Regulation Of Heart Rate Introduction
Heart rate is maintained within normal range constantly. It is subjected to variation during normal physiological conditions such as exercise, emotion, etc.
Table of Contents
however, under physiological conditions, the altered heart rate is quickly brought back to normal.
It is because of the perfectly tuned regulatory mechanism in the body through the nervous system.
Read And Learn More: Medical Physiology Notes
Heart Rate
Normal Heart Rate
Normal heart rate is 72/minute. It ranges between 60 and 80 per minute.
Heart Rate Tachycardia
Tachycardia is the increase in the heart rate above 100/minute.
Physiological conditions when tachycardia occurs are:
- Childhood
- Exercise
- Pregnancy
- Emotional conditions such as anxiety.
Pathological conditions when tachycardia occurs are:
- Fever
- Anemia
- Hypoxia
- Hyperthyroidism
- Hypersecretion of catecholamines
- Cardiomyopathy
- Valvular heart diseases.
Bradycardia
Bradycardia is the decrease in the heart rate below 60/ minute.
Physiological conditions when bradycardia occurs are:
- Sleep
- Athletic heart.
Pathological conditions when bradycardia occurs are:
- Hypothermia
- Hypothyroidism
- Heart attack
- Congenital heart disease
- Degenerative process of aging
- Obstructive jaundice
- Increased intracranial pressure.
Drugs that induce bradycardia are:
- Beta-blockers
- Channel blockers
- Digitalis and other antiarrhythmic drugs.
Regulation Of Heart Rate
Heart rate is regulated by the nervous mechanism. The nervous mechanism regulating heart rate consists of three components:
- Vasomotor center
- Motor (efferent) nerve fibers to the heart
- Sensory (afferent) nerve fibers from the heart.
Vasomotor Center – Cardiac Center
The vasomotor center is the nervous center that regulates the heart rate. It is the same center in the brain, which regulates blood pressure.
Earlier it was called the cardiac center.
The vasomotor center is bilaterally situated in the reticular formation of the medulla oblongata and the lower part of the pons.
The Vasomotor center has three areas:
- Vasoconstrictor area
- Vasodilator area
- Sensory area.
Vasoconstrictor Area- Cardioaccelerator Center
Vasoconstrictor Area Situation
It is situated in the reticular formation of the medulla in the floor of the IV ventricle and it forms the lateral portion of the vasomotor center.
It is otherwise known as the pressor area (formerly cardio accelerator center).
Vasoconstrictor Area Function
This area increases the heart rate. It increases the heart rate by sending accelerator impulses to the heart through sympathetic nerves.
It also causes constriction of blood vessels. Stimulation of this center in animals increases the heart rate and its removal or destruction decreases the heart rate.
Vasoconstrictor Area Control
The vasoconstrictor area is under the control of the hypothalamus and cerebral cortex.
Vasodilator Area – Cardioinhibitory Center
Vasodilator Area Situation
It is also situated in the reticular formation of the medulla oblongata on the floor of the IV ventricle.
It forms the medial portion of the vasomotor center. It is also called the depressor area (formerly the cardioinhibitory center).
Vasodilator Area Function
- This area decreases the heart rate. It decreases heart rate by sending inhibitory impulses to the heart through the vagus nerve.
- It also causes dilatation of blood vessels. Stimulation of this area in animals with a weak electric stimulus decreases the heart rate and, stimulation with a strong stimulus stops the heartbeat.
- When this area is removed or destroyed, the heart rate increases.
Vasodilator Area Control
The vasodilator area is under the control of the cerebral cortex and hypothalamus.
It is also controlled by the impulses from baroreceptors, chemoreceptors, and other sensory impulses via afferent nerves.
Sensory Area
It is in the posterior part of the vasomotor center, which lies in the nucleus of tractus solitaries in the medulla and pores.
This area receives sensory impulses via the glossopharyngeal nerve and vagus nerve from the periphery, particularly, from the baroreceptors.
In turn, this area controls the vasoconstrictor and vasodilator areas.
Motor (Efferent) Nerve Fibers To Heart
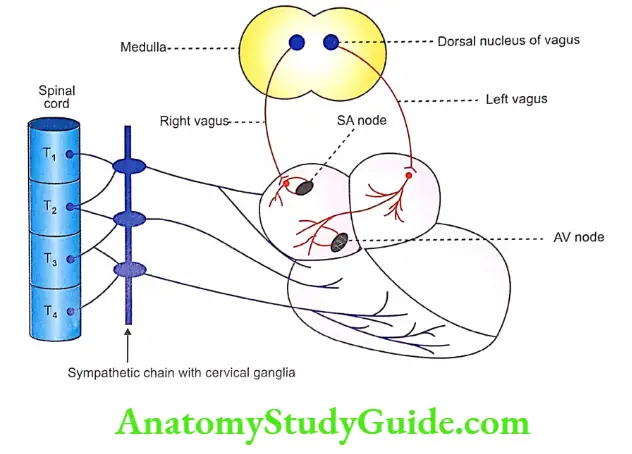
- The heart receives efferent nerves from both divisions of the autonomic nervous system.
- Parasympathetic fibers arise from the medulla oblongata and pass through the vagus nerve.
- The sympathetic fibers arise from the upper thoracic (T1 to T4) segments of the spinal cord.
Parasympathetic Nerve Fibers
The parasympathetic nerve fibers are the cardioinhibitory nerve fibers. These nerve fibers reach the heart through the cardiac branch of the vagus nerve.
Parasympathetic Origin
The parasympathetic nerve fibers supplying the heart arise from the dorsal nucleus of the vagus.
This nucleus is situated on the floor of the fourth ventricle in the medulla oblongata and is in close contact with the vasodilator area.
Parasympathetic Distribution
- The preganglionic parasympathetic nerve fibers from the dorsal nucleus of the vagus reach the heart bypassing the main trunk of the vagus and the cardiac branch.
- After reaching the heart, the preganglionic fibers K‘efinale on postganglionic neurons.
- The postganglionic fibers from these neurons innervate heart muscle.
- Most of the fibers from the right vagus terminate in the SA node. The remaining fibers supply the atrial muscles and AV node.
- Most of the fibers from the left vagus supply the AV node and some fibers supply the atrial muscle and SA node.
- Ventricles do not receive the vagus nerve supply. Few fibers are located in the bases of ventricles but the functions of these nerve fibers are not known.
Parasympathetic Function
The vagus nerve fibers are cardioinhibitory in function and carry inhibitory impulses from the vasodilator area to the heart.
Parasympathetic Vagal Tone
- Vagal tone is the continuous stream of inhibitory impulses arising from the vasodilator area.
- Heart rate is kept under control because of vagal tone.
- The impulses from the vasodilator area pass through the vagus nerve, reach the heart and exert an inhibitory effect on the heart.
- The heart rate is inversely proportional to the vagal tone.
- In experimental animals (dogs), the removal of vagal input (by sectioning the vagus) increases the heat rate.
- This proves the existence of vagal tone. Under resting conditions, the vagal tone dominates the sympathetic tone.
- The impulses from different parts of the body regulate the heart rate through the vasomotor center by altering the vagal tone.
- Vagal tone is also called cardioinhibitory tone or parasympathetic tone.
Effect of Stimulation of Vagus Nerve
- Effect of stimulation of right vagus nerve
- The right vagus supplies mainly the SA node. Stimulation of the right vagus in experimental animals such as dogs with a weak stimulus causes a reduction in heart rate and force of contraction.
- Stimulation with strong stimulus causes stoppage of the heart due to inhibition of the SA node.
- If the stimulus is continued for some time, the heart starts beating again; but the rate of contraction is slower than before.
- This is because of vagal escape. Vagal escape refers to the escape of the heart from the inhibitory effect of vagal stimulation.
Cause for vagal escape:
- Stimulation of the right vagus stops the heartbeat due to the inhibition of the SA node and atria.
- However, ventricles are not supplied by the vagus. So the ventricles are not inhibited by vagal stimulation.
- Because of this, when the stoppage of the heartbeat is continued for some time (by vagal stimulation) a part of ventricular musculature becomes the pacemaker and starts producing impulses.
- It results in the contraction of the ventricles which is called vagal escape. Thus, vagal escape includes only ventricular contractions.
- However, the rhythmicity of ventricular muscle is less and it is about 20/min.
Effect of stimulation of left vagus nerve
- Left vagus supplies mainly the AV node. Stimulation of the left vagus in the dog by a weak stimulus causes a slight reduction in the rate of ventricular contraction.
- The stimulation of the left vagus causes inhibition of the AV node. Because of the inhibition of the AV node, some of the impulses from the SA node are not conducted to ventricles.
- This is called the partial heart block. The ratio between atrial contraction and ventricular contraction is 2:1, 3:1, or 4:1, depending upon the strength of the stimulus.
- Stimulation of the left vagus with strong stimulus causes stoppage of ventricular contraction.
- This is because of the complete inhibition of the AV node. This is called complete heart block.
- The prolongation of stimulation causes idioventricular rhythm, which is different from the rhythm of atrial contraction.
Mode of Action of Vagus Nerve
The Vagus nerve inhibits the heart by secreting the neurotransmitter substance known as acetylcholine.
Sympathetic Nerve Fibers
Sympathetic nerve fibers supplying the heart have cardio accelerator functions.
Vagus Nerve Origin
The preganglionic fibers of the sympathetic nerves to the heart arise from lateral grey horns of the first 4 thoracic (T., to T4) segments of the spinal cord.
These segments of the spinal cord receive fibers from the vasoconstrictor area of the vasomotor center.
Course and Distribution
- The preganglionic fibers reach the superior, middle, and inferior cervical sympathetic ganglia situated in the sympathetic chain.
- The inferior cervical sympathetic ganglion fuses with the first thoracic sympathetic ganglion forming the stellate ganglion.
- From these ganglia, the postganglionic fibers arise. The postganglionic fibers form superior, middle, and inferior cervical sympathetic nerves.
- The superior sympathetic nerve innervates larger arteries and bases the heart.
- The middle one supplies the rest of the inferior nerve and serves as sensory (afferent) the heart.
Vagus Nerve Function
The sympathetic nerves are cardioaccelerators in function and carry cardioaccelerator impulses from the vasoconstrictor area to the heart.
Sympathetic Tone
- Sympathetic tone or cardio accelerator tone is the continuous stream of impulses produced by the vasoconstrictor area.
- The impulses pass through sympathetic nerves and accelerate the heart rate. Under normal conditions, the vagal tone is dominant over the sympathetic tone.
- Whenever the vagal tone is reduced or abolished, the sympathetic tone becomes powerful.
- It is generally believed that the sympathetic tone does not play an important role in the regulation of cardiac function under resting physiological conditions.
- However, it plays a definite role in increasing the heart rate during emergency conditions.
- The rate of contraction of a completely denervated heart of a dog is higher than the rate of an innervated heart in resting conditions.
- This shows that under resting conditions, the vagal tone is dominant over the sympathetic tone.
Effect of Stimulation on Sympathetic Nerves
Stimulation of sympathetic nerves increases the rate and the force of contraction of the heart.
The effect depends upon the strength of the stimulus.
Mode of Action of Sympathetic Nerves
Cardio acceleration by sympathetic stimulation is due to the release of the neurotransmitter substance, noradrenaline.
Sensory (Afferent) Nerve Fibers From the Heart
The afferent (sensory) nerve fibers from the heart pass through the inferior cervical sympathetic nerve.
These nerve fibers carry sensations of stretch and pain from the heart to the brain via the spinal cord.
Factors Affecting Vasomotor Center – Regulation Of Vagal Tone
The vasomotor center regulates cardiac activity by receiving impulses from different sources in the body.
After receiving the impulses from different sources, the vasodilator area alters the vagal tone and modulates the activities of the heart.
The various sources from which the impulses reach the vasomotor center are:
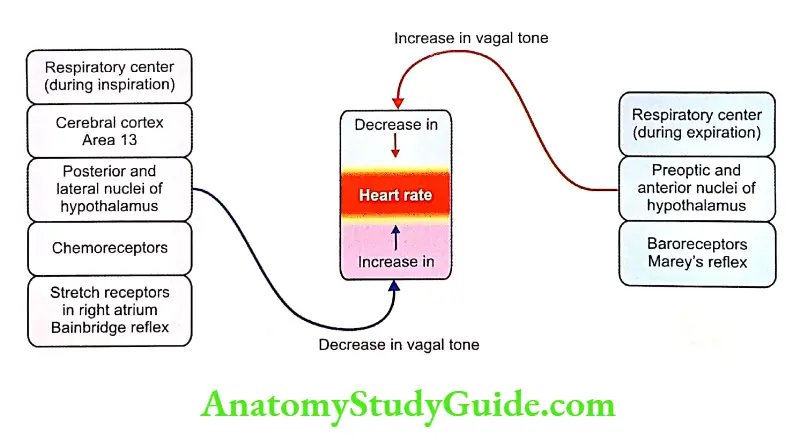
1. Impulses From Higher Centers
The vasomotor center is mainly controlled by the impulses from the higher centers in the brain.
The higher centers are the following.
Cerebral Cortex
Area 13 in the cerebral cortex is concerned with the emotional reactions of the body.
During emotional conditions, this area sends inhibitory impulses to the vasodilator area. This causes a reduction in vagal tone leading to cardio acceleration.
Hypothalamus
The hypothalamus influences the heart rate via the vasomotor center. Stimulation of posterior and lateral hypothalamic nuclei causes tachycardia.
Stimulation of preoptic and anterior nuclei causes bradycardia.
Impulses From Respiratory Centers
- In forced breathing, the heart rate increases during inspiration and decreases during expiration.
- This variation is called respiratory sinus arrhythmia. This is common in some children and in some adults even during quiet breathing.
- The sinus arrhythmia is due to the alteration of vagal tone because of the impulses arising from respiratory centers during inspiration.
- These impulses inhibit the vasodilator area resulting in decreased vagal tone and increased heart rate.
- During expiration, the respiratory center stops sending impulses to the vasodilator center. Now, vagal tone increases leading to a decrease in heart rate.
Impulses From Baroreceptors- Marey’s Reflex
Baroreceptors
The baroreceptors are the receptors, which give a response to changes in blood pressure. These receptors are also called pressoreceptors.
Baroreceptors Situation
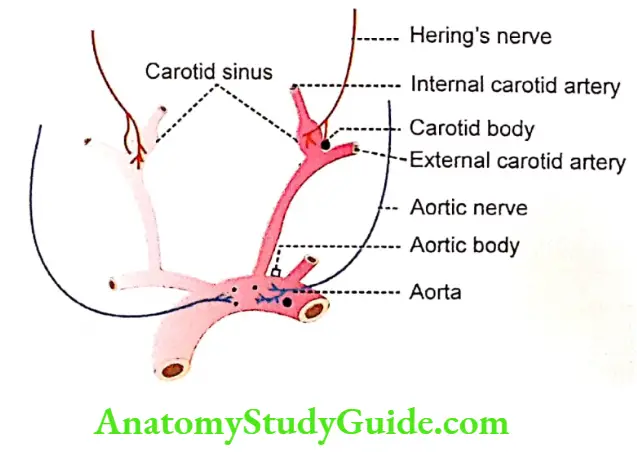
Based on the situation, the baroreceptors are divided into two types, carotid baroreceptors, and aortic baroreceptors.
Carotid baroreceptors are situated in the carotid sinus, which is present in the wall of the internal carotid artery near the bifurcation of the common carotid artery Tne posts baroreceptors are situated in the wall of the Peoria.
Baroreceptors Nerve Apply
- Baifficsepiofo in the carotid sinus is supplied by Hering’s nerve, which is the branch of the glossopharyngeal (IX cranial) nerve.
- The aortic baroreceptors are supplied by the aortic nerve, which is a branch of the vagus (X cranial) nerve.
- The nerve fibers from the baroreceptors reach the nucleus of tractus solitaries in the medulla oblongata.
- The tractus solitarius is situated adjacent to the vasomotor center.
Function- Marey’s Reflex
The baroreceptors regulate the heart rate through a reflex called Marey’s reflex.
The stimulus for this reflex is an increase in blood pressure.
Marey’s reflex is a cardioinhibitory reflex that decreases heart rate when blood pressure increases.
Whenever the blood pressure increases, the aortic and carotid baroreceptors are stimulated, and stimulatory impulses are sent to the nucleus of tractus solitarius via Hering’s nerve and aortic nerve (afferent nerves).
Now, the nucleus of tractus solitarius stimulates the vasodilator area, which in turn increases the vagal tone leading to a decrease in heart rate.
Marey’s reflex includes the aortic reflex and the carotid sinus reflex.
When pressure is less, the baroreceptors are not stimulated. So, no impulses go to the nucleus of tractus solitarius.
There are no inhibitory impulses to the heart and heart rate is not decreased.
Thus, the heart rate is inversely proportional to blood pressure.
Baroreceptors Marey’s law
According to Marey’s law, the pulse rate (which represents the heart rate) is inversely proportional to blood pressure.
The baroreceptors produce Marey’s reflex only during resting conditions.
So, in many conditions such as exercise, there is an increase in both blood pressure and heart rate.

4. Impulses From Chemoreceptors Chemoreceptors
Chemoreceptors are receptors giving respond to changes in chemical constituents of blood, particularly oxygen, carbon dioxide, and hydrogen ion concentration.
Chemoreceptors Situation
Peripheral chemoreceptors are situated in the carotid body and aortic body adjacent to baroreceptors.
Chemoreceptors Structure
The chemoreceptors are made up of special types of cells. These cells are of two types, type 1, or glomus cells, and type 2, or sustentacular cells.
Glomus cells have afferent nerve endings which are stimulated by hypoxia.
Type 2 cells are glial cells and provide support for type 1 cells.
Nerve Supply
The chemoreceptors in the carotid body are supplied by Henry’s, nerve, which is the branch of glossopharyngeal these in the aortic body are supplied by the aortic nerve.
Chemoreceptors Function
Whenever there is hypoxia, hypercapnia, and increased hydrogen ions concentration in the blood, the chemoreceptors are stimulated and inhibitory impulses are sent to the vasodilator area.
Vagal tone decreases and heart rate increases. The chemoreceptors play a major role in maintaining respiration than the heart rate.
Sinoaortic Mechanism and Buffer Nerves
The sinoaortic mechanism is the mechanism of baroreceptors and chemoreceptors in carotid and aortic regions that regulates heart rate, blood pressure, and respiration.
The nerves from these receptors are called buffer nerves.
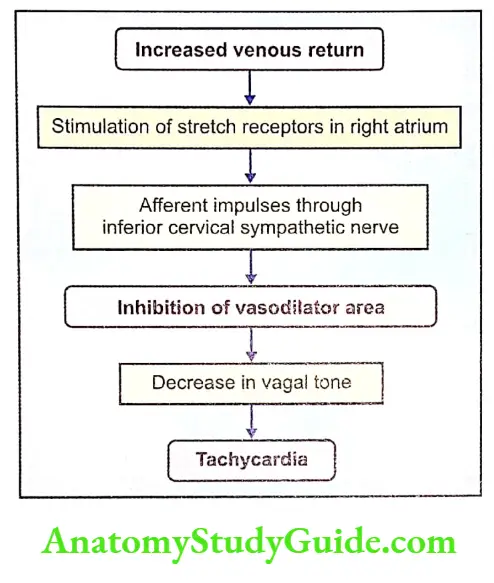
5. Impulses From Right Atrium – Bainbridge Reflex
Bainbridge reflex is a cardio accelerator reflex that increases the heart rate when venous return is increased.
Since this reflex arises from the right atrium, it is also called the right atrial reflex.
There are some stretch receptors in the wall of the right atrium. When venous return increases, the right atrium is distended. The right atrial distention stimulates the stretch receptors.
The stretch receptors, in turn, send inhibitory impulses through an inferior cervical sympathetic nerve to the vasodilator area of the vasomotor center.
The vasodilator area is inhibited resulting in a decrease in vagal tone and an increase in heart rate stimulation of sensory nerves produces varying effects. Impulses From Other Afferent Nerves
Examples:
- Stimulation of receptors in the nasal mucous membrane causes bradycardia. The impulses from the nasal mucous membrane pass via the branches of the V cranial nerve and decrease the heart rate
- Most of the painful stimuli cause tachycardia and some cause bradycardia. The impulses are transmitted via pain nerve fibers.
- Inhibitory impulses through an inferior cervical sympathetic nerve to the vasodilator area of the vasomotor center. The vasodilator area is inhibited resulting in a decrease in vagal tone and an increase in heart rate.
7. Bezold-Jarisch Reflex
Bezold-Jarisch reflex is the reflex characterized by bradycardia and hypotension caused by stimulation of chemoreceptors in the wall of left ventricles by substances such as alkaloids.
It is also called coronary chemoreflex. Vagal fibers form the afferent and efferent pathways of this reflex.
Bezold-Jarisch reflex is a pathological reflex and it does not occur in physiological conditions.
The conditions when this reflex occurs are myocardial Infarction, administration of thrombolytic agents, hemorrhage, aortic stenosis, or syncope.
Leave a Reply