Pituitary Gland Introduction
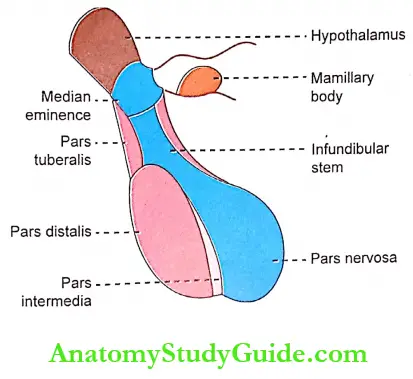
- The pituitary gland is also known as hypophysis. It is a small gland with a diameter of 1 cm and weight of 0.5.1 gm. It lies at the base of the brain in sella turcica.
- It is connected with the hypothalamus by the pituitary stalk or hypophyseal stalk.
On the basis of physiology, the pituitary gland is divided into two portions:
Table of Contents
- Anterior pituitary or adenohypophysis
- Posterior pituitary or neurohypophysis.
Read And Learn More: Medical Physiology Notes
- Between the two portions, there is a small, relatively avascular zone called pars intermedia. It forms a part of anterior pituitary.
- It is very small in human beings and is larger and more functional in some lower animals.
- Even though anterior pituitary and posterior pituitary are situated in such close approximation, both are entirely different in their development, structure, and function.
Anterior Pituitary
Anterior Pituitary Parts: Anterior pituitary consists of three divisions
- Pars distalis
- Pars tuberalis
- Pars intermedia.
Anterior Pituitary Development
- Anterior and posterior pituitary glands develop from different parts. The anterior pituitary is ectodermal in origin It arises from the pharyngeal epithelium as an upward growth known as Rathke’s pouch.
- The posterior pituitary is neuroectodermal in origin. And, it arises from the base of the brain or hypothalamus as a downward diverticulum. The Rathke’s pouch and the downward diverticulum from the hypothalamus meet midway between the roof of the buccal cavity and base of brain and lie close together
Anterior Pituitary Histology: Depending upon the staining property, the cells of anterior pituitary are classified into two types:
- Chromophobe cells
- Chromophil cells.
1. Chromophobe Cells: Chromophobe cells do not possess granules and stain poorly. These cells are not secretory in nature but are believed to be the precursors of chromophil cells. The chromophobe cells form about 50% of total cells in the adenohypophysis.
2. Chromophil Cells
- Chromophil cells contain large number of granules and are darkly stained. According to the staining nature, chromophil cells are of two types, acidophilic cells, or alpha cells, and basophilic cells, or beta cells.
- The alpha cells are about 35% and the beta cells are about 15%. Based on the secretory nature chromophil cells are classified into five types:
- Somatotropes that secrete growth hormone
- Corticotropes which secrete adrenocorticotropic hormone
- Thyrotropes which secrete thyroid-stimulating hormone
- Gonadotropes which secrete follicle-stimulating hormone and luteinizing hormone
- Lactotropes which secrete prolactin.
Somatotropes and lactotrophs are acidophilic cells, whereas others are basophilic cells. Somatotropes form about 30-40% of the chromophil cells. So, pituitary tumors that secrete large quantities of human growth hormone are called acidophilic tumors.
Regulation Of Secretion
- Hypothalamo-Hypophyseal Relationship
- It is the relationship between the hypothalamus and pituitary gland. Hypothalamus secretes several hormones which are transported to the anterior pituitary and posterior pituitary. But the mode of transport of these hormones is different.
- The hormones secreted by the hypothalamus are transported to anterior pituitary through hypothalamic-hypophysial portal blood vessels.
- But, the hormones from the hypothalamus to the posterior pituitary are transported by nerve fibers of the hypothalami-hypophyseal tract.
- Regulation of Anterior Pituitary Secretion
- Hypothalamus controls anterior pituitary through the releasing and inhibitory hormones (factors) which are called neurohormones.
- These hormones are secreted in the hypothalamus and transported from the hypothalamus to the anterior pituitary through hypothalami-hypophyseal portal vessels.
- Some special nerve cells present in the hypothalamus synthesize and secrete the releasing and inhibitory hormones. Such nerve cells are situated in various parts of the hypothalamus and send their nerve fibers (axons) into the median eminence and the tuber cinerium.
- The hormones secreted by these nerve cells are released into median eminence and tuber cinerium. From here these hormones are taken into the blood in hypothalamo- hypophyseal portal system and transported to the anterior pituitary.
- Releasing and Inhibitory Hormones: Hypothalamus secretes releasing hormones for most of the anterior pituitary hormones, and inhibitory hormones for few anterior pituitary hormones. Following are the hormones secreted by the hypothalamus:
- Growth hormone-releasing hormone (GHRH) – stimulates the release of growth hormone
- Growth hormone-releasing polypeptide (GHRP) – stimulates the release of GHRH and growth hormone
- Growth hormone inhibitory hormone (GHIH) or somatostatin – inhibits growth hormone release
- Thyrotropic-releasing hormone (TRH) – stimulates the release of thyroid-stimulating hormone
- Corticotropin-releasing hormone (CRH) – stimulates the release of adrenocorticotropin
- Gonadotropin-releasing hormone (GnRH) – the release of the gonadotropins – FSH and LH
- Prolactin inhibitory hormone (PIH) – inhibits prolactin secretion. It is suggested that PIH is dopamine.

Hormones Secreted By Anterior Pituitary: Anterior pituitary is also known as the master gland because it regulates many other endocrine glands. Six hormones are secreted by the anterior pituitary:
- Growth hormone (GH) or somatotropic hormone (STH)
- Thyroid-stimulating hormone (TSH) or thyrotropic hormone
- Adrenocorticotropic hormone (ACTH)
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH in females) or interstitial cell-stimulating hormone (ICSH in males)
- Prolactin.
- The first five hormones stimulate the other endocrine glands. Growth hormone also stimulates the secretory activity of liver and other tissues. Therefore, these five hormones are called tropic hormones.
- The follicle-stimulating hormone and the luteinizing hormone are together called gonadotropic hormones or gonadotropins because of their action on the gonads. Prolactin is concerned with milk secretion.
- Recently, the hormone β-Lipotropin is found to be secreted by anterior pituitary.
Growth Hormone
- Source of Secretion: GH is secreted by the acidophils of the anterior pituitary, which are also known as somatotropes.
- Chemistry, Blood Level, and Daily Output: GH is protein in nature having a single chain polypeptide with 191 amino acids. Its molecular weight is 21,500. The basal level of GH concentration in blood of a normal adult is up to 300 ng/dL and in children, it is about 500 ng/dL. Its daily output in adults is 0.5-1.0 mg.
- Transport: GH is transported in blood by GH-binding proteins (GHBPs).
- Half-life and Metabolism: The half-life of circulating growth hormone is about 20 minutes. The proteolytic degradation of GH occurs mainly in the liver and kidney.
- Actions of Growth Hormone:
- GH is responsible for the growth of almost all tissues of the body, which are capable of growing.
- It actually increases the size and number of cells. GH also causes specific differentiation of certain types of cells like bone cells and muscle cells.
- Thus, GH is responsible for the general growth of the body. Deficiency of GH in children causes stunted growth leading to dwarfism. And, hypersecretion of GH causes enormous growth of the body leading to gigantism.
- GH also acts on the metabolism of all three major types of foodstuffs in the body, viz. proteins, lipids, and carbohydrates.
1. On Metabolism: GH increases the synthesis of proteins, mobilization of lipids, and conservation of carbohydrates.
- On protein metabolism: GH accelerates the synthesis of protein by:
- Increasing the amino acid transport through the cell membrane: So, the concentration of amino acids in the cells increases and thus, the synthesis of proteins is accelerated.
- Increasing the RNA translation: GH increases the translation of RNA in the cells. Because of this, the ribosomes are activated and more proteins are synthesized. The translation of RNA by the effect of GH occurs even without the increase in transport of amino acid into the cells.
- Increasing the transcription of DNA to RNA: It also stimulates the transcription of DNA to RNA. This, in turn accelerates the synthesis of proteins in the cells.
- Decreasing the catabolism of protein: GH inhibits the breakdown of cellular protein. It helps in the building up of the tissues.
- Promoting the anabolism of proteins indirectly: GH increases the response of p cells of the islets in pancreas to glucose and arginine. It results in release of insulin which has an anabolic effect on proteins.
- On fat metabolism
- GH mobilizes fats from adipose tissue. Because of this, the concentration of fatty acids increases in the body fluids. These fatty acids are used for the production of energy by the cells. So proteins are spared.
- During the utilization of fatty acids for the production of energy, lot of acetoacetic acid is produced by the liver and released into the body fluids leading to ketosis.
- Sometimes excess mobilization of fat from the adipose tissue causes accumulation of fat in liver, resulting in fatty liver.
- On carbohydrate metabolism: The main action of GH on carbohydrates is the conservation of glucose. The major effects of GH on the carbohydrate metabolism are:
- Decrease in the peripheral utilization of glucose for the production of energy:
- GH reduces the peripheral utilization of glucose for energy production.
- It is because of the formation of acetyl CoA during the metabolism of fat influenced by GH. The acetyl CoA inhibits the glycolytic pathway.
- Moreover, since the GH increases the mobilization of fat, more fatty acid is available for the production of energy. By this way, the GH reduces the peripheral utilization of glucose for energy production.
- Increase in the deposition of glycogen in the cells: Since the glucose is not utilized for energy production by the cells, it is converted into glycogen. Thus, the concentration of glycogen increases in the cells.
- Decrease in the uptake of glucose by the cells: As the accumulation of glycogen increases in cells by the influence of the GH, the cells become saturated with glycogen. Because of this, no more glucose can enter the cells. Ultimately the blood glucose level increases.
- Diabetogenic effect of GH: Hypersecretion of GH increases blood glucose level enormously. It causes continuous stimulation of the p cells in the islets of Langerhans in the pancreas. So, insulin secretion increases.
- In addition to this, the GH also stimulates the p cells of islets in pancreas directly and causes secretion of insulin. Because of the excess stimulation, the p cells are burnt out at one stage.
- This causes a deficiency of insulin, which leads to true diabetes mellitus or full blown diabetes mellitus. This effect of GH is called the diabetogenic effect.
- Decrease in the peripheral utilization of glucose for the production of energy:
2. On Bones: In embryonic stage, GH is responsible for the differentiation and the development of bone cells. In later stages, GH increases the growth of the skeleton. It increases both the length as well as the thickness of the bones. In the bones, GH increases:
- Protein synthesis and deposition by chondrocytes and osteogenic cells
- Multiplication of chondrocytes and osteogenic cells
- Formation of new bones – this is because the GH causes conversion of chondrocytes into osteogenic cells
- Increases intestinal calcium absorption and thereby enhances the availability of calcium for mineralization of bone matrix.
- GH increases the length of the bones until epiphysis fuses with the shaft. Usually, fusion occurs at puberty. After the epiphyseal fusion, length of the bones cannot be increased.
- However, it stimulates the osteoblasts strongly. So, the bone continues to grow in thickness throughout life. Particularly, the membranous bones such as jaw bone and skull bones become thicker under the influence of GH.
- Hypersecretion of GH before the fusion of epiphysis with the shaft of the bones causes enormous growth of the skeleton leading to a condition called gigantism.
- And hypersecretion of GH after the fusion of epiphysis with the shaft of the bones leads to a condition called acromegaly.
Mode of Action of GH on Bones and Metabolism: GH acts on bones, growth, and protein metabolism through a substance called somatomedin, which is secreted by liver. GH stimulates the liver to secrete somatomedin. Sometimes, in spite of normal secretion of GH, dwarfism occurs due to the absence or deficiency of somatomedin.
Somatomedin: It is a polypeptide with a molecular weight of about 7500. Many somatomedins are found in animals. However, in human beings, only two somatomedins are present.
- Insulin-like growth factor-1 (IGF-I), which is also called somatomedin-C
- Insulin-like growth factor-2.
- Among the two somatomedins, the somatomedin-C (IGF-I) acts on the bones and induces growth and other effects on bones. It also acts on protein metabolism. Insulin like growth factor-ll plays important role in the growth of the fetus.
- Duration of action of GH and somatomedin-C
- GH is transported in blood by loose binding with plasma protein. So, at the site of action, the GH is released from the plasma protein rapidly.
- The action of the hormone also lasts only for a short duration of 20 minutes. But, the somatomedin-C binds with plasma proteins very strongly. Because of this, the molecules of somatomedin-C are released slowly from the plasma proteins.
- Thus, it can act continuously for a longer duration. The action of somatomedin-C lasts for about 20 hours. The mode of action of somatomedin is by the formation of the second messenger called cyclic AMP).
Growth Hormone Receptor
- Growth hormone receptor is called growth hormone secretagogue (GHS) receptor. It is a transmembrane receptor belonging to the cytokine receptor family.
- Growth hormone acts by binding with a single transmembrane receptor situated mainly in liver cells.
- The hormone-receptor complex induces various intracellular enzyme pathways resulting in the secretion of somatomedin. Somatomedin in turn executes the actions of growth hormone.
Regulation of GH Secretion: GH secretion increases in
- Hypoglycemia
- Fasting
- Starvation
- Exercise
- Stress and trauma
- Initial stages of sleep.
- GH secretion decreases in:
- Hyperglycemia
- Increase in free fatty acids in blood
- Later stages of sleep.
- GH secretion decreases in:
Role of the Hypothalamus in the Secretion of GH: Hypothalamus plays an important role in the regulation of secretion of GH. It regulates GH secretion by releasing three hormones:
- Growth hormone-releasing hormone (GHRH)
- Growth hormone-releasing polypeptide (GHRP)
- Growth hormone inhibitory hormone (GHIH) which is also called somatostatin.
These three hormones are transported from the hypothalamus to anterior pituitary by hypothalamic-hypophyseal portal blood vessels.
- Growth hormone-releasing hormone (GHRH): It is the important factor that increases the secretion of GH. It increases the GH secretion by stimulating the somatotropes of anterior pituitary.
- Growth hormone-releasing polypeptide (GHRP): It is another releasing hormone secreted by the hypothalamus. It promotes the release of GHRH from hypothalamus and GH from pituitary.
- Growth hormone inhibitory hormone (GHIH)- Somatostatin: The GHIH or the somatostatin inhibits the secretion of GH. Somatostatin is also secreted by delta cells of islets of Langerhans in pancreas.
Feedback Control
- GH secretion is under negative feedback control (Chapter 4) Hypothalamus releases GHRH and GHRP, which in turn promote release of GH from anterior pituitary, GH acts on various tissues. It also activates the fiver oaSls to secrete somatomedin-C (IGF-I).
- Mow. The somatomedin-C increases the release of GHIH from the hypothalamus. GHIH in turn inhibits release of GH from the pituitary. Somatomedin also inhibits the release of GHRP from the hypothalamus. It acts on pituitary directly and inhibits the secretion of GH.
- GH inhibits its own secretion by stimulating the release of GHIH from the hypothalamus. This type of feedback is called short-loop feedback control. Similarly, GHRH inhibits its own release by short-loop feedback control.
- Whenever the blood level of GH decreases, the GHRH is secreted from the hypothalamus. It in turn causes secretion of GH from pituitary.
- A variety of factors such as hypoglycemia, fasting, starvation, exercise, stress, and trauma promote the secretion GH by acting at the hypothalamic level. In a similar fashion, glucose and free fatty acids inhibit the secretion of GH.
- Role of Ghrelin in the Secretion of GH
- Ghrelin is a peptide hormone synthesized by epithelial cells in the fundus of stomach. It is also produced in smaller amount in the hypothalamus, pituitary, kidney, and placenta.
- Ghrelin promotes secretion of GH by stimulating somatotropes directly. The action of ghrelin on GH secretion is integrated with GHRH and GHIH.

Other Hormones Of Anterior Pituitary
- Thyroid Stimulating Hormone (TSH): TSH is necessary for the growth and the secretory activity of the thyroid gland. It has many actions on the thyroid gland. Refer Chapter 67 for details of TSH.
- Adrenocorticotropic Hormone (ACTH): ACTH is necessary for the structural integrity and the secretory activity of adrenal cortex. It has other functions also.
- Follicle Stimulating Hormone (FSH): FSH is a glycoprotein made up of one a subunit and a P subunit. The a subunit has 92 amino acids and β subunit has118 amino acids. The half-life of FSH is about 3 to 4 hours.
- Actions in males: In males, FSH acts along with testosterone and accelerates the process of spermiogenesis.
- Actions in females
- It is responsible for the development of graafian follicle from primordial follicle
- It stimulates the theca cells of graafian follicle and causes secretion of estrogen
- Promotes aromatase activity in granulosa cells resulting in conversion of androgens into estrogen.
- Luteinizing Hormone (LH)z: LH is a glycoprotein made up of one a subunit and a p subunit. The a subunit has 92 amino acids and [3 subunit has 141 amino acids. The half-life of LH is about 60 minutes.
- Actions in males
- In males LH is known as interstitial cell-stimulating hormone (ICSH) because it stimulates the interstitial ceils of Leydlg in testes.
- This hormone is essential for the secretion of testosterone from Leydig cells.
- It stimulates the Leydig cells and the quantity of testosterone secreted is directly proportional to the amount of ICSH available.
- Actions in females
- LH causes maturation of vesicular follicle into graafian follicle along with follicle-stimulating hormone
- It induces synthesis of androgens from theca cells of growing follicle
- It is responsible for ovulation
- It is necessary for the formation of corpus luteum
- It activates the secretory functions of the corpus luteum.
- Actions in males
- Prolactin: Prolactin is a single-chain polypeptide with 199 amino acids. Its half-life is about 20 minutes. Prolactin is necessary for the final preparation of mammary glands for production and secretion of milk. Prolactin acts directly on the epithelial cells of mammary glands and causes localized alveolar hyperplasia.
- β Lipotropin: This is a polypeptide hormone with 31 amino acids. It mobilizes fat from adipose tissue and promotes lipolysis. It forms the precursor of endorphins. This hormone acts through the adenyl cyclase.
Posterior Pituitary
Posterior Pituitary Parts: Posterior pituitary consists of three divisions
- The pars nervosa or infundibular process
- Neural stalk or infundibular stem
- The median eminence.
The pars tuberalis of anterior pituitary and the neural stalk of posterior pituitary together form the hypophyseal stalk.
- Posterior Pituitary Development: The posterior pituitary is neuroectodermal in origin. Development of posterior pituitary is explained along with the development of anterior pituitary.
- Posterior Pituitary Histology: Posterior pituitary is made up of neural-type of cells called pituicytes and unmyelinated nerve fibers.
- Pituicytes: Pituicytes are also called glial cells or fusiform cells. These cells have several processes and brown pigment granules. Pituicytes act as supporting cells and do not secrete any hormone.
- Unmyelinated Nerve Fibers: The unmyelinated nerve fibers come from supraoptic and paraventricular nuclei of the hypothalamus through the pituitary stalk.
- Other Structures: Neurohypophysis also has numerous blood vessels, hyaline bodies, neuroglial cells, and mast cells.
Hormones Of Posterior Pituitary: Posterior pituitary hormones are
- Antidiuretic hormone (ADH) or vasopressin
- Oxytocin.
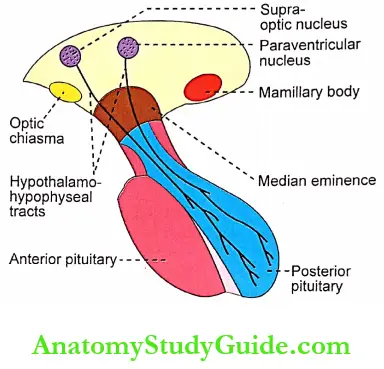
- Actually, the posterior pituitary does not secrete any hormone. ADH and oxytocin are synthesized in the hypothalamus. From the hypothalamus, these two hormones are transported to the posterior pituitary through the nerve fibers of the hypothalamohypophyseal tract by means of axonic flow.
- In the posterior pituitary, these hormones are stored at the nerve endings. Whenever the impulses from the hypothalamus reach the posterior pituitary, these hormones are released from the nerve endings into the circulation. Hence, these two hormones are called neurohormones.
- Experimental Evidence
- The fact that the posterior pituitary hormones are secreted by the hypothalamus and transported to the posterior pituitary is proved by experimental evidence.
- If the pituitary stalk is cut above the pituitary gland, by leaving the entire hypothalamus intact, the hormones drip through the cut end of the nerves in the pituitary stalk. This proves the fact that the hormones are secreted by the hypothalamus.
- Neurophysins:
- Neurophysins are the binding proteins that transport ADH and oxytocin from hypothalamus to the posterior pituitary via the hypothalami-hypophyseal tract and storage of these hormones in posterior pituitary.
- Neurophysin 1 or oxytocin neurophysin is the binding protein for oxytocin and neurophysin 2 or ADH-neurophysin is the binding protein for ADH.
Antidiuretic Hormone
- Source of Secretion:
- ADH is secreted mainly by the supraoptic nucleus of hypothalamus and in small quantity by the paraventricular nucleus.
- From here, this hormone is transported to the posterior pituitary through the nerve fibers of the hypothalamo-hypophyseal tract by means of axonic flow.
- Chemistry and Half-life: Antidiuretic hormone is a polypeptide, containing 9 amino acids. Its half-life is 18-20 minutes.
- Antidiuretic Hormone Actions
- The major function of ADH is retention of water by acting on kidneys. It increases the facultative reabsorption of water from distal convoluted tubule and collecting duct in the kidneys.
- In the absence of ADH, the distal convoluted tubule and collecting duct are totally impermeable to water. So reabsorption of water does not occur in the renal tubules and dilute urine is excreted.
- This leads to loss of large amount of water through urine. This condition is called diabetes insipidus and the excretion of large amount of water is called diuresis.
- Mode of Action on Renal Tubules: ADH increases water reabsorption in the tubular epithelial membrane by regulating the water channel proteins called aquaporins through V2 receptors.
- Vasopressor Action
- In large amount, the ADH shows constrictor action on the blood vessels, particularly the arteries, it constriction of the arteries in all parts of the body. Dm to the vasoconstriction, the blood pressure increases. ADH acts on blood vessels through V1A receptors.
- However, the amount of ADH required to cause this vasopressor effect is greater than the amount required to cause the antidiuretic effect.
- Regulation of Secretion: The secretion of ADH depends upon the volume of body fluid and the osmolarity of the body fluids. The potent stimulants of ADH secretion are:
- Decrease in the ECF volume
- Increase in osmolar concentration in the ECF.
- Role of osmoreceptors
- The osmoreceptors are the receptors, which give response to change in the osmolar concentration of the blood. These receptors are situated in the hypothalamus near supraoptic and paraventricular nuclei.
- When the osmolar concentration of blood increases, the osmoreceptors are activated.
- In turn, the osmoreceptors stimulate the supraoptic and paraventricular nuclei which send motor impulses to posterior pituitary through the nerve fibers and cause the release of ADH.
- ADH causes the reabsorption of water from the renal tubules. So only a small quantity of water with usual solutes is excreted out through the urine. This increases the volume of the ECF and restores the normal osmolarity.
- Role of osmoreceptors
Oxytocin
- Source of Secretion
- Oxytocin is secreted mainly by the paraventricular nucleus and a small quantity is secreted by the supraoptic nucleus in the hypothalamus.
- And it is transported from the hypothalamus to posterior pituitary through the nerve fibers of the hypothalami-hypophyseal tract.
- In the posterior pituitary, oxytocin is stored in the nerve endings of the hypothalami-hypophyseal tract. When suitable stimuli reach the posterior pituitary from the hypothalamus, oxytocin is released into the blood. Oxytocin is secreted in both males and females.
- Chemistry and Half-life: Oxytocin is a polypeptide, having 9 amino acids. It has a half-life about 6 minutes.
- Actions in Females: In females, oxytocin acts on mammary glands and uterus.
- Action of oxytocin on mammary glands
- It causes the ejection of milk from the mammary glands. The fact of the mammary glands are lined by myoepithelial cells. Oxytocin causes contraction of the myoepithelial cells.
- It squeezes the milk from the alveoli of the mammary glands to the exterior through the duct system and nipple. The process by which the milk is ejected from the alveoli of mammary glands is called the milk ejection reflex or milk letdown reflex. It is one of the neuroendocrine reflexes.
- Milk ejection reflex:
- Plenty of touch receptors are present on the mammary glands, particularly around the nipple. When the infant suckles the mother’s nipple, the touch receptors are stimulated and impulses are discharged.
- The impulses from the touch receptors are carried by the somatic afferent nerve fibers and reach the paraventricular and supraoptic nuclei of the hypothalamus.
- Now, the hypothalamus in turn, sends impulses to the posterior pituitary through the nerve fibers of the hypothalami-hypophyseal tract.
- The afferent impulses cause release of oxytocin into the blood. When the hormone reaches the mammary gland, it causes contraction of myoepithelial cells resulting in the ejection of milk from mammary glands.
- As this reflex is initiated by the nervous factors and completed by the hormonal action, it is called a neuroendocrine reflex. During this reflex, a large amount of oxytocin is released by positive feedback mechanism.
- Action on the uterus: Oxytocin acts on the pregnant uterus and nonpregnant uterus.
- On pregnant uterus:
- Oxytocin causes contraction of uterus and helps in the expulsion of fetus. Throughout the period of pregnancy, oxytocin secretion is inhibited by estrogen and progesterone.
- At the end of pregnancy, the secretion of these two hormones decreases suddenly, and the secretion of oxytocin increases.
- During the later stages of pregnancy, the number of receptors for oxytocin increases in the wall of the uterus. Because of this, the uterus becomes more sensitive to oxytocin.
- The secretion of oxytocin increases during labor. At the onset of labor, the cervix dilates, and the fetus descends through the birth canal.
- During the movement of the fetus through the cervix, the receptors on the cervix are stimulated and start discharging large number of impulses.
- The impulses are carried to the paraventricular and supraoptic nuclei of the hypothalamus by the somatic afferent nerve fibers. Now, these two hypothalamic nuclei secrete large quantity of oxytocin, which enhances labor by causing contraction of uterus.
- Throughout labor, large quantity of oxytocin is released by means of a positive feedback mechanism, i.e. oxytocin induces contraction of uterus, which in turn causes the release of more amount of oxytocin.
- The contraction of uterus during labor is also a neuroendocrine reflex. Oxytocin also stimulates the release of prostaglandins in the placenta. The prostaglandins intensify the uterine contraction induced by oxytocin.
- On nonpregnant uterus
- The action of oxytocin on the nonpregnant uterus is to facilitate the transport of sperms through female genital tract up to the fallopian tube by producing the uterine action during sexual intercourse.
- During the sexual intercourse, the receptors in the vagi ire are stimulated. The vaginal receptors generate the which are transmitted by somatic afferent nerves to the paraventricular and supraoptic nuclei of hypothalamus.
- When these two nuclei are stimulated, oxytocin is released, and transported by blood. While reaching the female genital tract, the hormone causes antiperistaltic contractions of uterus towards the fallopian tube, it is also a neuroendocrine reflex.
- The sensitivity of the uterus to oxytocin is accelerated by estrogen and decreased by progesterone.
- Action of oxytocin on mammary glands

- Action in Males: In males, the release of oxytocin increases during ejaculation. It facilitates the release of sperm into urethra by causing the contraction of smooth muscle fibers in the reproductive tract, particularly the vas deferens.
- Mode of Action of Oxytocin: Oxytocin acts on mammary glands and the uterus by activating G protein-coupled oxytocin receptor.
Applied Physiology Disorders Of Pituitary Gland
Disorders of endocrine gland occur either because of hyperactivity with increased secretion of the hormones or hypoactivity of the gland with decreased secretion of hormones. The disorders of pituitary gland are qiven in Table.

Hyperactivity Of Anterior Pituitary
1. Gigantism: Gigantism is a pituitary disorder characterized by excess growth of the body. The subjects look like giants with average height of about 7-8 feet.
- Gigantism Causes: Gigantism is due to hypersecretion of GH in childhood or in the pre-adult life before the fusion of epiphysis of bone with the shaft. Hypersecretion of GH is because of tumor of acidophil cells in the anterior pituitary.
- Gigantism Signs and symptoms:
- The general overgrowth of the person leads to the development of a huge stature with a height of more than 7 or 8 feet. The limbs are disproportionately long
- The giants are hyperglycemic and they develop glycosuria and pituitary diabetes. Hyperglycemia causes constant stimulation of (3 cells of islets of Langerhans in the pancreas and release of insulin. However, the overactivity of (3 cells of Langerhans in the pancreas leads to degeneration of these cells and deficiency of insulin. And, ultimately diabetes mellitus is developed
- The tumor of the pituitary gland itself causes constant headache
- Pituitary tumor also causes visual disturbances. It compresses the lateral fibers of optic chiasma leading to bitemporal hemianopia
- In most of cases, gigantism ends in hypopituitarism because of burning out of cells of anterior pituitary.
2. Acromegaly: It is a disorder characterized by the enlargement, thickening and broadening of bones, particularly in the extremities of the body.
- Acromegaly Cause: Acromegaly is due to the hypersecretion of GH in adults after the fusion of epiphysis with the shaft of the bone. Hypersecretion of GH is due to adenomatous tumor of anterior pituitary involving the acidophil cells.
- Acromegaly Signs and symptoms
- The striking facial features are. protrusion of supraorbital ridges, broadening of nose, thickening of lips, thickening, and wrinkles formation on the forehead, and protrusion of lower jaw (prognathism). The face with these features is called an acromegalic or guerrilla face
- Another characteristic feature of this disorder is the enlargement of hands and feet with bowing of spine called kyphosis
- The scalp is thickened and thrown into folds or wrinkles like a bulldog scalp. There is general overgrowth of body hair
- The visceral organs such as the lungs, thymus, heart, liver, and spleen are enlarged
- The thyroid gland, parathyroid glands, and adrenal glands show hyperactivity
- Hyperglycemia and glucosuria occur resulting in diabetes mellitus
- Hypertension
- Headache
- Visual disturbances – bitemporal hemianopia.
3. Acromegalic Gigantism: It is a rare disorder with symptoms of both gigantism and acromegaly. Hypersecretion of GH in children, before the fusion of epiphysis with shaft of the bones causes gigantism. And, if hypersecretion of the GH is continued even after the fusion of epiphysis, the symptoms of acromegaly also appear.



4. Cushing’s Disease: It is also a rare disease characterized by obesity.
- Cushing’s Disease Causes
- Cushing’s disease is because of basophilic adenoma of adenohypophysis. It increases the secretion of adrenocorticotropic hormone, which, in turn stimulates the adrenal cortex to release cortisol.
- It is also developed by hyperplasia or tumor of adrenal cortex. Usually, the disorder due to the pituitary cause is called Cushing’s disease, and when it is due to the adrenal cause, it is called Cushing’s syndrome.
Hyfoactivity Of Anterior Pituitary
1. Dwarfism: It is a pituitary disorder in children characterized by stunted growth.
- Dwarfism Causes: Reduction in the GH secretion in infancy or early childhood causes dwarfism. It occurs because of the following reasons:
- Deficiency of GH-releasing hormone from hypothalamus
- Deficiency of somatomedin-C
- Atrophy or degeneration of acidophilic cells in the anterior pituitary
- Tumor of chromophobes: It is a nonfunctioning tumor, which compresses and destroys the normal cells secreting the GH. It is the most common cause for hyposecretion of GH leading to dwarfism
- Panhypopituitarism: In this condition, there is reduction in the secretion of all the hormones of the anterior pituitary gland. This type of dwarfism is associated with other symptoms due to the deficiency of other anterior pituitary hormones.
- Dwarfism Signs and symptoms
- The primary symptom of hypopituitarism in children is the stunted skeletal growth. The maximum height of anterior pituitary dwarf at the adult age is only about 3 feet
- But the proportions of different parts of the body are almost normal. Only, the head becomes slightly larger in relation to the body
- Pituitary dwarfs do not show any deformity and their mental activity is normal with no mental retardation
- Reproductive function is not affected, if there is only GH deficiency. However, in panhypopituitarism, the dwarfs do not obtain puberty due to a deficiency of gonadotropic hormones.
- Laron dwarfism
- Laron dwarfism is a genetic disorder. It is also called GH insensitivity. It occurs due to the presence of abnormal growth hormone secretagogue receptors in liver.
- GHS receptors become abnormal because of the matador of genes for the receptors.
- The GH secretion is normal or high. But the hormone cannot stimulate growth because of the abnormal GHL receptors. So dwarfism occurs.
- Psychogenic dwarfism: Dwarfism occurs if the child is exposed to extreme emotional deprivation or stress. The short stature is because of a deficiency of GH. This type of dwarfism is called psychogenic dwarfism, psychosocial dwarfism or stress dwarfism.
- Dwarfism in dystrophia adiposogenitalis: Dystrophia adiposogenitalis or Frohlich’s syndrome is a pituitary disorder. Dwarfism occurs if it develops in children.
2. Acromicria: It is a rare disease in adults characterized by the atrophy of the extremities of the body.
- Acromicria Causes: Deficiency of GH in adults causes acromicria. The secretion of GH decreases in the following conditions:
- Deficiency of GH-releasing hormone from the hypothalamus
- Atrophy or degeneration of acidophilic cells in the anterior pituitary
- Tumor of chromophobes: It is a nonfunctioning tumor, which compresses and destroys the normal cells secreting the GH. This is the most common cause for hyposecretion of GH leading to acromicria
- Panhypopituitarism: In this condition, there is reduction in the secretion of all the hormones of anterior pituitary gland. Acromicria is associated with other symptoms due to the deficiency of other anterior pituitary hormones.
- Acromicria Signs and Symptoms
- Atrophy and thinning of extremities of the body, (hands and feet) are the major symptoms in acromicria
- Acromicria is mostly associated with hypothyroidism
- Hyposecretion of adrenocortical hormones also is common in acromicria
- The person becomes lethargic and obese
- There is loss of sexual functions.
3. Simmond’s Disease: It is a rare pituitary disease. It is also called pituitary cachexia.
- Simmond’s Disease Cause: it occurs mostly in panhypopituitarism, i.e. hyposecretion of ail the anterior pituitary hormones due to the atrophy or degeneration of anterior pituitary.
- Simmond’s Disease Symptoms
- A major feature of Simmond’s disease is the rapidly developing senile decay. Thus, a 30 years old person looks like a 60 years old person. The senile decay is mainly due to a deficiency of hormones from target glands of the anterior pituitary,
i.e. the thyroid gland, adrenal cortex, and the gonads - There is a loss of hair over the body and loss of teeth
- The skin on face becomes dry and wrinkled. So, there is a shrunken appearance of facial features. It is the most common feature of this disease.
- A major feature of Simmond’s disease is the rapidly developing senile decay. Thus, a 30 years old person looks like a 60 years old person. The senile decay is mainly due to a deficiency of hormones from target glands of the anterior pituitary,
Hyperactivity Of Posterior Pituitary
- Syndrome of Inappropriate Hypersecretion of Antidiuretic Hormone (SIADH): SIADH is the disease characterized by loss of sodium through urine due to hypersecretion of ADH.
- Simmond’s Disease Cause
- It occurs due to cerebral tumors, lung tumors, and lung cancers because the tumor cells and cancer cells secrete ADH.
- In normal conditions, ADH decreases the urine output by facultative reabsorption of water in distal convoluted tubule and the collecting duct.
- The urine that is formed is concentrated with sodium and other ions. Loss of sodium decreases the osmolarity of plasma making it hypotonic. The hypotonic plasma inhibits ADH secretion resulting in the restoration of plasma osmolarity.
- However, in SIADH secretion of ADH from tumor or cancer cells is not inhibited by hypotonic plasma. So there is continuous loss of sodium resulting in persistent plasma hypotonicity.
- Simmond’s Disease Signs and symptoms
- Loss of appetite
- Weight loss
- Nausea and vomiting
- Headache
- Muscle weakness, spasm, and cramps
- Fatigue
- Restlessness and irritability
In severe conditions, the patients die because of convulsions and coma.
Hypo Activity Of Posterior Pituitary
- Diabetes Insipidus: Diabetes insipidus is a posterior pituitary disorder characterized by excess excretion of water through urine.
- Diabetes Insipidus Causes: This disorder develops due to the deficiency ADH which occurs in the following conditions
- Lesion (injury) or degeneration of supraoptic and paraventricular nuclei of the hypothalamus
- Lesion in the hypothalami-hypophyseal tract
- Atrophy of posterior pituitary
- Inability of renal tubules to give response to ADH hormone. Such a condition is called nephrogenic diabetic insipidus.
- Diabetes Insipidus Signs and Symptoms
- Polyuria: Excretion of large quantity of dilute urine with increased frequency of voiding is called polyuria. The daily output of urine varies between 412 liters. In the absence of ADH, the epithelial cells of distal convoluted tubule in the nephron and the collecting duct of the kidney become impermeable to water. So, water is not reabsorbed from the renal tubule and collecting duct leading to loss of water through urine.
- Polydipsia: Intake of excess water is called polydipsia. Because of polyuria, lot of water is lost from the body. It stimulates the thirst center in the hypothalamus resulting in intake of large quantity of water.
- Dehydration: In some cases, the thirst center in the hypothalamus is also affected by the lesion. Water intake decreases in these patients and, the loss of water through urine is not compensated. So, dehydration develops which may lead to death.
Nephrogenic diabetes insipidus: It is a genetic disorder due to the inability of renal tubules to give response to ADH. It is caused by mutations of genes of V2 receptors or aquaporin 2.
Hypoactivityof Anterior And Posterior Pituitary
- Dystrophia Adiposogenitalis: Dystrophia adiposogenitalis is a disease characterized by obesity and hypogonadism affecting mainly the adolescent boys. It is also called Frohlich’s syndrome or hypothalamic eunuchism.
- Dystrophia Adiposogenitalis Causes: It is due to the hypoactivity of both anterior pituitary and posterior pituitary. The common cause of this disease is the tumor in the pituitary gland and hypothalamic regions concerned with food intake and gonadal development. Other causes are injury or atrophy of pituitary gland and the genetic inability of the hypothalamus to secrete luteinizing hormone-releasing hormone.
- Dystrophia Adiposogenitalis Symptoms
- Obesity is a common feature of this disorder. Due to the abnormal stimulation of feeding center, the person overeats and consequently becomes obese.
- Obesity is accompanied by sexual infantilism (failure to develop secondary sexual characters) or eunuchism. Dwarfism occurs if the disease starts in growing age. In children, it is called infantile or prepubertal type of Frohlich’s syndrome.
- This disease develops in adults also. When it occurs in adults, it is called adult type of Frohlich’s syndrome. In adults, the major symptoms are obesity and atrophy of sex organs.
- Other features of this disorder are behavioral changes and loss of vision. Some patients develop diabetes insipidus.
Leave a Reply