The Placenta Implantation
Placenta Introduction: The process by which blastocyst gets embedded in the endometrium is called implantation.
Table of Contents
1. Time: On 7th day after fertilization.
2. Site: Endometrium of posterior wall of fundus of uterus.
Read And Learn More: General Histology Question And Answers
3. Cells: The responsible cells are cells of the trophoblast. They have the property of adhesion, invasion, and erosion.
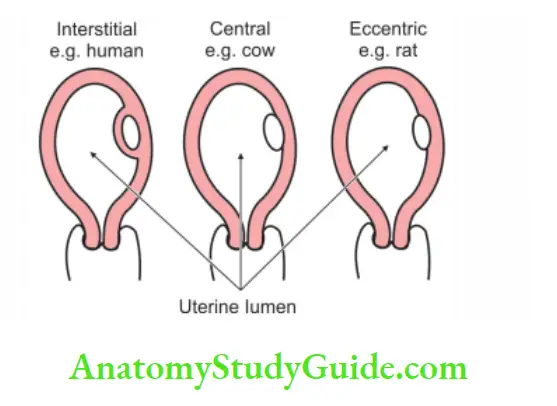
4. Types of implantation are
1. Interstitial: The blastocyst is embedded into stratum compactum of the endometrium.
For example Humans.
2. Central: The blastocyst is embedded in the cavity of uterus
For example Cow.
3. Eccentric: The blastocyst is embedded in the crypts of uterus
For example Rat
5. Placenta Pre-requisite:
- Dissolution of zona pellucida.
- Preparation of the endometrium. It is facilitated by progesterone, which is secreted by corpus luteum. This is called decidual reaction.
6. Placenta Actual process:
- The zona pellucida disappears.
- The trophoblast adheres to the endometrium.
- The trophoblast penetrates the endometrium by proteolytic action.
- The cells of the trophoblast proliferate.
7. Placenta Results of implantation:
1. Trophoblast differentiates into two layers
- Cytotrophoblast, and
- Syncytiotrophoblast.
2. Inner cell mass differentiates into epiblast cells, hypoblast cells with amniotic cavity, and yolk sac cavity.
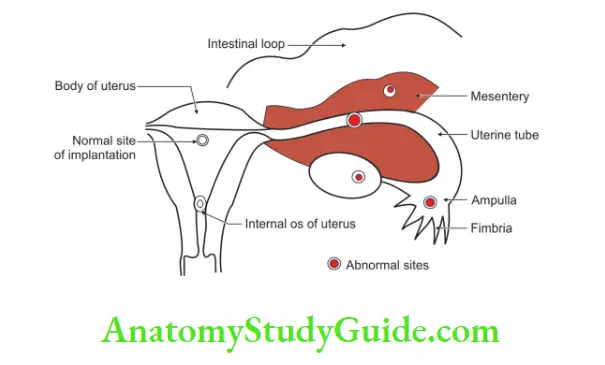
8. Placenta Abnormal sites of implantation of the ovum:
1. Implantation within the uterus:
1. Placenta praevia (prae—in front): The placenta is attached to the lower uterine segment completely or partially. It is characterized by painless hemorrhage in last trimester particularly in the 8th month of pregnancy.
2. Implantation outside the uterus:
- Tubal
- Cervical
- Peritoneal, and
- Ovarian
Excessive or deeper implantation results in postpartum hae morrhage.
9. Placenta Applied anatomy:
- Placenta accreta: It is abnormal adherence of part or whole placenta to the uterine wall. It may or may not have decidua basalis.
- Placenta increta: Placenta accreta with penetration of myometrium is called placenta increta.
- Placenta percreta: Placenta accreta with invasion of the myometrium and peritoneal cavity. It may invade other structures such as bladder.
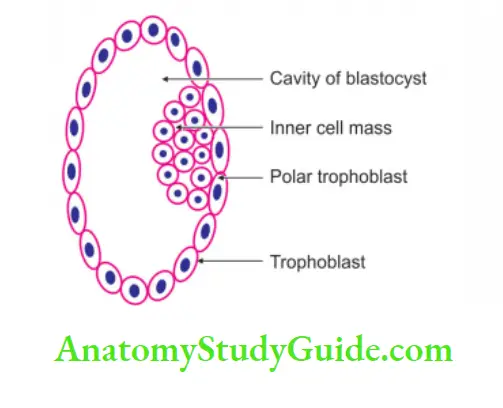
Blastocyst
Blastocyst Introduction: A blastula having a fluid-filled cavity is called blastocyst .
1. Chronological age: It is formed between 4th to 5th day of fertilization.
2. Parts:
- Blastocoele, and
- Inner cell mass (embryoblast).
- Trophoblast.
3. Blastocyst Formation: Cells of morula are of two types.
1. Cells forming the embryoblast: They give rise to embryo proper.
2. Trophoblast cells: These are subdivided into
- Polar cells: They give rise to chorion frondosum.
- Mural cells: They give chorion laeve. The cavity of the blastocyst is called blastocoele.
Decidua
Decidua Introduction: The uterine endometrium after implantation is called decidua.
1. Decidual reaction: After implantation, the endometrial glands accumulate glycogen and lipid secretion and this is called decidual reaction.
2. Decidua Following changes occur:
- Nuclei becomes rounded.
- The number of cytoplasmic organelle increases.
- The volume of the cytoplasm increases.
- The vascularity of the cell increases
3. Hormones responsible for the changes are:
- Progesterone
- HCG (human chorionic gonadotropin).
4. Decidua Functions:
- It gives mechanical support to the fertilized ovum and forms a suitable site for implantation.
- It provides nutrition to blastocyst.
- The decidua basalis forms maternal part of placenta and takes temporary function of placenta.
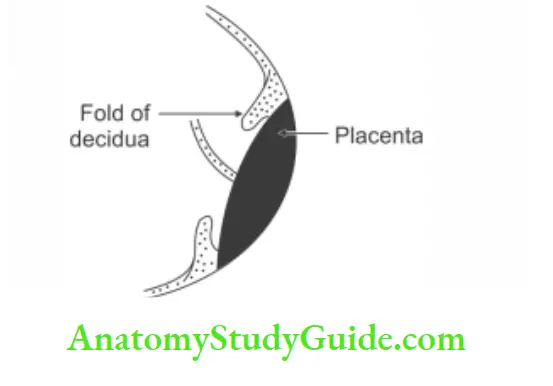
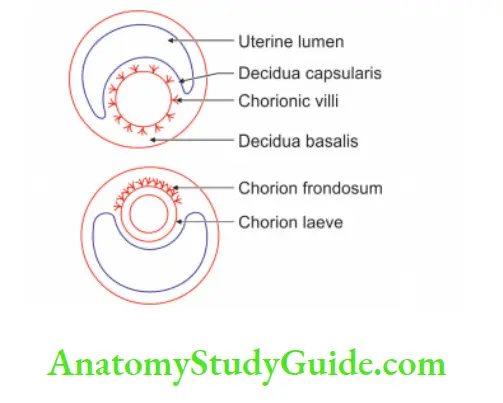
5. Parts of decidua:
- Decidua basalis: The portion of the decidua where the placenta is to be formed is called decidua basalis. It is deep to the developing blastocyst.
- Decidua capsularis: The part of the decidua that separates the embryo from the uterine lumen is called decidua capsularis.
- Decidua parietalis: The part lining rest of uterine cavity is called decidua parietalis.
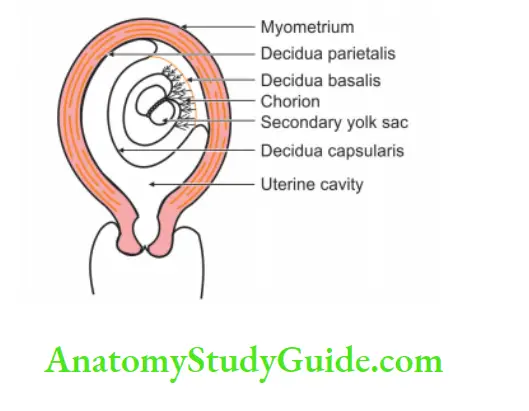
6. Decidua Fate:
1. The decidua basalis undergoes marked development and forms the maternal surface of placenta.
2. The decidua capsularis and parietalis are stretched and are fused with each other. It undergoes
- Atrophy. With the increase in size of amniotic cavity following changes occur.
- The extra-embryonic coelom obliterates.
- The amnion fuses with chorion.
- The amnio-chorionic membrane (chorion laevae) fuses with decidua capsularis.
3. The decidua capsularis disintegrates and fuses with decidua parietalis and obliterates the uterine cavity. At the time of delivery, placenta separates with decidua basalis and parietalis and is delivered.
Placenta
Placenta Introduction: The placenta is an important fetal membrane. It acts as a temporary endocrine gland and maintains the pregnancy after 1st trimester.
The placenta is a structure by which the fetus is attached to the mother and it gives nutrition to the embryo (or fetus) and excretes waste products from fetus to mother.
1. Formation: The placenta is formed from both fetal and maternal sources. The fetal source is chorion frondosum and the maternal source is decidua basalis.
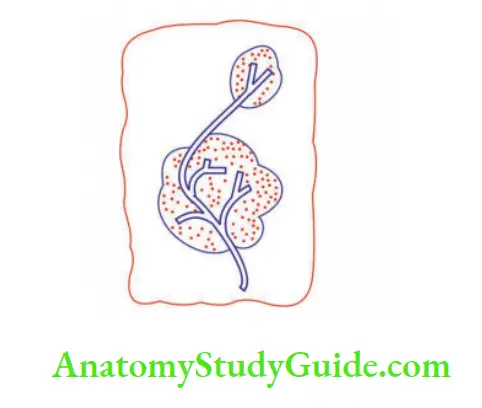
1. Formation of chorion frondosum: It follows the following stages
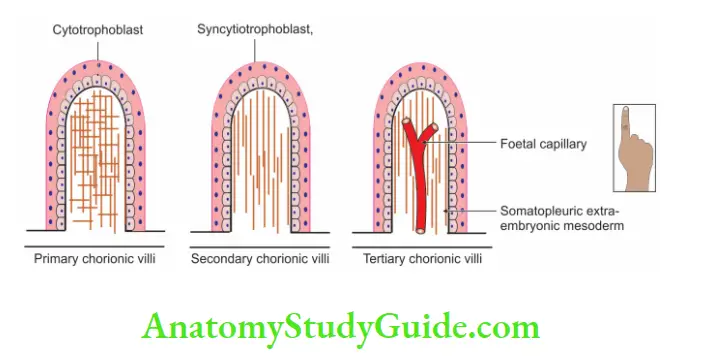
Primary stem villi: By the beginning of the 3rd week, a Cytotrophoblastic core is covered by a syncytiotrophoblastic layer and thus forms primary stem villi.
Secondary stem villi: Mesodermal core penetrates the primary stem villi and thus forms secondary stem villi.
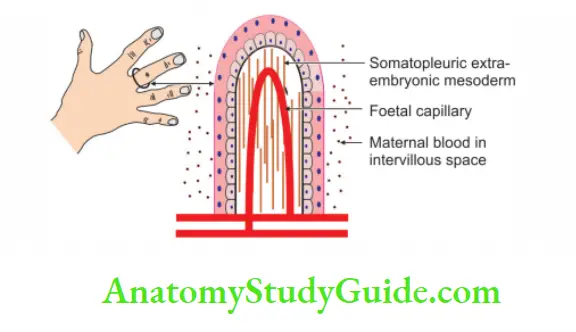
Tertiary stem villi: The blood vessels appear in the mesoderm of secondary villi to form tertiary villi. These vessels establish contact with the intra-embryonic circulatory system.
Cytotrophoblastic shell: The cytotrophoblast emerges through the syncytium of each villus until it reaches the maternal decidua where it spreads out to form a layer.
Thus, the shell is formed. The cytotrophoblastic shell gradually surrounds the syncytiotrophoblast entirely and attaches the chorionic sac firmly to maternal endometrial tissue.
Between the villi: Numerous intervillous spaces are formed. The villi on the embryonic pole continue to grow and expand and thus give rise to chorion frondosum. (The villi on the abembryonic pole degenerate and are called chorion larvae).
2. Decidua basalis: The decidua over the chorion frondosum is called decidua basalis. Chorion frondosum and decidua basalis together form the placenta.
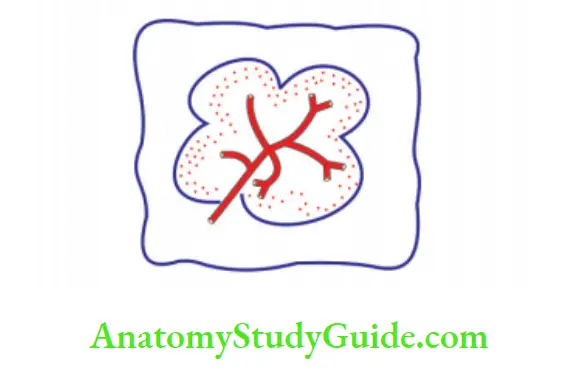
3. Placenta: The Placenta becomes subdivided into a number of lobes by septa that grow into the intervillous spaces from the maternal side. Each such lobe of the placenta is often called a maternal cotyledon.
If the placenta is viewed from the maternal side, the bases of the septa are seen as grooves, while the cotyledons appear as convex areas bounded by the grooves.
Each lobe contains the number of anchoring villi and their branches. One such villus and its branches constitute fetal cotyledon. The placenta then forms a compact mass. Structures found in the cut section of the placenta are
- Amnion
- Chorion
- Choriodecidual space
- Cotyledons
2. Placenta Attachment:
The placenta is attached mostly to the upper part of the posterior wall of the uterus.
3. Placenta Dimensions: At full term.
- Weight: 500-600 g.
- Diameter: 15-25 cm.
- Thickness: 3 cm
4. Functions of placenta:
1. It exchanges:
- Respiratory gases, i.e. O2 and CO2 between fetal and maternal blood.
- Nutrients and metabolic waste products between the fetus and the mother.
2. It transfers:
- Maternal antibodies to the fetus.
- Drug from mother to fetus.
3. It synthesizes the following hormones:
- Human chorionic gonadotropin (HCG).
- Somatotropic hormone.
- Estrogen
- Estradiol.
- Progesterone
- Relaxin
4. It detoxifies the toxic substances.
5. It connects the fetus to the mother.
5. Placenta Types:
The placenta may be of the following types
1. According to the position of the placenta:
- Placenta parietalis: When the placenta lies on the other walls of the uterus than the fundus.
- Placenta praevia.
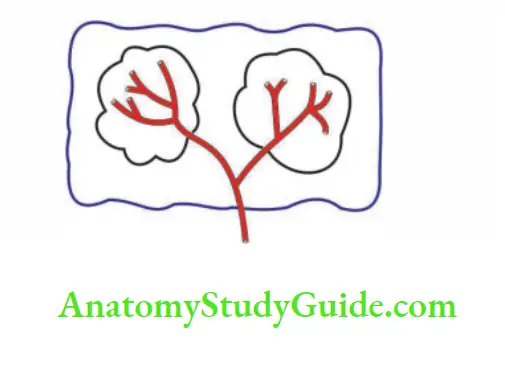
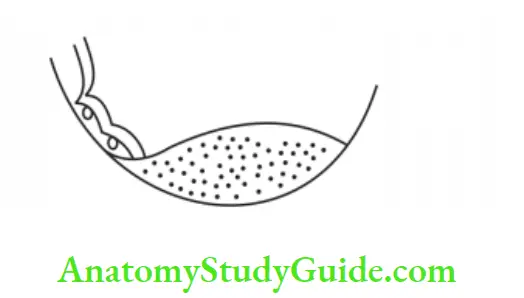
2. According to shape:
1. Discoid
![]()
2. Bilobed
![]()
3. Multilobed
![]()
4. Circumvallate, and
5. Placenta succenturiate (succenturiate—substitute).
3. According to the attachment of the umbilical cord:
- Marginal
- Velamentous
- Furcate, and
- Central.
6. Placenta Anomalies:
1. Hydatidiform or vesicular mole: It results from pathological overactivity of the trophoblast. It is simple, noninvasive new growth.
2. Chorioepithelioma: It is a highly malignant tumor. It results when the endometrium is too resistant to blastocyst.
Types of Placenta Depending upon Shape
1. Lobed: When the placenta is divided into lobes.
2. Bidiscoidal: It consists of the two discs.
3. Circumvallate: The peripheral margin of the placenta is surrounded by a sulcus and overlapped by a circular fold of decidua.
4. Placenta succenturiate: A small placenta is connected with the main placenta by blood vessels and membranes.
Types of Placenta Depending Upon Attachments
According to attachments of the umbilical cord
1. Marginal: When the umbilical cord is attached close to the margin of the placenta. This type of placenta is called battledore placenta. (Battledore racket used to strike the shuttle cock in play.)
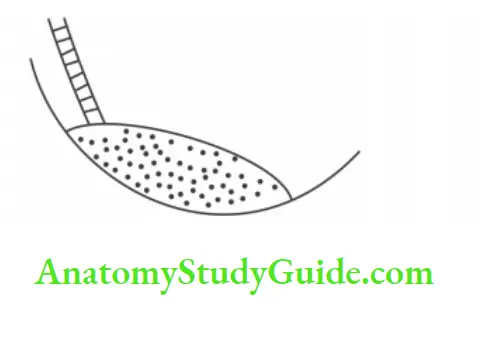
2. Velamentous (membranous or veil-like): When the cord fails to reach the placenta and is attached to the fetal membrane close to the periphery of the organ.
3. Furcate (furca—fork): When the blood vessels divide before reaching the placenta
4. Central: When the cord is attached nearer the center. This is a normal type.
Placenta Praevia
Placenta Praevia Introduction: Implantation of the placenta in the lower uterine segment is called placenta praevia.
1. Degrees of placenta praevia:
Degrees of placenta praevia – First degree: The attachment of the placenta extends into the lower uterine segment but does not reach the internal os.
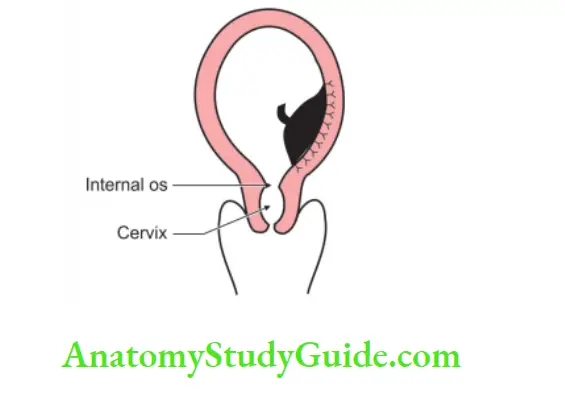
Degrees of placenta praevia – Second degree: The margin of the placenta reaches the internal os but does not cover it.
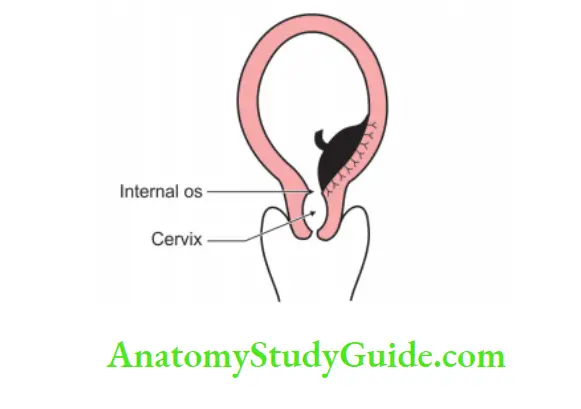
Degrees of placenta praevia – Third degree: The edge of the placenta covers the internal os, but when the os dilates during child-birth, the placenta does not occlude it
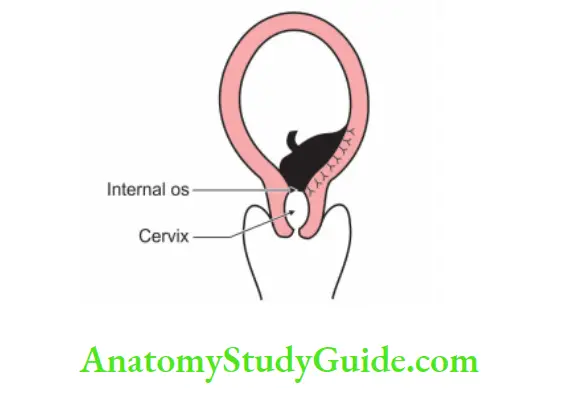
Degrees of placenta praevia – Fourth degree: The placenta completely covers the internal os and occludes the os even after it has dilated
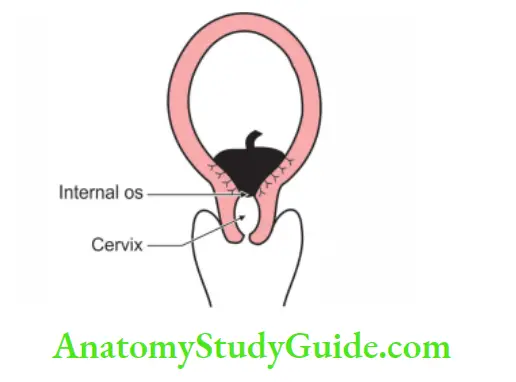
2. Incidence: 1: 200
3. Clinical features: Painless hemorrhage in the last trimester particularly in the 8th month is a diagnostic feature of placenta praevia. It is common in the 3rd and 4th degree of placenta praevia.
Chorion (Chorion—skin)
Chorion Introduction: The structures that cover the conceptus are called chorion They resemble skin. It develops from the cells of the trophoblast.
1. Formation: It is formed by:
- Trophoblast
- Somatopleuric extra-embryonic mesoderm.
2. Villi: Villi are formed as offshoots from the surface of the trophoblast. Villi arising from chorion are called chorionic villi. They grow into the surrounding decidua. They are of two types
Temporary: These are related to decidua capsularis and are called chorionic larvae.
Permanent: They are present in the decidua basalis and are called chorion frondosum (bearing villi). They undergo considerable development and form a disc Q-shaped mass called a placenta.
3. Chorionic villi can be subdivided into:
1. Depending upon the constituent of the villi:
Primary chorionic villi consist of
- Cytotrophoblast.
- Syncytiotrophoblast.
Secondary chorionic villi consist of
- Cytotrophoblast.
- Syncytiotrophoblast.
- Primary extra-embryonic mesoderm.
At the end of 3rd week, secondary villi are converted into tertiary villi.
Tertiary chorionic villi consist of
- Cytotrophoblast.
- Syncytiotrophoblast.
- Primary extra-embryonic mesoderm.
- Fetal blood capillaries.
2. According to the branching pattern, the villi may be:
- Truncus chore: Stem
- Rami chore: Branches
- Ramuli chorii: Finer branches—Ramuli are attached to the cytotrophoblastic shell.
4. Anomalies:
1. Hydatidiform or vesicular mole : (Hydatidiform resembling hydatid cyst, hydatid a drop of water) results from pathological overactivity of the trophoblast. It is simple, non-invasive new growth. This is because of the failure of vascularization of the placental villi.
Most moles are benign but 15% invade and destroy myometrium.
Incidence 1: 2000
The diagnosis of the hydatidiform mole is made by
- The estimation of high levels of chorionic gonadotrophin hormone, and
- Ultrasonography reveals the absence of an embryo.
Treatment: It does not abort spontaneously. It must be removed surgically.
2. Chorioepithelioma: It is a highly malignant tumor. It results when the endometrium is too resistant to blastocyst. It consists of the uncontrolled proliferation of cytotrophoblastic cells resulting in disorganized masses of invasive tissue. There is rapid metastasis to many other organs, including the lungs and brain.
The Maternal-Fetal Barrier
1. The maternal-fetal barrier consists of several structures separating maternal and fetal blood.
The structures forming placental barrier are:
Maternal structures:
- Maternal erythrocyte membrane
- Maternal blood
Placental structures:
- Syncytiotrophoblast
- Cytotrophoblast
- Cytotrophoblast basement membrane
- Villous connective tissue
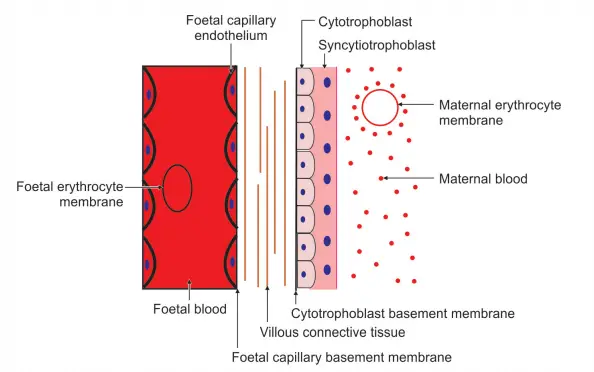
Fetal structures:
- Fetal capillary basement membrane
- Fetal capillary endothelium
- Fetal blood, and
- Fetal erythrocyte membrane.
2. As the placenta grows: The nature of the barrier between maternal and fetal blood also changes.
This barrier is reduced in various ways
1. The cytotrophoblast continuously divides and fuses to form the syncytiotrophoblast. It is no longer present as a barrier to diffusion.
2. The connective tissue stroma becomes spongier.
3. The fetal blood vessels migrate from the center of the villi toward the periphery. They displace intervening connective tissue elements.
3. The end result: The barrier between fetal and maternal blood is hardly 1 pm thick.
4. Maternal-Fetal Barrier Applied anatomy:
- Immunity from mother to fetus.
- Protection of fetus from syphilis in 1st trimester.
Leave a Reply