Surgical Endodontics – Presurgical Considerations
Before initiating the surgical procedure, the clinician should evaluate the following factors which affect the treatment outcome:
Table of Contents
- The success of surgical treatment versus nonsurgical retreatment
- Review of the medical history of the patient and consultation with the physician if required
- Patient motivation
- Aesthetic considerations like scarring
- Evaluation of anatomic factors by taking radiographs at different angles
- Periodontal evaluation
- Presurgical preparation
- Taking informed consent.
Read And Learn More: Endodontics Notes
Protocol of treatment
- Intraoral and localized swelling—only incision and drainage
- Diffuse swelling or it has spread into extraoral facial tissues or spaces—surgical drainage and systemic antibiotics
- Hard, indurated, and diffuse swelling—allow it to localize, become soft and fluctuant before incision and drainage
Surgical Incision And Surgical Drainage
Surgical Drainage Surgical drainage is indicated when purulent and/or hemorrhagic exudates forms within the soft tissue or the alveolar bone as a result of a symptomatic periradicular abscess
Surgical Drainage Steps
- Give local anesthesia
- Give an incision to the most dependent part of swelling with a scalpel blade, No. 11 or No. 12. Place a horizontal incision at the dependent base of the fluctuant area for effective drainage to occur.
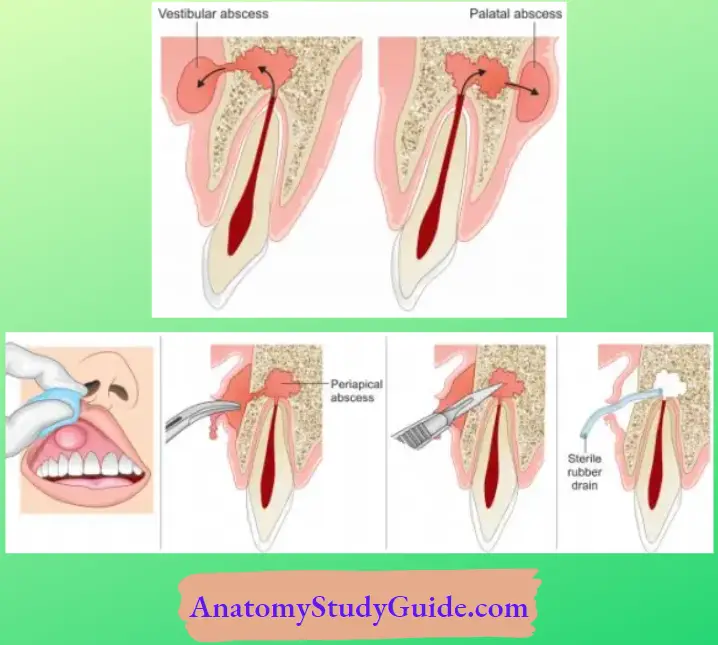
- (A) Large vestibular abscess;
- (B) Vestibular abscess is formed due to large periradicular abscess;
- (C) Incision is given at most dependent part of the lesion;
- (D) Drainage tube to drain the purulent exudates.
Periradicular Surgery
Local Anesthesia and Hemostasis
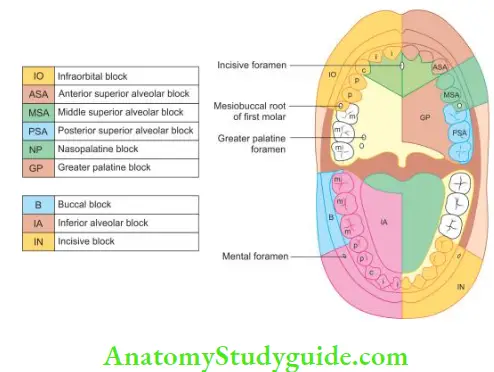
- Lidocaine with adrenaline is the local anesthesia of choice to obtain profound anesthesia and optimal hemostasis. If amide is contraindicated, then an ester agent, that is, procaine, proparacaine with levonordefrin, is indicated
- For nerve blocks, 2% lidocaine with 1:100,000 or 1:200,000 adrenaline is used. But for obtaining hemostasis, adrenaline concentration should be 1:50,000
- The rate of injection should be 1 mL/min with the maximum safe rate of 2 mL/min. The rapid injection produces localized pooling of solution in the injected site resulting in delayed and limited diffusion into the adjacent tissue, thus surface contact with microvasculature reduces, resulting in reduced hemostasis. Hemostasis is clinically indicated by the blanching of soft tissues
- Submucosal infiltration for hemostasis should be given with 30 gauze needles with the bevel toward bone and penetration just superficial to the periosteum at the level of root apices.
Receptor and mechanism of hemostasis
- Gage demonstrated that the action of a vasopressor drug on microvasculature depends on the predominant receptor type:
- α-Receptors—Stimulation of α-receptors (mainly in oral mucosa and gingiva) causes vasoconstriction, thus decrease in the blood flow
- β-Receptors—Stimulation ofβ-receptors (skeletal muscles) causes vasodilatation
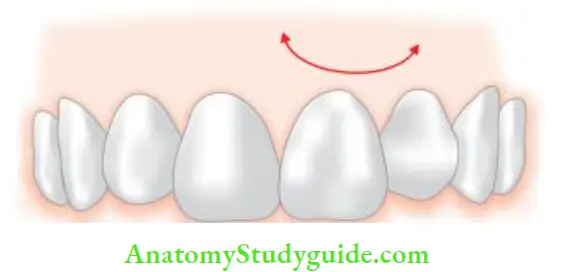
Reactive hyperemia: rebound phenomenon
- In reactive hyperemia, the concentration of vasoconstrictor decreases so it does not cause α adrenergic response but after some time blood flow increases more than normal leading to reactive hyperemia. It occurs due to rebound from an α to β response
- The rebound phenomenon is because of localized tissue hypoxia and acidosis caused by prolonged vasoconstriction
- Once this reactive hyperemia occurs, it is impossible to re-establish hemostasis by additional injections
Flap Designs And Incisions
Principles and Guidelines for Flap Designs
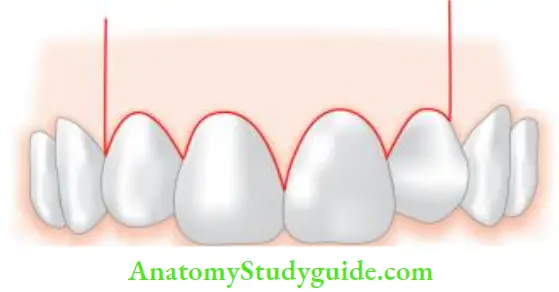
- Avoid horizontal and severely angled vertical incisions, because
- Gingival blood supply occurs from subperiosteal vessels and these follow a vertical course parallel to the long axis of teeth
- Collagen fibers of the gingiva and alveolar mucosa form attachments for crystal bone and suprarenal cementum to the gingiva and periosteum of radicular bone
- Avoid incisions over radicular eminences (for example in canines and maxillary first premolars)
- Incisions should be placed such that flap is repositioned over solid bone
- The base of the flip should be more than free margin to preserve an adequate blood supply
- Incisions should never be placed over areas of periodontal bone loss or periradicular lesions
- Hooley and Whitacre suggested that a minimum 5 mm of bone should exist between the edge of a bony defect and the incision line
- The extent of vertical incisions should be sufficient to allow the tissue retractor to seat on solid bone, thereby leaving the root apex well exposed
- The extent of horizontal incision should be adequate to provide visual and operative access with minimal soft tissue trauma
- Avoid incisions in the mucogingival junction
- Junction of horizontal sulcular and vertical incisions should either include or exclude the involved interdental papilla
- When the submarginal incision is used, there must be a minimum of 2 mm of attached gingiva around each tooth to be flapped.
Functions of a Flap
- Raise the soft tissue to give the best possible view and exposure of the surgical site
- To provide healthy tissue that will cover the area of surgery, decrease pain by eliminating bone exposure, and aid in obtaining optimal healing
Flap Classifiation
- Full mucoperiosteal flaps
- Triangular (single vertical releasing incision)
- Rectangular (double vertical releasing incision)
- Trapezoidal (broad-based rectangular)
- Horizontal (no vertical releasing incision)
- Limited mucoperiosteal flaps
- Submarginal curved (semilunar)
- Submarginal scalloped rectangular (Luebke-Ochsenbein)
Full Mucoperiosteal Flaps
In this, the entire soft tissue overlying the cortical plate in the surgical site is reflected. The major advantage of this type of flip is that subperiosteal vessels are maintained intact.
But disadvantages are postsurgical flap dislodgement, loss of soft tissue attachment level, and crestal bone height.
Triangular Flap (Fischer in 1940)
It is a full-thickness most commonly used flap in endodontics.
Triangular Flap Indications
- Maxillary incisor region
- Maxillary and mandibular posterior teeth
- It is the only recommended flap design for the posterior mandible region.
Triangular Flap Contraindications
- Teeth with long roots (maxillary canine)
- Mandibular anterior because of the lingual inclination of their roots.
Triangular Flap Advantages
- Enhanced rapid wound healing
- Ease of wound closure.
Triangular Flap Disadvantage
- Limited surgical access.
Rectangular Flap
It is an extension of the triangular flap. Here two vertical releasing incisions and a horizontal intracellular incision is given.
Rectangular Flap Indications
- Mandibular anterior
- Maxillary canines
- Multiple teeth.
This flap is not recommended for mandibular posterior teeth.
Rectangular Flap Advantages
- Enhanced surgical access
- Easier apical orientation
- Excellent wound healing potential.
Rectangular Flap Disadvantages
- Wound closure as flap reapproximation and postsurgical stabilization are more difficult than triangular flap
- The potential for flap dislodgement is greater.
Trapezoidal Flap
It was described by Neumann and Eikan in 1940. Trapezoidal flap is formed by two releasing incisions which join a horizontal intracellular incision at obtuse angles.
- Trapezoidal Flap Disadvantages
- Wound healing by secondary intention
- Pocketing or clefting of soft tissue
- Compromise in blood supply
- Contraindicated in periradicular surgery.
Envelope Flap
It is formed by a single horizontal intracellular incision and is usually recommended for corrective endodontic surgery.
Envelope Flap Indications
- For repair of perforation defects
- For root resections
- In cases of hemisections.
Envelope Flap Advantages
- Improved wound healing
- Easiness of wound closure and postsurgical stabilization.
Envelope Flap Disadvantages
- The extremely limited surgical access
- Essentially impractical for periradicular surgery, but some use it for palatal surgery.
Limited Mucoperiosteal Flaps
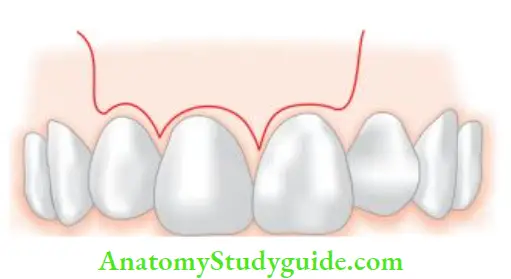
Semilunar Flap
- It was first given by Partsch, also known as Partsch incision.
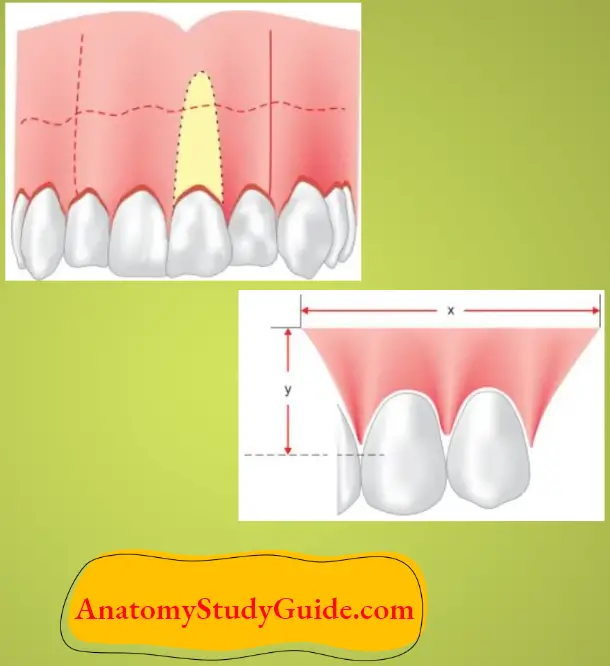
- It is formed by a single curved incision. It is called as semilunar flap because the horizontal incision is modified to have a dip toward the incisal aspect in the center of the flap, giving a resemblance to the half-moon.
Semilunar Flap Advantages
- Fast and easy to reflect
- No involvement of marginal and interdental gingiva.
Semilunar Flap Disadvantages
- Limited surgical access
- Difficult wound closure
- Poor apical orientation
- Potential for postsurgical soft tissue defects by incising through tissues unsupported by bone
- Maximum disruption of blood supply to unflipped tissues.
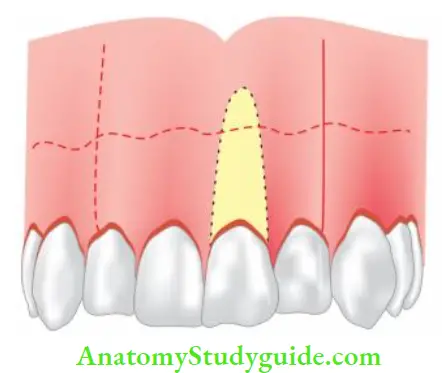
Ochsenbein-Luebke Flap/Submarginal Scalloped Rectangular Flap
- Ochsenbein-Luebke flp was developed by an endodontist and periodontist
- It is modification of a rectangular flap
- In this, a scalloped horizontal incision is given in the attached gingival which forms two vertical incisions made on each side of the surgical site.

Ochsenbein-Luebke Flap/Submarginal Scalloped Rectangular Flap Indications
- In the presence of gingivitis or periodontitis associated with field prosthesis
- Where bony dehiscence is suspected.
Ochsenbein-Luebke Flap/Submarginal Scalloped Rectangular Flap Advantages
- Marginal and interdental gingiva are not involved
- Unaltered soft tissue attachment level
- Crestal bone is not exposed
- Adequate surgical access
- Good wound healing potential—as compared to semilunar flap.
Ochsenbein-Luebke Flap/Submarginal Scalloped Rectangular Flap Disadvantages
- Disruption of blood supply to unflipped tissues
- Flap shrinkage
- Difficult flip reapproximation and wound closure
- Untoward postsurgical sequelae
- Healing with scar formation
- Limited apical orientation
- Limited or no use in mandibular surgery.
Leave a Reply