Physiology Of Pain Introduction And Definition
- Pain is defined as an unpleasant and emotional experience associated with or without actual tissue damage. The pain sensation is described in many ways sharp, pricking, electric, dull ache, shooting, cutting, stabbing, etc. Often it induces crying and fainting.
- It is produced by real or potential injury to the body. Often it is expressed in terms of injury. For example, pain produced by fire is expressed as a burning sensation pain produced by severe sustained contraction of skeletal muscles is expressed as cramps.
Read And Learn More: Medical Physiology Notes
Table of Contents
- Pains may be acute or chronic. Acute pain is a sharp pain of short duration with an easily identified cause. Often it is localized in a small area before spreading to neighboring areas.
- Usually, it is treated with medications. Chronic pain is intermittent or constant pain with different intensities. It lasts for longer periods. It is somewhat difficult to treat chronic pain and it needs professional expert care.
Benefits Of Pain Sensation
Pain is an important sensory symptom. Though it is an unpleasant sensation, it has protective or survival benefits such as:
- It gives a warning signal about the existence of a problem or threat. It also creates awareness of injury
- It prevents further damage by causing reflex withdrawal of the body from the source of injury
- It forces the person to rest or to minimize the activities thus enabling the rapid healing of the injured part It urges the person to take the required treatment to prevent major damage.
Components Of Pain Sensation
A pain stimulus produces two pain sensations
- Fast pain
- Slow pain.
- Fast pain is the first sensation whenever a pain stimulus is applied. It is experienced as a bright, sharp, and localized pain sensation. The fast pain is followed by the slow pain which is experienced as a dull, diffused, and unpleasant pain.
- The receptors for both components of pain are the same, i.e. the free nerve endings. But, the afferent nerve fibers are different. The fast pain sensation is carried by A5 fibers and the slow pain sensation is carried by C type of nerve fibers.
Pathways Of Pain Sensation
Pain sensation from various parts of the body is carried to the brain by different pathways which are:
- The pathway from the skin and deeper structures
- Pathway from face
- Pathway from viscera
- The pathway from the pelvic region
Pathway Of Pain Sensation From Skim And Deeper Structures
- Receptors: The receptors of pain sensation are the free nerve endings that are distributed throughout the body.
- First-Order Neurons: First-order neurons are the cells in the posterior nerve root ganglia that receive the impulses of pain sensation from the pain receptors through their dendrites. These impulses are transmitted to the spinal cord through the axons of these neurons.
- Fast pain fibers: Fast pain sensation is carried by Aδ type afferent fibers which synapse with neurons of the marginal nucleus in the posterior gray horn.
- Slow pain fibers: Slow pain sensation is carried by C-type afferent fibers which synapse with neurons of substantia gelatinosa of Rolando in the posterior gray horn.
- Second-Order Neurons: The neurons of the marginal nucleus and substantia gelatinosa of Rolando form the second-order neurons. Fibers from these neurons ascend in the form of the lateral spinothalamic tract.
- Fast pain fibers
- Fibers of fast pain arise from neurons of the marginal nucleus. Immediately after taking origin, the fibers cross the midline via the anterior gray commissure, reach the lateral white column of the opposite side, and ascend.
- These fibers form the neo-spinothalamic fibers in the lateral spinothalamic tract. These nerve fibers terminate in the ventral posterolateral nucleus of the thalamus. Some of the fibers terminate in the ascending reticular activating system of the brainstem.
- Slow pain fibers: The fibers of slow pain which arise from neurons of substantia gelatinosa, cross the midline and run along the fibers of fast pain as paleospinothalamic fibers in the spinothalamic tract. One-fifth of these fibers terminate in the ventral posterolateral nucleus of the thalamus. The remaining fibers terminate in any of the following
- Nuclei of the reticular formation in the brainstem
- Tectum of midbrain
- Gray matter surrounds the aqueduct of Sylvius.
- Fast pain fibers
- Third-Order Neurons: The third-order neurons of the pain pathway are the neurons in
- Thalamic nucleus
- Reticular formation
- Tectum
- Gray matter around the aqueduct of Sylvius.
- Axons from these neurons reach the sensory area of the cerebral cortex. Some fibers from reticular formation reach the hypothalamus.
- Center for Pain Sensation: The center for pain sensation is in the postcentral gyrus of the parietal cortex. Fibers reaching the hypothalamus are concerned with the arousal mechanism due to pain stimulus.
Pathway Of Pain Sensation From Face: Pain sensation from the face is carried by the trigeminal nerve.
Pathway Of Pain Sensation From Viscera: The pain sensation from the thoracic and abdominal viscera is transmitted by sympathetic (thoracolumbar) nerves. Pain from the esophagus, trachea, and pharynx is carried by vagus and glossopharyngeal nerves.
Pathway Of Pain Sensation From Pelvic Region: Pain sensation from deeper structures of the pelvic region is conveyed by sacral parasympathetic nerves.
Visceral Pain
Pain from the viscera is unpleasant. It is poorly localized.
Causes Of Visceral Pain
- Ischemia: The substances released during ischemic reactions like bradykinin and proteolytic enzymes stimulate the pain receptors of viscera.
- Chemical stimuli: Chemical substances like acidic gastric juice leak from ruptured ulcers into the peritoneal cavity and produce pain.
- Spasm of hollow organs: Spastic contraction of smooth muscles in the gastrointestinal tract and other hollow organs of viscera cause pain by stimulating the free nerve endings.
- Overdistention of hollow organs also causes pain.
Referred Pain
Referred Pain Definition: Referred pain is pain that is perceived at a site adjacent to or away from the site of origin. The deep pain and some visceral pain are referred to in other areas. However, the superficial pain is not referred to.
Examples Of Referred Pain
- Cardiac pain is felt in the inner part of the left arm and left shoulder
- Pain in the ovary is referred to as umbilicus Pain from the testis is felt in the abdomen
- Pain in the diaphragm is referred to the right shoulder
- Pain in gallbladder is referred to epigastric region
- Renal pain is referred to as loin.
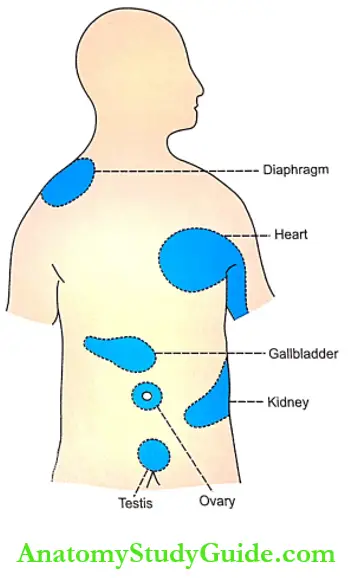
Mechanism Of Referred Pain
- Dermatomal Rule
- According to the dermatomal rule, pain is referred to a structure, which is developed from the same dermatome from which the pain-producing structure is developed.
- A dermatome includes all the structures or parts of the body, which are innervated by afferent nerve fibers of one dorsal root. For example, the heart and inner aspect of the left arm originate from the same dermatome. So, the pain in the heart is referred to left arm.
Neurotransmitters Involved In Pain Sensation
Glutamate and substance P are the neurotransmitters secreted by the pain nerve endings. The Aδ afferent fibers which transmit impulses of fast pain secrete glutamate. C-type fibers which transmit impulses of slow pain secrete substance P.
Analgesia System
- Analgesia system means the pain control system. The body has its own analgesia system in the brain which provides short-term relief from pain.
- It is also called an endogenous analgesia system. The analgesia system has its own pathway through which it blocks the synaptic transmission of pain sensation in the spinal cord and thus attenuates the experience of pain. In fact, analgesic drugs such as opioids act through this system and provide controlled pain relief.
Analgesic Pathway; The analgesic pathway that interferes with pain transmission is often considered as the descending pain pathway, the ascending pain pathway being the afferent fibers that transmit pain sensation to the brain.
- Role of Analgesic Pathway in Inhibiting Pain Transmission
- The fibers of the analgesic pathway arise from the frontal lobe of the cerebral cortex and hypothalamus.
- These fibers terminate in the gray matter surrounding the 3 ventricles and aqueducts of Sylvius (periaqueductal gray matter).
- The fibers from here, descend down to the brainstem and terminate on
- Raphe Magnus nucleus situated in the reticular formation of lower pons and upper medulla
- Nucleus reticularis paragigantocellularis situated in the medulla
- The fibers from these reticular nuclei descend through a lateral white column of the spinal cord and reach the synapses of the neurons in the afferent pain pathway situated in the anterior gray horn. The synapses of the afferent pain pathway are between:
- Aδ type afferent fibers and neurons of the marginal nucleus
- C-type afferent fibers and neurons of substantia gelatinosa of Rolando
- At the synaptic level, the analgesic fibers release the neurotransmitters and inhibit pain transmission before being relayed to the brain.
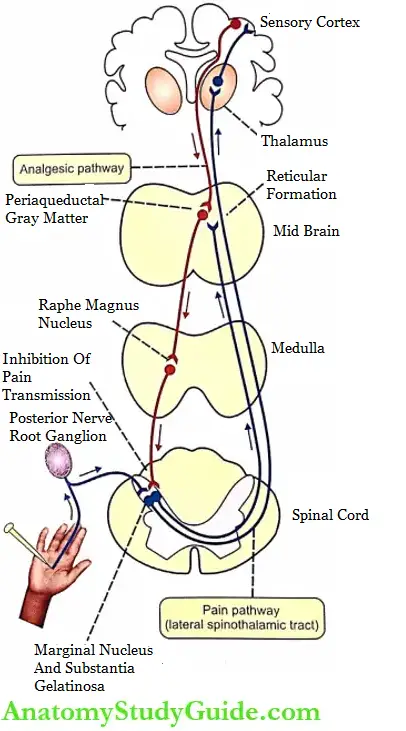
Neurotransmitters of Analgesic Pathway: The neurotransmitters released by the fibers of the analgesic pathway are serotonin and opiate receptor substances namely encephalin, dynorphin, and endorphin.
Gate Control Theory
- The psychologist Ronald Melzack and the anatomist Patrick Wall Gate proposed the gate control theory for pain in 1965 to explain pain suppression.
- According to them, the pain stimuli transmitted by afferent pain fibers are blocked by a gate mechanism located at the posterior gray horn of the spinal cord. If the gate is opened, pain is felt. If the gate is closed, pain is suppressed.
Mechanism of Gate Control at Spinal Level
- When pain stimulus is applied to any part of the body, besides pain receptors, the receptors of other sensations such as touch are also stimulated.
- When all these impulses reach the spinal cord through the posterior nerve root, the fibers of touch sensation (posterior column fibers) send collaterals to the neurons of the pain pathway, i.e. cells of the marginal nucleus and substantia gelatinosa.
- The impulses of touch sensation passing through these collaterals inhibit the release of glutamate and substance P from the pain fibers.
- This closes the gate and the pain transmission is blocked.
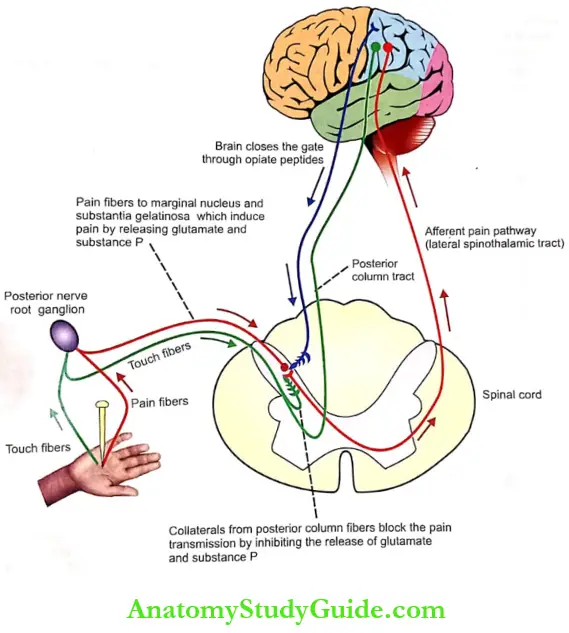
Role of Brain in Gate Control Mechanism: According to Melzack and Wall brain also plays some important role in the gate control system of the spinal cord as follows:
- If the gates in the spinal cord are not closed, the pain signals reach the thalamus through the lateral spinothalamic tract
- The signals are processed in the thalamus and sent to the sensory cortex
- The perception of pain occurs at the cortical level in the context of the person’s emotional status and previous experiences
- The person responds to the pain based on the integration of all this information in the brain. Thus, the brain determines the severity and extent of pain
- To minimize the severity and extent of pain, the brain sends a message back to the spinal cord to close the gate by releasing pain relievers such as opiate peptides
- Now the pain stimulus is blocked and the person feels less pain.
Significance of Gate Control
- Thus, the gating of pain at the spinal level is similar to presynaptic inhibition. It forms the basis for the relief of pain through rubbing, massage techniques, application of ice packs, acupuncture, and electrical analgesia.
- All these techniques relieve pain by stimulating the release of endogenous pain relievers (opioid peptides) which close the gate and block the pain signals.
Applied Physiology
- Analgesia: Analgesia means loss of pain sensation.
- Hyperalgesia: Hyperalgesia is the increased sensitivity to pain
- Paralgesia: Abnormal pain sensation is called paralgesia.
Leave a Reply