Pulpal Regeneration Techniques
- Once the pulp gets exposed, the aim of the treatment is to promote pulp tissue healing and preserve pulp vitality. Young permanent teeth are teeth that have recently erupted and where apical physiological root closure has not occurred.
- Normal physiological closure may take 2–3 years after the eruption. In such teeth, if there is an injury to the pulp, the aim of the treatment is to preserve the pulp vitality and promote healing.
- Vital pulp therapy procedures involve the removal of irritants of the pulp and placement of a protective material directly or indirectly over the pulp followed by tight-sealed restoration.
- Vital pulp therapy is performed to treat reversible pulpal injury to promote root formation and apical closure. Nonvital pulp therapy, that is, specification and pulpectomy are indicated if irreversible damage to the pulp has occurred.
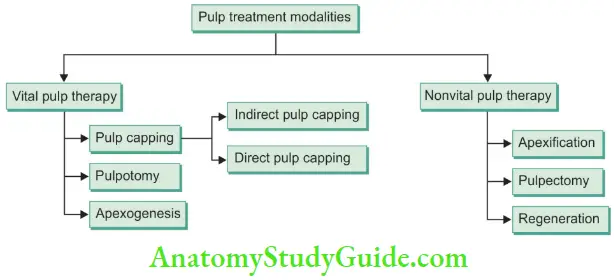
Table of Contents
Vital Pulp Therapy
Vital Pulp Therapy Definition: Vital pulp therapy is defined as a treatment that aims to preserve and maintain pulp tissue that has been compromised but not destroyed by caries, trauma, or restorative procedures.
It is specially indicated for young permanent teeth because of the high healing capacity of pulp tissue compared to older patients.
Dental pulp forms secondary dentin, peritubular dentin, and reparative dentin in response to biological and pathologic stimuli; it also keeps the dentin moist which in turn ensures the resilience and toughness of the dentin.
Also, the vital pulp provides protective resistance to mastication forces compared to endodontically treated teeth. So, it is always preferred to maintain the vitality of the pulp unless it is unavoidable.
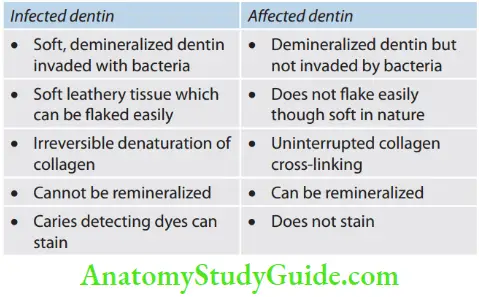
One should take care that the management of deep carious lesions approaching the pulp necessitates the removal of infected dentin while keeping the affected dentin to avoid inadvertent pulp exposure. Summarizes the differences between infected and infected dentin. Commonly used techniques for vital pulp therapy are pulp capping and pulpotomy.
Differences Between Infected And Affected Dentin.
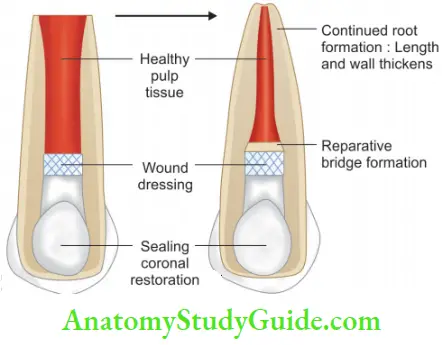
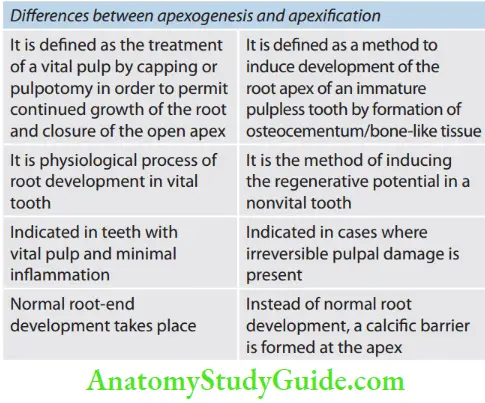
Apexogenesis
Apexogenesis is defined as the treatment of vital pulp by capping or pulpotomy to permit continued growth of root and closure of root apex.
Pulpotomy
According to Finn (1995), pulpotomy refers to the complete removal of the coronal portion of the dental pulp followed by the placement of a suitable medicament that will promote healing and preserve tooth vitality.
- Pulpotomy Rationale
- Maintain the integrity of radicular pulp tissue to allow continued root growth
- Pulp of immature teeth has significant reparative potential
- Pulp revascularization and repair occur more efficiently in teeth with open apex
- Root-end closure occurs in a tooth with vital pulp and minimum inflammation.
- Pulpotomy Objectives
- To maintain the vitality of the pulp to help root maturation
- Promote root-end closure and natural apical constriction
- Sustain a viable Hertwig’s epithelial root sheath to allow root development
- Form a dentinal bridge at the site of pulpotomy.
- Pulpotomy Indications
- Traumatized or pulpal involved vital permanent tooth with open apex
- Clinical and radiographic signs of radicular pulp vitality
- Pain, if present, is neither spontaneous nor persists after the removal of the stimulus
- No or easy-to-control hemorrhage from the amputation site.
- Pulpotomy Contraindications
- Symptoms of irreversible pulpitis
- Nonrestorable crown structure
- Pulp necrosis with radiolucency in furcal or periradicular areas
- Presence of purulent discharge
- Spontaneous pain
- Tenderness to percussion
- Mobility.
- Pulpotomy Criteria for Successful Pulpotomy
- No radiographic evidence of internal root resorption
- No radiographic sign of periradicular periodontitis
- Tooth should respond to pulp testing
- Tooth should be asymptomatic.
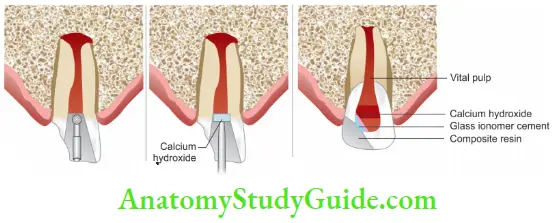
1. Cvek Pulpotomy/Partial Pulpotomy/Calcium Hydroxide Pulpotomy/Young Permanent Partial Pulpotomy
It was given by Cvek in 1993. Cvek showed that, with pulp exposures resulting from traumatic injuries, pulpal changes are characterized by a proliferative response with inflammation extending only a few millimeters into the pulp, whereas in teeth with carious exposure of the pulp, it may be necessary to remove pulpal tissue to a greater depth to reach noninflamed tissue.
- Cvek Pulpotomy Procedure
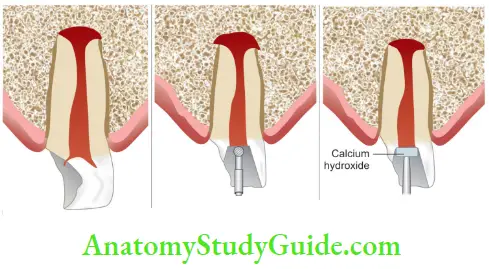
-
- Anesthetize and isolate the tooth
- Remove carious lesion with a slow speed round bur
- Remove the coronal pulp and control hemorrhage using sodium hypochlorite and moistened cotton pellets with slight pressure.
- Place calcium hydroxide or MTA over the amputation site
- If calcium hydroxide is placed, recall the patient, check dentin bridge formation, and place a permanent restoration
2. Cervical Pulpotomy/Complete Pulpotomy
- In young permanent teeth, a cervical pulpotomy is performed to allow root maturation. The procedure is performed in teeth in which it is assumed that healthy pulp tissue, with the potential to produce a dentin bridge and complete the formation of the root, still remains in the canal
- The technique is the same as that of partial pulpotomy except that it is up to root orifice.
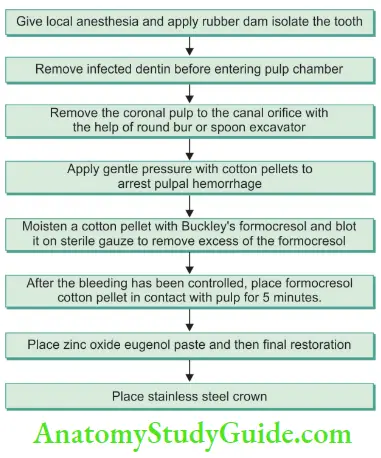
3. Formocresol Pulpotomy
It was introduced in 1904 by Buckley. He found that equal parts of formalin and tricresol would react chemically with the products of pulp inflammation to form a non-infective compound of a harmless nature. Sweet popularized this technique in 1930. It is preferred in primary teeth due to high (98%) clinical and radiographic success rate.
- Buckley’s formocresol consists of
- Formaldehyde 19%
- Tricresol 35%
- Glycerin 15%
- Water 31%
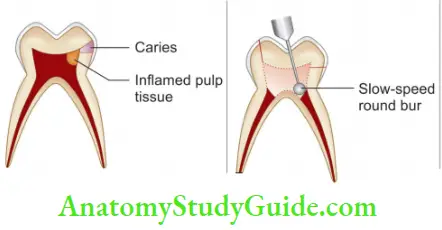
1. Tooth showing deep caries with inflamed pulp tissue
2. Remove coronal pulp till the orifice of the canals using round bur;
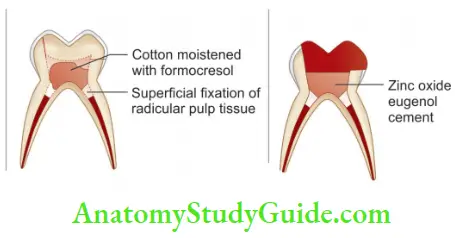
3. Place a cotton pellet moistened with formocresol on pulp tissue;
4. Place zinc
The technique of formocresol pulpotomy is shown.
4. Mechanism of Action
Formocresol is an effient bactericide. It has the ability to prevent tissue autolysis by the complex chemical binding of formaldehyde with peptide groups of side chain amino acids without changing the basic structure of protein molecules.
After 7 days of application, the pulp shows three distinct zones:
- Broad eosinophilic zone of fiction
- Broad pale-staining zone with poor cellular definition
- Zone of inflammation diffusing apically into normal pulp tissue. After 60 days, in a limited number of samples, the remaining tissue was believed to be completely field, appearing as a strand of eosinophilic fibrous tissue
5. Two-Visit Pulpotomy
It is used in cases of profuse and difficult-to-control bleeding. In this, paraformaldehyde paste is used which consists of:
- Paraformaldehyde—1 g
- Lignocaine—0.06 g
- Carmine—10 g
- Propylene glycol—0.5 mL
- Carbowax 1500—1.3 g
- Two-Visit Pulpotomy Technique
The procedure is same as for one-visit formocresol pulpotomy till hemorrhage control except for the following changes:
- Place cotton pellet moistened with paraformaldehyde over the pulpal exposure
- Place paraformaldehyde mixed with zinc oxide eugenol for 1–2 weeks. Formaldehyde vapors fi the tissues
- At the second visit, remove the cotton pellet and clean the pulp chamber with hydrogen peroxide. Alternatively, use an antiseptic dressing (equal parts of eugenol and formocresol with zinc oxide)
- Place IRM or glass ionomer cement over it
- Restore the tooth with stainless steel crown
- Other Materials Used for Pulpotomy
- Glutaraldehyde
- Ferric sulfate
- MTA
- Bone morphogenic proteins
- Laser
- Electrosurgical pulpotomy
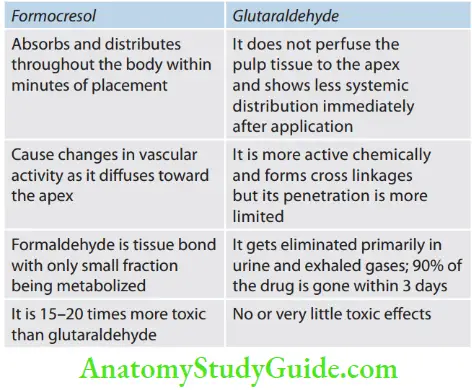
- Glutaraldehyde
It was suggested by Gravemade. Glutaraldehyde (2–4%) produces rapid superficial fiction of the underlying pulpal tissue. Unlike formoterol, a large percentage of the underlying pulpal tissue remains vital and free from inflammation. A narrow zone of eosinophilic, stained, and compressed, fied tissue is found directly beneath the area of application that bends into vital, normal-appearing tissue apically. With time, the glutaraldehyde field zone is replaced through macrophagic
action with dense collagen tissues; thus, the entire root canal tissue is vital - Differences Between Formocresol and Glutaraldehyde
- Ferric sulfate pulpotomy
- Ferric sulfate has been used due to its hemostatic effect. Due to its effct of controlling hemorrhage, it might minimize the chances of inflammation and internal resorption. In this, remove the coronal pulp, achieve hemostasis with a wet cotton pellet, and place 15.5% solution of ferric sulfate over the pulp stump for 10–15 seconds. Then rinse the pulp stump, dry it with a cotton pellet, and cover with zinc oxide eugenol and followed by permanent restoration.
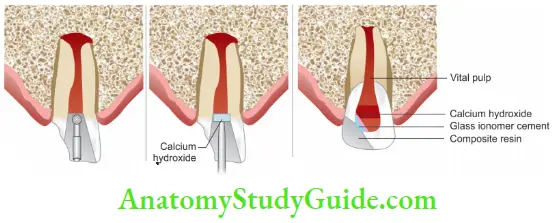
- Calcium hydroxide pulpotomy
- Harmann (1930) demonstrated the formation of reparative dentin over amputated vital pulps capped with calcium hydroxide. Calcium hydroxide is not a preferred dressing for pulpotomies in primary teeth because of the limited clinical success rate. Heilig et al. (1984) suggested that internal resorption results from the “embolization” process by which particles of calcium hydroxide work their way deep into the pulp tissue, forming focal points of inflammation.
- Technique: Place calcium hydroxide paste in chamber and press it with a sterile cotton pledge. Over it place resin-modified glass ionomer restoration.
- Harmann (1930) demonstrated the formation of reparative dentin over amputated vital pulps capped with calcium hydroxide. Calcium hydroxide is not a preferred dressing for pulpotomies in primary teeth because of the limited clinical success rate. Heilig et al. (1984) suggested that internal resorption results from the “embolization” process by which particles of calcium hydroxide work their way deep into the pulp tissue, forming focal points of inflammation.
- MTA pulpotomy
- MTA is more recent material used for pulpotomies with a high rate of success. It has excellent biocompatibility, an alkaline pH, radiopacity, and high sealing ability, and promotes regeneration of the original tissues when placed in contact with the dental pulp or periradicular tissues.
- Technique: Isolate the tooth with a rubber dam and remove the coronal pulp. Place the MTA over the pulp stump and close the tooth with temporary cement until the apex of the tooth close.
- MTA is more recent material used for pulpotomies with a high rate of success. It has excellent biocompatibility, an alkaline pH, radiopacity, and high sealing ability, and promotes regeneration of the original tissues when placed in contact with the dental pulp or periradicular tissues.
- Bone morphogenic proteins (BMPs)
- BMPs stimulate the induction and differentiation of mesenchymal cells with varying degrees of dentinal bridge formation.
- Laser pulpotomy
- Laser (erbium family, diode, Nd: YAG, CO2) can be used for the coagulation of pulp tissue over the pulp stump before the placement of zinc oxide eugenol or IRM. Clinical studies show either no significant difference between laser pulpotomy and conventional pulpotomy or in favor of laser pulpotomy. After removal of coronal pulp, hemorrhage is controlled with the laser, and capping material like MTA, zinc oxide, eugenol, or IRM is applied.
- Electrosurgical pulpotomy
- After the removal of the coronal pulp, the remaining tissues are cauterized with an electrocautery unit. The pulp chamber is filled with zinc oxide eugenol or IRM. It is a non-pharmacological method; cautery carbonizes and heat denatures the pulp and bacterial contamination.
- Glutaraldehyde
Apexification (Root-End Closure)
Apexification is the process of inducing the development of the root and the apical closure in an immature pulpless tooth with an open apex. It is different from apexogenesis in that in latter root development occurs by a physiological process.
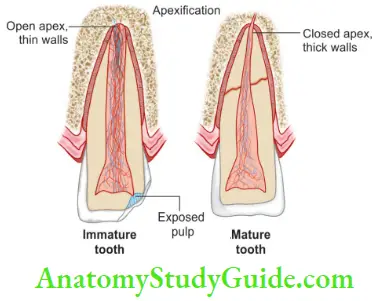
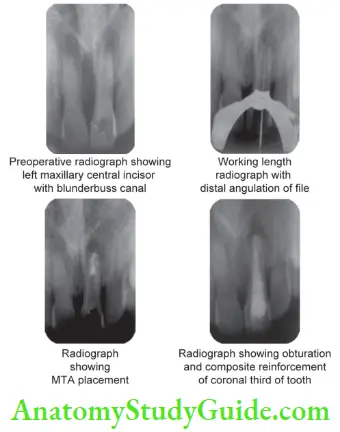
Apexification is defined as the method to induce a calcified barrier across an open apex of an immature pulpless tooth. Apexification is most commonly performed in traumatized incisors that have lost vitality, carious exposure, and in teeth with variations such as dens invagination with an immature root.
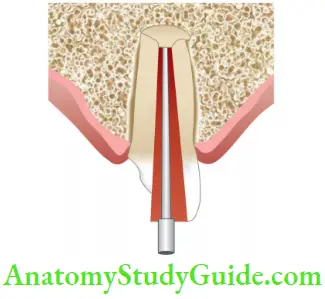
Apex in young permanent teeth may present two morphological variations; divergent with flying apical foramen (blunderbuss apex) and parallel to convergent apex. In both cases, conventional root canals cannot be performed.
- In young permanent teeth, specification is preferred over root canal treatment because
- Apex is funnel-shaped with an apical part wider than the canal
- Canal walls are thin and fragile
- Absolute dryness of the canal is difficult to achieve
- Objectives of Apexifiation
The main objective of apexification is to achieve an apical stop for obturating material. This apical step can be obtained by- Inducing natural calcified barrier at the apex or short of the apex
- Forming an artificial barrier by placing material at or near the apex
- Inducing the natural root lengthening by stimulating Hertwig’s epithelial root sheath
- Rationale of Apexifiation
- The main aim of apexification is to preserve Hertwig’s root sheath and apical pulp tissue.
- It is based on the fact that after the completion of root formation. Hertwig’s epithelial root sheath (HERS) disintegrates and its remnants remain at the apical end of root.
- HERS is considered to be highly resistant to infection, so even if the tooth is nonvital, viable HERS may be present at the apex which can help in further root development.
- In apexification, it is always suggested to complete biomechanical preparation 2 mm short of the radiographic apex to avoid any trauma to the apical pulp or her tissue present in that area.
- In cases when damage has already occurred to HERS, root formation cannot take place of its own. In such cases, an artificial barrier is created by placing a material in the apical portion. Hard barrier or calcified barrier which is formed in apexification has shown to possess a “Swiss cheese configuration.” It may mimic dentin or cementum or bone.
- Apexifiation Indications
In young permanent tooth with blunderbuss canal having:- Symptoms of irreversible pulpits
- Necrotic pulp
- Pulpoperiapical pathology with swelling, tenderness, or sinus
- Apexifiation Contraindications
- Teeth with vital pulp
- Teeth with very short roots and compromised periodontium
- Materials Used for Apexification
- Calcium hydroxide
- Calcium hydroxide in combination with other drugs like
- Camphorated paramonochlorophenol
- Cresanol
- Anesthetic solution
- Normal saline
- Ringer’s solution
- Zinc oxide paste
- Antibiotic paste
- Tricalcium phosphate
- Collagen calcium phosphate gel
- MTA
- Osteogenic protein 1 and 2
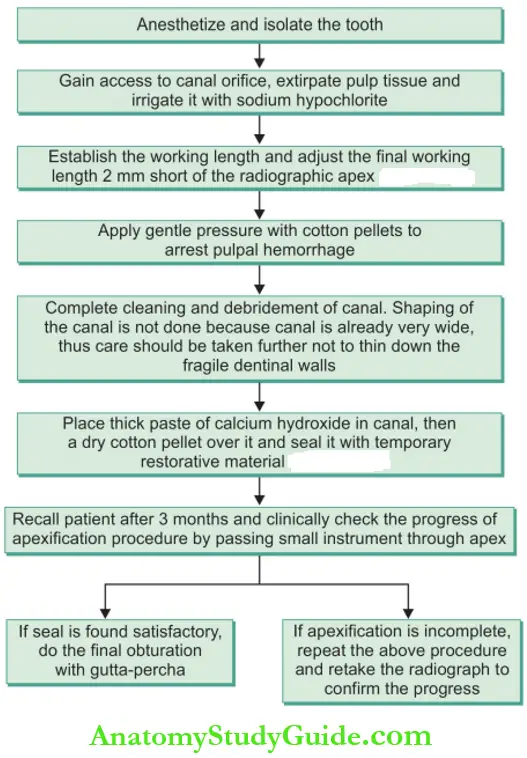
- Apexifiation Technique
Purpose of apexification is to induce root-end closure. It can be achieved in two ways viz; long-term procedure using calcium hydroxide dressing to allow the formation of a hard tissue barrier or as a short-term procedure creating an apical plug of MTA. - Long-Term Apexifiation Using Calcium Hydroxide
Apexification is traditionally performed using a calcium hydroxide dressing that disinfects the root canal and induces apical closure. High pH and low solubility retain its antimicrobial effect for a long time. Calcium hydroxide assists in the debridement of the root canal because it increases the dissolution of necrotic tissue when used alone or in combination with sodium hypochlorite. This procedure requires multiple visits and could take a year or more to achieve a complete apical barrier that will allow root canal filing using gutta-percha and sealer. The time needed for apexification depends on, the stage of root development and the status of the periapical tissue. The clinical technique of apexification using Calcium Hydroxide is shown.
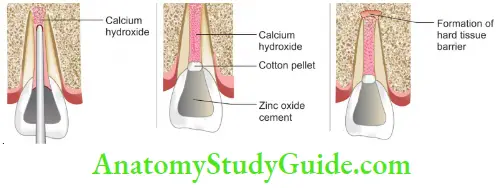
Types of Closure Which Can Occur during Apexification
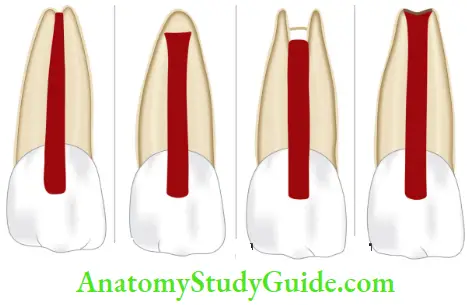
- Root-end development in normal pattern
- Apex closes but is wider at the apical end
- Development of calcifi bridge just coronal to the apex
- Formation of thin barrier at or close to the apex
- The time taken for this process for completion may range from 6 weeks to 18 months. Th final obturation of the canal should be carried out when there is
- Absence of any symptoms
- Absence of any fitula or sinus
- Absence or decrease in mobility
- Evidence of firm stop both clinically as well as radiographically
- Obturation in such teeth using lateral condensation is not advocated because the lateral pressure during compaction of gutta-percha may fracture the teeth. In such teeth, the vertical compaction method of obturation is preferred
- Since the dentinal walls are weak in such cases, restoration should be designed to strengthen the tooth. To strengthen the root, gutta-percha should be removed below the alveolar crest, the dentin is acid etched and then composite resin is placed. Placement of posts in such cases should be avoided as far as possible
- Short-Term Apexifiation with MTA (One-Visit Apexifiation)
MTA reduces the time needed for completion of the root canal treatment and restoration of the tooth. Apical barrier is achieved in one visit and the entire treatment is completed in a few visits. Care should be taken to perform complete debridement and disinfection of root canal and dentin walls because it is very difficult to remove MTA after it sets; if at all retreatment is required, it is done by apical surgery. The advantages of this technique are that patient compliance is less crucial, dentin does not lose its physical properties, and it allows earlier restoration and thus minimizing the likelihood of root fracture.
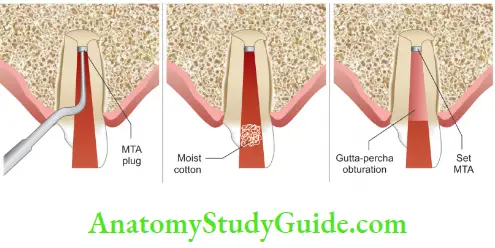
- MTA Apexifiation Technique
-
- Carry the MTA using a special carrier and compact 2-mm thick plug of MTA into the apical 4–5 mm using hand condensers or ultrasonic activation
- Cover MTA with wet cotton pellet and seal the tooth with a temporary restoration
- Differences between abiogenesis and specification
- After a few days, obturate the root canal filling using warm gutta-percha and give coronal restoration
.
Revascularization
- This new approach for treatment of immature necrotic and infected permanent teeth is based on the observation of spontaneous revascularization that occasionally occurs in the immature teeth after traumatic injury.
- With revascularization, root lengthening and apical closure with thickening of the canal walls is expected, thus improving the long-term of the young tooth. The nature of the hard tissue formed is not clear and can be cementum-like instead of dentin.
- The first step of the treatment is disinfection of the root canal space with sodium hypochlorite and using intracanal medicament like triple antibiotic paste.
- This combination contains metronidazole, ciprofloxacin, and minocycline which is effective in the disinfection of immature infected root canals and well tolerated by vital pulp tissue.
- After disinfection, bleeding is induced into the canal space through the apical foramen to create a scaffold on which new tissue will grow and repopulate the canal space. Over it, MTA is placed and the final restoration is given.
Coronal Restoration
- Restoration of the immature tooth following obturation with gutta-percha should be designed to strengthen the tooth as much as possible
- Placement of posts within the canal should be avoided unless no other means of restoration is possible
- Preparation of a post space has been shown to significantly weaken the remaining tooth structure, whereas acid etching and placement of a composite resin strengthen the tooth, making it more resistant to fracture
- In the apexified tooth, the gutta-percha should be removed below the alveolar crest, the dentin acid etched, and bonded composite resin placed to strengthen the root
Vital Pulp Therapy Conclusion
- It has been accepted that maintaining and regenerating pulp vitality is important for long-term tooth viability. Complete pulp regeneration and revascularization can be achieved after successful vital pulp therapy if vital pulp is in the canal.
- At the present time, stem cell-based tissue engineering approaches provide the most promising solution. The prognosis of vital pulp procedures has shown different results due to methodological variations between the different studies.
- The status of the pulp tissue and type of coronal restoration has a significant influence on the results. Among the different materials used, MTA appears to be more effective than calcium hydroxide for maintaining long-term pulp vitality in pulp capping and pulpotomy procedures.
- Further research and clinical trials are also needed to develop case selection guidelines, treatment approaches, and materials needed to maximize clinical success.
Leave a Reply