Kidney and Ureter
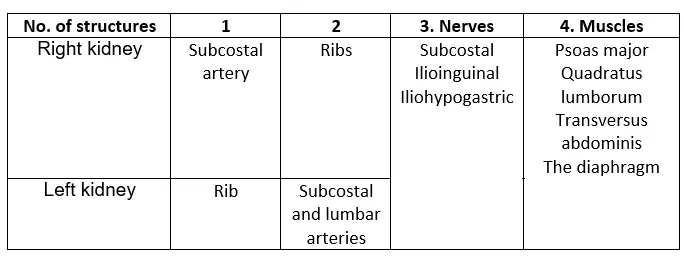
Question – 1: Name the nerves related to the Posterior Surface Of The Kidney
Table of Contents
Answer:
There are three nerves related to the posterior surface of the kidney
1. Iliohypogastric
2. Ilioinguinal and
3. Subcostal.
Read And Learn More: General Histology Question And Answers
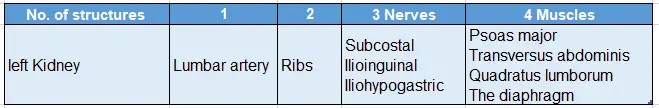
Question – 2: Give the relations of the posterior surface of left kidney
Answer:
Posterior surface: Costodiaphragmatic recess of the pleura is the most important relationship on the posterior surface of left kidney.
Other structures related on the posterior surface of left kidney
Vascular segments of the kidney
The renal artery gives five segmental branches, four from its anterior division and one from its posterior division.
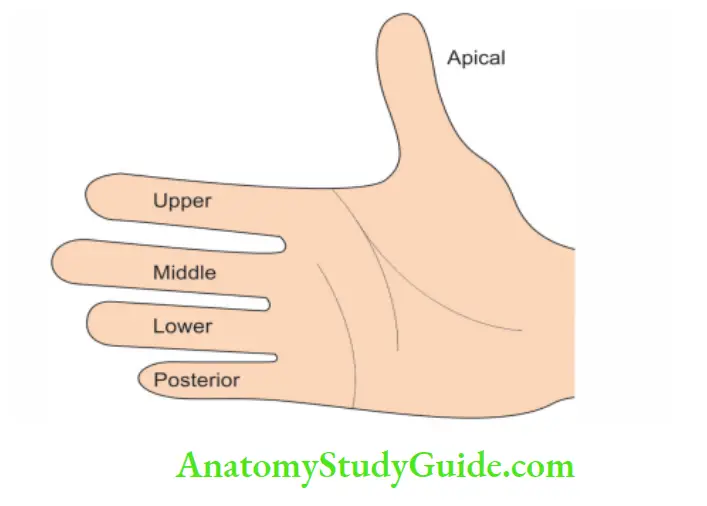
The segments on the anterior aspect are:
- Apical
- Upper
- Middle, and
- Lower on the anterior aspect.
On the posterior aspect, the segments are:
- Posterior
- Apical, and
- Lower segments.
Psoas major
1. Proximal attachments:
From the anterior surface and lower border of all lumbar vertebrae by 5 slips. Each slip arises from
The lateral surface of the bodies of two adjacent vertebrae, and
Intervertebral disc from T12 to L1 vertebrae.
2. Distal attachments: Tip and medial part of the anterior surface of the lesser trochanter of the femur.
3. Nerve supply: Branches of roots of spinal nerve L2, L3 and L4.
4. Action:
It is a strong flexor of the hip joint. It raises the trunk from a recumbent to a sitting position.
Maintains the stability of hip joint.
When acting alone, it brings lateral rotation of the same side.
5. Applied anatomy:
(Accumulation of pus or blood in the psoas sheath may compress the femoral nerve
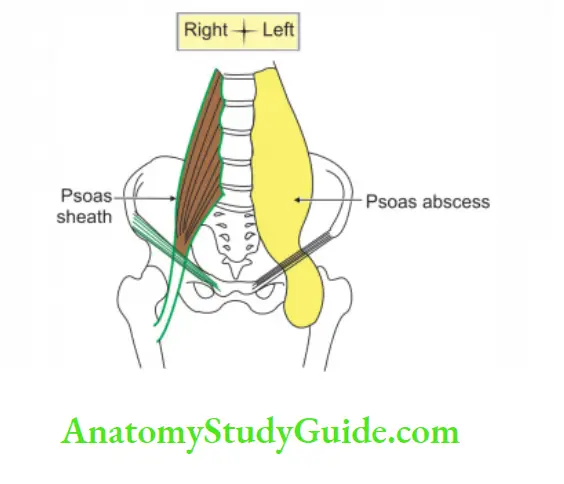 The right side shows normal psoas sheath. The left psoas sheath is distended with pus. It tracks under the inguinal ligament and is seen in the groin
The right side shows normal psoas sheath. The left psoas sheath is distended with pus. It tracks under the inguinal ligament and is seen in the groin
Renal angle
1. Definition: It is the angle between
The Lower margin of 12th rib, and
The outer border of erector spinae.
2. Posterior relation: Lower part of respective kidney.
3. Applied anatomy
- Pain arising from the kidney is dull aching.
- The pain of ureteric calculus begins at renal angle and radiates to the tip of urethra.
- The perinephric abscess causes swelling and tenderness at the renal angle.
- The kidney is approached by lumbar route. The incision should begin below the renal angle.
Floating kidney
1. Following structures support the kidney:
- Fatty capsule
- Fascial capsules
- Renal vessels
In the absence of a fatty capsule, the weight of the kidney is borne by the renal pedicle. It results into falling down the kidney and called a floating kidney.
2. The hypermobility of the kidney is called a floating kidney. The kidney is moved in a vertical plane not in horizontal plane.
3. Extreme degree of mobility makes the kidney pedunculated. The pedicle consists of double layer of peritoneum enclosing the renal vessels and nerves and ureters.
4. In operating the floating kidney, one should avoid opening the kidney in the peritoneal cavity. One should free the peritoneum before dissecting inward and forward.
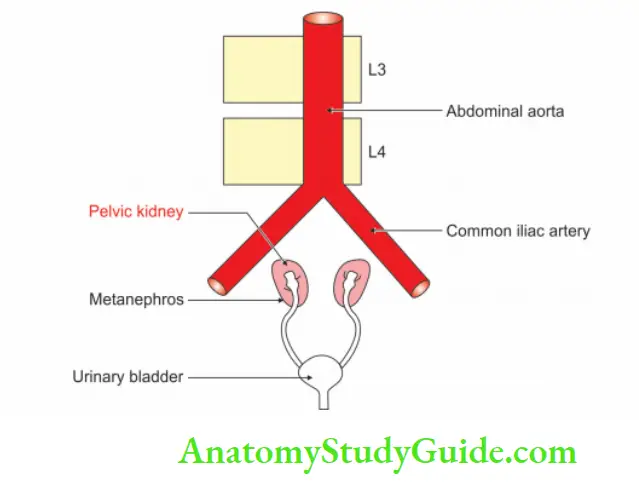
Pelvic kidney
1. Kidney present in the pelvic region is called the pelvic kidney
2. It is due to failure to ascend in the abdomen.
3. The commonest cause: It is due to the folding of the peritoneum projecting from the lateral pelvic wall. It prevents the ascent of the kidney.
4. Complications: Pelvic kidney has
- Abnormal position of the ureter, and
- Anomalous blood supply.
- It results in hydronephrosis
Renal fascia
Question 3: Describe the kidney under the following heads
1. Gross anatomy
2. Histology
3. Development, and
4. Applied anatomy.
Answer:
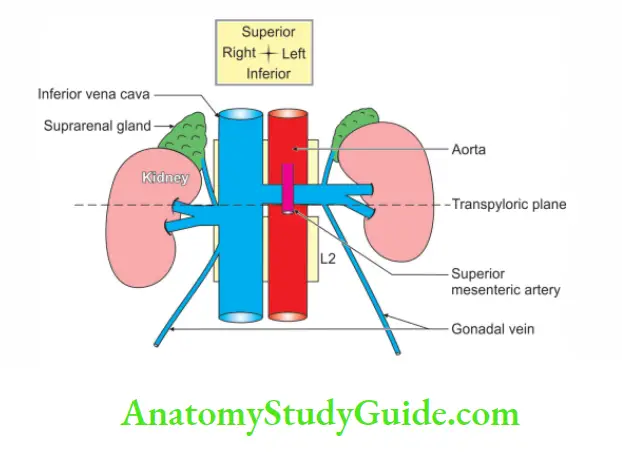
Introduction: Kidneys are the paired excretory organs present behind the peritoneum in the lumbar region.
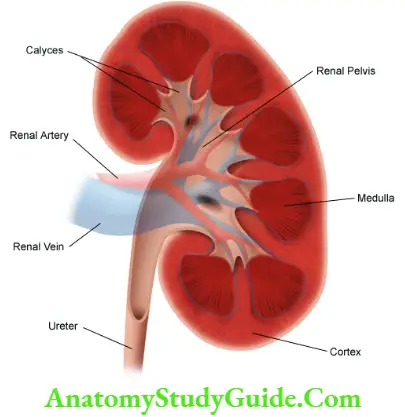
1. Gross anatomy
1. Shape: Bean ![]() shape.
shape.
Location: Kidneys are present in the epigastric, hypochondriac, lumbar and umbilical regions.
Extent: They extend from the upper border of vertebra T12 to the centre of vertebra L3. The left kidney is slightly higher level than the right kidney.
- Dimension:
- Thickness: 1″
- Width: 2″
- Coverings: 3 Length: 4″
- Weight: 5_ounces, i.e. 150 g.
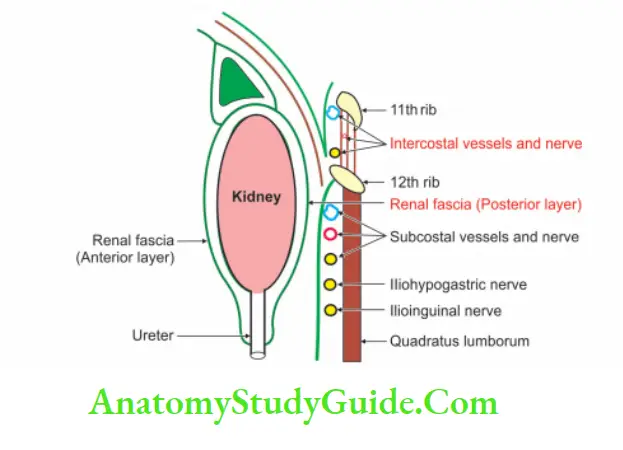
2. External features Coverings: There are three coverings
Fibrous capsule (true capsule):
1. Features:
- The fibrous capsule is a thin membrane.
- It closely invests the kidney. It lines the renal sinus.
2. Applied: Normally it can easily be stripped off from the kidney, but in certain diseases, it becomes adherent and cannot be stripped.
Fatty layer:
- Perirenal (perinephric) fat.
- It is formed by adipose tissue.
- It is present outside the fibrous capsule.
- It is thickest at the borders.
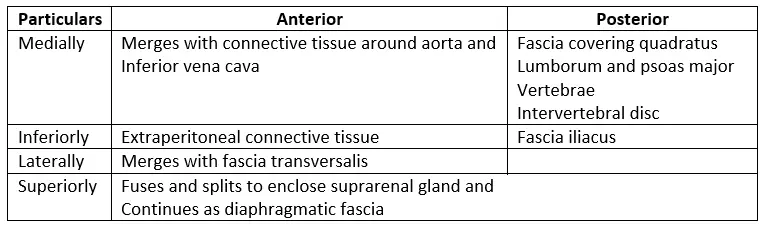
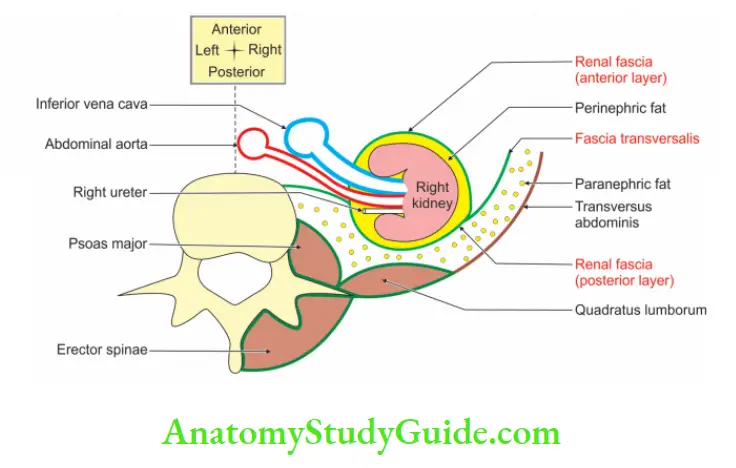
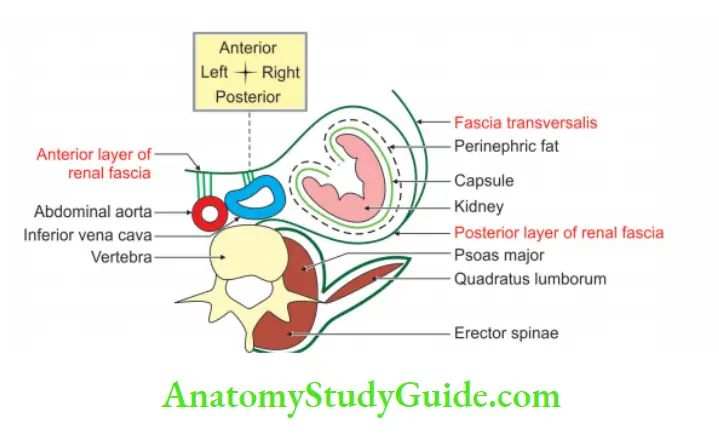
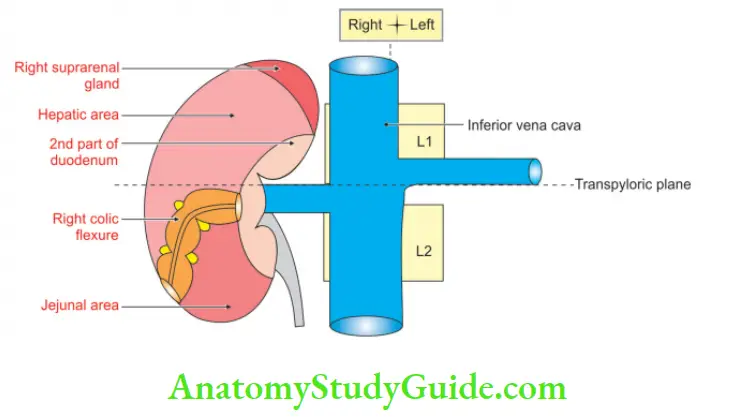
Fascial layer (false capsule):
- Renal fascia has anterior and posterior layers.
- The anterior layer is called the fascia of Toldt.
- The posterior layer is called the fascia of Zukerkandl.
- Following is the fate of these layers.
- Renal fascia
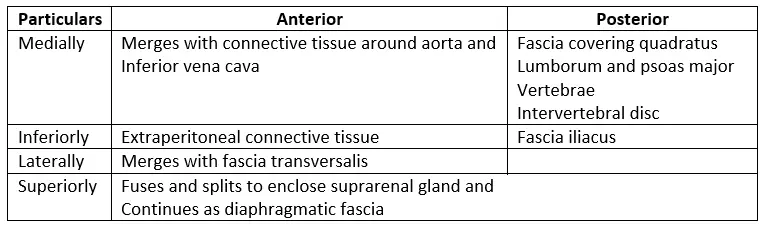
3. Relations of the right kidney:
Peritoneal relations:
- The anterior surface is partially covered with the peritoneum.
- The posterior surface is entirely non-peritoneal.
Visceral relations:
1. Anterior surface is related to
- Right adrenal gland
- Liver
- Hepatic flexure
- 2nd part of duodenum, and
- Jejunum.
Posterior surface: The costodiaphragmatic recess of the pleura is the most important relation on the posterior surface of left kidney.
Other structures related to the posterior surface of the right and left kidneys:
2. Medial border:
- Inferior vena cava, and
- Ureter.
3. Lateral border:
- Liver, and
- Ascending colon.
4. Relations of left kidney:
Peritoneal relations:
- The anterior surface is partially covered with the peritoneum.
- The posterior surface is entirely non-peritoneal.
Visceral relations:
1. Anterior surface:
- Adrenal gland
- Splenic flexure
- Pancreas
- Stomach, and
- Jejunum.
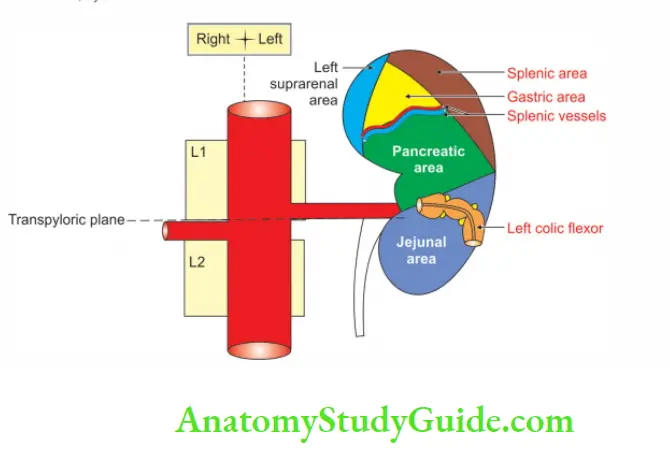
2. Medial border:
- Duodenojejunal flexure
- Inferior mesenteric vein
- Adrenal gland, and
- Ureter.
3. Lateral border:
- Descending colon
- Spleen.
5. Blood supply:
Arterial supply: The wide bored renal arteries supply the arterial blood to the kidney at a flow of 1 litre per minute.
1. Renal artery: It is a branch of the abdominal aorta which arises at the level of the intervertebral disc between L1 and L2. It enters the hilum and divides into
The anterior trunk which subdivides into four segmental arteries
- Apical
- Upper
- Anterior upper, and
- Lower.
The posterior trunk continues as the posterior segmental artery. The segmental artery divides into lobar branches.
- Interlobar arteries
- Arcuate arteries, and
- Interlobular arteries.
There is no collateral circulation between the segmental arteries.
2. Sometimes an accessory renal artery arises from the abdominal aorta. It supplies
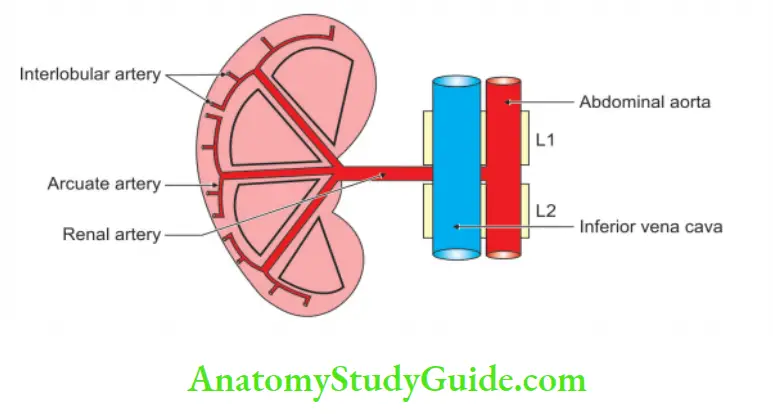
Venous drainage :
Veins form the renal segments and communicate with one another unlike the arteries
Features of veins:
- Small 5 to 6 renal veins unite at the hilum to form a single renal vein.
- Renal veins drain into the inferior vena cava.
- The left renal vein is longer than the right renal vein.
- The left renal vein receives the left gonadal and left suprarenal veins.
6. Nerve supply :
By renal plexus. This is formed by
1. The sympathetic fibres originate from the last three thoracic and 1st lumbar segments of the spinal cord (T10, L1). The sympathetic fibres are vasomotor in function.
2. The pain arising due to calculus present in the ureter or renal pelvic passes to the coeliac plexus > splanchnic nerve > sympathetic trunk > spinal cord. The pain is thus referred to the back and the lumbar region and radiates to the anterior abdominal wall and down to the external genitalia.
3. Parasympathetic nerves are derived from the vagus nerve. The functions are not clearly understood.
7. Lymphatic drainage:
The lymphatics of the kidney drain into para-aortic lymph nodes that are present at the level of origin of the renal arteries.
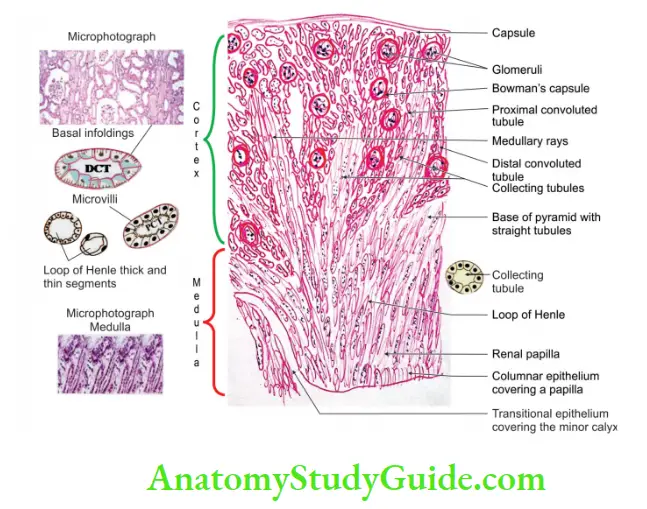
2. Histology
It consists of the inner medulla and outer cortex
1. Inner medulla: It presents about 8 to 18 renal pyramids which are striated, pale conical masses.
The base of the pyramid is directed to the cortex.
The apex projects into the wall of the renal sinus as renal papillae.
It contains duct of Bellini, that projects into the minor calyces.
Each minor calyx receives 2 or 3 renal papillae.
2. Outer cortex: It consists of two portions
1. An outer part towards the capsule, and
2. Inner part near the medulla. It is called the juxtamedullary cortex.
3. The cortex lying between two adjacent pyramids is called a renal column.
4. The cortex over the base of the pyramids is called a cortical arch. The cortex consists of
- Light-coloured areas are called the medullary rays, which are formed by the traversing collecting tubules.
- Dark-coloured areas are called convoluted parts.
3. Development
Chronological age: It develops in the 5th week and starts functioning in the 9th week of intrauterine life.
Germ layer: Intermediate mesoderm.
Site: In the pelvis.
Source:
1. The secretory part (nephron and renal corpuscle) develops from metanephric blastema.
2. The collecting part (minor calyx, major calyx, pelvis of kidney and ureter) develops from the ureteric bud which arises from the mesonephric duct.
Anomalies:
1. Depending upon incidence:
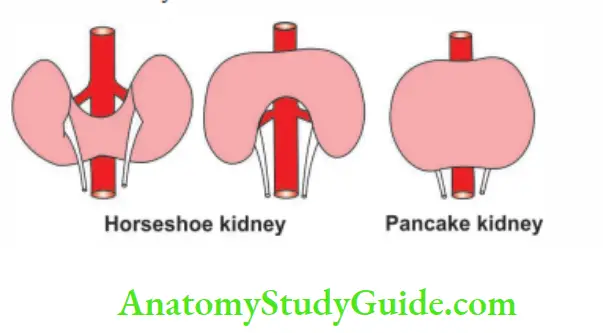
Horseshoe kidney: Inferior poles are usually fused (1/500).
Unilateral agenesis: Unilateral agenesis: of the kidney is relatively common (1/1000).
Bilateral agenesis (1/3000).
Congenital polycystic: There is a failure of fusion of the collecting and the secreting part.
It may be
- Autosomal dominant polycystic kidney disease (1/500 to 1/1000) or
- Autosomal recessive polycystic kidney disease (1/5000).
2. Depending upon the position, shape and rotation:
1. Anomalies of position:
- Failure to ascend: The kidney lies in the sacral region.
- Incomplete ascend: The kidney lies in the region of the lower lumbar vertebrae.
- Over ascend: The kidney lies in the thoracic cavity.
2. Anomalies of the shape:
- Horseshoe kidney: Lower or upper poles may be fused.
- Pancake € kidney: The two kidneys form one mass.
- Lobulated kidney: The nonnally lobulated and this lobulation may persist.
3. Abnormal rotation:
- Reverse rotation and
- Non-rotation of kidney.
4. Applied anatomy
1. The angle between the lower border of the 12th rib and the outer border of the erector spinae is known as the ‘renal angle’.
2. The tenderness of the kidney is elicited over this angle.
3. The danger of opening the pleural sac must be kept in mind while exposing the kidney from the back.
4. The hypermobile kidney can be moved vertically but not horizontally.
5. The kidney lies in the abundant fat present in the renal fascia.
6. In chronically debilitating patients, the kidney becomes hypermobile and produces symptoms of renal colic.
Question 4 : Describe the ureter under the following heads
1. Gross anatomy
2. Histology
3. Development, and
4. Applied anatomy.
Answer:
Introduction: The ureters are a pair of narrow, thick-walled muscular tubes. They carry urine from the kidneys to the urinary bladder.
1. Gross anatomy
1. Measurements:
Length: 25 cm (10″) of which
- 1.5″ lies in the abdomen, and
- 2.5″ lies in the pelvis. b. Diameter: 3 mm
2. Constrictions: Ureter is slightly constricted at 5 places.
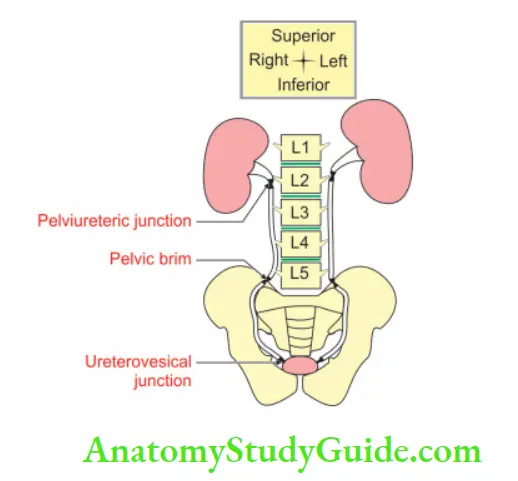
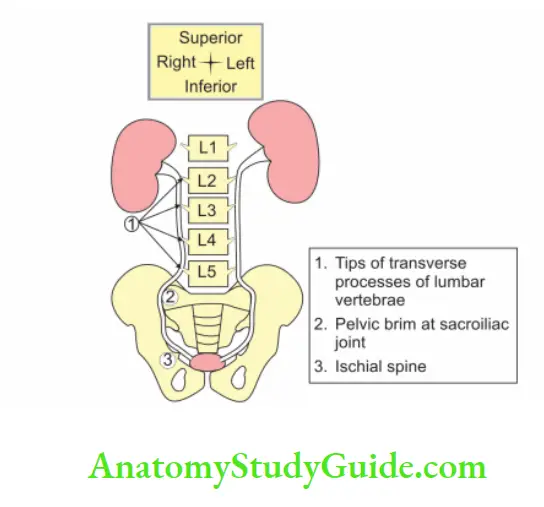
1. At the pelvic ureteric junction.
2. At the brim of the lesser pelvis.
3. Point of the crossing of the ureter by
- Ductus deferens in male ♂ .
- Broad ligament of the uterus in female ♀.
4. During its passage through the urinary bladder wall, and
5. At its opening in the lateral angle of the trigone of the bladder.
3. Course:
1. It begins in the renal sinus as a funnel ![]() shaped dilation, called the renal pelvis. It gradually narrows to the lower end of the kidney and becomes ureter proper.
shaped dilation, called the renal pelvis. It gradually narrows to the lower end of the kidney and becomes ureter proper.
2. The ureter passes downwards and lies medial to the tips of transverse processes of the lumbar vertebrae.
3. It crosses the pelvic brim at the sacroiliac joint.
4. It passes to the ischial spine and enters the urinary bladder obliquely to open into the trigone of the bladder.
4. Relations of ureter:
In the abdominal part: This is described in the
1. Renal pelvis: The structures are arranged from anterior to posterior. They are as follows
- Renal Vein (V)
- Renal Artery (A)
- Ureter most posteriorly (U).
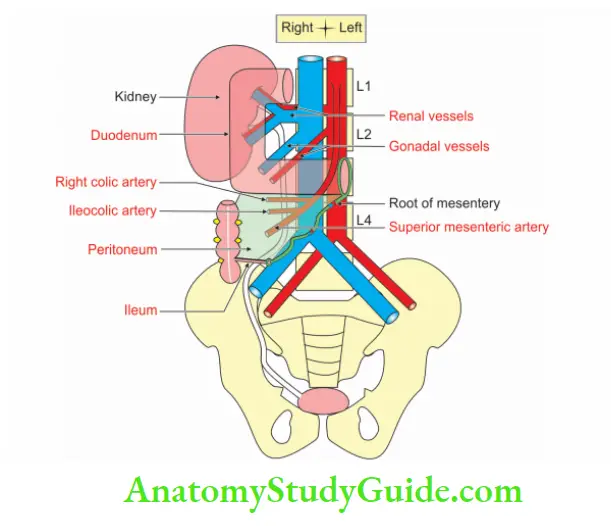
2. Anteriorly and on the right side:
- Peritoneum
- 3rd part of the duodenum
- Gonadal vessels
- Right colic vessels
- The root of the mesentery, and
- Ileocolic vessels.
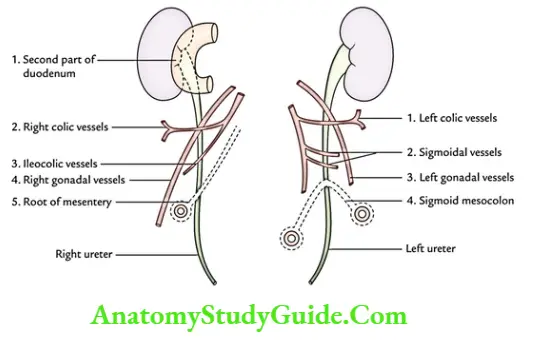
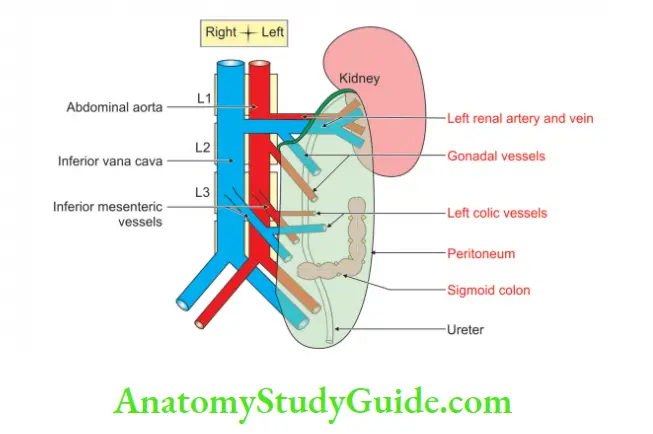
3. Anteriorly and on the left side:
- Peritoneum
- Left colic vessels
- Gonadal vessels, and
- Sigmoid colon.
4. Posteriorly:
- Psoas major
- Tips of the transverse processes, and
- Genitofemoral nerve.
5. Medially:
1. On the right side: Inferior vena cava.
2. On the left side
- Left gonadal vein, and
- Inferior mesenteric vein.
6. Relations of the ureter in the pelvis:
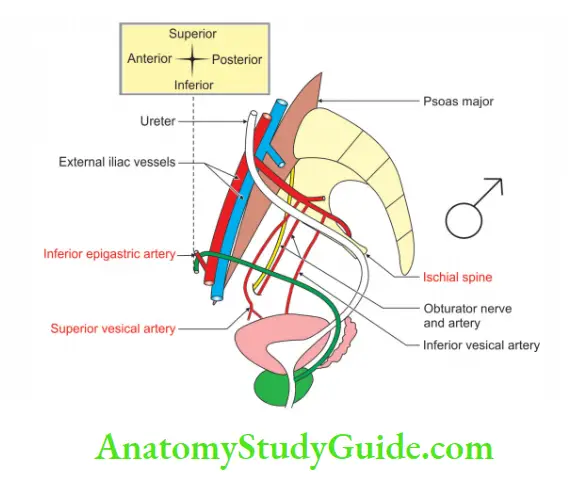
In its downward course:
1. Posteriorly:
- Internal iliac artery
- The anterior trunk of the internal iliac artery
- Internal iliac vein
- Lumbosacral trunk, and
- Sacroiliac joint.
2. Laterally: It crosses the following structures (‘NAAV from above downwards)
- Obturator Nerve (N)
- Obliterated umbilical Artery (A)
- Obturator Artery (A)
- Obturator Vein (V)
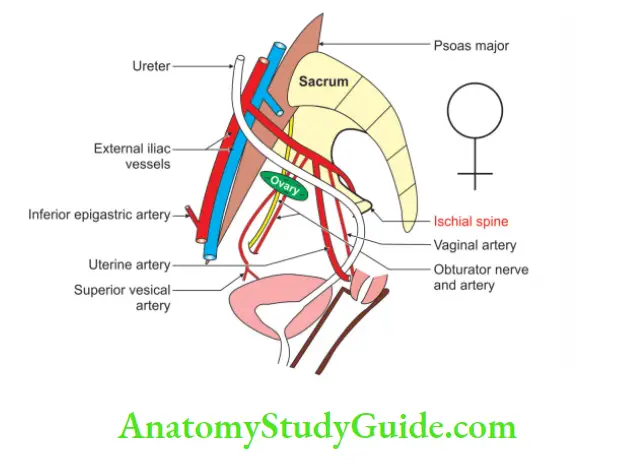
A word about ovarian fossa:
Note: In females, ♀ ureter forms the posterior boundary of the ovarian fossa.
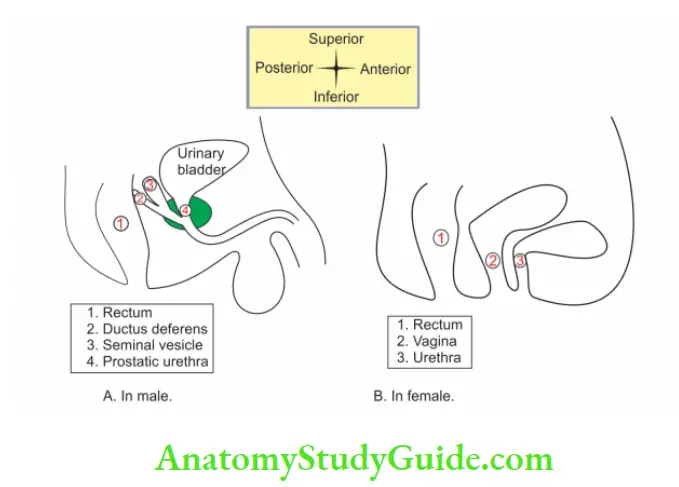
In its forward course:
1. Male ♂:
- The ductus deferens: It crosses the ureter from above and medially.
- Seminal vesicle.
2. Female ♀:
- The broad ligament of the uterus.
- Uterine artery: It crosses above and in front of the ureter from the lateral to the medial side.
- It then passes upwards to enter between the two layers of the broad ligament.
- Ureter lies 2 cm lateral to supravaginal part of the cervix.
It lies posterior to the vagina.
Intravesical part: It is oblique and acts as a valve. It prevents the regurgitation of urine
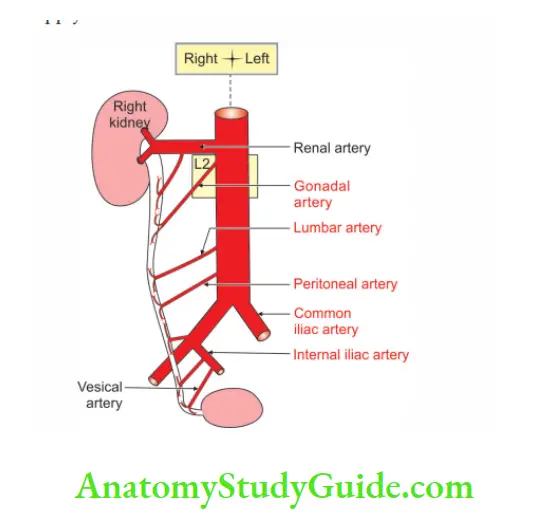
5. Blood supply:
Arterial supply: It is supplied by the different arteries in three different parts
1. Upper part: Receives branches from the
- Renal artery, a branch of the abdominal aorta
- The gonadal artery, a branch of the abdominal aorta, and
- Colic arteries are branches of superior and inferior mesenteric arteries.
2. Middle part:
- Branches from the abdominal aorta
- Gonadal arteries, and
- iliac arteries, terminal branches of the abdominal aorta
3. Pelvic part:
Branches of internal iliac artery
- Vesical arteries
- Middle rectal
- Uterine artery
The arteries of the ureter lie close to the peritoneum. They divide into ascending and descending branches. They form a plexus on the surface of the ureter and supply it.
Venous drainage: veins correspond to the arteries and drain into the inferior vena cava.
6. Nerve supply:
- The ureter is supplied by sympathetic (T10-L1) and parasympathetic (S2-S4) nerves.
- They reach the ureter through the renal, aortic and hypogastric plexuses.’
- All the nerves appear to be sensory in function. Parasympathetic nerves are motor in function.
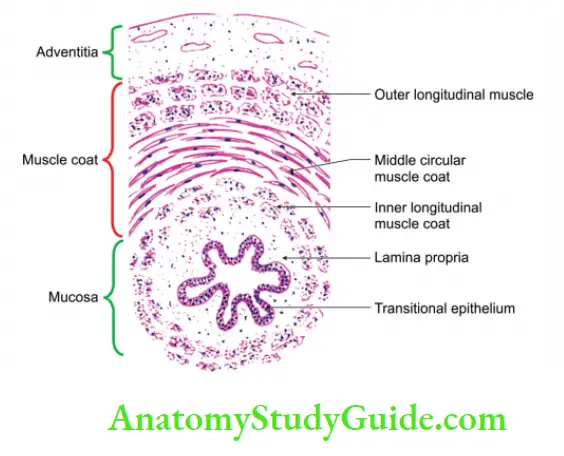
2. Histology
It is lined by
Fibrous coat: It is composed mainly of elastic fibres. It is continuous with the
capsule of the kidney and adventitia of the urinary bladder.
Muscle coat:
1. In the upper part of the ureter
- The outer coat is circular, and
- The inner coat is longitudinal.
2. In the lower part of the ureter
- The outer coat is longitudinal
- Intermediate is circular, and
- The Innermost is longitudinal.
3. No submucous coat
4. Mucous membrane
1. It is lined by transitional epithelium: No distinct basal lamina.
- The cells of the epithelium rest on a fibrous tissue containing many elastic fibres.
- The plasma membrane of the surface epithelium is unusual.
- It encloses special glycoproteins. It is believed that these glycoproteins make the membrane impervious.
- They prevent the entry of toxic substances present in urine. Thus, they protect adjacent tissue.
2. Lamina propria: It is thrown into 6 longitudinal folds when the ureter is empty.
3. No muscularis mucosa.
3. Development
Chronological age: It develops in the 5th week to the 9th week of intrauterine life.
Germ layer: Mesoderm.
Source: It is developed from the ureteric bud which arises from the caudal end of the mesonephric duct.
The upper part of the ureteric bud forms major and minor calyces of the renal pelvis and the lower part forms the ureter.
Site: Para-axial mesoderm
Anomalies:
1. The ureter may be partially or completely duplicated. It is usually associated with the duplication of kidneys.
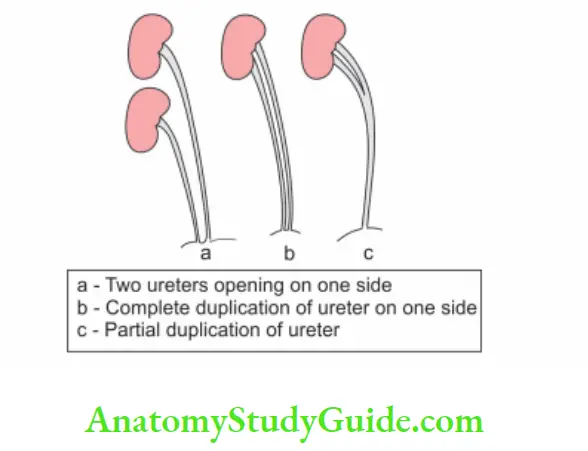
2. Abnormal sites of the opening of the ureter. The ureter may open in the
- Prostatic urethra
- Ductus deferens
- Seminal vesicles, or
- Rectum.
3. The upper end of the ureter may be blind.
4. The ureter may be dilated (hydro-ureter) because of the obstruction of the urine flow.
4. Applied anatomy
1. During hysterectomy or surgical removal of the uterus, the ureter may be injured at the following points.
- During ligation of the ovarian vessels in the infundibulopelvic ligament.
- At the site of crossing of the uterine artery by the side of the cervix.
- The left ureter is more likely to be damaged (water under the bridge) due to its close relation with the cervix.
2. Renal colic: It is the severe pain arising from the ureter due to the ureteric stone (s).
3. It causes spasms of the ureter. It starts in the loin and radiates down to the groin, scrotum (or the labia majora), and the inner side of the thigh.
4. Because of the common innervation of the ureter and the skin of the above organ, the pain is referred to the above-said regions.
5. The ureteric stone is liable to become impacted at one of the constricted sites.
6. The ureteric stone lodged in the lower part of the ureter in females ♀ can be felt by per vaginal examination.
7. This is because of the close relationship of the ureter to the lateral fornix of the vagina.
8. The abdominal part of the ureter receives blood supply from the medial side, therefore, the surgery of the ureter of the abdominal part is done by approaching from the lateral side.
9. The pelvic part of the ureter receives its blood supply from the lateral side, hence the pelvic part of the ureter is approached from the medial side.
Leave a Reply