Restoration of Endodontically Treated Teeth Introduction
The long-term success of endodontically treated teeth depends upon the skilled integration of endodontic and restorative procedures. Postendodontic restoration is necessary to prevent fracture of the remaining tooth structure, reinfection of the root canal, and to replace the missing tooth structure.
Table of Contents
Importance Of Coronal Restoration
Postendodontic coronal restoration is important to prevent the ingress of microorganisms into coronal pulp. To prevent coronal leakage, the clinician should
- Temporarily seal the tooth during or after the treatment
- Provide adequate coronal restoration after treatment
- Do long-term follow-up so as to evaluate the integrity of the restoration
Read And Learn More: Endodontics Notes
But, even a properly done endodontic treatment can fail due to the following reasons:
- Poor quality of temporary restoration
- Delay in permanent restoration after completion of endodontic treatment
- Poor marginal integrity of final restoration
- Fractured tooth
Therefore, it is very important to seal the root canal system during or after the endodontic treatment. Commonly used materials for temporary restoration are IRM and Cavit.
Factors Making Endodontically Treated Teeth Different From Vital Teeth
Endodontically treated teeth are more susceptible to fracture than unrestored vital teeth and also lack a lifelike translucency, thus requiring specialized restorative treatment.
Differences between endodontically treated and vital teeth are
- Structural changes/architectural changes
- Changes in the dentin physical characteristics/moisture loss
- Change in esthetics
Structural Changes/Architectural Changes
Fracture resistance of the tooth decreases as more tooth structure is lost due to decay, dental procedures, and endodontic therapy A tooth does not become more brittle due to endodontic treatment, but it is loss of structural integrity (provided by the dome-shaped roof of pulp chamber at the time of endodontic access cavity preparation) which leads to increased risk of tooth fracture.
This compromised structural integrity makes the tooth insufficient to perform its function because of loss of occlusion with its antagonist and adjacent teeth. In addition, the excessive removal of radicular dentin during canal preparation compromises the root.

Changes in the Dentin Physical Characteristics/Moisture Loss
Dehydration and loss of collagen intermolecular crosslinking cause irreversible altered physical properties of endodontically treated teeth. A decrease in 14% strength and toughness of dentin has been observed in endodontically treated teeth.
Clinical implication: Cementation of the active post can induce mechanical stresses that may result in root fracture and failure of post endodontic restorations.
Esthetic Consideration
Non vital teeth show loss of translucency and discoloration due to various reasons like necrotic pulp, endodontic procedures, and root canal filling materials. Loss of tooth structure due to fracture or caries also requires further esthetic consideration for restoration of endodontically treated teeth.

Biomechanical Changes
The proprioceptive feedback mechanism is lost after endodontic treatment. This might subject an endodontically treated tooth to greater loads than a vital tooth. Tidmarish showed that a normal tooth is a hollow laminated structure which deforms under load but complete elastic recovery occurs after physiological loading.
Restorative Treatment Planning For Endodontically Treated Teeth
The following factors should be taken into consideration before planning restoration for endodontically treated teeth:
- Amount of the tooth structure present
- Occlusal forces and the anatomic position of the tooth
- Restorative requirements
- Esthetic requirements.
Amount of the Tooth Structure
This is the most important factor that dictates the choice of restoration and is not under the control of the clinician. The resistance form of an endodontically treated tooth depends on the amount of radicular dentin and coronal tooth structure present.
Loss of tooth structure in endodontically treated teeth can vary from minimal access cavity to an extensively damaged tooth. Restorative treatment decision depends upon the amount of remaining tooth structure present.
Ingrid Peroz et al. (2005) classified the restoration plan of endodontically treated teeth depending on the number of walls remaining around the access cavity preparation.
- Class 1: Four remaining walls around the access cavity preparation: If all axial walls of the cavity remain with a thickness >1 mm, then only intracoronal restoration of the access cavity if sufficient, provided the tooth is not subjected to undue occlusal forces
- Classes 2 and 3: Two or three remaining walls around access cavity preparation: In these cases, a core followed by a crown is indicated
- Class 4: One remaining wall around the access cavity preparation: In such cases, a post is indicated
- Class 5: No remaining wall around the access cavity preparation: Placement of post is mandatory in these cases.
According to Cohen, the choice of post-endodontic restoration depends upon the amount of the remaining coronal tooth structure.
- A tooth with minimal loss of structure is inherently stronger and can be restored with only coronal restoration
- A tooth with >50% of remaining coronal structure can be restored with a crown
- A tooth with 25–50% of remaining coronal structure can be restored with nonrigid post
- A tooth with <25% of the remaining coronal structure, or <3–4 mm of cervical tooth structure must be restored with rigid posts.

Structurally compromised teeth are prone to
- Root fracture
- Dislodgement of the prosthesis
- Recurrent caries
- Endodontic failure as a result of coronal–apical leakage
- Invasion of biologic width causing periodontal injury
Occlusal Forces and the Anatomic Position of the Tooth
- Anterior teeth with minimal loss of tooth structure can be restored with coronal restoration. If a tooth is discolored, bleaching and veneer should be considered.
- Anterior teeth with heavy horizontal forces should be restored with stronger restorative components
- A posterior tooth with considerable structure requires restoration with an onlay or crown to protect it against fracture. In case of extensive tooth damage, post/core followed by crown is indicated

- (A) direct composite restoration;
- (B) bleaching of discolored teeth.
Restorative Requirements
Teeth included as abutments in the field or partial dentures undergo more force and thus need additional retention and protection against fracture and caries due to leakage.
Esthetic Requirements
Loss of translucency and discoloration in endodontically treated teeth especially in the esthetic zone require restorative materials like tooth-colored posts, composites or ceramic cores and ceramic crowns.
Requirements of a Tooth to Accept a Post and Core
- Optimal apical seal
- Absence of fitula or exudate
- Absence of active inflmmation
- No sensitivity to percussion
- Absence of associated periodontal disease
- Sufficient bone support around the root
- Sound tooth structure coronal to the alveolar crest
- Absence of any fracture of the root
Contraindications of Placing Post
- Presence of signs of endodontic failures like a poor apical seal, active inflmmation, presence of fistula or sinus, and tenderness on percussion
- If adequate retention of the core can be achieved by natural undercuts of crown
- If there are horizontal cracks in the coronal portion of the teeth
- When tooth is subjected to excursive occlusal stresses like lateral stresses of bruxism or heavy incisal guidance.

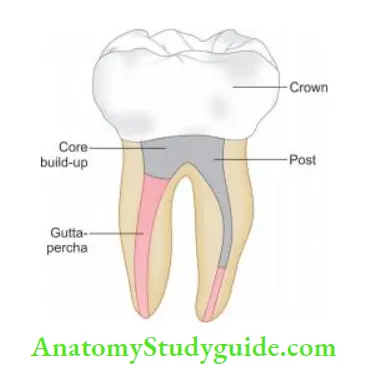
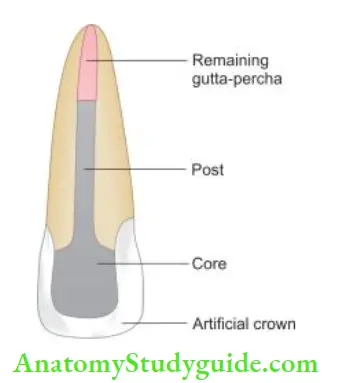
Components Of The Restored Tooth
Components of the restored tooth
Parts of fully restored tooth:
- Residual tooth structure
- Restorative components:
- Post
- Core
- Luting agent
Residual Tooth Structure
The prognosis of an endodontically treated tooth depends on the amount of remaining coronal tooth structure present above the marginal gingiva. A minimum of 1.5–2 mm of the axial wall height of the tooth structure with a thickness of ≥1 mm is shown to significantly reduce the incidence of fracture in nonvital teeth.
This is referred to as the ferrule effect (for details please see page number 445).
Restorative Components
Post
It is a relatively rigid, restorative material placed in the root of nonvital teeth for retention of the core and to transmit the forces on the core to the root (Cohen).
Traditionally, endodontically treated teeth received a post to reinforce them and a crown to protect them.
Purpose of using post
- It helps to retain the core
- It helps to distribute the stresses through the radicular dentin to the root apex
Earlier, it was believed that post strengthens or reinforces the tooth but it has been shown by various studies that posts actually weakens the tooth and increases the risk of root fracture.
Therefore, a post should be used only when there is insufficient tooth structure remaining to support the final restoration.
Ideal requirements of a post
- A post should
- Provide maximum protection of the root to resist root fractures
- Provide maximum retention of the core and crown
- Be easy to place
- Be less technique sensitive
- Have high strength and fatigue resistance
- Be visible radiographically
- Be biocompatible
- Be easily retrievable when required
- Be esthetic
- Be easily available and not expensive
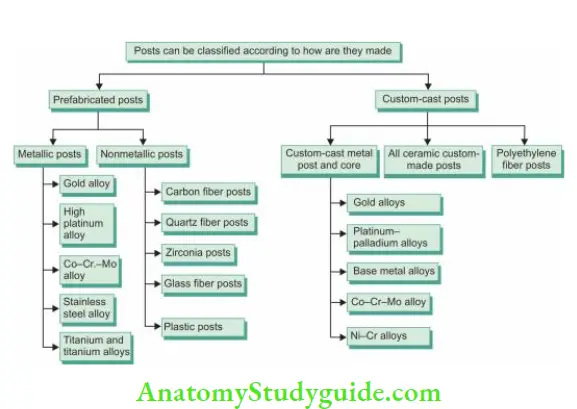
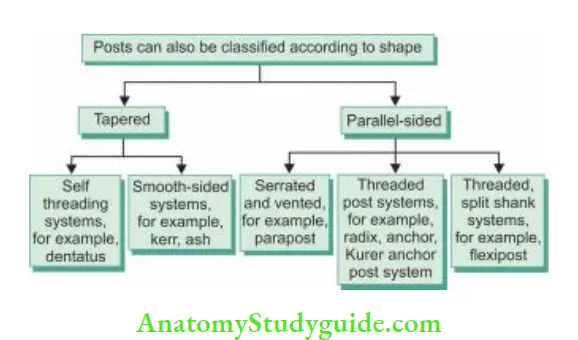
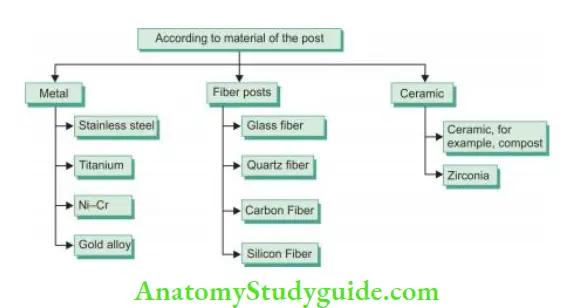
Classification Of Posts

Biomechanical Considerations in Post and Core-Treated Teeth
- The normal tooth under functional forces experiences bending stresses, with compressive stress on one side and tensile stress on the other
- In tooth restored with post and core, the stress distribution pattern is different because post–the core–tooth system bends as a single unit
- The difference in the stress distribution predisposes the tooth structure to increased stress and fracture
- Tensile stresses from the post are transmitted to the tooth with a characteristic pattern depending on the modulus of elasticity (MOE) of the post. MOE of the post should be as near as possible to that of dentin for the best stress distribution
- If a post has a higher modulus than the tooth, the stress concentration is near the apical end of the post. This is evident in cases of the rigid post where root fracture originates at the apex of the post
- When the modulus of the post is similar to that of dentin, stress concentration is near the top of the post resulting in stress concentration near the cervical end. These nonrigid posts result in loss of marginal seal
Stresses produced in
- Tapered post > Parallel post
- Active posts > Passive post
- Shorter post > Longer post
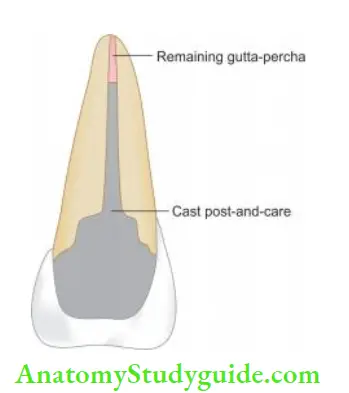
Custom-Cast Metal Post
The custom-fabricated cast gold post and core has been used for decades as foundation restoration. The custom-cast metal post is a post of choice for single-rooted teeth, especially when the remaining coronal tooth structure supporting the artificial crown is minimal.
In such cases, the post must be capable of resisting the rotation which can be better achieved by custom-cast posts.
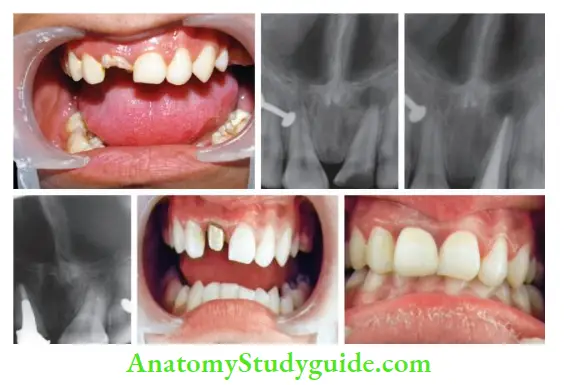
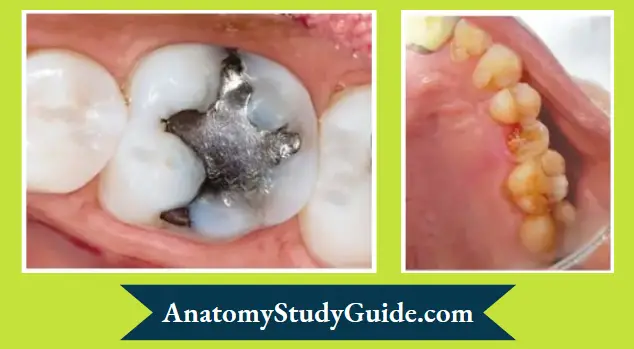
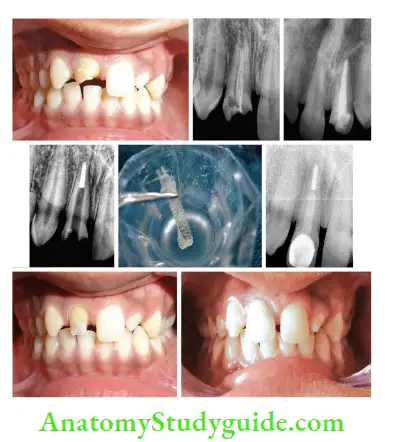
- (A) Preoperative photograph;
- (B) preoperative radiograph showing grossly carious 11;
- (C) Postobturation radiograph;
- (D) Canal space prepared cast and core post-cemented;
- (E) Trial fi of cast post and core;
- (F) Postoperative photograph.

- (A) Preoperative photograph;
- (B) Postoperative photograph;
- (C) Preoperative radiograph;
- (D) Postobturation radiograph;
- (E) Space prepared for the post;
- (F) Postoperative radiograph after cast post and core cementation.

- (A) Preoperative photograph;
- (B) Tooth preparation of right central incisor and cast post and core on left central incisor;
- (C) Postoperative photograph;
- (D) Preoperative radiograph;
- (E) Postobturation radiograph;
- (F) Space prepared for the post;
- (G) Postoperative radiograph after cast post and core cementation.
Custom-Cast Metal Post Advantages
- Adaptable to large irregularly shaped canals
- Better core retention because the core is an inherent part of the post
- In multirooted teeth, they are cost-effective
- A better choice for small teeth
- Beneficial in cases where the angle of the core must be changed in relation to the post
Custom-Cast Metal Post Disadvantages
- Requires more chair side time
- Very rigid so lead to greater stress concentration in root causing root or post-fracture
- Poor esthetics
- Require temporization
- Prone to corrosion
- Risk of casting inaccuracy
- Difficult retrieval
- Hypersensitivity in some cases is because of Ni–Cr ions.
All Ceramic Post and Cores Advantages
- Excellent esthetics
- Biocompatibility
- Good radiopacity.
All Ceramic Post and Cores Disadvantages
- Brittle, so not indicated in high-stress conditions like bruxism
- Very rigid, so more risk of root or post-fracture.
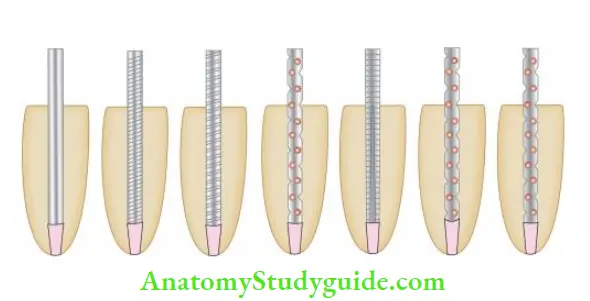
Prefabricated Posts
Indications of Prefabricated Posts
- Sufficient width and length of the root structure is present
- Roots are of circular cross-section, for example, roots of maxillary premolars
- Gross undercuts in root canals make pattern fabrication for cast posts difficult.
Prefabricated Metal Posts
These have been widely used for the past 20 years. They are available in various metal alloys and can be available in active or passive forms.
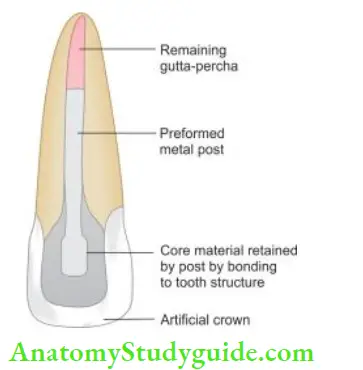
Prefabricated Metal Posts Advantages
- Simple to use
- Less time consuming
- Easy retrieval (of passive posts)
- Available in various shapes and sizes
- Retentive within the root especially serrated and parallel-sided posts
- Radiopaque
- Cost-effective.
Prefabricated Metal Posts Disadvantages
- Not conservative because the root is designed to accept the post
- Cannot be placed in tortuous canals
- Poor esthetics
- Very rigid
- Difficult retrieval of active posts
- Prone to corrosion
- Tapered posts can have wedging effect in the canal.
Carbon Fiber Posts
Carbon fiber posts were introduced by Duret et al. in 1996 based on the carbon fiber reinforcement principle. Carbon fiber post consists of a bundle of stretched carbon fibers embedded into an epoxy matrix. This was the first nonmetallic post introduced to dentistry. Th original form of carbon post was black and unesthetic.
Carbon Fiber Posts Advantages
- Clinical procedure is less time consuming
- Strong but low stiffness and strength than ceramic and metal posts
- Easily retrievable
- Less chair side time
- Modulus of elasticity similar to dentin
- Biocompatible
- Good retention.
Carbon Fiber Posts Disadvantages
- Black in color, so unaesthetic
- Radiolucent, so difficult to detect radiographically
- Flexural strength decreases by 50% of moisture contamination
- On repeated loading show a reduced modulus of elasticity
Glass Fiber Post
It was introduced in 1992. It consists of unidirectional glass fiers embedded in a resin matrix which strengthens the dowel without compromising the modulus of elasticity.
- (A) Preoperative photograph;
- (B) Preoperative radiograph;
- (C) Postobturation radiograph;
- (D) Postspace preparation;
- (E) Customizing fier post;
- (F) Radiograph after post-cementation;
- (G) After tooth preparation;
- (H) Postoperative photograph.
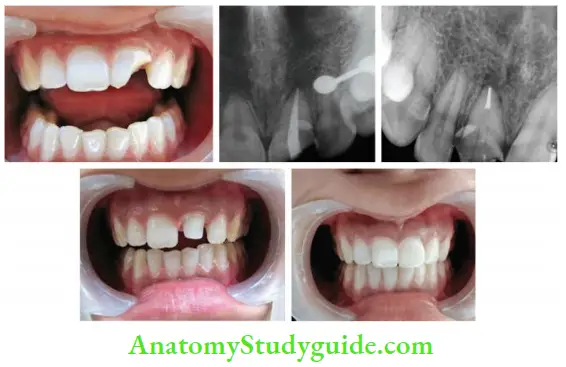
Restoration of right maxillary central incisor using fier post followed by the crown:
- (A) Preoperative photograph;
- (B) Postobturation radiograph;
- (C) Radiograph after fier post placement;
- (D) Composite core build up;
- (E) Postoperative photograph.
Glass Fiber Post Advantages
- Esthetically acceptable
- Modulus of elasticity similar to dentin
- Biocompatible
- Distributes stresses over a broad surface area, thus increasing the load threshold
- Easy to handle and place
- Less time consuming
- Favorable retention in conjunction with an adhesive bonding technique
- High resistance to fracture
- Easy retrieval
Glass Fiber Post Disadvantages
- Poor radiographic visibility
- Expensive
- Technique sensitive
Zirconia Post
These were introduced in dentistry in late 1980 by Christel et al. They are made from fine grained tetragonal\ zirconium polycrystals (TZP).
They possess high flexural strength and fracture toughness.
Glass Fiber Post Advantages
- For teeth with severe coronal destruction, zirconia posts provide adequate strength
- Smaller zirconia posts can be used for an all-ceramic post and core construction for narrower canals
- A combination of glass ceramic and zirconia ceramic can be used because of their similarity in coefficient of thermal expansion
Glass Fiber Post Disadvantages
- Adhesion to tooth and composite is compromised which becomes a problem for retreatment
- They are brittle with a high modulus of elasticity
- When used with direct composite resin buildup, high stresses, and functional forces may lead to microleakage and their deformation because of high polymerization shrinkage and high coefficient of thermal expansion of composites
- Expensive
Factors To Be Considered While Planning Post And Core
The following factors are considered while planning posts:
- Retention and resistance form
- Preservation of tooth structure
- Ferrule effect
- Mode of failure
- Retrievability
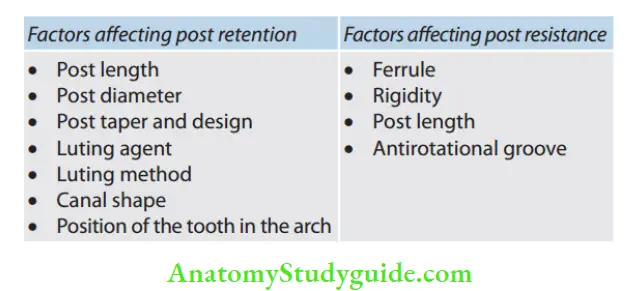
Retention and the Resistance Form
Retention and the resistance form are the two important properties affecting the longevity of the post. Postretention refers to the ability of the post to resist vertical dislodging forces.
Postresistance refers to the ability of the post and the tooth to withstand lateral and rotational forces.
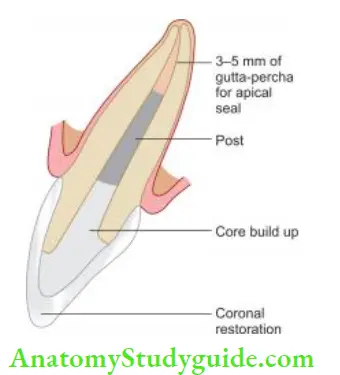
Post Length
The length of the post is one of the most important factors affecting the longevity of the post. As the length of the post increases, so does the retention. About 5% of the failures occur due to the loosening of the post.
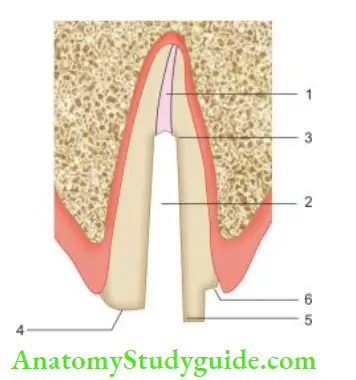
1. Adequate apical seal,
2. Minimum canal enlargement,
3. Adequate post length,
4. Positive horizontal stop,
5. Vertical wall to prevent rotation,
6. Extension of the final restoration margin onto the sound tooth structure
Guidelines regarding post length
- For metal posts (nonadhesive cementation):
- The post should be as long as two-third the length of the canal
- The length of the post should be at least the coronal length of the core
- The post should be at least half the length of the root in the bone
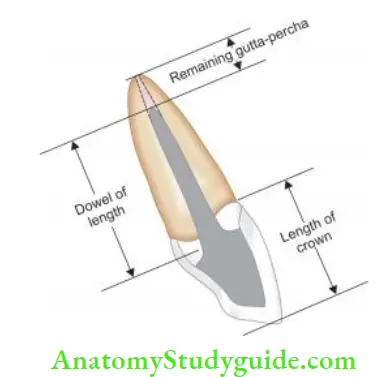
- For fier posts (adhesive cementation):
- The post should extend to a maximum of one-third to one-half the length of the canal
- The length of the post should be at least the coronal length of the core
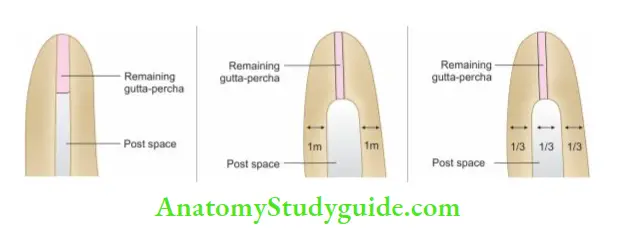
Other important factors to be considered in the selection of the post length include
- The post should be as long as possible without disturbing the apical seal. At least 3–5 mm of the apical gutta-percha should be retained
- To decrease the dentinal stress, the post should extend ≥4 mm apical to the bone crest
- Molar posts should not extend >7 mm apical to the canal orifice so as to avoid the risk of perforation of the root canal
Post Diameter
It has been seen that post diameter has little difference in the retention of a post, but an increase in post diameter increases the resistance form but it also increases the risk of root fracture.
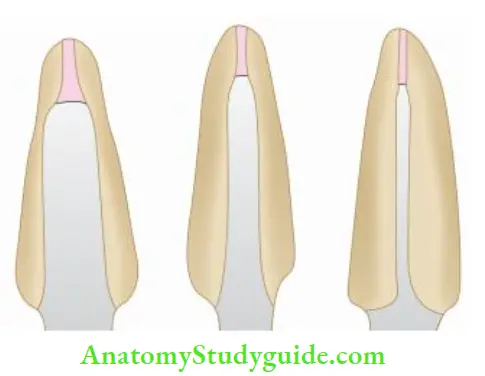
Presently, there are three different theories regarding the post diameter in literature. These are
- Conservationist: It suggests the narrowest diameter that allows the fabrication of a post to the desired length. It allows minimal instrumentation of the canal for post-space preparation. According to this, teeth with smaller dowels exhibit greater resistance to fracture
- Preservationist: It advocates that ≥1 mm of sound dentin should be maintained circumferentially to resist the fracture
- Proportionist: This advocates that post width should not exceed one-third of the root width at its narrowest dimensions to resist fracture. The guideline for determining the appropriate diameter of the post involves the mesiodistal width of the roots.
Post Taper and Design
- Parallel-sided posts may distribute stress more evenly than tapered posts, which may have a wedging effect
- The parallel posts generate the highest stress at the apex
- High stresses can be generated during insertion, particularly with parallel-sided smooth posts with no vent
- Threaded posts produce high stress during insertion and loading.
Luting Agents
The post is retained in the prepared post channel with dental cement. The factors that influence the durability of the bond of the post to the root are compressive strength, tensile strength, and adhesive qualities of the cement, cement’s potential for plastic deformation, microleakage, and water imbibition.
The most common luting cement are zinc phosphate, polycarboxylate, glass ionomer, resin-modified glass ionomer, and resin-based cement. The primary disadvantage of zinc phosphate cement is solubility in oral fluids and lack of true adhesion.

Resin modified glass ionomer cement is not indicated for post cementation, because of its hygroscopic expansion. Currently, the trend is shifting toward the use of adhesive cement. The rationale for using this cement is that adhesive bonding to root canal dentin has to strengthen effect on the tooth in addition to the retention of the restoration.
The disadvantage of resin cement is technique sensitivity. The bonding to root canal dentin can be compromised due to use of various irrigants and eugenol-based sealers. Eugenol can prevent or stop polymerization reactions and can interfere with bonding.
Luting Method
The luting method also affcts the retention of the post. Since luting agents are susceptible to moisture present in the canal, so canal should be absolutely dry.
The optimal method of cementation of posts is
- Dry the canal
- Mix the cement according to the instructions
- Uniformly place the cement in the canal
- Place the post into the canal with the least possible force to reduce the stress
- Vents should be made to release the hydrostatic pressure when the posts thrust back
Canal Shape
The most common shape of the canal is ovoid and prefabricated posts usually come parallel in shape, so these are unlikely to adapt along their entire interface with canal walls.
To determine the appropriate post length and width to avoid root perforation, one must know root taper, proximal root invagination, root curvatures, and angle of the crown to the root during the preparation of the post space.
Position of Tooth in the Dental Arch
The location of the tooth in the dental arch also affects post-retention. For example, the maxillary anterior region is at high risk for failure because of effect of compressive, tensile, shearing, and torquing forces especially at the post–dentin interface.
If all factors are equal, then the post of posterior teeth tends to be more retentive than anterior ones.
Preservation of the Tooth Structure
One should try to preserve a maximum of the coronal and radicular tooth structure whenever possible. Minimal removal of radicular dentin for post-space preparation should be the criteria. Further enlargement of posts only weakens the tooth.
Various studies have shown the use of bonded posts, but their strengthening effect degrades with time because of the weakening of resin dentin bond as the tooth is exposed to functional stress.
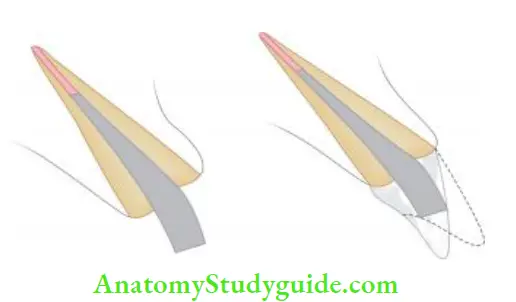
Ferrule Effct
Ferrule is derived from the Latin word Ferrum means iron and variola means bracelet, that is crown bracing against remaining supragingival tooth tissue.
As per “The Glossary of Prosthetic Terms” Ferrule is defined as “a metal ring/band used to fit the root or crown of a tooth. It can be correlated to wine barrels. The metal band, which encompasses the wooden barrel, gives support when the barrel is full.”
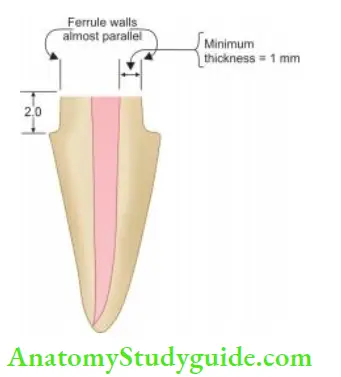
According to Sorensen and Engelman, the ferrule is defined as the “360° metal collar of the crown surrounding the parallel walls of the dentin extending coronally to the shoulder of the preparation”.
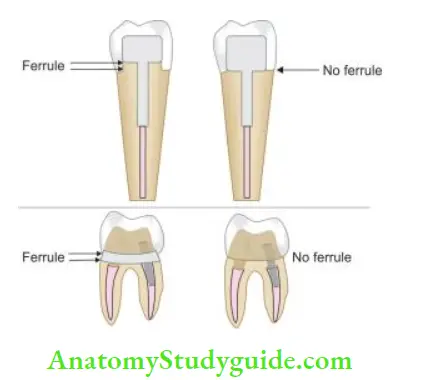
It has been seen that a ferrule with 1–2 mm of vertical tooth structure doubles the resistance to fracture than in teeth without any ferrule effect. This is called as crown ferrule that is, the crown ferrule is ferrule created by overlying crown engaging the tooth structure. The core ferrule is part of cast metal.
The height of the ferrule may vary according to different functional occlusal loading. For example, the maxillary incisor needs a longer ferrule on the palatal aspect and the mandibular incisor needs a longer ferrule on the labial aspect.
Sometimes when adequate tooth structure is not present, crown lengthening or orthodontic eruption is needed of a tooth to provide an adequate ferrule.
Requirements of the Ferrule
- The axial wall height of the ferrule must be ≥1–2 mm
- The ferrule should consist of parallel axial walls
- The margins of the preparation should rest on the sound tooth structure
- Restoration should completely encircle the tooth
- The restoration should not completely encroach on the biological width. A minimum of 4–5 mm of supra bony tooth structure should be available to accommodate for the restoration and attachment apparatus
- A ferrule with a minimum thickness of 1 mm is needed to be effctive
Functions of Ferrule
Sorensen and Engelman (1990) found that 1.5–2 mm of ferrule reduces the fracture resistance of endodontically treated teeth. They showed that the protective effect of the ferrule is because
- It dissipates the forces that concentrate at the cervical area of the clinical crown. Lack of ferrule may result in fracture because of forcing core, post, and root to high function stresses
- It protects the integrity of the root by bracing action
- It reduces the lateral forces exerted during post insertion
- It resists the wedging effect of the tapered posts
- It resists the functional lever forces

Secondary Ferrule/Core Ferrule
Sometimes a contra bevel is given on a tooth being prepared for a cast post with a collar of metal which encircles the tooth. This serves as secondary ferrule independent of ferrule provide by the cast crown.
Mode of Failure
All post systems show some percentage of failure but with a variable range. Post failures are higher in cases of nonrestorable teeth.
Factors affecting clinical longevity of post and core
- Magnitude and direction of force
- Tooth type
- Thickness of remaining dentin
- Post selection
- Quality of cement layer
Failures of posts and core can occur in the form of
- Post fracture
- Root fracture
- Core fracture
- Post dislodgement
- Esthetic failures

Retrievability
Ideally, a post system selected should be such that if an endodontic treatment fails, or failure of post and core occurs, it should be retrievable.
Metal posts especially the cast post and core system is difficult to remove.
Fiber posts are easy to retrieve, whereas zirconium and ceramic posts are difficult to remove.
Posts can be removed by
- Use of rotary instruments and solvents
- Use of ultrasonic
- Using special kits like Masserann kit, post-removal system, and endodontic extractors
Preparation Of The Canal Space And The Tooth
- Take a radiograph and assess the case for the length and diameter of the post according to the tooth type. Remove the gutta-percha filing from the root canal while maintaining the apical seal
- Prepare the canal space using Gates-Glidden drills or Peeso reamers. The canal space enlargement depends on the type of the post. If it is custom-made, the main requirement is minimal space preparation without undercuts.
- For prefabricated posts, generally, specific penetration drills for each system are supplied for canal preparation
- Various errors can occur during root canal preparation for post-space-like periapical extrusion of obturation material, disturbance of apical seal, over-enlargement of the canal space, and perforation
- Following the preparation of canal space, preparation of, coronal tooth structure should be prepared in the same manner as if an intact crown irrespective of the remaining tooth structure
- Remove all the unsupported tooth structure
- Place an anti-rotational notch with the help of a cylindrical diamond or carbide bur. This is done to provide the anti-rotational stability
- Ferrule effect is provided thereafter. The remaining coronal tooth structure is sloped to buccal and lingual surfaces so as to provide a collar around the occlusal circumference of the preparation.
- This gives rise to 360° ferrule effect. Ferrule ensures that the final restoration encircles the tooth apical to the core and rests on a sound tooth structure. It also presents the vertical root fracture by posts
- Finally, eliminate all the sharp angles, and undercuts and establish a smooth finish line.

Core
The core is the supragingival portion that replaces the missing coronal tooth structure and forms the center of the new restoration. Basically, it acts as a miniature crown.
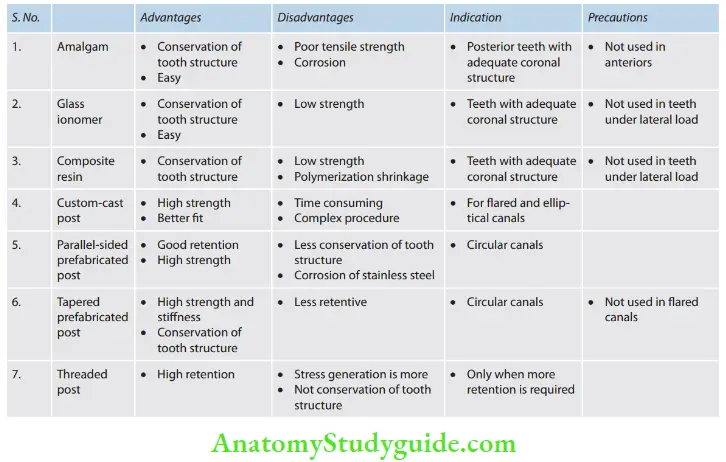
Core build-up materials available are
- Dental amalgam
- Resin-modifid glass ionomers
- Composite resin
- Reinforced glass ionomers cement
Ideal requirements for a core material
- Compressive strength to resist intraoral forces
- Biocompatibility
- Ease of manipulation
- Flexural strength to present core dislodgement
- Ability to bond to the tooth structure and post
- Coefficient of thermal expansion similar to dentin
- Minimal water absorption
- Dimensionally stable
- No reaction with chemicals
- Low cost
- Easily available
- A contrasting color to tooth structure except when used for anterior teeth
Composite Resins
Composite resin is the most popular core material and has some characteristics of an ideal build-up material.
Composite Resins Advantages
- Bonded to many of the current posts and to the remaining tooth structure to increase retention
- High tensile strength and the tooth can be prepared for a crown immediately after polymerization
- It has fracture resistance comparable to amalgam and cast post and cores, with a more favorable fracture pattern when they fail. It is tooth-colored and can be used under translucent restorations without affecting the esthetic result
Composite Resins Disadvantages
- Composite shrinks during polymerization, causing gap formation in the areas in which adhesion is weakest. It absorbs water after polymerization, causing it to swell and undergoes plastic deformation under repeated loads
- Adhesion to dentin on the pulpal floor is generally not as strong or reliable as to coronal dentin. Strict isolation is an absolute requirement. If the dentin surface is contaminated with blood or saliva during bonding procedures, the adhesion is greatly reduced. Although composite resin is far from ideal, it is currently the most widely used build-up material
Cast Core
The core is an integral extension of the post and it does not depend upon the mechanical means of retention on the post. It prevents dislodgement of the core and the crown from the post. But sometimes valuable tooth structure must be removed to create a path of withdrawal. The procedure is time-consuming and expensive.
Amalgam Core
- Amalgam has been used as a build-up material, with well-recognized strengths and limitations. It has good physical and mechanical properties and works well in high-stress areas
- In many cases, it requires the addition of pins or other methods to provide retention and resistance to rotation. Placement can be clumsy when there is minimal coronal tooth structure and the crown preparation must be delayed to permit the material time to set.
- Moreover, amalgam can cause esthetic problems with ceramic crowns, it makes the gingiva look dark. There is a risk of tattooing the cervical gingiva with amalgam particles during the crown preparation.
- For these reasons and potential concerns about mercury, it is no longer widely used as a build-up material.
- Amalgam has no natural adhesive properties and should be used with an adhesive system for buildup
Glass Ionomer Cements
The glass ionomer materials, including resin-modified glass ionomer, lack adequate strength and fracture toughness as a build-up material and should not be used in teeth with extensive loss of tooth structure.
It is also soluble and sensitive to moisture. When there is minimal loss of tooth structure and a post is not needed, GIC works well for block out such as after removal of a MOD restoration.
Biomechanical criteria for evaluation of core materials
- Bonding (maximum to least) Resin composites > glass ionomers> amalgam
- Strength Amalgam > resin composite > glass ionomers
- Ease of use Resin composites > amalgam > glass ionomers
- Setting time Resin composite > glass ionomers> amalgam
- Dimensional stability Amalgam > glass ionomers> composite resins
Custom-Made Post
A custom-made post can be cast from a direct pattern fabricated in the patient’s mouth, or an indirect pattern can be fabricated in the dental laboratory.
Direct Procedure
- Lightly lubricate the canal and notch a loose fitting plastic dowel. It should extend to the full depth of the prepared canal. Use the bead-brush technique to add resin to the dowel and seat it in the prepared canal
- Do not allow the resin to harden fully within the canal. Loosen and reseat it several times while it is still rubbery
- Once the resin has polymerized, remove the pattern Form the apical part of the post by adding additional resin and reseating and removing the post, taking care not to lock it in the canal
- Identify any undercuts that can be trimmed away carefully with a scalpel
The post pattern is complete when it can be inserted and removed easily without binding in the canal. Once the pattern has been made, additional resin is added for the core.
Indirect Procedure
- Any elastomeric material will make an accurate impression of the root canal if a wire reinforcement is placed to prevent distortion
- Cut pieces of orthodontic wire to length and shape them like the letter J. Verify the fit of the wire in each canal. It should fit loosely and extend to the full depth of the post space. If the fi is too tight, the impression material will strip away from the wire when the impression is removed
- Coat the wire with tray adhesive. If subgingival margins are present, tissue displacement may be helpful.
- Lubricate the canals to facilitate the removal of the impression without distortion
- Using a lentils spiral, fill the canals with elastomeric impression material. Before loading the impression syringe, verify that the lentils will spiral material in an apical direction (clockwise). Pick up a small amount of material with the largest lentil spiral that fits into the post space
- Insert the lentils with the handpiece set at low rotational speed to slowly carry material into the apical portion of the post space. Then increase handpiece speed and slowly withdraw the lentils from the post space
- This technique prevents the impression material from being dragged out. Repeat until the post space is filed
- Then insert the impression tray. Remove the impression, evaluate it, and pour the working cast. In the laboratory, roughen a loose-fitting plastic post and, using the impression as a guide, make sure that it extends into the entire depth of the canal
- Apply a thin coat of sticky wax to the plastic post and, after lubricating the stone cast, add soft inlay wax in increments. Start from the most apical and make sure that the post is correctly oriented as it is seated to adapt the wax. When this post pattern has been fabricated, the wax core can be added and shaped
Core Fabrication
- The core of a post-and-core restoration replaces the missing coronal tooth structure and thereby forms the shape of the tooth preparation. It can be shaped in resin or wax and added to the post pattern before the assembly is cast in metal. This prevents possible failure at the post-core interface
- The core can also be cast onto most prefabricated post systems (although there is then some concern that the casting process may unfavorably affect the physical properties of wrought metal posts)
- A third alternative is to make the core from a plastic restorative material such as amalgam, glass ionomer, or composite resin
Investing And Casting
- A cast post-and-core should fi somewhat loosely in the canal. A tight fi may cause root fractures
- The casting should be slightly undersized, which can be accomplished by restricting the expansion of the investment (i.e., by omitting the usual ring liner or casting at a lower mold temperature)
- The casting alloy should have suitable physical properties. Extrahard denture gold (ADA Type 4) or nickel-chromium alloys have high moduli of elasticity and are suitable for cast posts
- A sound casting technique is essential because any detected porosity could lead to a weakened casting that might fail in function. Casting a core onto a prefabricated post avoids problems of porosity
Evaluation
The practitioner must be particularly careful that casting defects do not interfere with the seating of the post; otherwise, root fractures will result. Post-and-cores should be inserted with gentle pressure.
However, the marginal fi of a cast foundation is not as critical as that of other cast restorations, because the margins will be covered by the final casting. The shape of the foundation is evaluated and adjusted as necessary.
No adjustments should be made immediately after cementation because the vibration from the bur could fracture the setting cement and cause premature failure.
Cementation
The luting agent must fill all dead space within the root canal system. Voids may be a cause of periodontal inflmmation via the lateral canals. A rotary (lentils) paste filer or cement tube is used to fill the canal with cement.
Th post-and-core is inserted gently to reduce hydrostatic pressure, which could cause root fracture. If a parallel-sided post is being used, a groove should be placed along the side of the post to allow excess cement to escape.
Restoration Of Endodontically Treated Teeth Conclusion
Following the endodontic treatment, it is necessary to restore the original morphology and function of the tooth which can be achieved by restoration of the endodontically treated teeth. The restoration should begin at the earliest possible because teeth exposed to oral conditions without optimal restoration cannot resist the occlusal forces and oral bacteria for a long period which can result in treatment failure.
Restoration of an endodontically treated tooth begins with an understanding of its physical and biomechanical properties and anatomy. Through various new materials that have become available over the past many years, the basic concepts of restoring endodontically treated teeth remain the same. Most post systems can be used successfully if basic principles are followed.
After the selection of the post system, finally, it is the choice of core material and final restoration which increases the longevity of the treated tooth. Selection of a post should be made by keeping in mind its strength, modulus of elasticity, biocompatibility, retrievability, esthetics, and cost.
Leave a Reply