Preventive Orthodontics Introduction
Preventive orthodontics is described as the action taken to preserve the integrity of what appears to be abnormal occlusion at a specific time.
Table of Contents
Various malocclusions could be prevented with prudent preventive orthodontic procedures.
Through the knowledge and interest of the clinician and understanding of the parents are required to plan and provide this time-bound dynamic method of treatment.
This chapter will deal, in detail, with the need and procedures for preventive orthodontics.
Simple pertinent steps go a long way in establishing an ideal teeth-and-jaw relationship essential for functional and aesthetic occlusion.
Read And Learn More: Paediatric Dentistry Notes
Prenatal And Post-Natal Infant Care For Prevention Of Malocclusion
Malocclusion can be prevented or reduced by following prenatal and post-natal measures.
Prenatal Measures To Prevent Malocclusion:
The aetiology of malocclusion includes genetic and environmental factors.
Prevention of congenital malformations of dentofacial structures begins with precautions taken during the time of pre-conception and morphogenesis of the foetus.
Therefore, it could be said that efforts for the prevention of malocclusion begin as early as the intrauterine formative stage.
It is imperative to educate expecting mothers about various teratogens, precautions to be taken and preventive measures.
Prenatal measures that prevent malocclusion are as follows:
1. Occurrence of chromosomal abnormalities and genetic aberrations is high in children born to closely related parents.
There is an increased probability of both parents carrying the same defective gene.
Pair of recessive genes get to express in such cases.
Avoiding consanguineous marriages can prevent these congenital malformations to a great extent though they may even occur in children of unrelated parents due to gene mutation.
2. Expecting mothers should be educated about the following factors that could, in future, precipitate malocclusion in the child, and they should be advised to take necessary preventive steps:
- Exposure to drugs and chemicals such as anticonvulsants and ethyl alcohol
- Exposure to radiation, infection or injury
- Intrauterine constraints such as large firoids
- Multiple pregnancies
- Maternal endocrine/systemic disturbances
3. Inclusion of micronutrients in the diet is important. Folic acid in early months prevents facials left. Calcium and phosphorous are critical for the mineralisation of teeth.
Post-Natal Measures To Prevent Malocclusion:
Post-natal measures that prevent malocclusion include the following:
- Adequate breastfeeding provides nutrition and immunity to the infant. Apart from this, the suckling and swallowing action during breastfeeding helps in the proper growth of jawbones.
- When bottle feeding is inevitable, the nipple should be of a physiological shape and size. Non-physiological nipples mould the alveolar arch in an unfavourable way and cause open bite when weaning is delayed.
- Leaving the feeding bottle with milk in the infant’s mouth for a long time, especially at night, should be avoided as it may lead to loss of tooth material and nursing bottle caries.
- Sugars should be avoided or scarcely used with the bottle feed: Direct sugars in the bottle feed, especially when left for a long period in the infant’s mouth, increase the incidence of caries. Caries-prone diet and frequent snacks between meals should be avoided even when the child grows up.
- Psychological needs of the infant should be attended to by the parents and pacifies should be avoided. Psychological insecurity of the child due to neglect or rejection may lead to oral habits such as thumb-sucking and lip-biting. Children may become addicted to pacifiers, the prolonged use of which also initiates harmful oral habits.
- The gum pads of a newborn should be wiped with a cotton cloth to maintain oral hygiene. A finger brush can be used when teeth erupt. Periodic check-ups with a clinician are mandatory from the time teeth erupt in the oral cavity. Toddlers should be introduced to proper brushing techniques and monitored while brushing.
Preventive Orthodontic Procedures
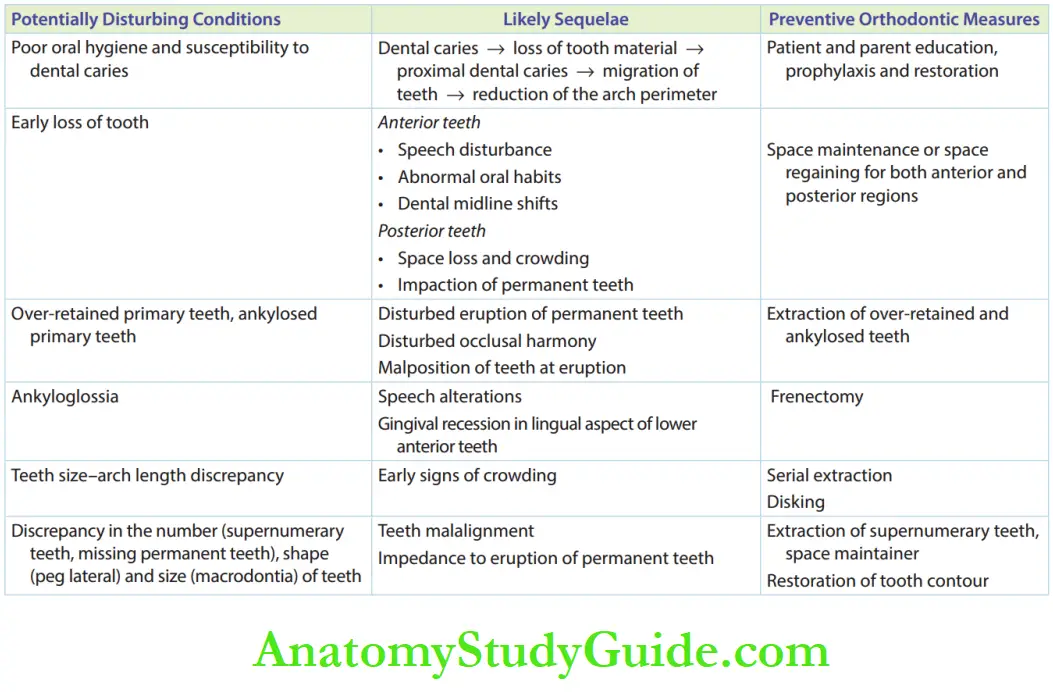
Potentially disturbing intraoral conditions, their likely sequelae and the need for time-bound management should be well understood.
These conditions must be checked at every review visit of the child.
Dental Caries Management
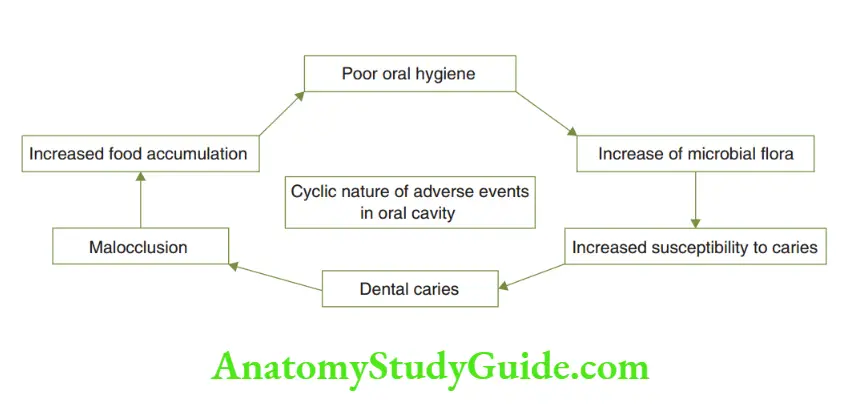
Poor oral hygiene, dental caries and malocclusion form a vicious cycle of adverse events in the oral cavity.
Poor oral hygiene predisposes one to dental caries. Dental caries is the most common cause of loss of tooth or tooth material.
Early loss of a tooth or tooth material leads to disturbances in the alignment of permanent teeth, leading to malocclusion.
Malocclusion can result in poor oral hygiene.
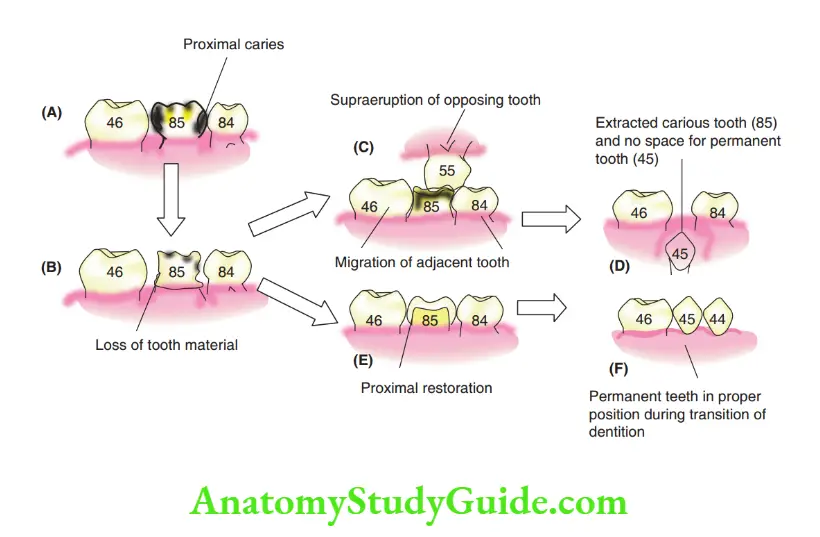
Proximal Tooth Surface Caries
Proximal tooth surface caries cause loss of proximal tooth structure.
When the tooth structure is not restored, the mesial, distal and opposing teeth migrate to reestablish contact with the carious tooth.
This results in loss of arch length and supra eruption of the opposing tooth.
When subsequently the carious tooth exfoliates, the permanent successor does not find sufficient space to erupt in the arch and is likely to get impacted or erupt in crowding.
Early proximal rehabilitation of the carious tooth structure prevents migration of adjacent teeth and supra eruption of the opposing tooth.
This maintains the arch length. When the arch space is preserved, the permanent successor has favourable chances of erupting in a proper position.
Preservation of tooth or tooth material is an important aspect of the prevention of malocclusion.
As the integrity of teeth and the arch is threatened by dental caries, prevention of dental caries and early restoration of decayed tooth surfaces are one of the primary preventive orthodontic measures.
Prophylaxis and re-establishment of the structural contour of the tooth are the simplest methods of preventing malocclusion.
Prophylaxis comprises parent and patient education on the following aspects:
- Brushing techniques
- Need for regular review visits
- Food habits
- Topical fluoride application
Early re-establishment of the lost structural contour of the tooth can be achieved by restorations, pulpal treatment and crowns for anterior and posterior teeth.
Early Loss Of Teeth
Primary teeth guide the eruption of their permanent successors.
The exact coordination between the exfoliation of a primary tooth and the eruption of its permanent successor is still not clear.
When the predecessor’s primary tooth is lost very early, the absence of a trigger to initiate the eruption of the corresponding permanent tooth may cause a delayed eruption of the latter.
Early loss of primary teeth occurs due to either trauma or dental caries.
This causes the migration of neighbouring teeth into the space thus created.
The possible outcomes of early loss of primary teeth and migration of adjacent teeth range from delayed eruption/crowding/impaction of the permanent teeth.
Sequelae of early loss of the primary anterior teeth and the fist and second molars are discussed in the following text.
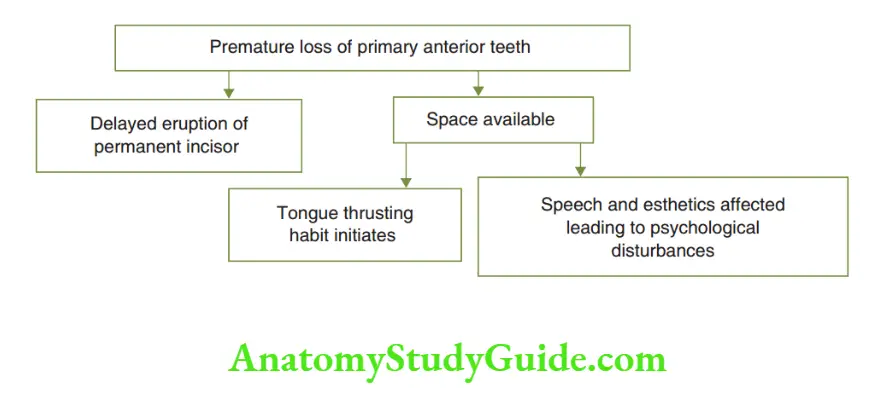
Loss Of Primary Anterior Teeth
Early loss of primary anterior teeth causes a delayed eruption of the permanent anterior teeth.
The space thus created alters the clarity of pronunciation and invites certain oral habits such as tongue thrusting.
The facial aesthetics of the child is also affected due to the absence of anterior teeth.
The ridiculing and teasing by peers cause psychological disturbances in the child.
Loss Of Primary First Molars
The deciduous fist molar usually erupts by 2 or 21/2 years of age and exfoliates at around 10 years.
This tooth is replaced by the first premolar. The hypothetical situations and sequelae of early loss of the deciduous fist molar are discussed with the help, the most probable consequence being the impaction of premolars.
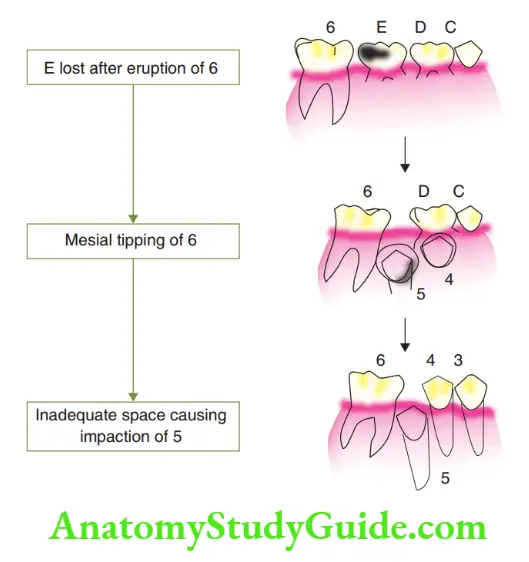
depicts a situation where the primary first molar is lost before the eruption of the permanent first molar.
This causes mesial migration of the primary second molar and mesial bodily movement of the permanent first molar into the alveolar trough.
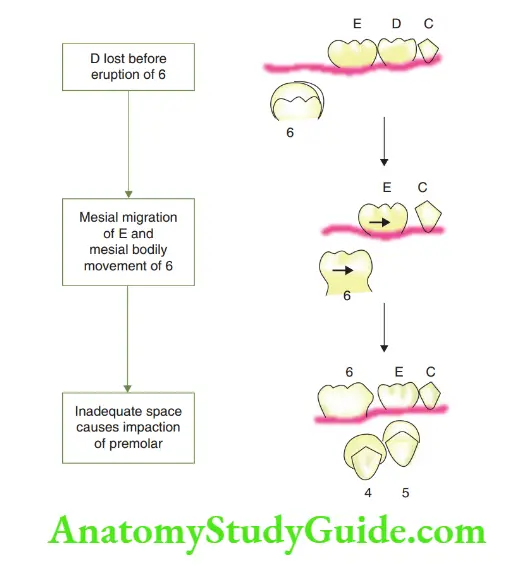
As there is inadequate space to accommodate two premolars, crowding/impaction of premolars is expected in this situation.
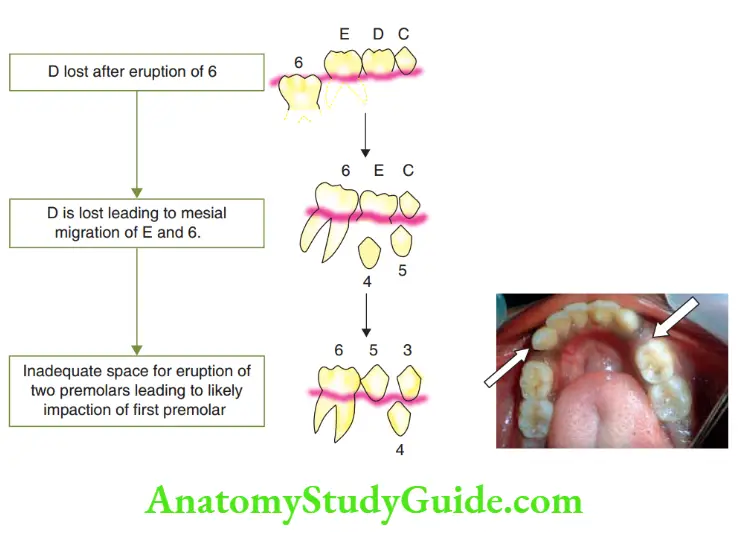
Loss of the primary fist molar after the eruption of the permanent first molar is the second situation depicted.
The second primary molar and the first permanent molar tip mesially into the space created by the lost primary first molar.
There is inadequate space for the eruption of two premolars, leading to crowding/impaction of the first premolar.
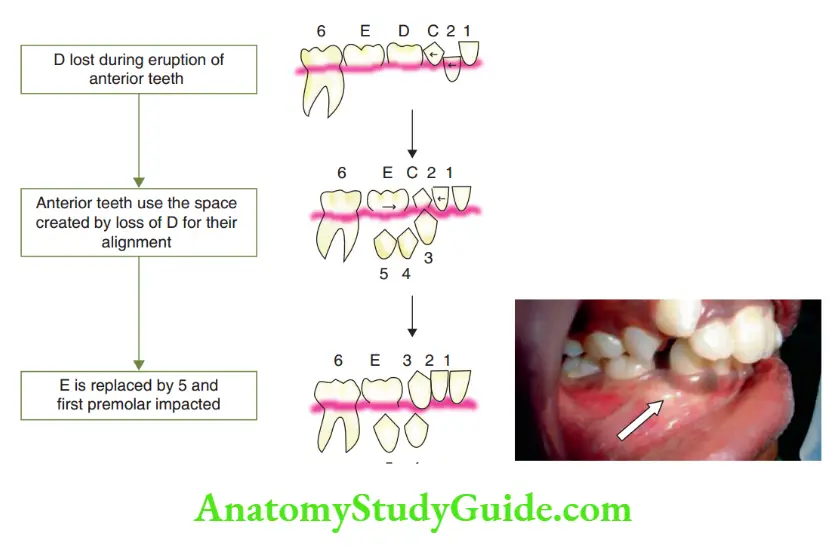
Loss of the primary fist molar during the eruption of permanent anterior teeth is the third situation depicted.
The erupting anterior teeth occupy all the space available between them and the primate space is utilised for the settling of the canines.
A bulge is evident on the buccal aspect of the alveolar mucosa in the premolar region indicating insufficient space in the arch for the eruption of premolars.
The premolar tooth may erupt buccally or remain impacted.
Loss Of Second Primary Molars:
The second primary molar normally erupts by around 21/2 years of age and exfoliates at around 11–12 years.
The roots of this tooth act as a guiding plane for the eruption of the first permanent molar depicting two hypothetical situations that may lead to malocclusion due to the early loss of the second primary molar.
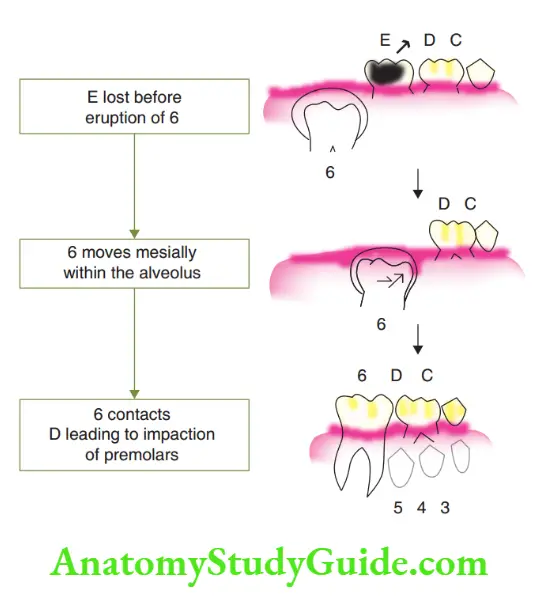
The loss of the second primary molar before the eruption of the first permanent molar is the first situation.
The eruption guidance for the first permanent molar is absent when the second primary molar is lost before the eruption of the first permanent molar.
The first permanent molar tends to move mesially within the bony trough of the alveolus.
The tooth continues to tip mesially upon eruption and contacts the first primary molar.
The arch perimeter is severely reduced due to this migration, leaving inadequate space for the erupting premolars.
The second situation is the loss of the second primary molar after the eruption of the first permanent molar.
the first permanent molar erupts into the arch place with the roots of the second primary molar as the guiding plane.
Premature loss of the second primary molar causes mesial tipping of the first permanent molar into its space.
The arch perimeter is reduced, leading to inadequate space for the erupting premolars.
While the first premolar may erupt, the second premolar either may get impacted or its path of eruption may be altered. The premolar may erupt buccally or lingually, causing severe crowding.
Space Maintainers:
Premature loss of primary teeth causes disturbances in eruption, alignment and function of permanent dentition.
Such situations have to be prevented to avoid the resulting malocclusion.
The space created by the premature exfoliation of the primary teeth has to be preserved for the proper eruption of the permanent teeth.
Space maintainers are passive appliances that occupy the mesiodistal space created by prematurely lost tooth or tooth material until the permanent successor erupts into that place.
Appliances designed to regain and then maintain space are called active space maintainers or space regainers.
A space maintainer that prevents supra eruption of the opposing tooth into the space created is called a ‘functional space maintainer’.
Indications
The following are the indications of a space maintainer:
1. When root development of the successor’s tooth is less than one-third: A tooth does not begin its eruption journey before one-third of its root formation is complete.
The eruption is likely to take considerable time if less than one-third of the root is formed.
This time is sufficient to allow the neighbouring teeth to migrate into the space originally occupied by the lost primary tooth in the arch.
2. When the assessed eruption time of the permanent tooth is not within 3–4 months: One-millimetre thickness of bone covering the erupting tooth is resorbed in 3–4 months.
Considering this fact, a space maintainer is required when the bone thickness is more than 2 mm.
3. When occlusion is not locked: Intact cusp-to-groove occlusion between upper and lower posterior teeth prevents migration of adjacent teeth into the available spaces.
A space maintainer is indicated if such a locking occlusion does not exist.
4. Space discrepancy: When some space discrepancies like crowding or closed primary dentition already exist, more space loss cannot be afforded. The available spaces have to be maintained to avoid undesirable loss of space.
5. Unilateral congenitally missing tooth: Congenital absence of a tooth on one side of the arch can cause migration of teeth, leading to an unaesthetic shift of the dental midline.
The lateral incisor is the commonest congenitally missing anterior tooth.
Midline shift must be anticipated in such situations and a space maintainer is indicated to preserve the midline and the space of that particular tooth for future management.
6. When functions are affected: Loss of incisors can affect speech, while loss of posterior teeth may affect mastication.
The spaces of prematurely exfoliated teeth have to be maintained to preserve the functions of these teeth.
Contraindications:
A space maintainer is not indicated when the successor’s tooth is about to erupt.
This is evident by observing the radiograph, which does not reveal any bone overlying the erupting successive permanent tooth.
The completion of three-fourths of root formation and one-third of root calcification of the permanent tooth indicates that the tooth will erupt soon.
Severe spacing may be seen in the case of microdontia and spaced primary dentition.
Space crisis may not be encountered due to the presence of primary spacing and primate spacing.
Such children are kept under regular observation and space maintainers are indicated only when threatening occasions arise.
Requisites Of A Space Maintainer:
A good space maintainer should have the following requisites:
- It should be rigid enough to withstand functional forces and maintain space.
- It should not interfere with functions such as speech and mastication.
- It should not interfere with the growth process.
- It should be simple to maintain and clean.
- It should be biocompatible and should not irritate the soft tissues.
- It should be passive and should not exert force to displace other tooth/teeth.
Removal Of A Space Maintainer:
The objective of a space maintainer is to hold and maintain the space along the arch perimeter until the corresponding permanent tooth occupies its position.
The appliance is therefore held until signs of the eruption of the permanent tooth are sighted and confirmed with radiographs.
Periodic review is mandatory and parents have to be adequately educated about the purpose of the appliance.
A denture-type appliance is likely to interfere with eruption or redirect the erupting tooth if left unattended.
A prosthetic space maintainer indicates that the space of a permanently lost tooth has to be replaced with a permanent prosthesis at an appropriate time.
Classification/Designs Of Space Maintainers:
Space maintainers can be designed by the clinician as per the individual needs of the patient.
The designs widely used address all the requisites of a space maintainer with a scientific understanding.
Modifications in incorporation and elimination designs are up to the prudent clinician.
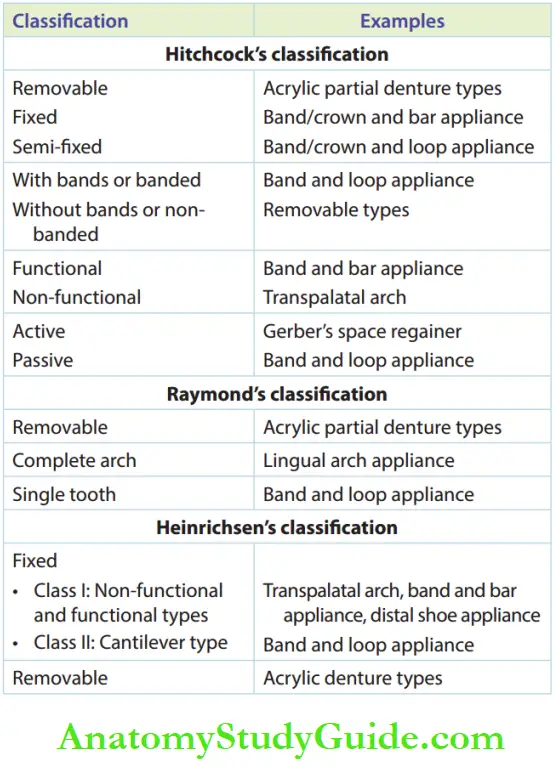
Several authors such as Hitchcock, Raymond C Throw and Heinrichsen have classified space maintainers in various ways. The space maintainers commonly used in current practice are listed.
Band and Loop Space Maintainer:
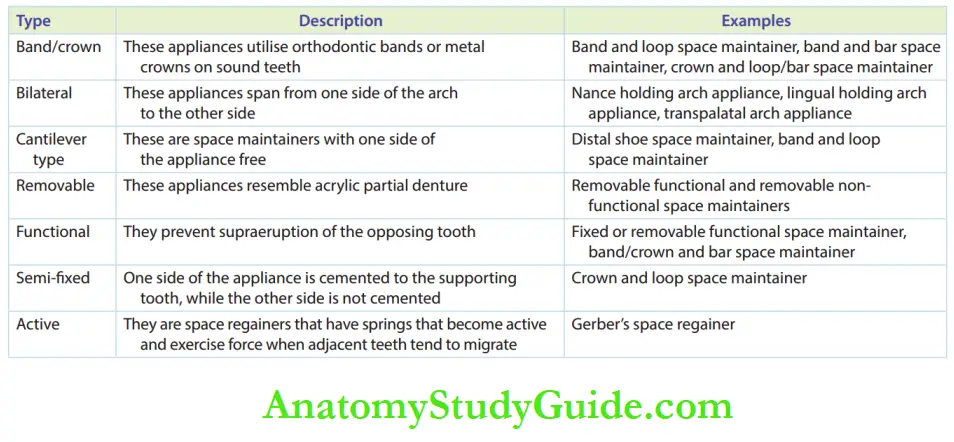
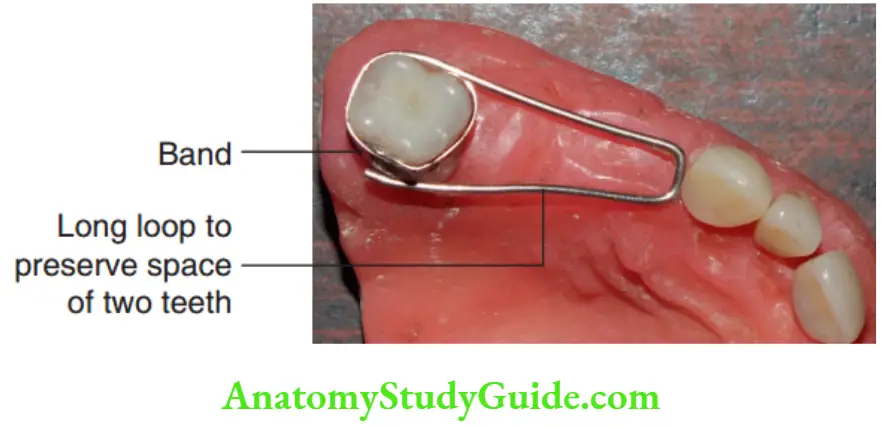
Band and a loop space maintainer is a fied, banded, unilateral, passive and non-functional space maintainer.
It consists of a band adapted to the tooth distal to the edentulous space and a loop that spans the space to be maintained.
Design And Construction:
An impression of the arch with the band on the tooth distal to the edentulous space is recorded. The band is transferred to the working cast.
A loop is fabricated using a 19-gauge stainless steel wire.
It is bent to span through the edentulous space and passively contacts the mesial tooth just below its contact area.
This loop wire is soldered to the band. The bent loop inculcates the following features:
- It is bent with no sharp kinks/bends.
- The loop is 8 mm wide to avoid any possible interference with the erupting tooth.
- 1 mm of soft tissue relief is provided while contacting the mesial tooth passively.
- It is well adapted to follow the contour of the soft tissue.
- It is soldered on the band at the middle third causing no occlusal interference (occurs, if in the occlusal third) or no plaque accumulation (occurs, if in the gingival third).
The appliance is well-finished, polished and luted in place with appropriate cement.
Clinical Applications:
The appliance can be used for posterior spaces, especially for the premolar area.
The advantages of this design are as follows:
- Relatively simple, quick and easy to fabricate
- Does not interfere with the jaw-growth process
- Allows uninterrupted eruption of the successor’s tooth
The disadvantages are as follows:
- The band and loop are fixed appliances with a cantilever-type design, attached only distally. The loop can sag down stripping the distal gingiva of the mesial tooth.
- Any banded appliance is plaque retentive, thus increasing the caries proneness of the tooth. This appliance is not preferred in children with high caries susceptibility.
- It does not prevent supra eruption of the opposing tooth as it is non-functional.
Modifications:
- Band and distal loop: Sometimes the mesial tooth is banded with the loop distal to it.
- Band and long loop: This appliance maintains the space for two teeth. A crosswire may be placed at the prospective point of the eruption of the succedaneous teeth to add stability to the long wire.
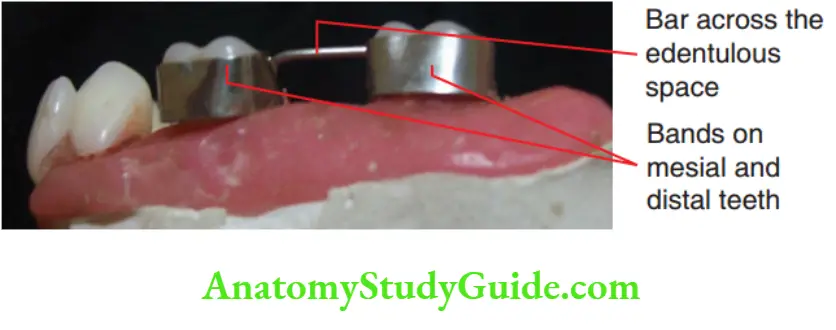
Band And Bar Space Maintainer:
Band and bar appliance is a fied, banded, unilateral, passive and functional space maintainer.
The teeth are mesial and distal to the edentulous space and are banded with a bar between the bands.
Design And Construction:
The two bands on the mesial and distal teeth are transferred to a working cast.
A bar, connecting the bands, is soldered at an occlusal level to contact the opposing tooth.
The appliance is finished, polished and luted with suitable cement.
Clinical Applications:
Band and bar appliances are used to preserve posterior space while preventing supra eruption of opposing teeth.
The advantages of this appliance are as follows:
- There is no possibility of harming the gingiva, such as the band and loop appliance.
- It is a functional appliance and prevents supra eruption of the opposing tooth.
The disadvantages of the appliance are as follows:
It is possibly more caries-concentive than a band and loop as it has two bands.
If left unattended for a long time, the presence of a bar may interfere with the complete eruption of the tooth.
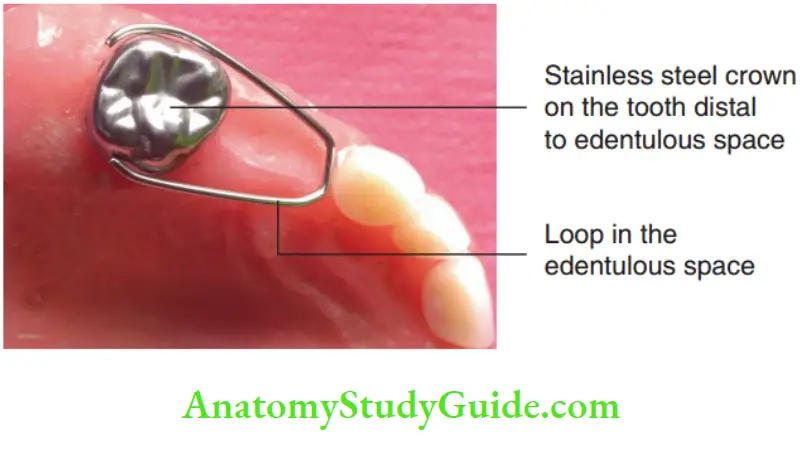
Crown and Loop Space Maintainer:
Crown and loop appliance is a fied, unilateral, passive and non-functional space maintainer.
The appliance consists of a loop in the edentulous area and a
crown on the tooth distal to it.
Design And Construction:
A stainless steel crown is adapted onto the sound tooth abutting the space of the lost tooth and an impression is recorded.
The crown is transferred to a working cast and the loop is soldered to the crown. The appliance is finished and polished before cementing it in the arch.
Clinical Applications:
This appliance is quite similar to a band and loop appliance, except that it includes a stainless steel crown instead of a band.
It is indicated when the tooth distal to the edentulous space is endodontically treated or indicated for a stainless steel crown.
When the caries activity is very high, a full-coverage crown is best indicated in place of a band to combat caries incidence.
Otherwise, crown and loop space maintainers share the same advantages and disadvantages as the band and loop space maintainers.
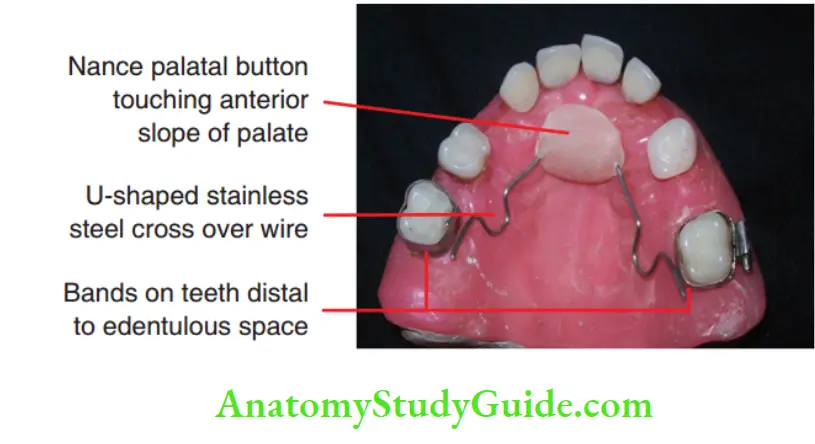
Nance Holding Arch Appliance:
Nance holding arch is a fied, bilateral, passive and nonfunctional space maintainer.
It is indicated in bilateral premature loss of maxillary primary teeth.
Design And Construction:
Nance holding arch consists of bands fabricated on molars distal to the edentulous spaces on either side of the arch.
The bands are connected to each other with a ‘U-shaped stainless
steel wire running from one molar to the anterior palatal area and then to the other molar.
An acrylic button, called the Nance palatal button, is incorporated in the anterior part of the wire.
The acrylic button contacts the anterior slope of the palate and not the anterior teeth.
Clinical Applications:
Nance holding arch is used for holding bilateral posterior spaces.
This appliance is especially indicated when the spaces are immediately mesial to teeth on which bands can be fabricated.
A transpalatal arch appliance (discussed in the following pages) is futile in such situations as it allows the simultaneous movement of molars on either side.
The advantage of the Nance holding arch appliance is that it preserves the space of multiple teeth and several modifications are possible.
The disadvantage, though not documented adequately, is the possibility of growth retardation in the transverse dimension and plaque accumulation between the button and palatal tissues.
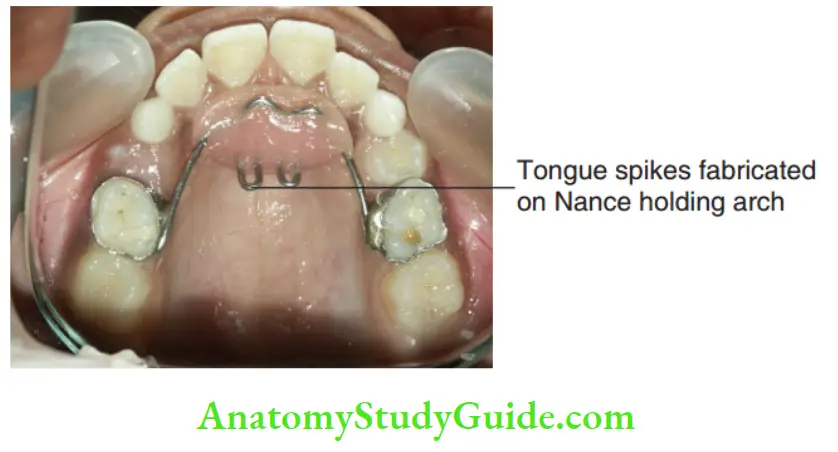
Modifications:
1. Nance holding arch with spurs: Spurs or extension wires can be soldered to the Nance holding arch appliance when more than two bilateral edentulous spaces have to be maintained.
The spurs extend from the Nance holding arch appliance to the alveolus and contact the mesial or distal surfaces of teeth, preventing their migration into adjacent spaces.
2. Fixed functional space maintainer: In case of premature loss of primary anterior teeth, the Nance palatal button can be extended anteriorly and pontics or prosthetic teeth can be soldered there to replace the lost anterior teeth. This becomes a fixed functional appliance.
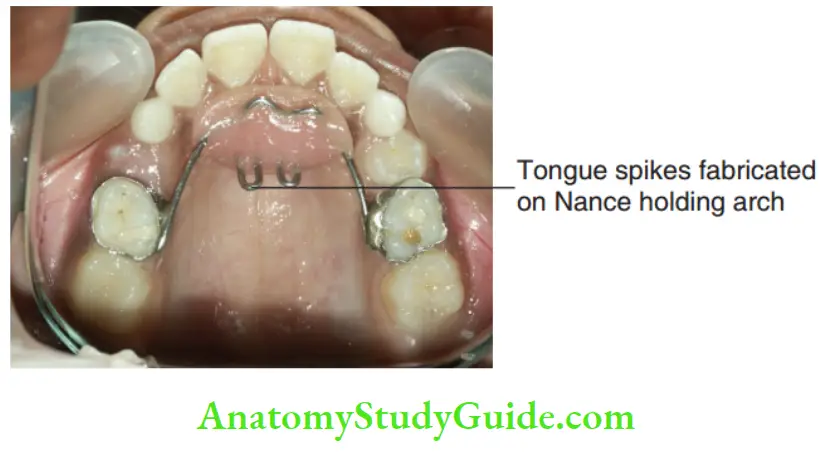
3. Habit-breaking combo appliance: Wire spikes can be fabricated and acrylic on the Nance palatal button in cases of oral habits such as thumb sucking/tongue thrusting. Such an appliance can maintain the edentulous space and serve as a habit-breaking appliance.
Lingual Holding Arch:
The lingual holding arch is a fied, bilateral, passive and non-functional space maintainer. It is indicated for the maintenance of bilateral edentulous spaces in the mandibular arch.
Design And Construction:
Bands are fabricated on the teeth distal to the bilateral edentulous space, preferably on the molars.
A wire is bent in a ‘U’ shape and adapted close to the tissues on the lingual gingiva, passively touching the cingulate of permanent incisors.
The wire is soldered to the lingual surfaces of lower molar bands on either side.
The appliance is then trimmed and polished before luting.
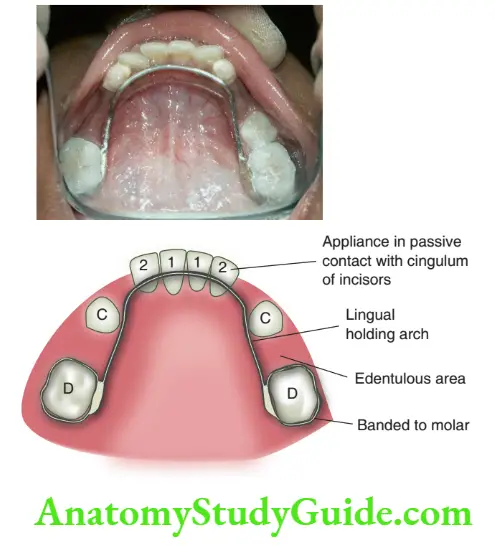
Clinical Applications:
Lingual holding arch appliance is highly useful to preserve the space of the first primary molar when there is premature exfoliation (arch length deficiency) or therapeutic extraction (serial extraction) of the primary canines.
The appliance effectively holds bilateral spaces in the lower arch.
The disadvantage is that the arch cannot be indicated until lower anterior teeth have erupted fully as it may interfere with the eruption of these teeth.
Until the eruption of lower anterior teeth, bilateral posterior spaces have to be preserved with separate band and loop appliances on either side.
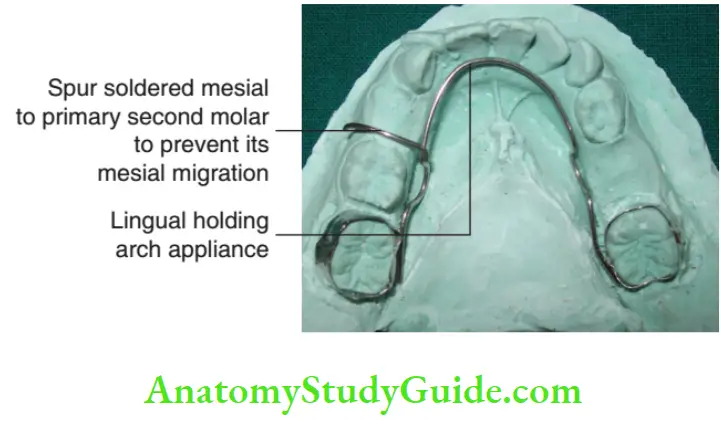
Modifications:
1. Lingual holding arch with spurs: This modification of the lingual arch space maintainer is efficient when multiple bilateral spaces have to be maintained.
Spurs can be soldered on the lingual archwire corresponding to each tooth, mesial or distal to every edentulous space.
2. Active lingual arch appliance: U-loops are incorporated in the lingual arch when lower anterior teeth are reclined and crowded.
Activating the U-loops allows the proclamation of the incisors, leading to decrowding of incisors.
This appliance is contraindicated when crowding is associated with proclined incisors.
3. Active lingual arch space regainer: U-loops are incorporated in the lingual arch closer to the molar teeth when they have migrated anteriorly causing space loss in the arch. Activating the U-loop results in mild destabilisation of molars.
4. Lip pads/lip bumper anchor: The lingual holding arch can have a parallel labial wire crossing the dentition to anchor lip pads/lip bumper, thus assisting in the elimination of the lip-biting habit.
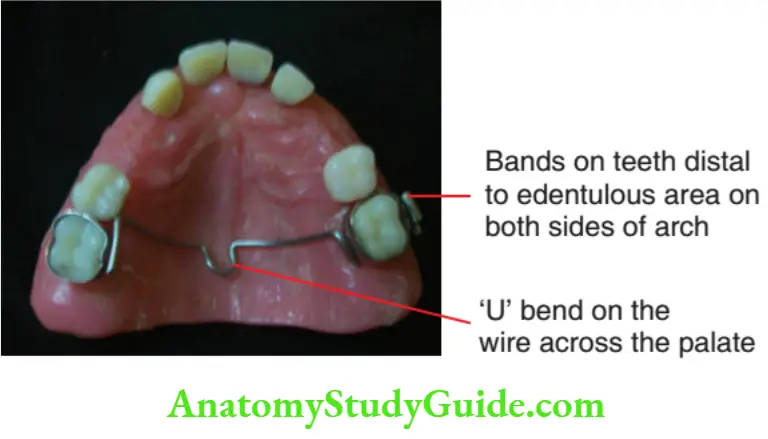
Transpalatal Arch:
Transpalatal arch (TPA) is a field, bilateral, passive and non-functional space maintainer used for unilateral posterior space maintenance.
Design And Construction:
The appliance comprises bands on the teeth distal to the edentulous space and the most distal molar on the opposite side.
A 19-gauge stainless steel wire is bent and well adapted to follow the contour of the palate, with a relief of 2 mm from it.
The wire is incorporated with a U-bend in the centre and is soldered to the molar bands on either side. The appliance is finished and polished before cementing.
Clinical Applications:
The trans-palatal arch is a bilateral space maintainer used for unilateral posterior space maintenance.
It has the advantage of being sturdy and resisting deformation. Though trans palatal arches are strong appliances, they are contraindicated for maintenance of bilateral spaces and spaces immediately mesial to them.
Amaxillarymolartendsto rotates anteriorly and palatally when it migrates mesially with the axis of rotation around its palatal root.
In the case of bilateral edentulous spaces, molars on either side will have the tendency to rotate anteriorly and palatally.
Hence, this appliance is contraindicated when bilateral spaces immediately mesial to them have to be preserved (e.g. loss of both second primary molars)
Modifications:
1. Arch expansion appliance: The U-loop of the trans-palatal arch can be activated to obtain arch expansion.
2. Space regainer: trans palatal arch can also be modified to destabilise molars, derogate molars and regain space.
3. Molar intrusion appliance: The tongue delivers an intrusive force on the molars when the U-loop of the appliance is fabricated about 3–5 mm away from the palate and in contact with the tongue at rest position.
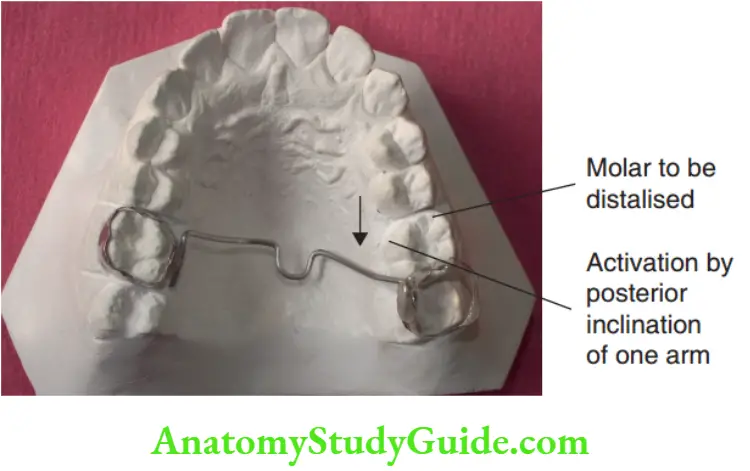
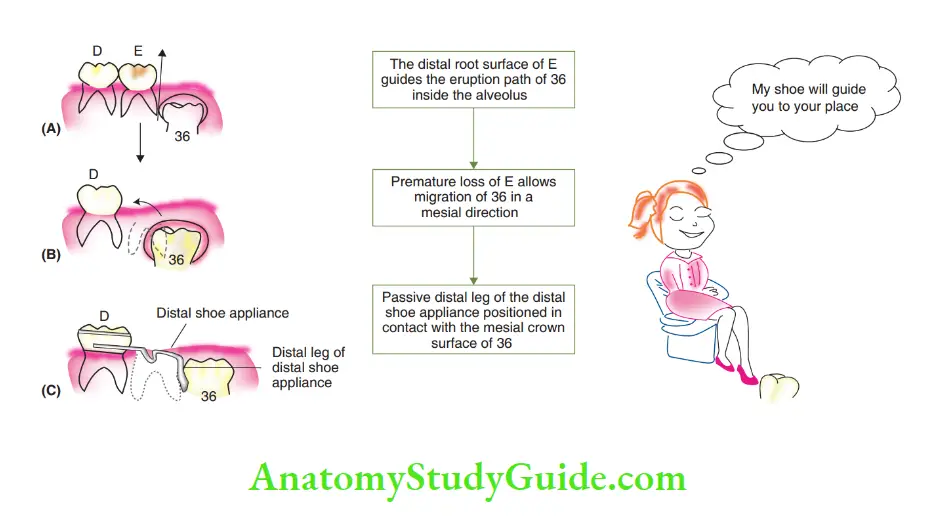
Distal Shoe Space Maintainer/Willet’s Appliance:
A distal shoe space maintainer is a semi-fitted, unilateral, passive and non-functional space maintainer designed by Willet.
It is indicated for the maintenance of the space of a lower second primary molar, which is to be extracted before the eruption of the first permanent molar.
The distal extension of the appliance is embedded into the alveolus and hence it is called an ‘intra-alveolar appliance’.
The appliance is also called an ‘eruption guidance appliance’ as it guides the eruption of the first permanent molar into place.
Rationale Of Distal Shoe Appliance:
The lower first permanent molar has a mesio-occlusal path of eruption.
The distal root surface of the second primary molar is believed to guide the eruption of the first permanent molar.
In the absence of the second primary molar, there is the bodily movement of the first permanent molar follicle.
The migrated molar erupts mesially as there is no mesial stop or guidance.
This causes moderate to severe loss of arch length. It also leaves inadequate space for the eruption of the second premolar in future.
The distal shoe appliance is fired when a second primary molar is lost before guiding the erupting first permanent molar.
The distal leg of the appliance is positioned passively in contact with the mesial surface of the erupting first permanent molar.
It acts as a proxy to the root surface of the lost second primary molar.
Thus, the appliance provides a guiding plane for the eruption of the permanent first molar.
The distal shoe appliance is not indicated in the maxillary arch as the maxillary first permanent molar has a disto-occlusal path of eruption.
Premature loss of the maxillary second primary molar is therefore believed to have no effect on the position of the maxillary permanent first molar.
Design And Construction
The steps in the fabrication of the appliance are as follows:
Step 1: An intraoral periapical (IOPA) radiograph is taken to calculate the length of the arm and the depth of the shoe to be designed.
Step 2: A band/crown is fabricated on the fist primary molar (D) and the distal shoe appendage is fabricated. A stainless steel wire is bent accordingly.
Step 3: An impression is taken along with a band/crown on ‘D’.
The band/crown on D is transferred to the prepared working cast.
In the cast, the second primary molar is scraped off and a hole corresponding to the distal surface of the primary second molar, as calculated, is created.
The distal shoe end is then positioned in the created socket or hole while the other end contacts the band/crown on ‘D’. The wire and band/crown are soldered together.
The prepared appliance is removed from the cast and trimmed.
The appliance is polished, sterilised and kept ready before the extraction of the primary molar for cementation immediately after the extraction procedure.
Step 4: The second primary molar is extracted.
When the bleeding is controlled, the distal shoe maintainer is placed in the arch and an IOPA radiograph is taken.
The position of the distal shoe should be passive, mesial and adjacent to the crown of the first permanent molar.
The shoe ends should never be on the occlusal surface of the erupting molar, which would prevent the eruption of the molar.
Necessary adjustment of the wire is done until a satisfactory position of the appliance is confirmed with IOPA radiographs.
Step 5: The distal shoe appliance is cemented on the first primary molar and it is mandatory to check the eruption path of the permanent tooth periodically
Clinical Applications:
A distal shoe space maintainer is the only appliance that guides the erupting first permanent molar.
The appliance is indicated when the second primary molar requires extraction and the child has not reported with a tooth extracted already.
The first primary molar is capable of being banded or crowned.
The first permanent molar has started its eruption process, as observed from the level of root formation.
The contraindications of the distal shoe maintainer are as follows:
- Medicallycompromisingconditions such as bleeding disorders, compromised immunity
- Lack of patient cooperation
- Poor oral hygiene and multiple dental caries
Modifications:
The space maintainer was originally designed by Willet in 1932. A ‘V-shaped distal extension was suggested by Roche.
On eruption of the first permanent molar, the distal shoe appliance has to be replaced with one of the following appliances:
1. Reverse band and loop (band and a distal loop): The band is on the first primary molar and the loop contacts the fully erupted permanent molar.
2. Conventional band and loop: The band is on the permanent molar and the loop contacts the first primary molar.
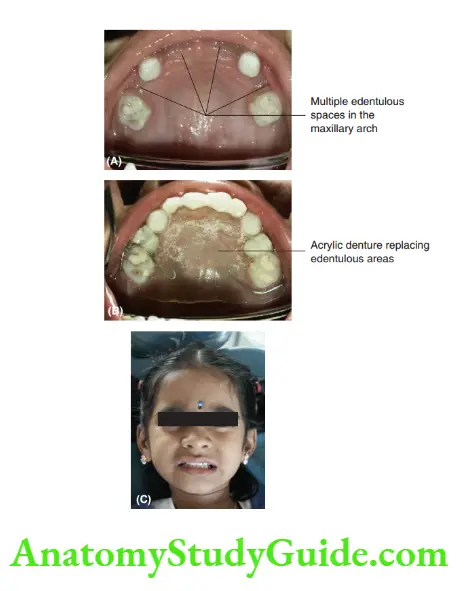
Removable Functional Space Maintainer:
A removable functional space maintainer is a removable, unilateral/bilateral, passive and functional appliance.
It is indicated to rehabilitate function when multiple anterior or posterior teeth are prematurely lost.
It resembles an acrylic partial denture. Design, construction, wear instructions and maintenance are quite similar to those of an acrylic partial denture.

Clinical Applications:
The removable functional space maintainer maintains multiple spaces, enhances oral hygiene and does not increase caries incidence.
Besides space maintenance, the appliance enhances aesthetics and self-esteem through the following functions:
- Establishes occlusion and prevents supra eruption of the antagonist’s tooth
- Enables labiodental sounds such as /f/ and /v/
- Helps in mastication
- Maintains the normal adult swallowing pattern
This space maintainer is sought when rehabilitation of several functions is considered as important as space maintenance.
The appliance has the following disadvantages:
- The appliance is removable and requires the child’s compliance for using it.
- Appliances may be broken or frequently lost by the children.
- The appliance has to be repaired or redone possibly once in 18 months in accordance with jaw growth.
- The appliance is not indicated for special children or emotionally immature children and epileptics.
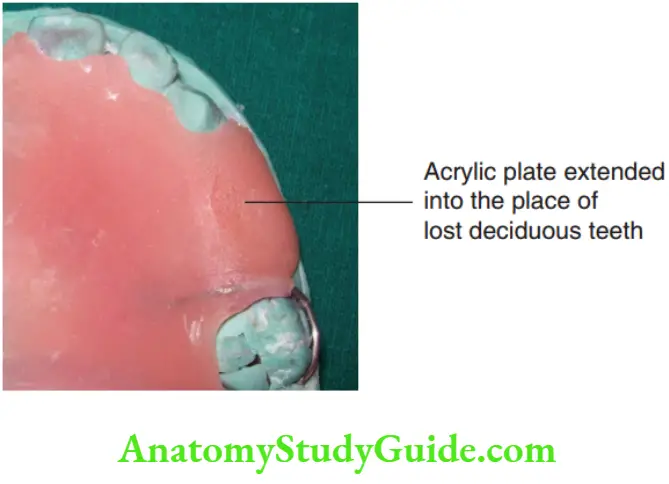
Removable Non-Functional Space Maintainer:
A removable non-functional space maintainer is quite similar to the functional variety except that it bears an extended acrylic flange in place of lost teeth.
It does not rehabilitate any function other than space maintenance.
The flange must be hollowed out from the inside/trimmed when the permanent tooth erupts.
The disadvantage is that the appliance does not prevent the supra eruption of opposing teeth.
Fixed Functional Space Maintainer:
A fixed functional space maintainer is one that rehabilitates function while delivering fixed space maintenance.
These appliances are fitted on both ends of the edentulous area with bands or crowns.
A horizontal wire at the occlusal level is soldered to bands on either side.
The wire prevents the supra eruption of opposing teeth. The band/crown and bar and trans palatal arches (explained before) are also fixed functional space maintainers.
These appliances are indicated for non-compliant children.
Clinical Applications:
As two teeth are connected with a wire, they are prevented from functioning independently.
They function as a single unit and stress exerted on one tooth is passed on to the other tooth also. This problem is addressed by the ‘broken stress space maintainer’.
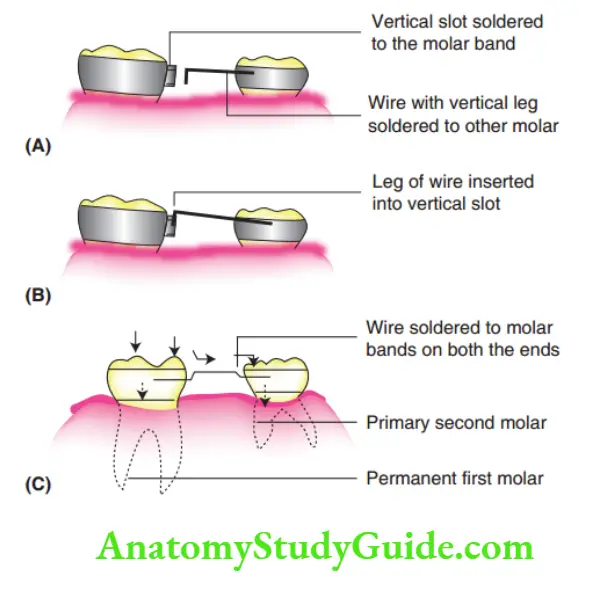
Broken Stress Space Maintainer:
A broken stress space maintainer can be used in place of a fixed space maintainer as it allows independent movement of the teeth attached to the appliance.
Design And Construction:
This appliance is split into two components. It consists of a band with a vertical slot or tube on one tooth and a wire with a vertical leg soldered to the other tooth.
The vertical leg of the wire is inserted into the vertical slot of the other tooth.
The leg moves freely within the slot but does not slip out.
The teeth on either side of the edentulous area exhibit independent vertical movement as there are no attachments firing both of them.
Occlusal stresses are not transmitted between the two teeth in this stress-broken space maintainer.
Clinical Applications:
Teeth experience enormous load during biting and chewing.
Each tooth responds to this load by very mild vertical and lateral movements within its periodontium as the periodontal fires act as shock absorbers.
The essential independent movements are prevented by a fixed functional space maintainer.
When two teeth are connected to the field space maintainer, any force exerted upon one tooth gets transmitted unnecessarily to the adjacent tooth through the connecting bar as discussed with field space maintainers.
The two teeth function as a single unit with no freedom for vertical movement.
A broken stress space maintainer is designed to break this transmission of force and allows independent vertical movement of the teeth involved.
Less Commonly Used Space Maintainers:
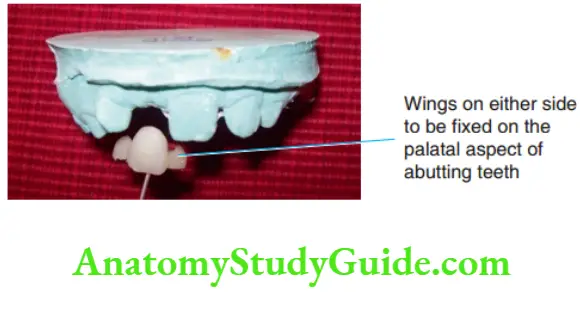
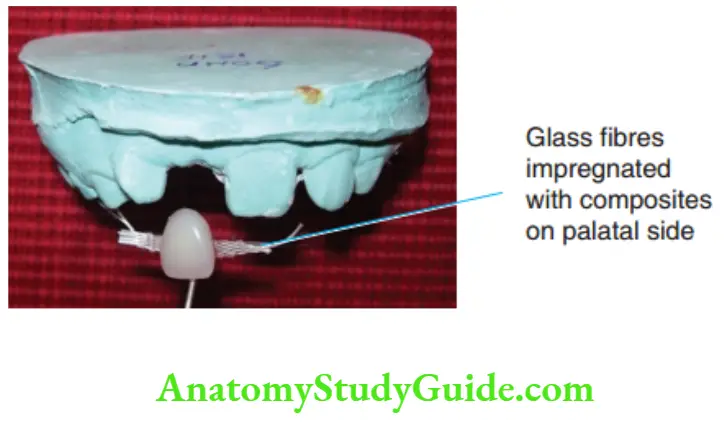
Less frequently used space maintainers include Maryland bridges, glass fire-reinforced space maintainers and cantilever bridges.
These simple and effective space maintainers can be prefabricated or fabricated chairside.
These are mainly used in the anterior region. A Cantilever bridge is an appliance where a butting tooth receives a crown to which a prosthetic tooth is attached.
Maryland bridges are mostly resin-reinforced bridges. They have a prosthetic tooth with resin or metal wings on either side.
These wings fit onto the palatal surfaces of abutting teeth on either side and are found using resins or other cementing agents.
Glass fire reinforced bridge utilises glass fires on palatal surfaces to fit a prosthetic tooth with its abutting teeth.
The fires are translucent and aesthetic. They are cemented with composite luting cement.
Management Of Deviation From Normalcy During Transition
Knowledge of the chronology of teeth, tooth formation and eruption and exfoliation data is a basic necessity for the identification of a deviation from normalcy.
As each individual’s biological timetable varies, a range of normalcy has to be allowed for every individual.
Details of milestones and general health status recorded in the patient’s history are valuable indicators.
Differentiation between ‘variations-within-acceptable-range’ and ‘deviations’ has to be identified prudently.
Problems Encountered During The Transition Phase:
1. Over-retained primary tooth: Over-retained tooth occupies space of the permanent tooth and leads to crowding and crossbites. such teeth are extracted when identified.
2. Delayed eruption of permanent teeth: The aetiology for the delay in eruption of permanent teeth could be systemic or local, requiring investigations.
The identified local aetiological factor like an impacted supernumerary tooth requires immediate removal.
3. Submerged tooth/submerged molar (ankylosed primary teeth): Submerged tooth is an over-retained or ankylosed tooth, mostly a molar, occurring due to either trauma or the missing successor tooth.
It affects the occlusal settlement of permanent dentition by not offering the critically required leeway space.
Occlusal surfaces of these primary teeth, molars in particular, lie below the occlusal plane and therefore cause supra eruption of the opposing teeth.
A crown is fabricated on this submerged tooth to prevent supra eruption.
4. Presence of supernumerary teeth: Supernumerary teeth affect the proper settlement of occlusion by occupying additional space in the arch.
They prevent the normal eruption process of permanent teeth in that region and need to be extracted at the earliest.
5. Ankyloglossia/tongue tie: Short lingual frenum restricts the free protrusive movement of the tongue.
Apart from affecting pronunciation, it also exerts a constant pull on the lingual interdental papilla of lower incisors, leading to a gingival recession in that region.
A frenectomy is done to relieve the short frenum.
6. High attachment of maxillary labial frenum: This results in median diastema and erosion of bone at the alveolar crest.
If the lifting of the lip and stretching of the frenum cause blanching of the incisive papillary region, a frenectomy is indicated.
7. Occlusal interference/occlusal prematurity: Occlusal interference can cause mandibular crossbite, later establishing a skeletal disharmony.
Wear facets in primary teeth are clues to this condition. Selective grinding is done after localising the premature contact.
Elective Extraction Procedures:
The primary dentition is gradually replaced by permanent teeth in sequential order during the transition phase of dentition.
The final occlusion of permanent dentition settles in an ideal way when factors such as arch size, teeth size and the order of replacement are normal.
But it is unfortunate that not all individuals have such an ideal arrangement.
Malocclusion results when the abovementioned factors do not correlate with each other.
Certain elective extraction procedures are suggested when such dissociation is observed.
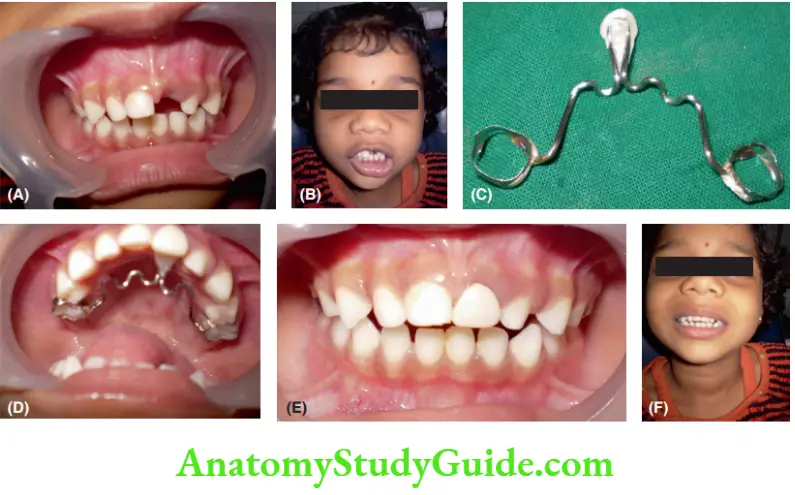
Space is provided for a newly erupting tooth by removing a primary tooth Patient with over-retained deciduous teeth.
obstructing its way space. The extractions are planned in three common ways for a smooth transition from deciduous dentition to permanent dentition. They are
- Serial extraction procedure
- Timed extractions
- Wilkinson’s extraction procedure
Serial Extraction Procedure:
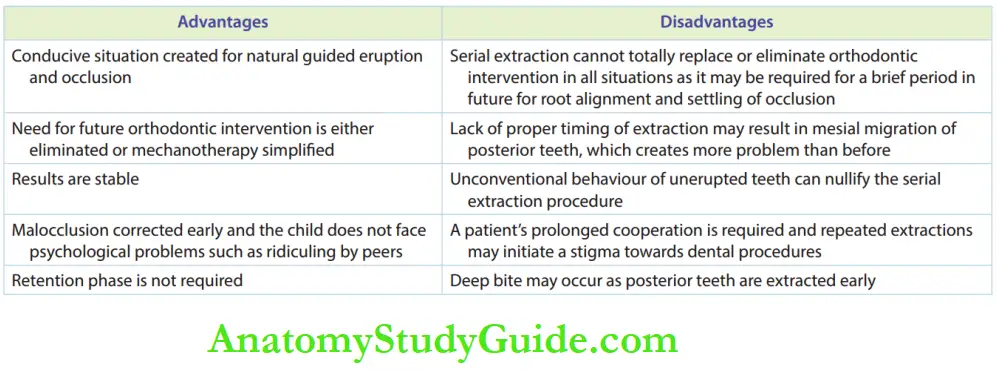
A serial extraction procedure can be described as a programme of selective extraction of deciduous and some permanent teeth over a period of time, with the objective of relieving crowding and facilitating the eruption of the remaining teeth into improved positions.
The concept was introduced by Bunon and the term ‘serial extraction’ was coined by Kjellgren and popularised by Nance.
Nance is called the father of serial extraction. Dewel described serial extraction as an orthodontic procedure that involves the orderly removal of selected primary and permanent teeth in a predetermined sequence.
Hotz suggested ‘Guidance of eruption as a better term for teeth are guided to occupy ideal positions by this procedure.
Unexfoliated primary teeth hinder the path of eruption of permanent teeth.
Inadequate space for erupting permanent teeth results in crowding.
Serial extraction provides adequate space for the emerging permanent teeth and allows them to attain a favourable self-guided position and alignment in the arch.
This simple, pre-planned, scheduled extraction procedure either eliminates or reduces the severity of malocclusion.
Future orthodontic treatment time and the need for complicated mechanotherapy are produced
Indications
Serial extraction is indicated in the following situations:
1. Mild-moderate tooth size–arch length discrepancy (TSALD): This occurs when the size of a tooth is larger for the given arch length.
The signs of this discrepancy are as follows:
- Crowded/closed deciduous dentition
- Lingual eruption of the permanent lateral incisor
- Unilateral loss of deciduous canine leading to the possibility of midline shift
- The gingival recession of lower deciduous incisors
- Permanent canine erupting over the lateral incisor
- Proclamation of erupting permanent anterior teeth
2. Class I malocclusion
Contraindication:
The following are the contraindications of the serial extraction procedure:
- Skeletal discrepancy
- Severe tooth size–arch length discrepancy beyond capabilities of providing space through serial extraction.
- Open bite and deep bite
- Spacing is anticipated in case of congenital absence of teeth. Periodic observation is sufficient when adequate spacing is present
- Clef lip and cleft palate conditions: Clef alveolus disrupts dental lamina and leads to unpredictability in terms of size, shape and number of teeth in the clef region. Congenital absence of teeth is common in the cleft alveolus. The serial extraction procedure does not benefit such cases
Prerequisite Records:
Diagnostic casts are required to quantify the discrepancy by application of mixed dentition analysis.
The model analysis is indispensable for assessing the discrepancy between mesiodistal dimensions of deciduous and permanent teeth.
A radiographic examination is necessary for all analyses. IOPA may help sometimes.
The lateral cephalogram rules out the skeletal discrepancy. Orthopantomogram (OPG) helps in checking the presence and position of all permanent teeth to avoid iatrogenic malocclusions.
depicts an OPG where the left lower fist premolar has been extracted as a part of a serial extraction
procedure, without verifying the unfavourably impacted permanent canine.
Procedure:
There are three established methods of serial extraction

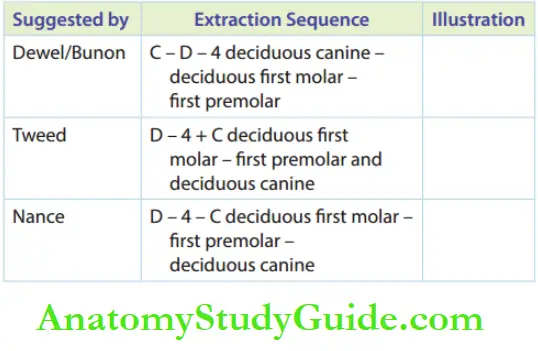
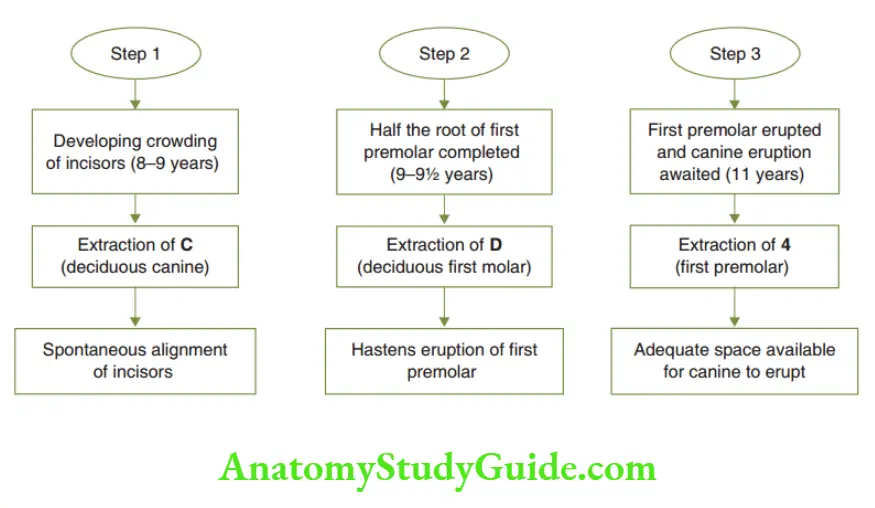
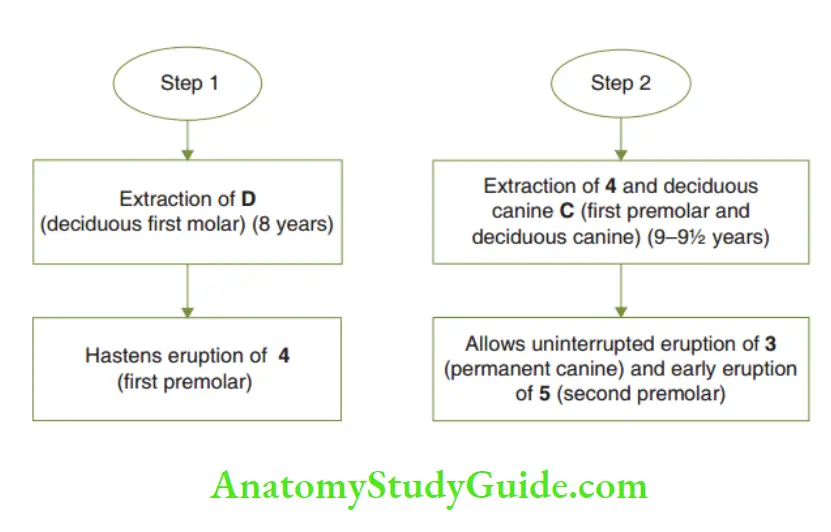
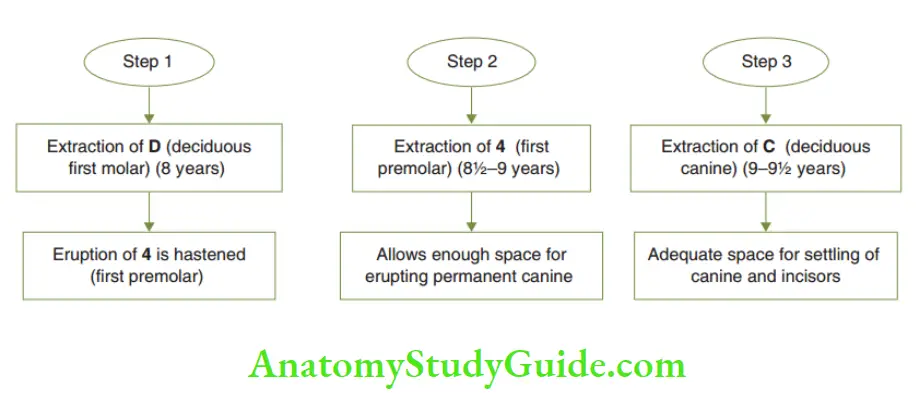
A modification of Dewel’s method is suggested when a permanent canine erupts before premolar.
With the evidence of eruption of permanent canine ahead of the first premolar, the primary fist molar is extracted.
The first premolar is enucleated or it is removed from the socket even before the eruption.
Tweed’s and Nance’s methods are indicated in the mandibular arch only.
Normally, lower canines erupt before premolars. First premolars are hastened to erupt before canines in these two methods.
The advantages and disadvantages of serial extraction are listed. Despite its disadvantages, serial extraction is a recommended procedure for a properly motivated patient.
Timed Extraction:
Timed extraction is a procedure where the primary anterior teeth are extracted when there is evidence of the eruption of the corresponding permanent teeth palatal or lingual to.
This procedure differs from the serial extraction procedure in the following ways:
The permanent teeth are not extracted.
Extraction is carried out in the anterior or incisor region only.
Serial extraction includes the extraction of posterior teeth to allow space for canines.
Wilkinson’s Extraction:
According to Wilkinson, the first permanent molar is more susceptible to caries.
All the first permanent molars are extracted by around 8–9 years of age.
The second permanent molar makes a bodily movement within the alveolus erupt in place of the extracted first permanent molar.
The space of the second permanent molar is said to be utilised by the third molar.
This procedure is performed to avoid frequent impaction of the third molar due to a lack of space.
However, the third molars are the most unpredictable teeth in terms of presence, size and shape.
Extraction of the first permanent molar without confirming the presence and position of the third molar makes this procedure less desirable.
Moreover, the advantage of the first permanent molar serving as an anchor unit for future orthodontic treatment is also lost in this procedure.
Summary
1. Paediatric orthodontics concentrates on preventive and interceptive orthodontics.
2. Potential disturbing conditions during the transition phase:
- Poor oral hygiene and dental caries susceptibility,
- early loss of a tooth,
- over-retained primary tooth,
- delayed eruption of permanent teeth,
- ankylosed tooth,
- ankyloglossia,
- premature occlusal interference,
- teeth size–arch length discrepancy,
- high frenal attachment,
- supernumerary tooth and
- altered shape and size of the tooth.
3. Space maintainers are passive appliances or restorations that occupy and hold mesiodistal space left by a prematurely lost tooth or decayed tooth material.
4. When a space maintainer prevents supereruption of the tooth in the opposing arch into the space, it is called a ‘functional space maintainer’.
5. A partial denture serves as a space maintainer.
6. Distal shoe maintainer ( D S M): A space maintainer with an intra-alveolar wire extending at its distal shoe end, guiding a lower first permanent molar while maintaining the space of a lower second primary molar.
Broken stress space maintainer: Breaks stress transmission from one part to the other part of an appliance.
8. Fixed unilateral space maintainers: Crown and loop space maintainer, band and loop space maintainer, crown and bar space maintainer, band and bar space maintainer, distal shoe appliance.
9. Fixed bilateral non-functional space maintainers: trans palatal arch (TPA), Nance space holding arch, lower lingual holding arch.
10. Space maintainer is held until signs of the eruption of the permanent tooth are sighted and confirmed with radiographs.
11. Serial extraction is a concept introduced by Bunon. Nance is called the ‘father of serial extraction’.
12. Dewel’s method: C – D – 4; Tweed’s method: D – (4 + C); Nance’s method: D – 4 – C.
Leave a Reply