Regenerative Endodontics
Regenerative endodontics is one of the most thrilling developments in endodontics which uses the concept of tissue engineering to restore the root canals to a healthy state, allowing for continued development of the root and surrounding tissue.
Table of Contents
This development in the regeneration of a functional pulp–dentin complex gave hope to retaining the natural dentition.
Regenerative endodontics employs the role of tissue engineering which employs the use of stem cells. A stem cell is a special kind of cell that has a unique capacity to renew itself and give rise to specialized cell types.
Although most cells of the body, such as heart cells or skin cells, are committed to performing a specific function, a stem cell is uncommitted and remains uncommitted, until it receives a signal to develop into a specialized cell.
Read And Learn More: Endodontics Notes
Definition Of Tissue Engineering
The first definition of tissue engineering given by Langer and Vacanti is “as an interdisciplinary field that applies the principles of engineering and life sciences toward the development of biological substitutes that restore, maintain, or improve tissue function or a whole organ.”
MacArthur and Oreffo defined tissue engineering as “understanding the principles of tissue growth and applying this to produce functional replacement tissue for clinical use.”
Strategies of Stem Cell Technology
Three Strategies to stem cell technology
- Conductive
- Inductive
- Cell-base transplantation
1. Stem Cell Technology Conductive
The conductive approach utilizes biomaterials in a passive manner to facilitate the growth or regenerative capacity of the existing tissue.
An example of this is guided tissue regeneration in which the appropriate use of barrier membranes promotes predictable bone repair and new attachment with new formation of cementum and periodontal ligament fibers.
2. Stem Cell Technology Inductive
The induction approach involves activating the cells in close proximity to the defect site with specific biological signals like bone morphogenic proteins (BMPs).
Urist fist showed that new bone could be formed at non mineralizing or ectopic sites after implantation of powdered bone containing BMPs, which turned out to be the key elements for inducing bone formation.
Limitation of this technique is that the inductive factor for a particular tissue may not be known.
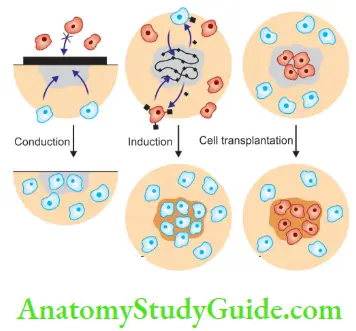
3. Cell-Base Transplantation
This approach involves direct transplantation of cells grown in the laboratory.
Triad of Tissue Engineering
Tissue engineering employs the use of three materials:
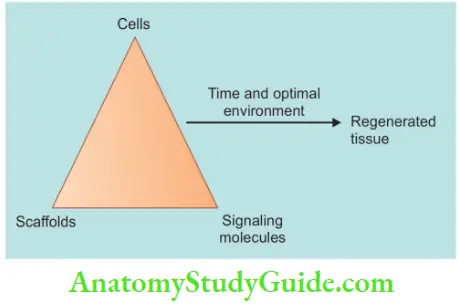
- Stem cells/Progenitor cells,
- Morphogens/Signaling molecules/Growth factors and
- Scaffold/Matrix
1. Stem Cells/Progenitor Cells Stem cells are undifferentiated cells that divide and respond to specialized cells on response to morphogens. Progenitor cells retain the differentiation potential and high proliferation capability but have lost the self-replication property, unlike stem cells.
- Unique Characteristics of Stem Cells
- They exist as undifferentiated cells and maintain this phenotype by the environment and/or the adjacent cell populations until they are exposed to and respond to the appropriate signals
- Ability to self-replicate for prolonged periods
- Maintain their multiple differentiation potentials throughout the life of the organism
- Categories of Stem Cells According to their Source
- Autologous cells: These are obtained from the same individual to whom they will be re-implanted. The advantage of autologous stem cells is that they have minimum problems with rejection and pathogen transmission; however, the disadvantage is limited availability
- Allogeneic cells: These are obtained from the body of a donor of the same species
- Xenogeneic cells: These are those isolated from individuals of another species. In particular, animal cells have been used quite extensively in experiments aimed at the construction of cardiovascular implants
- Syngeneic or isogenic cells: These are isolated from genetically identical organisms, such as twins, clones, or highly inbred research animal models
- Primary cells are from an organism
- Secondary cells are from a cell bank
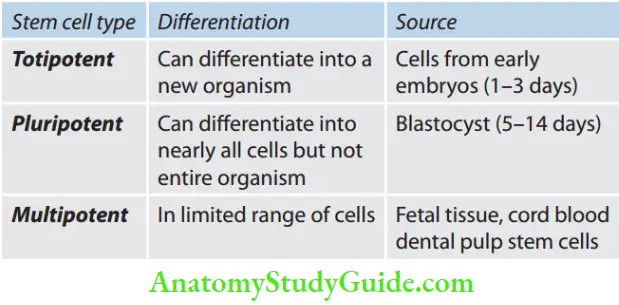
- Categories of stem cells according to their potency:
- Stem Cell Markers
Every cell in the body is coated with specialized proteins on their surface called receptors that have the capability of selectively binding to other “signaling” molecules. The stem cell markers are similar to these cell surface receptors. Each cell type, for example, a liver cell, has a certain combination of receptors on their surface that makes them distinguishable from other kinds of cells. Researchers use the signaling molecules that selectively adhere to the receptors on the surface of the cell as a tool that allows them to identify stem cells. The signaling molecules have the ability to fluoresce or emit light energy when activated by an energy source such as an ultraviolet light or laser beam. This, stem cell markers help in identifiation and isolation of stem cells.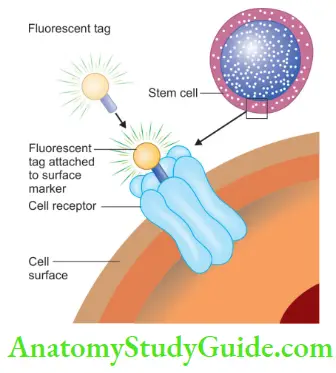
- Isolation of Stem Cells
Stem cells can be identified and isolated from mixed cell populations by the following four techniques: -
-
- By staining the cells with specific antibody markers and using a flow cytometer. This process is called fluorescent antibody cell sorting (FACS)
- Physiological and histological criteria. This includes phenotype, chemotaxis, proliferation, differentiation, and mineralizing activity
- Immunomagnetic bead selection
- Immunohistochemical staining
-
Tooth bud tissues containing stem cells are dissociated enzymatically and mechanically and filtered to remove even small clumps of cells, generating single-cell suspensions. The tissue is then plated in vitro and cultured to eliminate differentiated cell types. The resultant culture contains an enriched dental stem cell population.
2. Morphogens/Signaling Molecules/Growth Factors
These trigger the differentiation of selected mesenchymal stem cells into odontoblast-like cells.
- Morphogens Functions
- To stimulate division of neighboring cells and those infiltrating the defect [example: growth factors—platelet-derived growth factor (PDGF)]
- To stimulate the differentiation of certain cells along a specific pathway (example: differentiation factors—BMP)
- To stimulate angiogenesis
- To serve as chemoattractants for specific cell types
- Diffrent types of morphogens are
- Embryonic tooth development
- BMPs
- Fibroblast growth factors (FGFs)
- Hedgehog proteins (Hhs)
- Tumor necrotic factor (TNF)
- Transforming growth factor (TGF)
- Insulin-like growth factor (IGF)
- Colony stimulating factor (CSF)
- Epidermal growth factor (EGF)
- Interleukins (IL)
- PDGF
- Nerve growth factor (NGF)
- Embryonic tooth development
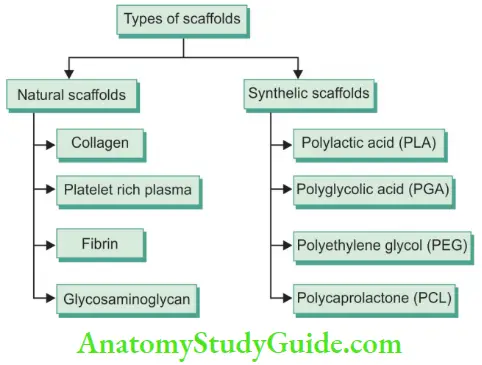
3. Scaffld/Matrix
Scaffold provides a physicochemical and biological three-dimensional microenvironment for cell growth and differentiation, promoting cell adhesion and migration
Scaffold is used to guide, organize, and provide physical and chemical signals, and help in the growth and differentiation of cells.
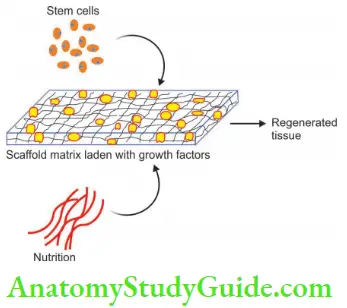
Tissues are composed of cells, insoluble extracellular matrix (ECM), and soluble molecules serving as regulators of cell functions. ECM consists of collagen, glycoprotein, and proteoglycan and it is important for growth and function of different cells involved.
Plasma-rich protein (PRP) is an autologous, easy-to-prepare scaffold rich in growth factors, that degrades, and forms a three-dimensional fibrin network.
Regenerative Endodontics Procedures
1. Regenerative Endodontics Procedures Definition
Regenerative endodontics is defined as biologically based procedures designed to physiologically replace damaged tooth structures, including dentin and root structures, as well as the pulp–dentin complex.
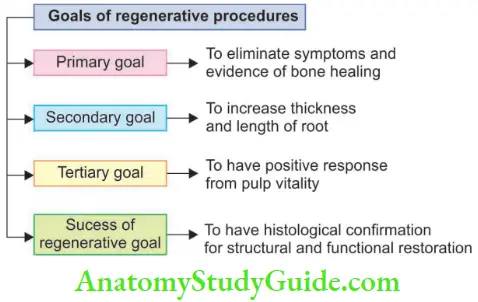
According to the American Association of Endodontists’ Clinical Considerations for a Regenerative Procedure, the primary goal of the regenerative procedure is the elimination of clinical symptoms and resolution of apical periodontitis and the secondary goal is the thickening of canal walls and continued root maturation.
The primary goal is the same as that of endodontic treatment but difference between the two is that after disinfecting the canals in endodontic treatment, roots are filled with biocompatible materials, and in the regenerative procedure, roots are filled with the host’s own vital tissue.
Different techniques of tissue engineering applied for regenerative endodontics are
- Root canal revascularization via blood clotting
- Postnatal stem cell therapy
- Pulp implantation
- Scaffld implantation
- Injectable scaffold delivery
- Three-dimensional cell printing
- Gene delivery
2. Root Canal Revascularization via Blood Clotting
In non-vital teeth with immature roots, materials like calcium hydroxide, MTA, dentine, and other bioactive materials were used to form an apical barrier against which obturation could be done.
But each material comes with its own advantages and disadvantages. Problems with calcium hydroxide are like long treatment time occupying canal space physically it so no room for vital tissue to proliferate; high pH may cause necrosis of tissue and barrier formation is often porous and non-continuous.
MTA is placed in the apical third of the immature root to create a stop for the filing material but it does not allow new tissue to grow into the root canal thus the root remains thin and weak.
Hence, apexification does not lead to continued root formation or thickening of the root canal wall, leading to the risk of an undesirable side effect of a short and weakened root that is susceptible to fracture.
An alternative treatment regime is preferred to overcome these problems, that is, pulp revascularization.
- Root Canal Revascularization via Blood Clotting Definition
Revascularization is the procedure to re-establish vitality in a non-vital tooth to allow the repair and regeneration of tissue. It allows further development of root and dentin structures with a better long-term prognosis. In teeth with open apices and necrotic pulp, some vital pulp tissue and Hertwig’s epithelial root sheath remains which may proliferate once the canal is disinfected.- Disinfection of root canal
- Placement of a matrix in the canal for tissue growth
- Bacteria tight seal of the access opening
- Root Canal Revascularization Indications
- The teeth that present with symptoms of acute or chronic apical periodontitis (i.e., pain, diffuse facial and/or mucosal swelling, tenderness to percussion, or intraoral sinuses)
- Radiographically, the tooth had an immature apex, either blunderbuss or in the form of a wide canal with parallel walls and an open apex. On the electric pulp test, the affected tooth is non-vital Teeth with an apical opening of more than 1 mm show greater success with revascularization procedures by encouraging the ingrowth of tissue into root canal space
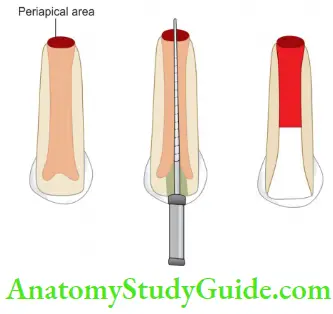
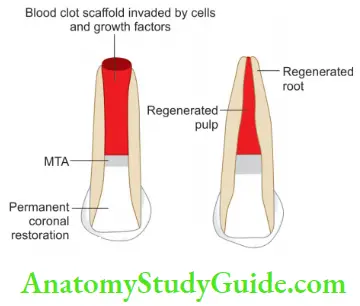
- Root Canal Revascularization Technique
1. Tooth showing immature apex with wide canal and open apex;
2. Endodontic file in the canal, 2 mm beyond the established working length to induce bleeding;
3. Allow the blood clot to form 3 mm below CEJ;
4. Place MTA over clot;
5. Regenerated root showing thickening of canal walls and closure of apex.- Root Canal Revascularization First appointment
- After anesthetizing, isolate the tooth with a rubber dam
- Prepare the access cavity and gently flush the canal 5.25% with sodium hypochlorite solution
- Dry the canal using sterile paper points
- Place a mixture of ciprofloxacin 200 mg, metronidazole 400 mg, and minocycline 100 mg in a root canal 2 mm from the working length and leave for 7 days
- Seal the tooth with the sterile sponge and a temporary filling
- Recall after 3–4 weeks
- Root Canal Revascularization Second appointment
- Evaluate the patient for resolution of signs and symptoms of infection like pain, swelling, sinus, etc.
- Repeat antimicrobial treatment if required
- Isolate the tooth and copiously irrigate it with 5.25%
- NaOCl and gently place the small hand file to remove the antimicrobial dressing
- Dry the canal using sterile paper points
- Introduce a size no. 40 K-fie into the root canal 2 mm beyond the working length to induce some bleeding into the root canal
- Allow the bleeding to reach a level 3 mm below the cementoenamel junction (CEJ) and leave the tooth for 15 min so that a blood clot is formed. Blood clot acts as a scaffld and source of growth factors to facilitate regeneration and repair of the tissue into the canal
- Place mineral trioxide aggregate over the clot carefully up to the level of CEJ followed by a wet cotton pellet and restore it with a temporary dressing material
- After 1 week, restore the tooth with a composite restoration and recall the patient for clinical and radiographical evaluation
- Patients are recalled after a minimum of 1 year. The criteria of success are
- Lack of symptoms
- Radiographic evidence of increased root length
- Radiographic evidence of increased root canal thickness
- Root Canal Revascularization First appointment
- Mechanism of Revascularization
- Few cells remain at the apical end of the root canal. These cells might proliferate into the newly formed matrix and differentiate into odontoblasts under the organizing influence of cells of Hertwig’s epithelial root sheath, which are quite resistant to destruction, even in the presence of inflammation. The newly formed odontoblasts can lay down tubular dentin at the apical end, causing abiogenesis as well as on lateral aspects of dentinal walls of the root canal, reinforcing and strengthening the root
- Continued root development due to multipotent dental pulp stem cells (DPSCs), which are present in permanent teeth and might be present in abundance in immature teeth. These cells from the apical end might be seeded onto the existing dentinal walls and might differentiate into odontoblasts and deposit tertiary or tubular dentin
- Stem cells in the periodontal ligament can proliferate, grow into the apical end and within the root canal and deposit hard tissue both at the apical end and on the lateral root walls
- Root development could be attributed to stem cells from the apical papilla or the bone marrow. Instrumentation beyond the confines of the root canal to induce bleeding can also transplant mesenchymal cells from the bone into the canal lumen. These cells have an excellent proliferative capacity. Transplantation studies have shown that human stem cells from bone marrow can form bone or dentin in vivo
- Blood clots being a rich source of growth factors could play an important role in regeneration. These include PDGF, vascular factor, and tissue growth factor and could stimulate differentiation, growth, and maturation of fibroblasts, odontoblasts, cementoblasts, etc. from the immature undifferentiated mesenchymal cells in the newly formed tissue matrix.
- Advantages of Revascularization Procedure
- Short treatment time, after control of infection, it can be completed in a single visit
- The approach is simple and can be completed without using expensive biotechnology
- Continued root development and strengthening of root as a result of reinforcement of lateral dentinal walls by deposition of hard tissue
- Regeneration of tissue in root canal systems by a patient’s own blood cells avoids the possibility of immune rejection and pathogen transmission from replacing the pulp with a tissue engineered construct
- Cost-effective
- Obturation of canal not required so avoids root fracture by forces of lateral compaction technique
- Limitations of Revascularization Procedure
- The composition of cells found in fibrin clot is unpredictable resulting in variations in treatment outcome
- Crown discoloration, development of resistant bacterial strains, and allergic reactions to intracanal medications
- The entire canal may get calcified compromising esthetics and not allowing future endodontic treatment if required
- Long-term clinical results not available
- Post and core are not possible because vital tissues in the apical two third of the canal can’t be compromised for post-placement
3. Postnatal Stem Cell Therapy
There are two stem cells categories according to their origin:
- Embryonic stem cells (pluripotent): These can be isolated from the normal blastocyst and can give rise to all derivatives of three layers. They are highly plastic and can give rise to any kind of specialized cell type and yet maintain their undifferentiated state pluripotent cells.
- Postnatal cells: These can be collected directly from the bone marrow or umbilical cord blood. They are less plastic and have a limited life cycle and thus have limited potential of differentiation than embryonic stem cells.
- Stem cells of dental origin
- Postnatal dental pulp stem cells (DPSCs)
- Stem cells obtained from deciduous teeth (SHED)
- Periodontal ligament stem cells (PDLSCs)
- Dental follicle progenitor stem cells (DFPCs)
- Stem cells from the apical papilla (SCAP)
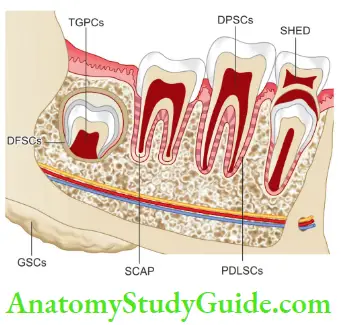
- Dental Pulp Stem Cells (DPSCs)
Dental pulp contains the dentinogenic progenitors, i.e., DPSCs that are responsible for dentin repair. They can regenerate dentin–pulp-like complex which is composed of a mineralized matrix with tubules lined with odontoblasts and fibrous tissue containing blood vessels in an arrangement similar to the dentin–pulp complex is found in normal human teeth. Stem Cells from Human Exfoliated Deciduous Teeth (SHED) These are the cells present in living pulp remnants of exfoliated deciduous tooth consisting of connective tissue, blood vessels, and odontoblasts. These can differentiate into odontoblast-like cells that form dentin-like structures. - Periodontal Ligament Stem Cells (PDLSC)
These are present in enzymatically digested PDL (Periodontal ligament) and can form cementum/PDL-like structures as thin layers of cementum that are interfaced with dense collagen fibers, similar to Sharpey’s fibers. Their differentiation is believed to be due to Hertwig’s epithelial root sheath cells. - Dental Follicle Precursor Cells (DFPCs)
These are derived from developing tissue and have shown greater plasticity than other dental stem cells. They can differentiate into odontoblasts in vitro. - Stem Cells from Apical Papilla (SCAP)
These are found in the apical papilla found at the apices of developing teeth at the junction of the apical papilla and dental pulp. The apical papilla is important for the development of root. It is the soft tissue present at the apices of developing permanent teeth, lying apical to the epithelial diaphragm. An apical cell-rich zone is present between the apical papilla and pulp. These cells can undergo odontoblastic, osteogenic, or neurogenic differentiation. In postnatal stem cell therapy, cells are injected in the disinfected root canal. This approach is quick, easy to deliver, and relatively painless.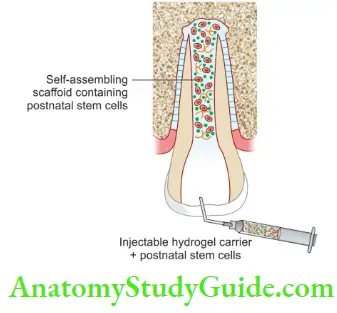
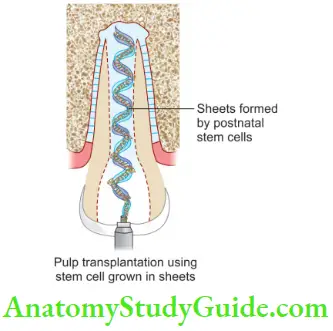
4. Pulp Implantation
Here replacement pulp tissue is transplanted in the disinfected root canal. This pulp tissue is got from stem cells that are grown in a laboratory. This pulp tissue is grown in sheets in vitro on biodegradable polymer nanofibers. These sheets are rolled together to form a 3-D pulp tissue that can be implanted into root canal system. But this procedure does not ensure that cells properly adhere to the root canal walls. Moreover, sheets of cells lack vascularity so only the apical part of the root canal receives these cellular constructs.
5. Scaffold Implantation
During dental pulp regeneration, an ideal scaffold should also ensure good neurovascular supply to new pulp tissue, for example, DPSCs are seeded on a three-dimensional polyglycolic acid matrix and grown in vitro, and then surgically implanted.
6. Three-Dimensional Cell Printing
This technique is used to precisely position the cells and thus constructed tissue mimics the natural dental pulp tissue structure. Here an inkjet device is used to disperse the layers of cells suspended in a hydrogel to recreate dental pulp tissue. But for this, precise 3-D models for individual pulp cavities and an effective delivery system are required.
7. Injectable Scaffld
Here polymerizable hydrogels alone or containing cell suspensions are delivered by injections. This may promote regeneration by providing a substitute for an Extracellular matrix (ECM) but has low cell survival and has limited control over tissue formation.
8. Gene Therapy
It is the means of delivering genes for growth factors, morphogens, and ECM molecules to somatic cells of individuals resulting in the therapeutic effect. Gene can induce a natural biological process by expressing a molecule involved in regenerative response for the target tissue.
Regenerative Endodontics Conclusion
- Due to the emergence of regenerative endodontic procedures, clinicians should re-evaluate the current clinical protocols while treatment planning of some clinical cases is done.
- This is especially important when dealing with immature teeth which carry potent stem cells which can enable the tissue to regenerate and repair better than mature tissues.
Leave a Reply