Principles Of Surgical Access To Root Structure
Normally, when the radiolucent area is present periodically, the root is visible through the cortical plate. But if periapical radiolucency is not present, then the bone is to be removed to gain access to the root. Guidelines to be strictly followed for determining the location of root apex are
Table of Contents
- Assess the angulation of the crown to the root
- Measure the entire tooth to root length
- Locate the root from coronal to the apex where bone covering root is thinner. Once it is located, then remove the covering bone with light brush strokes working in an apical direction
- Expose radiographs from diffrent angles
- Probe the apical region using an endodontic explorer or straight curette to know whether a small defect is present or not
- If a small defect is present in the bone, then place a small piece of lead sheet, gutta-percha point, or plug of alloy to know the position of the apex.
Read And Learn More: Endodontics Notes
Periradicular Curettage
It is a surgical procedure to remove diseased tissue from the alveolar bone in the apical or lateral region surrounding a pulpless tooth.

- (A) Preoperative radiograph;
- (B) Obturation;
- (C) Mucoperiosteal flap raised;
- (D) Window preparation in 11;
- (E) Periapical curettage;
- (F) Sutures placed.
Indications
- Access to the root structure for additional surgical procedures
- For removing the infected tissue from the bone surrounding the root
- For removing overextended filings
- For removing necrotic cementum
- For removing a long-standing persistent lesion especially when a cyst is suspected
- To assist in rapid healing and repair of the periradicular tissues.
Surgical Technique
- Give local anesthesia, design a flap, and expose the surgical site
- Use a bone curette to remove the pathologic tissue surrounding the root. Insert curette between soft tissue and bone, apply pressure against the bone
- After removing the tissue from the bony area, grasp the soft tissue with the help of tissue forceps and send it for histopathological examination.
Root-End Resection
An apicoectomy is the surgical resection of a tooth and its removal together with pathological periapical tissue.
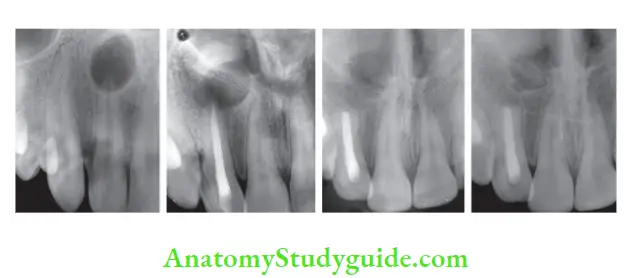
- (A) Preoperative radiograph;
- (B) Post obturation radiograph;
- (C) Radiograph after periapical surgery and root resection;
- (D) Follow-up after 12 months showing a decrease in size of periapical radiolucency.

- (A) Preoperative radiograph showing periapical radiolucency;
- (B) Radiograph after obturation;
- (C) Follow-up 6 months after surgery;
- (D) Follow-up 12 months after surgery.

- (A) Preoperative radiograph;
- (B) After removal of previous root canal filing;
- (C) Postobturation radiograph;
- (D) After elevation of flap;
- (E) After cyst enucleation and root-end resection.
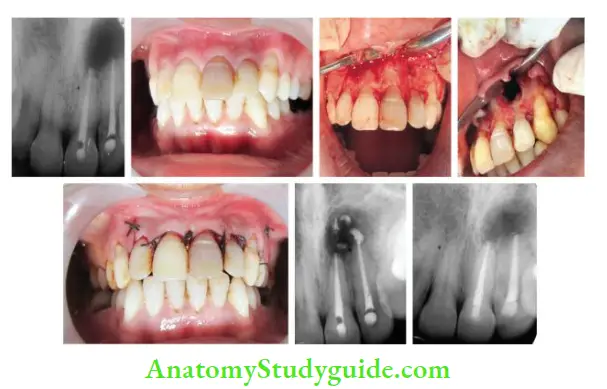
- (A) Radiograph showing obturation of maxillary central and lateral incisor;
- (B) Preoperative photograph;
- (C) Raising the flap;
- (D) Curettage of the periapical lesion;
- (E) Postoperative photograph;
- (F) Postoperative radiograph;
- (G) Follow-up radiograph after 3 months.
Indications
- Inability to perform nonsurgical endodontic therapy due to anatomical, pathological, and iatrogenic defects in root canal
- Persistent infections after conventional endodontic treatment
- Need for biopsy
- Need to evaluate the resected root surface for any additional canals or fracture
- Medical reasons
- Lack of time
- For removal of iatrogenic errors like ledges, fractured instruments, and perforation which are causing treatment failure
- For evaluation of the apical seal
- Blockage of the root canal due to calcifi metamorphosis or radicular restoration.
Factors to be Considered Before Root-end Resection
Instrumentation
A high-speed handpiece with surgical length fissure bur is preferred because round bur may result in gouging of the root surface.
Nowadays, the use of Er: YAG laser for root-end resection is recommended as it produces a clean and smooth root surface, decreases the permeability of root surface and reduces postoperative pain and discomfort.
Extent of Resection
According to Cohen et al., the length of root tip resection depends upon the frequency of lateral canals and apical ramifications at the root end. It was found that when apical 3 mm is resected, lateral canals are reduced by 93% and apical ramifications by 98%.
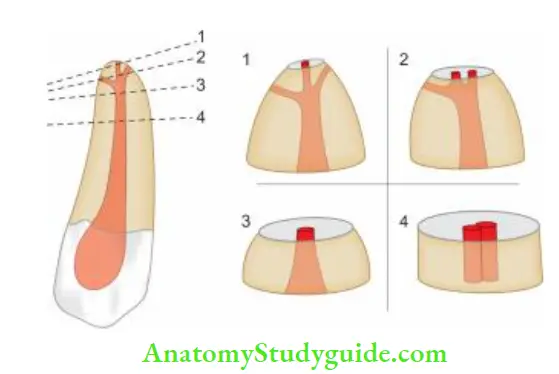
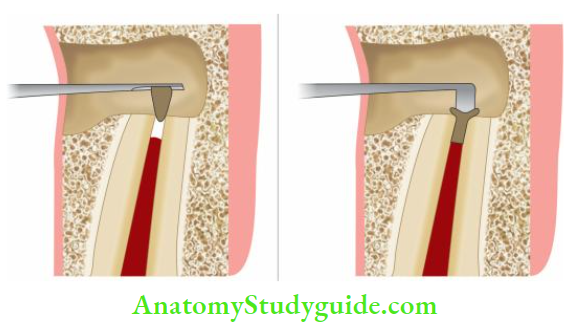
The angle of Root-End Resection
Earlier it was thought that root-end resection at 30–45° from the long axis of the root facing buccally or facially provides improved accessibility and visibility of resected root end.
But studies have shown that beveling of the root end results in the opening of dentinal tubules on the resected root surface which communicate with root canal space, causing apical leakage even after retrofitting is done.
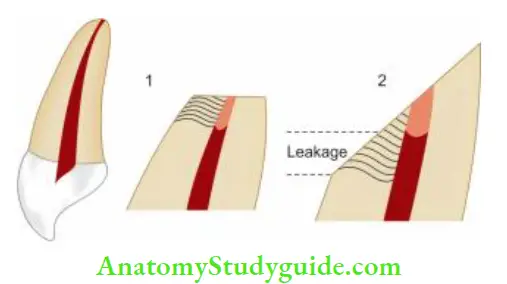
So, a bevel of 0–10° is recommended for resection because
- It allows the inclusion of lingual anatomy with less reduction
- If multiple canals are present, an increase in bevel causes an increase in distance between them
- With a short bevel, its easier to keep instruments within the long axis of the tooth (so to avoid unnecessary removal of radicular dentin) than with a long bevel
- Long bevel exposes more dentinal tubules to the oral environment resulting in microleakage over a period of time
Root-End Preparation
The main objective of root-end preparation is to create a cavity to receive root-end filing. Root-end preparation should accept filing materials so as to seal of the root canal system from periradicular tissues.
Car and Bentkover defined an ideal root-end preparation as “a class 1 preparation at least 3.0 mm into root dentine with walls parallel to a coincident with the anatomic outline of the pulp space”.
Five requirements are suggested for a root-end preparation to fulfill:
- Apical 3 mm of root canal must be cleaned and shaped
- Preparation must be parallel to the anatomic outline of the pulp cavity
- Creation of an adequate retention form
- Removal of all isthmus tissue if present
- The remaining dentine walls should not be weakened
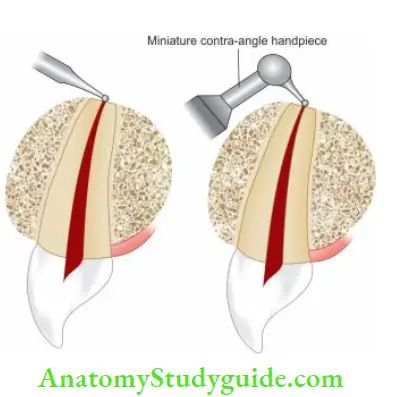
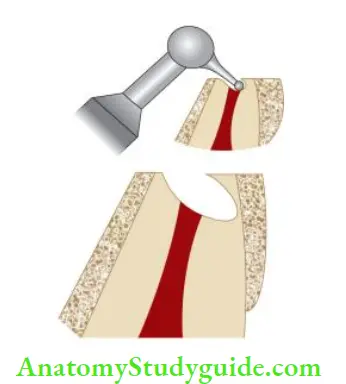
Traditional Root-End Cavity Preparation
A miniature contra-angle or straight handpiece with a small round or inverted cone bur is used to prepare a class I cavity at the root end within confines of the root canal.
Though, these preparations seem to be placed along the long axis of the tooth, they are directed palatally causing perforations
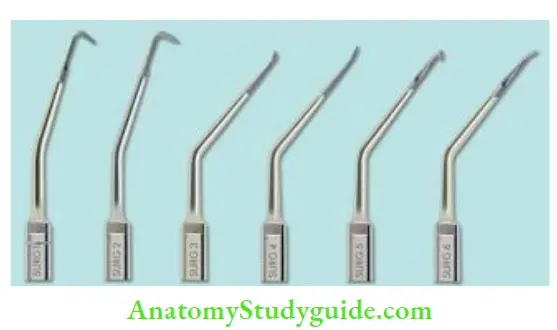
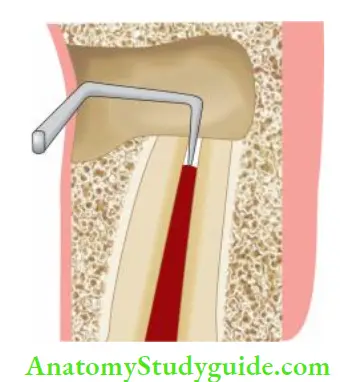
Ultrasonic Root-End Preparation
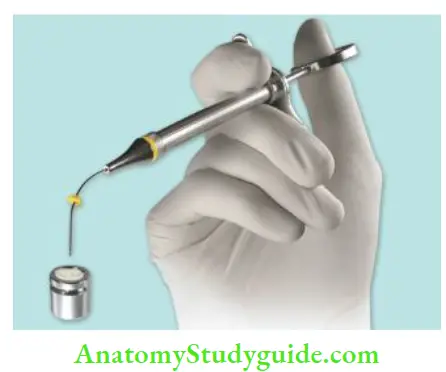
It was developed to resolve the main shortfalls of bur preparation. In this, specially designed ultrasonic root-end preparation instruments are developed which result in smaller preparation size with minimal bevel, parallel walls for better retention, and less debris and smear layer than those prepared with a bur.
Retrograde Filling
The main aim of nonsurgical or surgical endodontics is three-dimensional obturation of the root canal system. Therefore, after apical surgery, the placement of a root-end filling material is an equally important step. To place a material in the retro preparation, it is mixed in the desired consistency, placed into the retro preparation, and compacted with the help of a burnisher.
After it is set, the excess is removed with a carver or periodontal curette. Finally, the root-end filing is finished with carbide finishing bur and a radiograph is taken to confirm the correct placement of the filing.
Root-End Filling Materials
An ideal root-end filling material should
- Be well tolerated by periapical tissues
- Adhere to the tooth surface
- Be dimensionally stable
- Resist dissolution
- Promote cementogenesis
- Be bactericidal or bacteriostatic
- Be noncorrosive and electrochemically inactive
- Not stain tooth or periradicular tissue
- Be readily available and easy to handle
- Allow adequate working time, then set it quickly
- Be radiopaque
Commonly used root-end filling materials
- Amalgam
- Gutta-percha
- Gold foil
- Titanium screws
- Glass ionomers
- Zinc oxide eugenol
- Cavit
- Composite resins
- Polycarboxylate cement
- Poly HEMA
- Super ethoxy benzoic acid (EBA)
- Mineral trioxide aggregate (MTA)
Amalgam
It is one of the most popular and widely used retrograde filling materials since the last century.
Amalgam Advantages
- Easy to manipulate
- Readily available
- Well tolerated by soft tissues
- Radiopaque
- Initially provides a tight apical seal
Amalgam Disadvantages
- Slow setting
- Dimensionally unstable
- It shows leakage
- Stains overlying soft tissues, resulting in the formation of tattoo
- More cytotoxic than IRM, super EBA, or MTA
Zinc Oxide Eugenol Cement
Unmodified ZOE cement is weak and has a long setting time and high water solubility. In contact with moisture, it releases free eugenol which is responsible for most of the effects caused by zinc oxide eugenol cement.
Intermediate Restorative Material
- The intermediate restorative material is a ZOE cement reinforced by the addition of 20% polymethacrylate by weight to zinc oxide powder.
- It shows low water solubility, and milder reaction than unmodified ZOE cements.
Super Ethoxybenzoic Acid
It is a ZOE cement modified with EBA to alter the setting time and increase the strength of the mixture.
Super Ethoxybenzoic Acid Advantages
- Low solubility and non-resorbable
- Radiopaque
- Strongest and least soluble of all ZOE formulations
- Yield high compressive and tensional strength
Super Ethoxybenzoic Acid Disadvantages
- Difficult to manipulate because setting time is short and greatly affected by humidity
- Tends to adhere to all surfaces so difficult to place
Mineral Trioxide Aggregate
- Mineral trioxide aggregate (MTA) is composed of tricalcium silicate, tricalcium aluminate, tricalcium oxide, bismuth oxide, and silicate oxide
- Its pH is 2.5 (when set) and the setting time is 2 h 45 min.
MTA Placement Technique
Mix MTA powder and liquid and carry it to the cavity with an amalgam carrier or messing gun compact it using microbloggers and clean the surface with a damp cotton pellet
MTA Placement Technique Advantages
- Excellent biocompatibility, in contact with periradicular tissues, it forms cementum
- Hydrophilic so not adversely affected by blood or moisture
- Radiopaque
- MTA Placement Technique DisadvantagesMore difficult to manipulate
- Longer setting time
- Expensive
Composite Resins
- Though composite resins have shown superior physical properties but they are very technique sensitive.
- Since it is very difficult to obtain a total dry field, their use is not encouraged as root-end filling material.
Reapproximation Of The Soft Tissue
Following surgery, a final inspection of the root-end filling and cleaning of the surgical site is done and a radiograph is taken to assess the presence of any root fragments or surplus root-end filling material.
Repositioning of the Flap
The flap is replaced in the original position with the incision lines approximated as close as possible.
Now flap is compacted by applying light yet firm pressure for 2–5 min with the help of damp surgical gauze. This compression helps in an approximation of the wound edges and their initial adhesion.
Leave a Reply