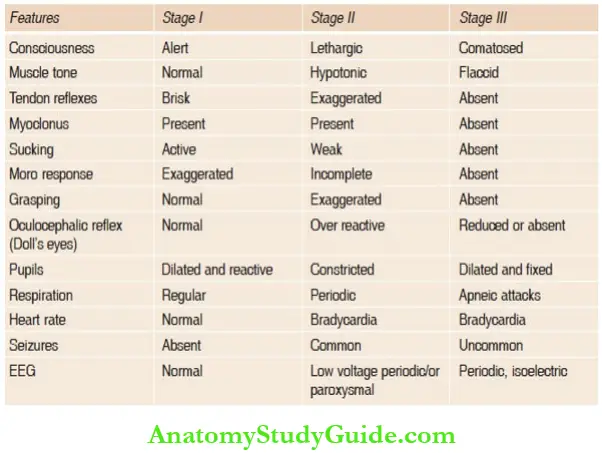
Infants with fetal hypoxia or birth asphyxia should be closely monitored for the severity of hypoxic-ischemic encephalopathy (HIE) by the Sarnat staging system ( The occurrence of seizures within 36 hours of age usually heralds the onset of hypoxic-ischemic encephalopathy (HIE).
Brainstem involvement is ominous and characterized by irregularity of breathing, apneic attacks, changes in pupillary size and dysconjugate eye movements, poor sucking and swallowing with pooling of secretions in the oral cavity
Sensory Functions:
Sensory testing is of limited value in the newborn. The response to painful stimuli should be assessed if injury or disease of peripheral nerves or spinal cord is suspected. The anal reflex must be elicited in infants with neural tube defects.
Examination of Hips:
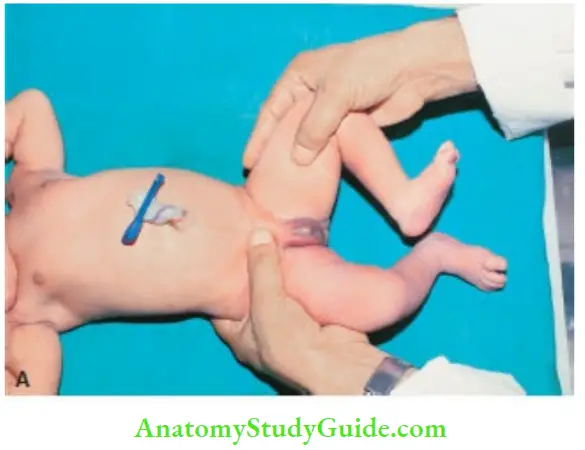
The hip joints should be examined for evidence of developmental dysplasia of the hips (DDH). The condition is more common in girls especially firstborn, with breech presentation, post-dated, and associated with oligohydramnios.
There may be family history of the condition and infant may have other associated postural deformities especially in the feet.
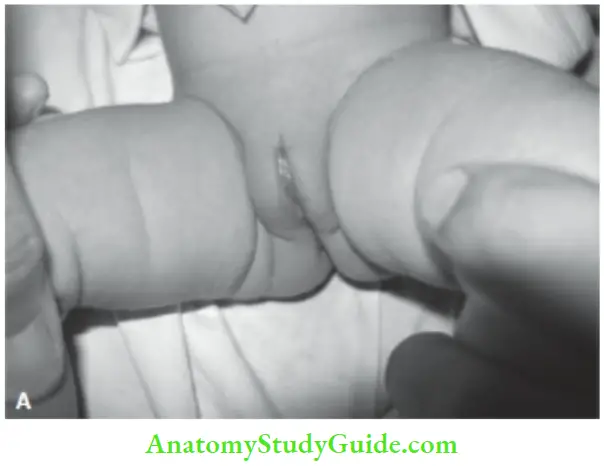
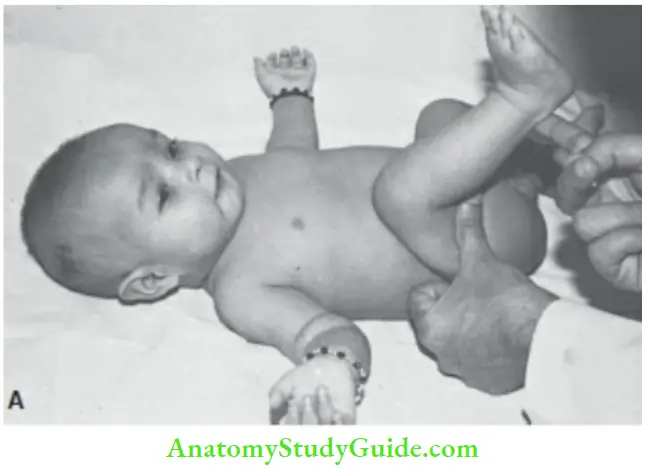
The classical signs of dislocation are not seen in the neonatal period. The instability of the hip joint is best detected by modified Ortolani/Barlow maneuvers as described below.
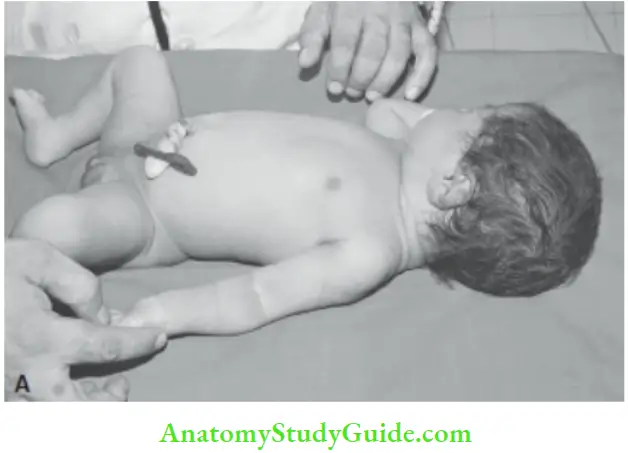
The infant is placed on his back with legs towards the examiner. The baby should be undressed from waist downwards. The examination should be performed with care, gentleness, and warm hands.
Infants should be calm, relaxed, and adequately fed. It is preferable to test one hip at a time. The examiner tries to assess whether tire hip is dislocated or it is unstable and dislocate.
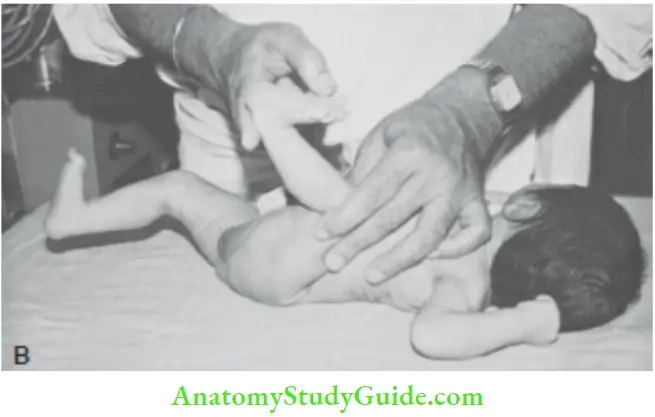
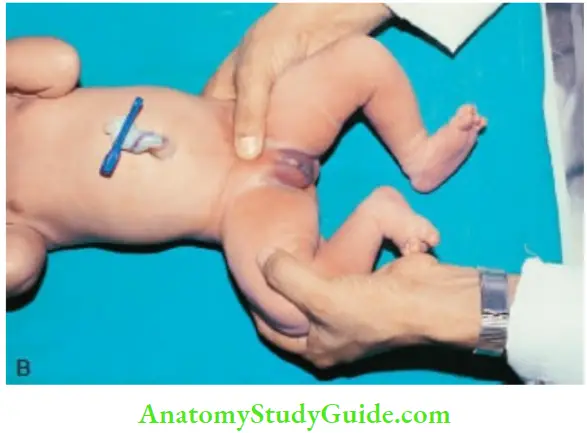
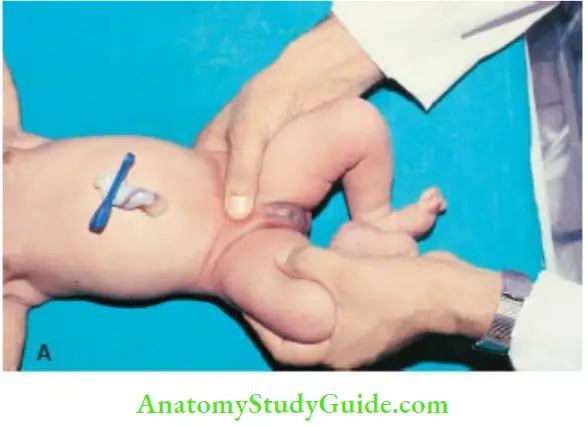
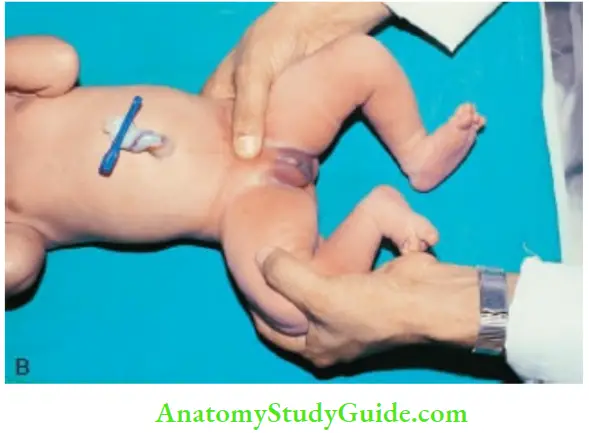
For examination of the left hip, the examiner steadies the infant’s pelvis between the thumb of his left hand placed on the symphysis pubis and the fingers under the sacrum
The left thigh is flexed by keeping the knees bent. It is grasped by the examiner’s right hand by placing a middle finger on the outside over the greater trochanter and thumb on theinner side of the thigh opposite the lesser trochanter.
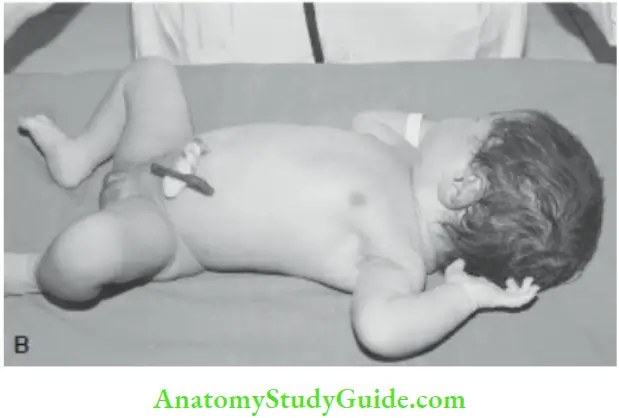
In the first maneuver, the examiner assesses whether the hip is dislocated or not (Ortolani or reduction test).
The pressure is applied over the greater trochanter with the middle finger by abducting the hip and lifting tire thigh upward in an attempt to relocate the displaced femoral head back into the acetabulum.
If the head is felt to move (usually not more than 0.5 cm) into the acetabulum with or without a palpable and/or audible ‘Clunk’, it confirms the presence of dislocation.
If the dislocation is not present, an effort is then made to test for subluxation (dissociability) of the hip by the Barlow test (stress test).
With the thumb placed on the inner side of the thigh, backward and outward pressure is applied to the head of the femur in an attempt to dislocate it.
If the femoral head is felt to move backward over the rim of the acetabulum, for a distance of 0.5 cm, with or without a palpable or audible clunk, the hip is said to be dislocatable.
The right hip is examined by reversing the role of the examiner’s hands. The ligamentous clicks without movement of the head of the femur in or out of the acetabulum may be elicited in 5–10 percent of hips and should be disregarded.
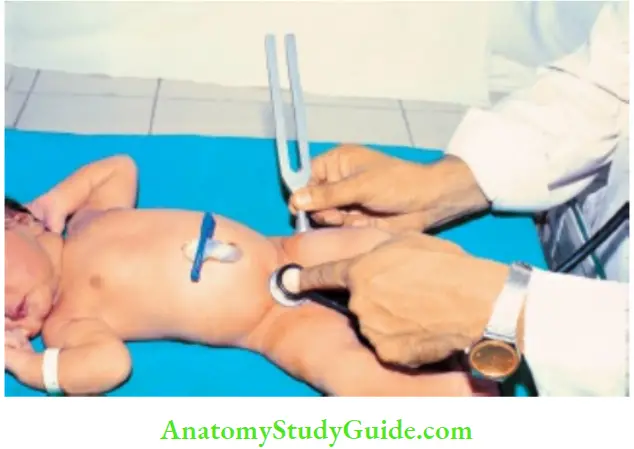
Auscultatory method:
It is based on the principle that the vibrations of the timing fork placed on the greater trochanter cannot be transmitted to the pubic symphysis on the dislocated side.
The chestpiece of the stethoscope is placed on the pubic symphysis and the foot of the vibrating timing fork is placed on the greater trochanter on either side one after the other
There is poor transmission of vibrations of the tuning fork when the femoral head is dislocated.
The “Dislocatable” femoral head cannot be identified by this method, bilateral congenital dislocation of hips, and the transmission of vibrations of tuning fork would be adversely affected on both sides.
Older Infants (>3 months):
In infants with untreated congenital dislocation of hips, there may be asymmetry of gluteal and thigh folds, shortening of the affected limb, and limitation of abduction of the affected hip.
The Allis’s sign may be positive, i.e. in a supine child when both knee joints and hips are flexed and feet are held flat on the cot, the knee on the affected side will be at a lower level due to posterior dislocation of the hip.
Infants with untreated unilateral DDH are likely to manifest with limping and toe walking on affected side while bilateral DDH is associated with increased lumbar lardosis, prominent buttocks, and a waddling gait.
Infants suspected to have DDH should undergo a dynamic ultrasound examination of hip joint by a skilled pediatric radiologist.

Daily “Clinical Screening” Of The Baby
Between first day of examination and the day of discharge, a detailed examination is unnecessary and may in fact be harmful for the baby for fear of introducing infection.
The baby-mother dyad should be approached twice a day to enquire about any feeding problems, vomiting, or bowel disorders and to assess and allay.
The anxiety of the mother regarding various developmental peculiarities may attract her attention. The onset and intensity of jaundice should be watched.
Any evidence of superficial infections, such as conjunctivitis, pyoderma, umbilical sepsis, and oral thrush should be looked for.
Examination At Discharge
A detailed examination of the baby at the time of discharge is essential to make sure that no anomalies and birth injuries have been missed and initial lactational and feeding difficulties have been surpassed.
Careful auscultation of the heart is essential because previously detected functional murmur may no longer be audible and new murmurs may appear any time during the neonatal period.
It is recommended to screen the baby for arterial oxygen saturation with a pulse oximeter and if SaO2 is less than 85 percent on two occasions in a hemodynamically stable baby, 2D echocardiography should be done to exclude congenital heart defect.
The mother should be advised about feeding, vitamins and iron supplements, general cleanliness, immunizations, and given an appointment for visit to the Well Baby Clinic.
High-risk babies discharged from the NICU should be followed up for developmental assessment and detailed examination of the central nervous system and special senses in a Special Developmental Clinic.
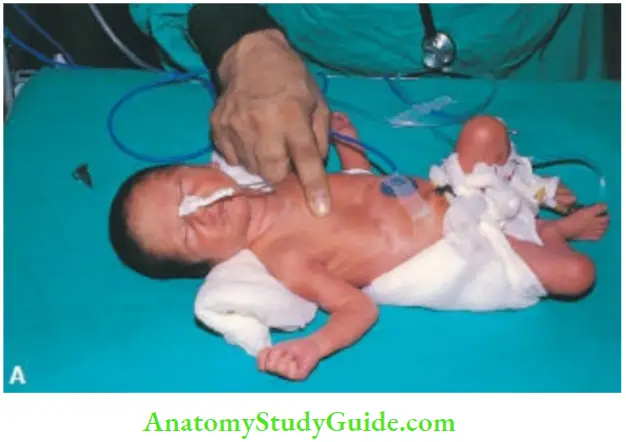
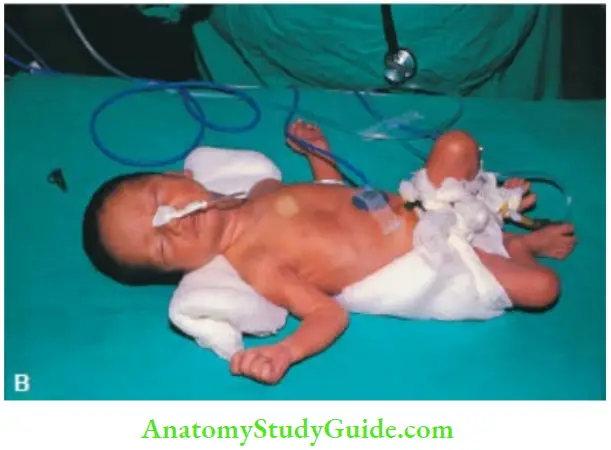
Sick Babies In The Nicu
Babies are looked after in the neonatal intensive care unit (NICU) when a baby is extremely preterm, critically sick, malformed or when mother is unwell or unwilling to look after the baby. Check perinatal events and nature of resuscitation provided.
Look for various life-threa tenting conditions, like RDS, seizures, sepsis, jaundice, bleeding manifestations and shock. Ask for history of procedures, like CPAP, assisted ventilation and its duration, whether received surfactant or not, oxygen dependency, thoracostomy, simple or exchange blood transfusion.
What are the findings on a routine ultrasound examination of brain and indirect ophthalmoscopy for ROP?
Check the vital signs on the monitor. Assess hemodynamic stability including activity, color, capillary refill time by pressing over the sternum. Is the baby having any respiratory distress or apneic attacks?
Is the baby tolerating the enteral feeds without any abdominal distension or gastric residuals. The baby should be screened for sepsis, patent ductus arteriosus, necrotizing enterocolitis, and intraventricular hemorrhage.
Is the daily weight gain velocity of the baby satisfactory? The baby should be screened daily to look for clinical criteria to assess the well-being of the baby in the NICU
Cot-side criteria indicating that a preterm baby is healthy:
- Baby is alert, active, and pink.
- Vital signs are stable.
- The trunk is warm to the touch and extremities are reasonably warm and pink.
- No respiratory distress and apneic attacks.
- The baby is tolerating enteral feeds without any vomiting and abdominal distension.
- Daily weight gain is 1.0–1.5% of the body weight, i.e. 10–15 g/kg per day
Leave a Reply