The Central Nervous System
Table of Contents
The examination and evaluation of the nervous system in children is a daunting task. Some ingenuity, use of special tricks, and adoption of a non-structured “play attitude” is mandatory to elicit cooperation and best dividends.
Like other body organs, the central nervous system in children is a dynamic, developing, and maturing system. A newborn baby has a brain weight of about 70% of an adult, while his body weight is only 5% of average adult weight. Almost 15% brain growth occurs during the first year of life and about 10% during the remaining preschool years.
Read and Learn More Pediatric Clinical Methods Notes
Developmental disorders due to hypoxia, congenital anomalies, and inborn errors of metabolism are by and large limited to children. The possibility of the neurological symptoms being due to a systemic disease rather than CNS disease, is more likely in children than adults.
Anatomy
The nervous system consists of the brain and spinal cord (central nervous system) and peripheral nerves(peripheral nervous system). The neuron has a cell body and axon which terminates at a synapse and constitutes the functioning unit of the nervous system.
Astrocytes provide the structural framework for die neurons and control their biochemical environment and provide die blood-brain barrier. The brain consists of two cerebral hemispheres, each with four functionally specialized lobes, the brainstem, and cerebellum.
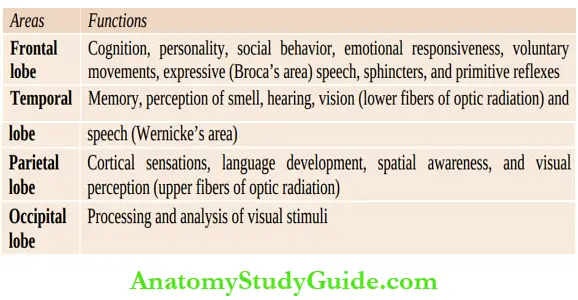
The cortical functions of various lobes are listed in. The brainstem consisting of die midbrain, pons, and medulla oblongata, contains die nuclei of cranial nerves and all die sensory and motor pathways entering and leaving the cerebral hemispheres.
The cerebellum, which lies below the cerebral hemispheres and posterior to die brainstem, is responsible for coordination, posture, and steady gait. The brain is covered by three membranes, die outermost dura mater, middle arachnoid, and innermost pia mater.
The subarachnoid space between the arachnoid and pia is filled with cerebrospinal fluid. The spinal cord contains afferent and efferent fibers, which are arranged in functionally discrete bundles, are responsible for motor reflexes, sensory information for touch, temperature, pain, and proprioception.
Peripheral nerves are made up of large myelinated axons and smaller slower unmyelinated axons. The sensory cell bodies of peripheral nerves are situated in the dorsal root ganglia while the motor cell bodies are located in the anterior horn cells of the spinal cord.
The left and right hemispheres are credited to have different functions and attributes. The left hemisphere (dominant hemisphere) is endowed with masculine characteristics, like cognition, logic, reasoning, analytical skills, language, communication skills, public speaking, mathematical skills, etc.
The right hemisphere is credited with feminine or artistic characteristics, like painting, music, dance, poetry, peace, poise, insight, extrasensory perception or intuition, creativity, spirituality, etc. We are all provided with mixed characteristics of both right and left hemispheres in various combinations.
Ask for presenting complaints. Identify the precise timing and onset of the neurological disease, whether acute, subacute or insidious. Record the evolution or progression of the disease process.
Assess whether the disease is stationary, progressive, or improving. Ask in detail the developmental status of the child before the onset of the disease.
Preceding or concurrent history of fever and its severity should be asked. History of perinatal distress factors and abnormalities, head injury and immunizations before the onset of CNS manifestations should be recorded.
Ask for any history of medications and accidental or suicidal poisoning in a comatose child. Headache, neck and/or spinal stiffness and photophobia are suggestive of meningeal irritation.
Ask for symptoms suggestive of raised intracranial tension, such as headache, especially on rising up in the morning, vomiting without preceding nausea, enlargement of head size, and diplopia. Excessive and unexplained high-pitched crying may be the sole symptom of raised intracranial tension (ICT) in infants.
Rarely, raised intracranial pressure may cause stretching and compression of the intracranial component of vagus nerve leading to the development of stridor due to bilateral vocal cord paralysis. The salient components of history are summarized in
Key points on history:
- Presenting symptoms
- Onset: Sudden, subacute, insidious
- Fever: Preceding or concurrent and its severity
- Neuromotor development before the onset of CNS disease
- Evolution: Is the condition improving, stationary, slowly progressive or rapidly progressive?
- Are there any symptoms suggestive of raised intracranial tension and meningeal irritation?
- Seizures and their morphology
- Is there any involvement of special senses and sphincters?
- Mental status: Alert, irritable, lack of interest, drowsy, stuporous or comatosed
- Family history of similar disease, epilepsy, tuberculosis, an inborn error of metabolism, and
consanguinity - Etiologic history: Perinatal events, trauma, drugs and toxins, infection or post-infectious degenerative disorder
Enquire details about any seizures, i.e. onset, type, precedingaura, seizure morphology, postseizure phenomenon, frequency of fits, and response to previous treatment.
Ask about any disturbances referable to special senses and sphincters. Family history of similar disease, tuberculosis and epilepsy should be enquired. The history of consanguinity among parents should be asked.
General Physical Examination
The ‘containers’ of CNS, i.e. skull and spine should be examined in detail. Look for size, shape, symmetry, swellings, sutures, and fontanels of skull. In craniosynostosis, skull becomes oddshaped because of the cessation of growth of the skull bones at right angle to the prematurely fused sutures. Macewen’s sign (cracked pot sound on percussion of skull) should be looked for.
It is physiological during early infancy because sutures are open. Auscultation and transillumination of skull is useful in selected cases. Look for any operative scars on the spine due to repair of meningomyelocele or over the scalp for placement of ventriculoperitoneal shunt.
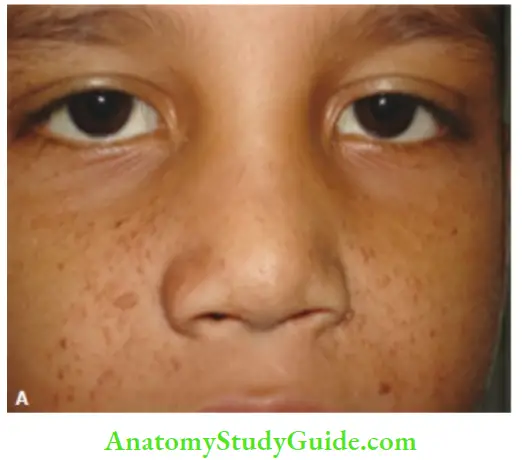
Face should be examined for any dysmorphism and characteristic facies suggestive of developmental, chromosomal, and metabolic disorders. Obesity, sleep disturbances, and features of diabetes inspidus are suggestive of hypothalamic disorder. The skin should be screened for any evidences of neuroectodermal dysplasia,
For example, Adenoma sebaceum, strawberry mark on the face, telangiectasia of bulbar conjunctiva or vascular malformation of the retina, café-au-lait spots, shagreen or ash-leaf spots, etc. Skin rash and petechiae should be looked for. Teeth should be examined for brownish discoloration and blueline over the gums and Hutchison’s teeth.
Eyes should be examined for proptosis, corneal opacities, buphthalmos, Kayser-Fleischer ring (golden-green discoloration in the form of crescent in the inner layer of peripheral cornea just inside the limbus), and cataracts.
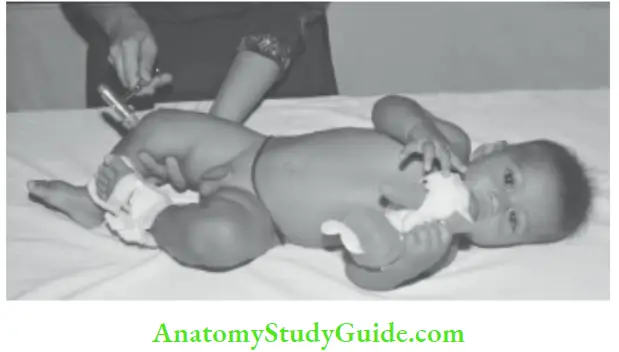
Vital signs should be recorded keeping in mind that bradycardia, rise in blood pressure and Cheyne-Stokes breathing may be indicative of raised intracranial tension. Trousseau’s sign(carpopedal spasms) and nerve irritability (Chvostek’s sign) should be looked for in a child with history of tetanic spasms.
In the Chvostek sign, tapping of the facial nerve just anterior to the tragus, results in contraction of the facial muscles with blinking of eyelids and twitching of the corner of the mouth. Although a useful sign of tetany, it may be present in normal newborn babies.
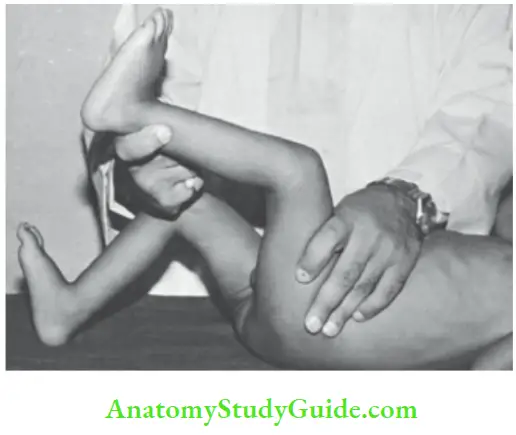
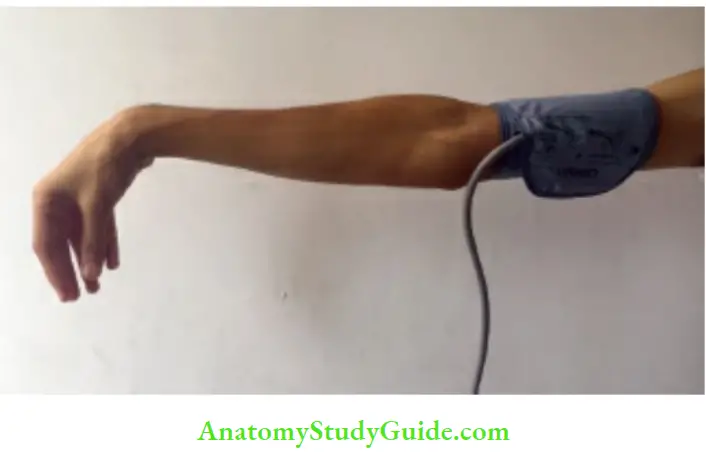
Carpopedal spasms or Trousseau’s sign can be elicited by occlusion of the blood vessels with a sphygmomanometer cuff. The cuff is inflated beyond the systolic blood pressure and held in place for 3 minutes.
The peroneal sign is elicited by tapping the peroneal nerve over the head of the fibula. The sign consists of dorsiflexion and eversion of the foot.



Record temperature, pulse, respiration and blood pressure. Look for Cushing’s response to raised intracranial tension, i.e. bradycardia, elevation of blood pressure, and abnormalities in respiratory pattern.
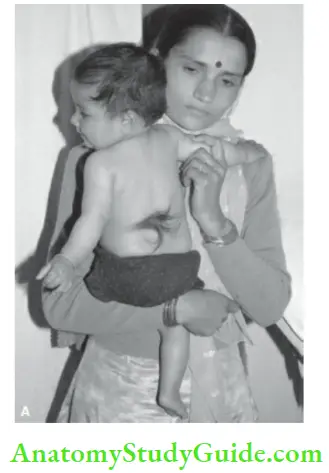
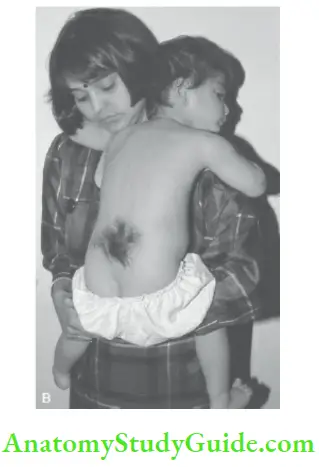
Look for anemia, cyanosis, jaundice, lymphadenopathy, hepatosplenomegaly, and abdominal mass. Spine should be examined for any evidences of developmental defects (platybasia, Klippel-Feil deformity, meningocele, pilonidal sinus, a tuft of hair, etc.), trauma, Pott’s disease, epidural abscess, primary neoplasm or metastatic deposits.
Sinus tract over the region of dorsal spine and fracture of base of skull may be associated with recurrent pyogenic meningitis. Enquire whether child is right or left handed. The handedness is established around 3 years of age.
Left handers have a diffuse representation of language function in the brain and their recovery from aphasia is better compared to right handers.
If an infant below 2 years has a preference to use one limb, it suggests weakness or paralysis of the other limb. The salient components of general physical examination are listed in
Key points on general physical examination:
- General appearance, posture, nature of the disability, build and nutrition, and anthropometry
- Skull and spine: Size, shape, sutures, fontanels, Macewen’s sign, auscultation, transillumination, and spinal deformities
- Facial dysmorphism, abnormalities of teeth, eyes, ears, and oral cavity, and evidence of neuroectodermal dysplasia
- Anemia, cyanosis, jaundice, hepatospleno-megaly, and abdominal mass
Vital signs including Trousseau’s sign - Evidences of meningeal irritation: Neck rigidity, Kernig’s sign,
- Brudzunski’s sign, tripod sign, and photophobia
- Evidences of raised intracranial pressure: Cushing’s response, i.e. bradycardia, elevation of blood pressure and abnormalities in respiratory pattern.
- Evidences of herniation of the hippocampus, i.e. unilateral dilated and fixed pupil, paralysis of upward gaze with involvement of vital centers in brainstem. Macewen’s sign and papilledema
- Handedness of the child
Examination Of the Central Nervous System
Most pediatricians lack the confidence and are often frustrated while conducting neurological examination of young children. With tact, experience and patience, the neurological examination of an infant should not be an ordeal, rather it should be fun both for the examiner and the patient.
Adopt an attitude of play activity in conformity with the age and developmental status of the child. Harness your ingenuity, imagination, and tact effectively by literally coming down to the level of the child. Smiling at the infant and speaking in soft and reassuring tones during the examination are highly effective to elicit cooperation.
Attempt should be made to identify all neurological abnormalities, localize the probable site of lesion in CNS and identify etiology and diagnosis of the disease process. The salient components of CNS examination are summarized in
Key points on CNS examination:
- Higher functions: Level of consciousness, orientation in time and place, memory, emotional status, and speech
- Developmental screening and handedness of the child
- Cranial nerves
- Motor system: Posture, muscle bulk, tone, power, trophic changes, abnormal movements, coordination, deep tendon jerks, and gait
- Sensory system
- Superficial reflexes
- Brainstem signs
- Cerebellar signs
- Autonomic dysfunction
- Localization of the lesion
Essential Tools
The pediatric neurologist should have colored toys/cubes, a reflex hammer, bell, flashlight with rubber adaptor, fiberglass tape measure, objects for testing stereognosis, tuning fork (128 Hz for vibration sense and 256 Hz for Rinne test), a two-point discriminator, development kit, and ophthalmoscope.
Higher Mental Functions
1. Level of consciousness :
The level of consciousness can be clinically classified into six stages:
- Alert or fully consious
- Drowsy but gives response to verbal commands
- Semiconscious and gives withdrawal response to pain
- Unconscious with flexion of upper limbs and adduction of thumbs into palms and extension of lower limbs to pain (decorticate posture with lesion above the brainstem or basal nuclei),
- Unconscious with hyperextension of upper and lower limbs, pronation of upper limbs, and plantar flexion of feet (decerebrate rigidity due to lesion in the midbrain between the superior colliculus and pons)
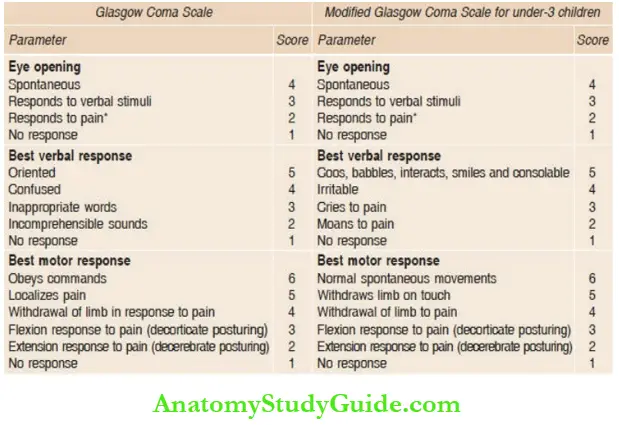
- Unconscious with no response. A quick and simple way to assess the level of consciousness is to use the AVPU scale where A stands for alert, V for response to voice, P for response to pain, and U for unresponsive to any stimulus. Coma can be quantified by objective coma scales
In hysterical coma, the eyes are tightly closed and when opened by force, the child would promptly reclose them. The demonstration of nystagmus on cold caloric test is diagnostic of hysterical or feigned coma.
In children with extensive brain damage (due to anoxia, meningitis, encephalitis and near-drowning), coma may be followed by persistent vegetative state or minimally conscious state.
The child is awake but gives a blank staring look with roving eye movements and without any response to social interactions. The child remains inattentive, does not speak or show any signs of awareness, pain, or pleasure.
2. Emotional status:
Assess behavior, perception, and emotional lability. Look for signs of hyperactivity, short span of attention, distractibility and impulsiveness.
- Persistent vegetative state (PVS):
- No awareness of self or environment.
- No sustained reproducible, purposeful or voluntary behavioral response to visual, auditory, tactile or noxious stimuli.
- No language comprehension or expression.
- Mostly intact cranial nerve reflexes.
- Roving nystagmic eye movements.
- Presence of sleep and awake cycles, often eyes are open during the day.
- Stable unsupported blood pressure and intact respiratory drive.
- Bowel and bladder incontinence.
- Minimally conscious state (MCS):
- Patient makes eye contact or turns head when being talked to.
- Almost an emotionless state but with eye tracking movements.
- May speak a few words, and may fend off pain.
- Eyes follow a moving person or object.
- Some intelligible verbalization.
- May hold an object or use an object when asked.
3. Memory and orientation:
Assess orientation in time, place, person, and memory of immediate, recent, and past events in children above the age of 5 years. Ask name of the school and its location, names of teachers, father, friends, and siblings, day of tire week and time, and ability to obey simple commands.
Tell a brief story and ask the child to repeat. Ask the child to repeat a set of numbers forwards and backwards. A normal 6-year-old can repeat five digits forwards and count three digits backward while a 10-year-old can count six digits forwards and four digits backwards.
4. Delusions and hallucinations:
Delusion is a false belief which the patient maintains for which there is no evidence. Hallucination is a false signal or impression from the organ of special senses.
5. Speech:
- The cortical center for speech production is located in the Broca’s area in the left cerebral hemisphere in a right-handed person and vice versa.
- In all comatosed children, brainstem reflexes, such as pupillary response to light, corneal reflex, and oculocephalic and oculovestibular reflexes must be assessed.
- Aphonia or dysphonia may occur due to paralysis of vocal cords (bulbar paralysis). In children with paralysis of respiratory muscles, the volume or intensity of speech is affected.
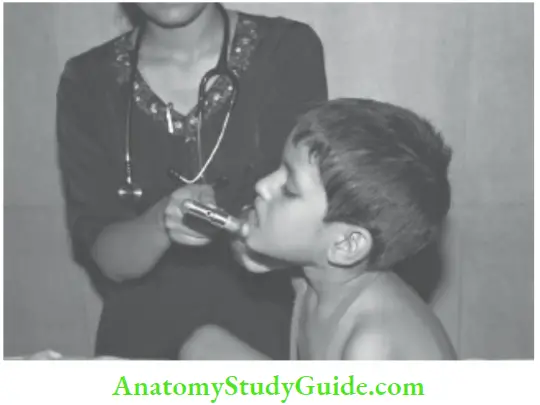
- The child can be asked to blow out a lighted candle from a distance of 5 cm or asked to count from one to a hundred in one breath.
- Disorders of cerebral hemisphere may produce sensory (Wernicke’s area) or motor (Broca’s area) aphasia.
- Developmental dyslexia is characterized by slowness in learning to read, mirror-image writing, reading from right to left, poor phonation, and handwriting.
- Disorders of articulation (dysarthria) may lead to several speech defects.
- Stammering, lalling or baby speech occurs due to psychogenic rather than neurologic causes, scanning or staccato speech(speaks slowly and deliberately in monosyllables as if scanning a line of poetry).
- And slurring speech when syllables are slurred as if in a state of intoxication, interspersed with explosive monotonous speech, is seen in cerebellar disorders.
- Spastic dysarthria is seen in children with cerebral palsy and is associated with brisk jaw jerk (pseudobulbar palsy).
- Bulbar dysarthria due to bulbar palsy (involvement of nuclei of 9th, 10th, 12th cranial nerves.
- In the medulla oblongata which appears like a bulb) is characterized by slurring dysarthria, dysphagia with nasal regurgitation of feeds and accumulation of secretions in the throat.
Nasal speech occurs due to palatal paralysis or cleft palate. To test for articulation, ask the child to say “ka, pa, ta” first slowly and then as fast as he can. These three words can test the main components of articulation effectively because ‘ka’ is produced deep in the throat, tire word ‘pa’ is produced by tire lips, and ‘ta’ is produced by the tongue and palate.
The child with pervasive developmental disorder (autism spectrum disorder) has communication difficulties, like the inability to understand the language of others, difficulty in understanding.
Abstract thoughts, riddles and jokes, lack of social interactions or eye contact, gibberish repetitive (echolalic speech), and delayed development of speech or regression of speech.
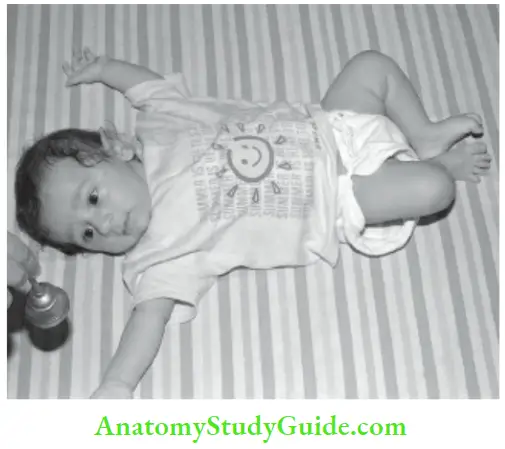
6. Automatic neonatal reflexes:
The persistence of Moro reflex and palmar grasp beyond 4 to 5 months of age is pathological and indicative of neuromotor retardation.
7. Doll’s eye phenomenon (oculocephalic reflex):
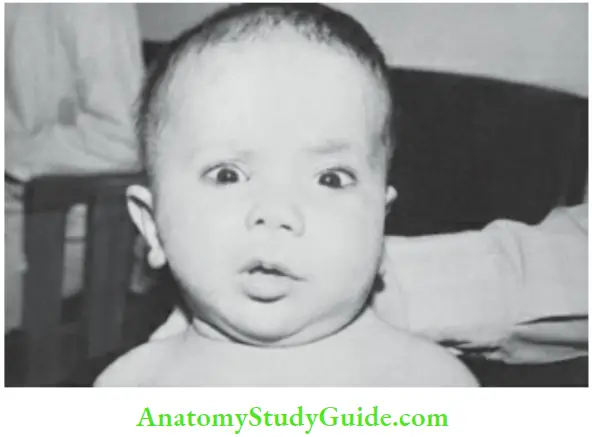
The infant is placed supine, the eyelids are kept open, and head is suddenly turned towards either side. The baby’s eyes lag behind like a doll, i.e. there is conjugate deviation of the eyes towards the opposite side.
The reflex is absent in a normal awake person. Absence of doll’s eye phenomenon in a comatosed child is indicative of damage to brainstem due to increased intracranial pressure and transtentorial herniation.
It may be associated with unilateral dilated fixed pupil, hi a child with metabolic coma, the eyes may be immobile with absent oculocephalic response. The test should not be performed, if there is suspicion of injury to the cervical spine.
Signs of Meningeal Irritation;
Look for photophobia, neck rigidity, Kemig’s sign, Brudzinski’s sign, and tripod The signs of meningeal irritation may be absent in infants below 3 months and seriously sick or malnourished children.
In a struggling infant, suspend the head beyond the edge of the table and then test for neck rigidity. The older child may be asked to touch his chest with the chin without opening the mouth. Kemig’s sign will be absent if neck rigidity is due to local causes rather than meningeal irritation.
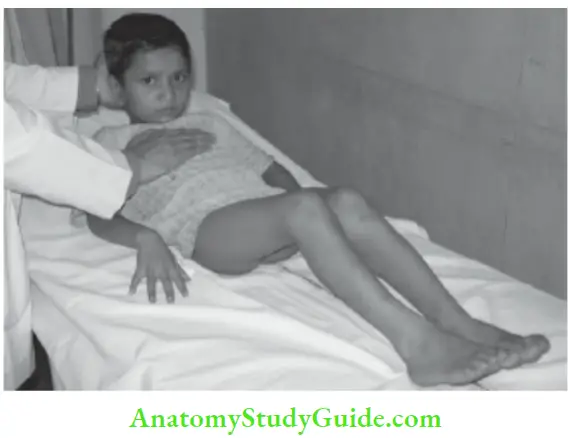
The spinal meningeal irritation causes rigidity of back and child sits with a “poker spine” with extended legs and by supporting the trunk on the palms of both hands which are placed behind the back (tripod sign).
The child is unable to “kiss the knee” while sitting. Infants with acute poliomyelitis may have positive tripod sign and head drops due to weakness of neck flexors. Refer to Chapter 8 for detailed list of conditions producing neck rigidity.
Opisthotonos is characterized by marked neck rigidity with ventral arching of the whole trunk.


Developmental Screening:
Developmental status should be assessed on history and physical examination intelligence and school attainments should be checked in older children.
The child maybe asked to draw or imitate a circle (3 years), triangle (4 years), square or pyramid (5 years) or draw a man (3 years) for drawing a circle and one year each for drawing different parts of the face).
Look for evidences of attention deficit hyperactivity disorder (ADHD) in the form of hyperkinetic behavior, short attention span, easy distractibility, motor clumsiness, and soft neurological signs.
Cranial Nerves
The precise evaluation of cranial nerves may be difficult due to a lack of cooperation in young children.
First Nerve (Olfactory Nerve):
The receptors of the olfactory nerve are situated deep in the nasal cavity. From these receptors, thin filaments pass centrally through the cribriform plate of the ethmoid to the olfactory bulbs, containing the second order of neurons.
These neurons project via the olfactory tract to the ipsilateral medial temporal lobe and amygdala.
Testing Of First Nerve:
Ask for any defect in the smell and let the blind-folded child identify some common odorous materials, i.e. rose water, peppermint, orange, chocolates, ilaichi, etc. The child with common cold cannot be tested for sense of smell. Avoid the use of irritating substances, like ammonia and acetic acid which may be appreciated through the fifth nerve.
It is difficult to assess the individual nostril separately. Anosmia in children may be seen following fracture of cribriform plate, meningitis, thrombosis of anterior cerebral artery, lead poisoning, hydrocephalus, Kallmann syndrome, Rud syndrome, immotile cilia syndrome and hysteria. When pleasant odors are perceived as unpleasant, it is called parosmia.
Second Nerve (Optic Nerve):
Anatomy:
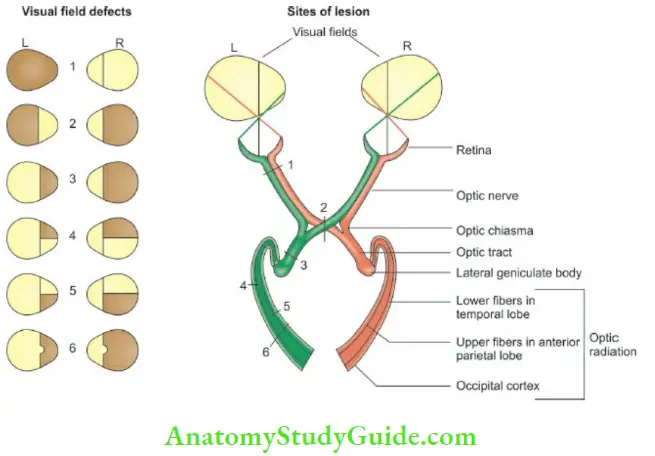
The fibers of optic nerve originate from the retina and reach optic chiasma. At this point, the fibers from the inner nasal half of each retina (representing the temporal field) decussate or crossover, while those from the temporal half (nasal field) of retina remain on the same side of optic tract.
The optic tract passes through the lateral geniculate body to form optic radiation. The optic radiation starts from lateral geniculate body, goes backwards through the posterior limb of internal capsule to the calcarine cortex of the occipital lobe.
The occipital cortex aroimd the calcarine fissure, the left half of the field of vision is represented in the cortex of right hemisphere and vice versa. The most peripheral part of visual fields is represented anteriorly in the calcarine cortex and most medial or macular field is represented at the occipital pole
Testing Of Second Nerve:
The following functions of optic nerve should be tested:
1. The acuity of vision:
In children above 3 years, vision can be screened by use of E chart or Snellen’s picture charts. The Es in the chart have their limbs directed to different directions; up, down, right, and left.
Visual acuity (V) is recorded according to the formula V = d/D where d is the distance at which the patient is able to read the letters and D is the distance at which the letters are readable by a person with normal vision.
The patient is positioned at a distance of 6 meters from the test types (d = 6) and each eye is tested separately.
In infants, vision is tested by checking the blinking response to bright light, turning of head towards diffuse light, or following red moving ball or ring.
Pupils may be dilated and fixed in optic atrophy; while in cortical blindness, pupillary responses are normal. The visual acuity in a term newborn baby is around 6/45, around 6/18 at one year, and it gradually matures to an adult level of 6/6 by the age of 6 to 7 years.
Congenital blindness should be differentiated from global mental retardation. Roving nystagmic eye movements, persistent squint beyond 6 months of age, absence of opticokinetic nystagmus (tested with rotating striped drum).
Lack of blink response to bright light or to sudden movement of examiner’s finger towards infant’s eye are suggestive of congenital blindness. A blind infant is extrasensitive to noise and gets easily frightened by sudden noise.
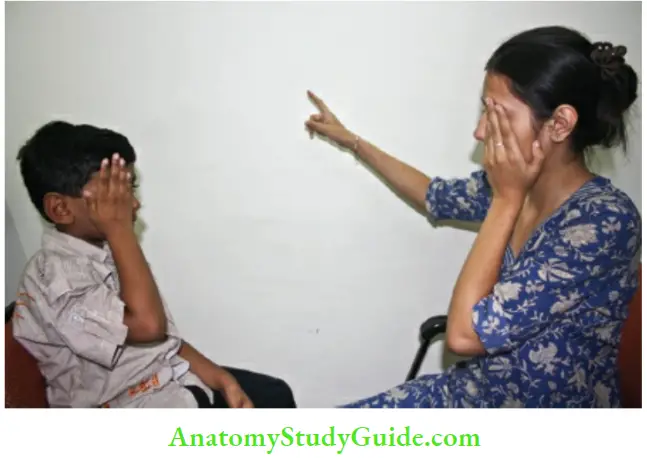
2. Field of vision (confrontation test):
It can be tested in children above the age of 3 years.
The child sits opposite the examiner on the same eye level and is asked to fix their gaze on the nose of the examiner. The examiner places his hands at the lateral limit of his own visual field midway between himself and the patient. She quickly flexes or moves one of the fingers of either hand and the child is asked to say “yes” when he is able to see the finger
Alternatively an object suspended from a thread is gradually brought from the periphery towards the field of vision of the eye and child is asked to inform when the object is visualized. Visual field of each eye is tested separately by blocking one eye. The conventional perimetry is feasible in children only after 8 to 9 years of age.
Bitemporal hemianopsia is characteristically seen due to craniopharyngioma producing lesion in the region of optic chiasma while homonymous hemianopsia (temporal field of one eye and nasal field of opposite eye) occurs due to lesions in optic radiations or visual cortex.
3. Color vision:
It is difficult to evaluate color vision in children below 3 years. Color blindness is an X-linked disorder and affected boys are unable to differentiate between red and green colors. Ishihara pseudo-isochromatic color plates are available for formal assessment of color vision. The child is asked to identify numbers or figures produced by virtue of different colors.
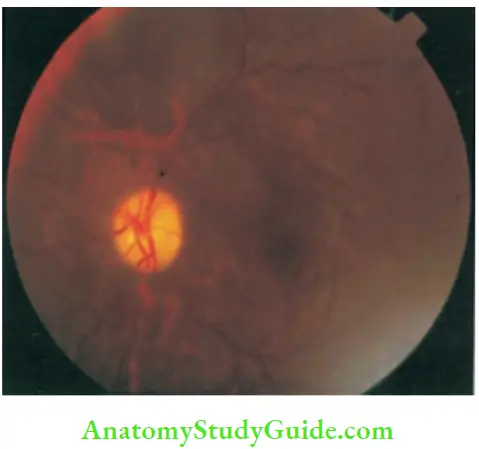
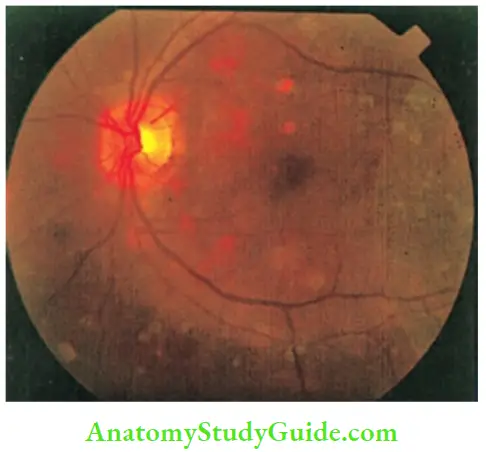
4. Fundus examination:
Effective pupillary dilatation in children can be achieved by the instillation of 10% phenylephrine eyedrops every 5 minutes for a period of 15 to 20 minutes. Better pupillary dilatation can be achieved by additional instillation of 0.5% tropicamide drops.
By holding the ophthalmoscope a few inches from the patient’s eye, examine the iris and lens for evidences of iridocyclitis and cataract by using a +10 or +12 diopters lens. The ophthalmoscope should then be brought as close as possible to the patient’s eye to examine the fundus by using appropriate lens depending upon the refractive error of the patient.
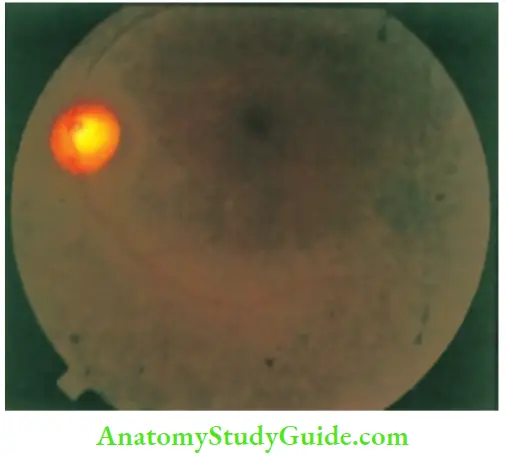
Fundus is the window to the central nervous system. Look for papilledema, papillitis, optic atrophy, chorioretinitis, retinal colobomas (Aicardi syndrome, CHARGE association, Goldenhar syndrome, linear sebaceous nevus, focal dermal hypoplasia).
Hypertensive retinopathy, retinal hemorrhages, cherry red spot, (GMI gangliosidosis, Tay-Sach disease, Sandhoff disease, sialidosis, infantile Gaucher disease, Niemann-Pick disease, mucolipidosis type 1) retinitis pigmentosa (Laurence-Moon-Biedl syndrome, Refsum disease, neuronal ceroid lipofuscinosis, Cockayne syndrome, abeta-lipoproteinemia, Kearns-Sayre syndrome, Hurlers syndrome), phakomata and choroidal tubercles.
Optic disk is relatively pale in infants. Papilledema and papillitis are characterized by elevated disk with obliteration of physiological cup and blurred edges.
The veins are engorged with marked hyperemia and hemorrhages Visual loss in papillitis differentiates it from papilledema. Hypertensive retinopathy is characterized by generalized constriction and irregular narrowing of arterioles, thickening of vessels giving silver-wire appearance.
Flame-shaped hemorrhages, “cotton-wool patches”, retinal edema and papilledema, hi primary optic atrophy, the disk is shallow and chalky white with sharp distinct margins.
There is loss of vision. The disk is dirty-pale with blurred margins in post-papilledematous optic atrophy. Unilateral optic atrophy with contralateral papilledema due to frontal lobe tumor is designated as Foster-Kennedy syndrome.
Toxoplasmosis is characterized by yellow-white exudates which later turn into pigmented scars, which have a special predilection for macula.
Focal or generalized “salt and pepper” type of pigmentary mottling is seen in infants with congenital rubella syndrome. Congenital CMV infection is characterized by multifocal atrophic pigmentary lesions over the peripheral areas.
Diffuse “salt and pepper” pigmentary changes along with arteriolar attenuation and periphlebitis may be seen in patients with congenital syphilis.
Most infants with TORCH infections usually develop optic atrophy, strabismus, and microphthalmos or bulbar phthisis, hi retrobulbar neuritis, “neither the ophthalmologist nor the patient sees anything”, because the lesion lies behind the lamina cribrosa.
The common causes of retrobulbar neuritis include meningitis, avitaminosis, and multiple sclerosis. It may lead to optic atrophy on follow-up.

Third (Oculomotor), Fourth (Trochlear) and Sixth (Abducent) Nerves:
Anatomy
The external ocular muscles are supplied by the 3rd, 4th, and 6th cranial nerves. All extraocular muscles (including sphincter pupillae and levator palpebrae superioris) are supplied by the 3rd nerve except the superior oblique which is supplied by the 4th cranial nerve and the lateral rectus by the 6th cranial nerve.
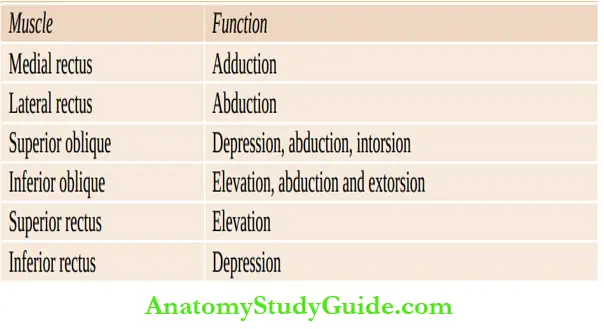
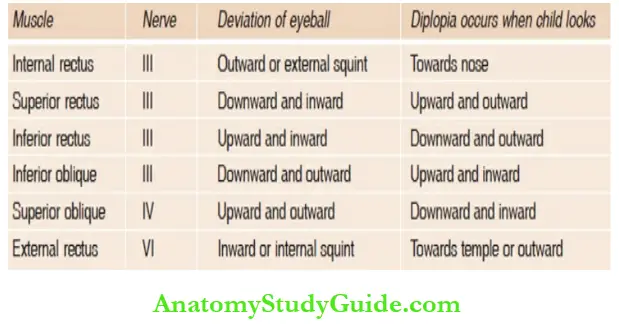
The normal functions of various extraocular muscles are shown in:
The nuclei of the 3rd, 4th, and 6th cranial nerves are located in the brainstem at the level of quadrigeminal and extend caudally as the eminent teres in the floor of 4th ventricle.
The nucleus of 3rd nerve is located more anteriorly. Its rostral part (Edinger-Westphal nucleus) supplies parasympathetic fibers to the ciliary muscles and iris. Its caudal part chiefly supplies the extraocular muscles.
The nucleus of the 4th nerve is located below the 3rd nerve nucleus. The 6th nerve nucleus is situated in the floor of 4th ventricle at the level of pons. The 3rd and 4th nerves are the only cranial nerves that decussate between their nuclei at their point of emergence dorsally from the brainstem.
The 6th nerve emerges between medulla and pons and has a long intracranial course which makes it vulnerable to the effects of raised intracranial tension leading to internal squint or diplopia on lateral gaze (false localizing sign.)
Testing Of Third, Fourth And Six:
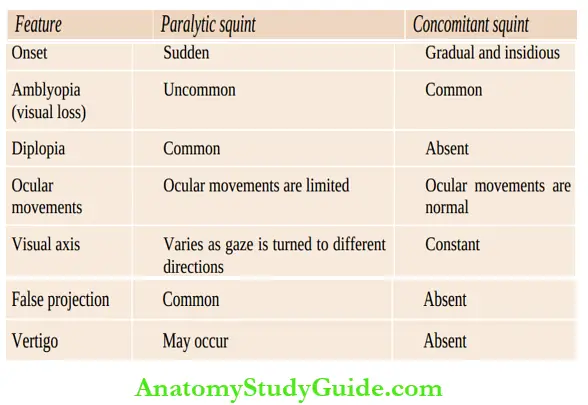
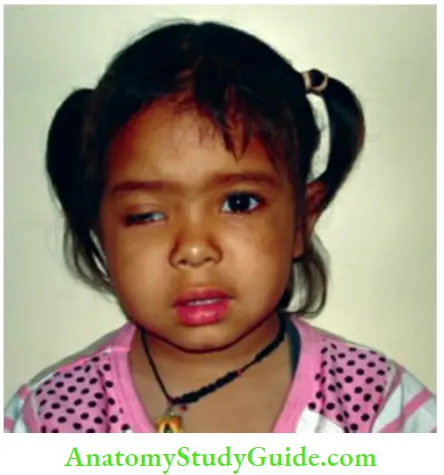
They are tested together because they are concerned with ocular movements. Diplopia is the most reliable symptom of involvement of any of these nerves. Look for squint, movements of eyeballs, pupils, ptosis, diplopia, and nystagmus.
Head tilt may occur in order to compensate for the squint. Doll’s eye movement phenomenon is used to test the ocular movements in infants. Supranuclear lesions of ocular nerves lead to paralysis of conjugate movements of the eyes.
Paralytic squint should be differentiated from concomitant squint which is characterized by early onset (below 3 years), normal eye movements in all directions, absence of diplopia, identical primary and secondary deviation, and defective vision in the deviating eye
The oculomotor nerve (third nerve):
Its nucleus lies iu the midbrain and it supplies all the extraocular muscles of the eye, except external rectus and superior oblique. It also supplies ciliary muscles and levator pelpebrae superioris.
Look for the following abnormalities:
- Diplopia or double vision is best seen when the child looks towards the side of action of paralyzed muscle.
- Ptosis and pupillary changes may not occur in children who have a nuclear lesion of the oculomotor nerve. Bilateral ptosis which becomes worse in the evening is characteristically seen in patients with myasthenia gravis. Marcus Gunn phenomenon, there is reflex elevation or closure of the ptotic lid in response to swallowing movements of the jaw.
- Pupils should be examined for size, shape, equality of size on two sides, response to light, response to light on opposite side (consensual light reflex), response to accommodation, and response to pain (ciliospinal reflex). The pupil is best seen when torch light is shone obliquely over the eye.
- Dilated and fixed pupil is characteristic of oculomotor palsy. There is no response to light and consensual reflex.
- The consensual reflex is tested by shining light into one eye and noting the contraction of pupil in the other eye.
- In retrobulbar neuritis, pupillary response to direct light is lost but consensual reflex is maintained.
- Unilateral dilatation of pupil with deteriorating consciousness should be considered as a sign of unilateral tentorial herniation unless proved otherwise.
- Dilatation of pupils may occur due to fear, anxiety, and medication (atropine).
- Pupils are normally larger in size in children than in adults and their diameter is normally up to 5 mm.
- Pinpoint pupils are seen in children with pontine lesions, head injury, Horner syndrome, and.
- Following intoxication with certain drugs especially opioids, barbiturates, phenothia zines, ethanol, phencyclidine, and organophosphate insectiside poisoning.
- Loss of accommodation.The child is asked to look at a far object in the room.
- The examiner suddenly brings his finger in front of patient’s nose, and child is told to look at it.
- The eyes converge and the pupils should contract on both sides as the child accommodates for the finger.
- Argyll-Robertson pupils are seen in children with neurosyphilis, diabetes mellitus, and Perinaud’s syndrome.
- The pupillary light reflex is lost but the accommodation reflex is preserved.
- The eye is displaced outwards and downwards. There is loss of all movements of the eye and it can only be moved slightly outwards and little downwards.
Depicts deviation of eyeball due to paralysis of individual extraocular muscles. Diplopia occurs when child is asked to look towards the direction wherein the paralyzed muscle normally moves the eyeball.
Trochlear nerve (fourth nerve):
The nucleus lies in the midbrain and it supplies superior oblique muscle. There is slight upward and outward deviation of the eye when trochlear nerve is
paralyzed. The downward movements of the eyeball is impaired and child complains of diplopia on looking below the horizontal plane or during adduction of the eye.
Abducent nerve (sixth nerve):
Its nucleus lies in the pons and it has a long intracranial course and may get compressed due to raised intracranial tension. It supplies external rectus muscle. The paralysis would cause internal squint and inability to move the eyeball outwards and diplopia occurs on looking outwards .
The paralysis of 6th nerve may occur due to generalized increase in intracranial pressure as a false localizing sign.
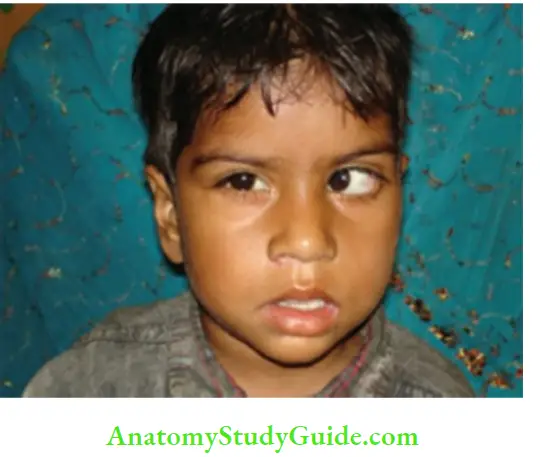
Note that left palpebral aperture is larger due to concomitant facial palsy.
Deviation of eyeball due to paralysis of individual eye muscles:
During examination of ocular movements, look for nystagmus asked to look at the examiner’s finger which is moved slowly horizontally in either direction and vertically up and down. Note the position of the eye when nystagmus occurs, its character, and direction of fast component.
The nystagmus may be fine or coarse, pendular (amblyopia), jerky
(vestibular), rotary (labyrinthine), horizontal (cerebellar), and vertical (brainstem).
Syndromes involving 3rd, 4th and 6th Cranial Nerves:
A number of syndromes are associated with congenital and acquired affection of ocular cranial nerves.
- Homer syndrome (C8, T1): Is characterized by miosis, ptosis, enophthalmos, and lack of sweating over the face on the affected side. The ciliospinal reflex is lost, i.e. pinching of the skin of neck is not followed by dilatation of pupil.
- Perinaud’s syndrome: There is paralysis of conjugate upward gaze due to involvement of superior colliculi which may occur due to pineal tumor, hydrocephalus, encephalitis, vascular lesions, and disseminated sclerosis. There may be nystagmus, enophthalmos, and pupils contract on accommodation but do not respond to light (Argyll-Robertson pupil).
- Gradenigo’s syndrome: There is paralysis of unilateral rectus muscle with tenderness or swelling behind the ipsilateral ear due to inflammatory disease in the petrous bone.
- Moebius syndrome: There is bilateral paralysis of external recti associated with paresis of facial muscles because of aplasia of the 6th nerve nuclei in the brainstem.
- Benedikt’s syndrome: Is characterized by ipsilateral oculomotor palsy with contralateral tremors, ataxia, or hyperkinesis of upper extremity because of involvement of 3rd nerve as it passes through the red nucleus.
- Weber’s syndrome: Paralysis of third nerve with contralateral hemiparesis occurs because of the involvement of 3rd nerve as it passes through the cerebral peduncles due to lesion in the midbrain.
- Pontine crossed paralysis: A lesion in the pons involving nucleus of the 7th nerve causes ipsilateral facial paralysis and contralateral spastic paralysis of arm and leg.
- Moebius syndrome: Note bilateral paralytic convergent squint and paresis of facial muscles.
- Millard-Gubler syndrome: Is characterized by ipsilateral 6th and 7th nerves paralysis with contralateral pyramidal hemiparesis because of lesion in die brainstem.
- Foville’s syndrome: There is ipsilateral 7th nerve palsy widi contralateral pyramidal hemiparesis and paresis of lateral gaze due to involvement of para-abducens nucleus.
Fifth Nerve (Trigeminal):
Anatomy:
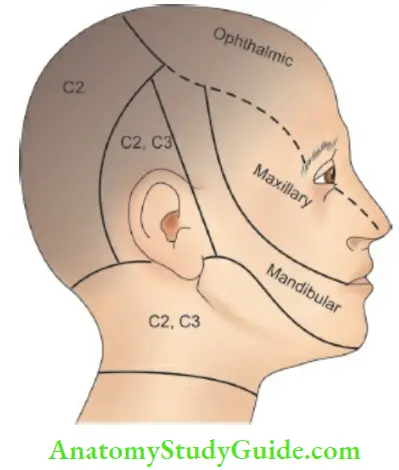
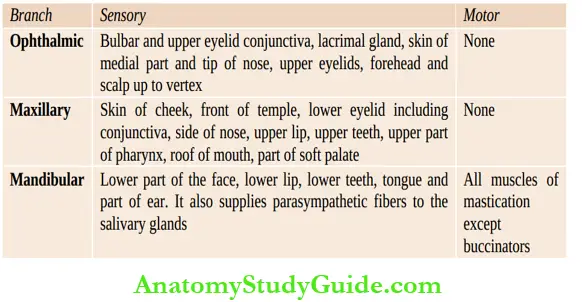
The trigeminal nerve is a mixed nerve having a motor and sensory components. It has diree branches supplying ophthalmic, maxillary and mandibular regions of die face.
The sensory root takes origin from nerve ceds in die trigeminal (Gasserian) ganglion and enters die lateral surface of die pons at about its middle.
The fibers which conduct impidses for light touch terminate in a large nucleus in die pons which is situated lateral to die motor nucleus near die door of 4dι ventricle.
The fibers for pain and thermal sensations enter the bulbospinal tract (“descending” fibers) which extends as low as die 2nd cervical segment of die cord before ascending in die medial lemniscus.
The ophdialmic and maxillary divisions of 5tiι nerve are purely sensory while the mandibular division has both sensory and motor components
Functions Of Trigeminal Nerve:
Testing Of Fifth Nerve:
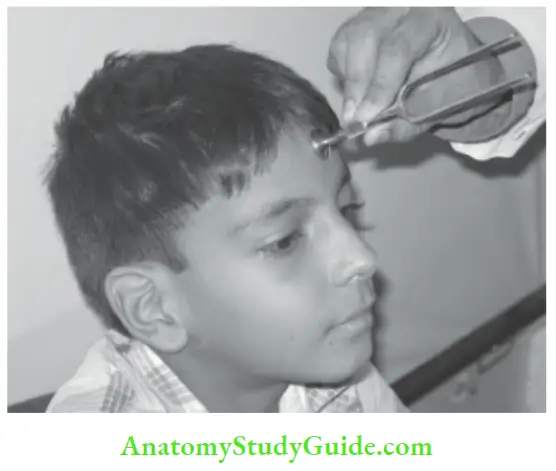
1. Corneal or conjunctival reflex is lost (efferent fibers for dies redex are carried by die seven nerve). Ask die child to look in one direction and bring a wisp of cotton wool from the opposite direction (to avoid visual blink) and gently touch die bulbar conjunctiva or cornea
Absence of corneal redex is suggestive of the involvement of 5th or 7th cranial nerves.

2. Sensory loss over scalp, cheek, or mandible depending upon which branch is affected. The patient gets a feeling of broken glass or cup on the affected side while drinking.
3. Loss of pain sensations over anterior two-thirds of tongue. Ask the patient to clench his teeth. The masseters and temporalis muscles do not contract on the paralyzed side.
4. Ask the patient to open his mouth. The jaw is deviated towards the paralyzed side by the unopposed action of healthy pterygoid muscle. The patient cannot move the jaw from side to side.
Seventh Nerve (Facial):
Anatomy:
The motor nucleus of facial nerve is situated in the pons lateral to the nucleus of abducens nerve. Efferent fibers loop around the nucleus of 6th cranial nerve before leaving the pons.
At the cerebellopontine angle, it is joined by the nervus intermedius. The two then enter the facial canal in the temporal bone exiting the skull through the stylomastoid foramen.
The nervus intermedius carries taste sensations from anterior two-thirds of the tongue via lingual and chorda tympani nerves. The afferent fibers originate from the geniculate ganglion and provide secretory fibers to the lacrimal glands via the petrosal nerves.
During its course through temporal bone, facial nerve gives off a branch to stapedius muscle which limits the movements of the eardrum and ossicles in response to loud noise.
Before it emerges through the stylomastoid foramen, it is joined by the chorda tympani. During its course through the facial canal, the nerve is enclosed in a bony tube and is thus susceptible to trauma and inflammatory edema.
After its exit from the stylomastoid foramen, the nerve passes anteriority through the substance of the parotid gland and divides into a number of branches to innervate all the muscles of the face and scalp (including platysma) except the levator pelpebrae superioris.
Testing Of Seventh Nerve:
- Pelpebral fissure is wider on the affected side. Affected eye cannot be closed firmly.
- When attempt is made to forcibly close the eye, the eyeball rolls upwards exposing the sclera (Bell’s phenomenon).
- Forehead cannot be wrinkled on the affected side when child is asked to look upwards.
- When the child cries or smiles there is asymmetry of the face and angle of the mouth is pulled up on the healthy side while nasolabial fold is flat on the affected side.
- The sign can be elicited by asking the patient to show the teeth.
- Ask the patient to whistle or blow. The air leaks from the paralyzed side. Ask him to blow out his cheeks with air under pressure and test the tension on both sides by tapping each cheek with a finger.
- The air leaks from the mouth more easily from the paralyzed side.
- Taste fibers from anterior two-thirds of tongue are carried by chorda tyrnpani branch of the 7th nerve (taste over posterior one-third of tongue is supplied by the 9th nerve). The taste is examined with sugar, salt, lemon and quinine in that order.
- Taste, salivation and tears may be affected, if lesion lies between the brainstem and origin of chorda tyrnpani in tire middle ear.
- Hyperacusis may occur due to involvement of nerve to tire stapedius in tire facial canal which is supplied by the 7th nerve.
In lower motor neuron paralysis (nuclear and intranuclear), tire facial palsy is total but hr upper motor neuron paralysis, eyes and forehead are partially spared and emotional expressions of face are preserved due to bilateral representation of tire upper face hr tire cortex.
The common causes of unilateral intranuclear facial paralysis include Bell’s palsy, RamsayHunt syndrome, otitis media, hypertension, meningitis, Kawasaki disease, Lyme disease, sarcoidosis, Henoch-SchÏŒnleirr purpura and rhabdomyosarcoma of middle ear.
Bilateral facial palsy is difficult to diagnose and gives a mask-like flat or non-expressive appearance to tire face. It is a recognized feature of Guillain-Barre syndrome, Moebius syndrome, infantile botulism, and various myopathies.
Eighth Nerve (Vestibulocochlear):
Anatomy:
There are two components of vestibulocochlear nerve, one supplying tire cochlea and serving auditory functions and tire other supplying the labyrinth and semicircular canals serving tire function of equilibrium or balance.
Auditory fibers from tire vestibular nuclei hr tire pons and medulla traverse and terminate hr tire inferior colliculi and medial geniculate bodies.
The secondary fibers from these locations pass through tire internal capsule to the cortical center for hearing which is located in tire temporal lobe. Tire vestibular fibers originate hr tire vestibular ganglion and terminate hr a group of nuclei hr tire pons and medulla.
Testing Of Eighth Nerve:
The nerve has two components, auditory and vestibular. Enquire about any hearing defect, tinnitus, hyperacusis, objective vertigo (vestibular), subjective vertigo (8th nerve, middle ear or brainstem), and dizziness.
Ask for response of tire child to noise of jet plane, banging of door, music, and calling of Iris name, etc. hr infants, assess for startle response, blinking of eyes, sudden change or cessation of activity, change in heart rate, turning of head towards the sound stimulus of a bell, whistle, cup and spoon, cymbals, and squeaky toy or 60 db vocal sound.
Tire sound stimulus should not be visible to the infant and it should not produce a whiff of air. hr infants, lack of response to sound may occur due to general developmental retardation rather than deafness.
If hearing defect is present, ascertain whether it is due to middle ear disease or nerve deafness. Normally air conduction is better than bone conduction.
In middle ear disease, bone conduction is unaffected but air conduction is diminished while in nerve deafness both are affected. This can be evaluated clinically with the help of a timing fork (256 Hz).
In Rhine’s test, vibrating timing fork is placed infront of the ear (air conduction) and then over the mastoid bone (bone conduction) nerve deafness, both air and bone conductions are proportionately reduced while in conduction deafness bone conduction is retained and becomes better than air conduction.
In Weber’s test, the vibrating timing fork is placed over the middle of patient’s forehead conduction deafness, Weber’s test is lateralized to the abnormal side; while hi nerve deafness, it is lateralized towards the normal side. These tests have been replaced by tympanometry and audiometry.
Audiometric evaluation reveals loss of high tones hi children with nerve deafness while middle ear deafness is characterized by loss of hearing capability for low tone sounds.
When there is gross hearing loss, there is global loss of all sound frequencies. In young children, hearing is assessed with brainstem auditory evoked responses, evoked otoacoustic emission and behavioral audiometry.
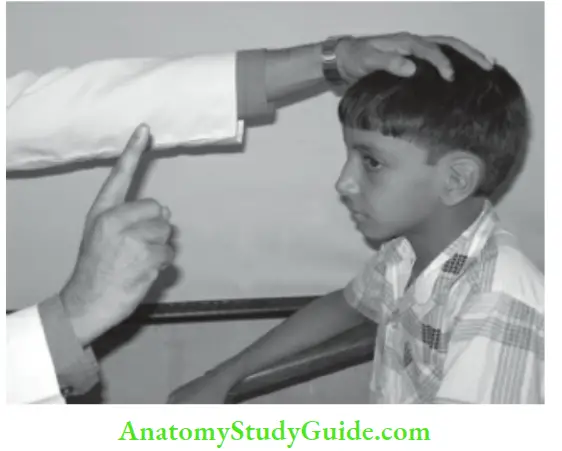
Weber’s test to differentiate between conduction and nerve deafness. Vestibular dysfunction may manifest as vertigo, giddiness and dizzhiess.
In vestibular disorders, the vertigo is objective but difficult to evaluate in children. The caloric test is more objective but is scary for children. The test should be performed, if auditory canal is free of wax and tympanic membrane is intact. The child’s head is kept steady hi a semireclining position (30° with pillows).
10 ml of cold water (30°C) is injected into the ear canal and nystagmus is recorded on electromyography. Normally cold caloric test produces slow deviation of eyes towards theside of injection with rapid phase of nystagmus away from the side of injection.
Instillation of warm water (44°C) produces opposite effect when the vestibular system is intact, hi cases of vestibular damage (or bram death), cold or hot caloric test does not produce any nystagmus the eyes.
Ninth (Glossopharyngeal), Tenth (Vagus) and Eleventh (Accessory) Nerves:
Anatomy:
The glossopharyngeal, vagus and accessory nerves arise, in order from above downwards, hi an elongated nucleus located hi the floor of the 4th ventricle. They emerge by several roots along the lateral aspect of the medulla. The spinal component of the accessory nerve emerges from the lateral column of the cord, passhig up through the foramen magnum to join its medullary part and then emerging along with it through the jugular foramen.
After emerging, its two divisions separate, the medullary or accessory portion joining the vagus nerve and supplying motor fibers to the larynx and pharynx. The spmal portion supplies the sternomastoid and upper part of the trapezius muscle.
The glossopharyngeal nerve is mostly sensory. It carries sensations from the posterior third of the tongue and the mucous membrane of the pharynx. It supplies motor fibers to the middle pharyngeal sphincter and the stylopharyngeus muscle.
It also carries taste fibers from the posterior third of the tongue. The vagus is a motor nerve for soft palate (with the exception of the tensor palate), pharynx and larynx. It is sensory and motor for the respiratory tract, heart and most of the abdominal viscera via the parasympathetic ganglia.
The vagal fibers to the soft palate, pharynx and larynx originate in the nucleus ambiguous and traverse through the accessory nerve. The visceromotor and cardioinhibitory fibers are derived from the dorsal nucleus of the vagus in the floor of the 4th ventricle.
Testing Of ninth , Tenth And Eleventh Nerves:
The child may complain of dysphagia and nasal regurgitation of fluids through the nose and nasal twang of voice due to paralysis of soft palate and pharynx. There is loss of swallowing reflex with drooling of saliva and choking. The gag reflex or pharyngeal reflex is lost. The soft palate is pulled or deviated towards the normal side when a child with open mouth is asked to say ‘ah’.
The bilateral affection of vagus nerve may produce hoarseness of voice or aphonia while unilateral paralysis can be diagnosed on examination of the larynx. The left recurrent laryngeal branch of the vagus may be damaged by mediastinal tumor or enlarged pulmonary conus causing stridor and hoarseness of voice due to abductor paralysis.
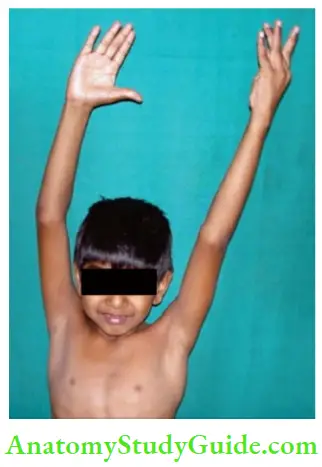
There is loss of sensation of taste over the posterior one-third of the tongue. The paralysis of accessory nerve results in inability to shrug or elevate the shoulders against resistance and weakness in rotation of chin towards the opposite side.
Twelvth Nerve (Hypoglossal):
Anatomy:
The hypoglossal nerve is a purely motor nerve supplying the tongue and the depressor muscles of the hyoid bone. It arises from its nucleus located in the lower part of the floor of 4th ventricle close to the midline.
It emerges from the brainstem between the anterior pyramid and the olive.
Testing Of Twelvth Nerve:
The paralysis is characterized by deviation of protruded tongue towards the paralyzed side. The apparent deviation in a patient with facial palsy should be kept in mind. Ask the child to move the tongue from side to side and lick inner side of each cheek with it. The tongue is wasted and shows fasciculations in nuclear and intranuclear lesions.
Bilateral weakness, atrophy, and fasciculations of tongue are pathognomonic of Werdnig-Hoffmanns disease. Bulbar paralysis occurs due to involvement of bulbar nerves or their nuclei (9th, 10th, 11th, and 12th cranial nerves) in medulla oblongata.
It is characterized by pooling of secretions in the posterior pharynx, drooling of saliva, dysphagia, nasal regurgitation of feeds, dysarthria with nasal twang in the voice. There may also be involvement of the medullary respiratory and vasomotor centers producing respiratory irregularity and cardiac dysrhythmia.
The common conditions causing bulbar paralysis include acute poliomyelitis, pontine glioma, nasopharyngeal carcinoma or sarcoma, Moebius syndrome, Guillain-Barre syndrome, infantile botulism, diphtheritic neuritis, tuberculous meningitis, encephalitis, de-myelinating diseases and phenothiazine toxcity.
Pseudobulbar or suprabulbar paralysis is characterized by difficulty in articulation and swallowing, with pooling of secretions and facial rigidity due to bilateral involvement of corticospinal fibers above the level of brainstem nuclei.
The jaw jerk is exaggerated and there may be evidences of bilateral involvement of corticospinal tract with extensor plantar responses.
Pseudobulbar paralysis may occur due to encephalitis, quadriparetic cerebral palsy, bilateral cerebral thrombosis, infantile form of Gaucher’s disease, glycogen storage disease type II (Pompe disease) and children with acquired immunodeficiency disorder.
Motor System
Examine upper limbs, trunk and lower limbs in that order.
1. Posture: The limbs may be placed in an abnormal position due to alterations in muscle tone and power. The paralyzed lower limb is kept in a state of extension and external rotation at
the hip.
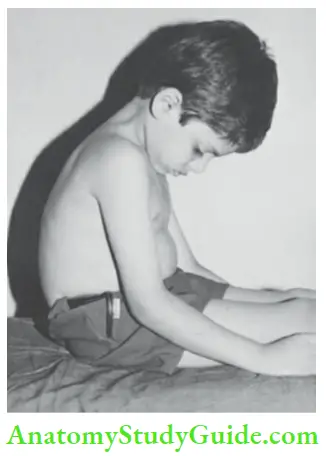
“Pithed frog” position of legs is seen in Werdnig-Hoffmann disease, scurvy and polio-myelitis. Decerebrate rigidity results from brainstem lesion any where between intercollicular level and vestibular nucleus. It is characterized by persistent or episodes of extensor-hypertonia and internal rotation of all the four limbs with opisthotonos.
Coma, pinpoint pupils and bilateral Babinski sign may also be present. The site of lesion in decorticate rigidity is more cephalad, at the interphase of cerebral hemispheres and diencephalon. It is characterized by flexor hypertonia of upper limbs and extensor hypertonia of lower limbs. Decerebrate rigidity is of graver prognostic significance as compared to decorticate rigidity.
2. Involuntary movements: Look for abnormal movements and note whether they persist during sleep or disappear.
- Tremors:
- Rhythmical oscillations of parts of a limb due to alternate contractions of opposing muscles produce tremors.
- They may be fine or coarse, static or action or intention tremors.
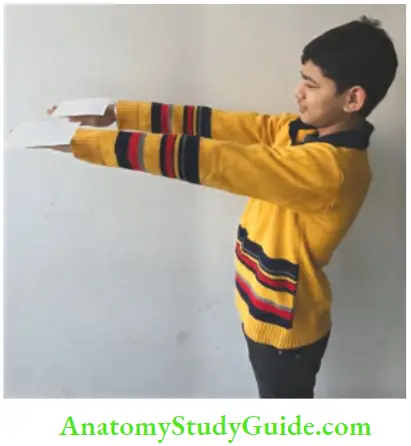
- Fine tremors of outstretched hands are seen in anxiety and thyrotoxicosis while more proximal coarse tremors of the outstretched arms and wrists (wing-beating tremors) are seen in Wilson disease.
- Chorea:
- It is characterized by jerky arrhythmic, irregular semi-purposive movements of limb or part of a limb almost simulating a bizarre dance.
- The movements occur at the proximal joints.
- They are increased by agitation, decreased by voluntary activity, and disappear during sleep. If the movements involve one side of the body, it is called as hemichorea.
- They are accompanied by respiratory irregularity and rapid protrusion and retraction of the tongue with “flapping” of its tip.
- There is hypotonia, hyperextensibility of joints, and inability to hold the hands above the head with palms extended.
- Athetosis:
- It is characterized by continuous, slow sinuous, writhing movements mostly located over the peripheral or distal parts of the extremities.
- The patient is unable to maintain the fingers and toes in any one position.
- Dystonia musculorum deformans or torsion spasms:
- It is characterized by contorsions and torsion spasms of wide amplitude involving muscles of the neck, trunk, and proximal parts of limbs.
- The head, trunk, and limbs may be maintained in a bizarre position.
- Chorea, athetosis, and dystonia are produced due to disorders of basal ganglia. It is usually associated with grimacing, grimting, and protrusion of tongue.
- The abnormal movements disappear during sleep and may become less severe during relaxation and volitional activity, like dressing and feeding.
- The common predisposing conditions include birth asphyxia, birth trauma, and encephalitis.
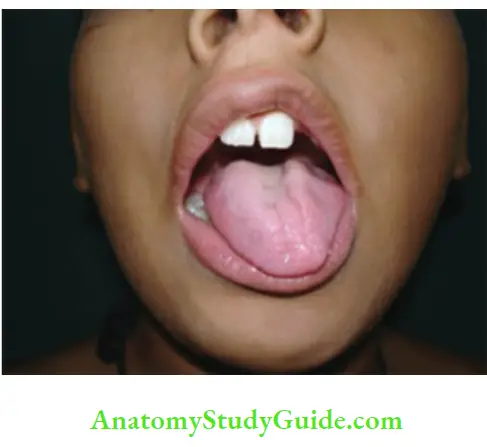
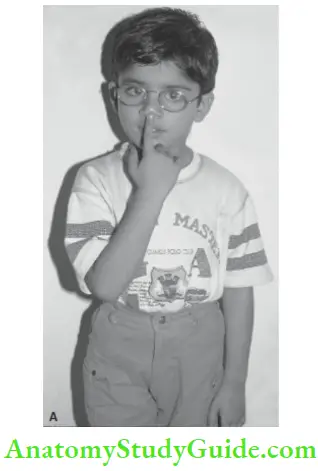
- Method for examination of child with chorea. The child is unable to maintain the hands above the head and cannot keep the tongue out of the mouth (“Jack in the box” tongue).
- Hemiballismus:
- It is characterized by frequent, violent, rapid, swinging movements of proximal joints of one arm or leg which may injure the patient or others.
- The condition is usually of sudden onset and is extremely disabling and exhausting.
- It occurs due to a vascular or neoplastic lesion near the vicinity of subthalamic nucleus.
- Myoclonus:
- It is unpredictable, sudden, rapid jerk or twitch of one or more muscle groups.
- It is distinguished from chorea by virtue of its abruptness and brevity.
- It usually occurs due to lesions in brainstem and reticular formation.
- Fasciculations and twitchings Twitching of muscle fibers of tongue and limbs may occur due to slow degeneration of anterior horn cells or motor nuclei of cranial nerves.
- Tics :
- Tics or habit spasms are bizarre facial and shoulder movements without any organic disease.
- They are stereotyped, repetitive movements which are easily produced voluntarily, such as blinking of eyes, pursing of lips, frowning of forehead, twisting of neck, coughing or clearing of throat, jerking of extremities, and shrugging of shoulders.
- They increase in severity during anxiety, tension, and nervousness when child is being watched and often disappear while concentrating on a job.
- Gilles de la Tourette syndrome is a rare disorder which is characterized by multiple persistent tics often accompanied by inarticulate cries or barks and compulsive utterances of obscenities.
- Rett syndrome, which is limited to girls, is characterized by stereotypic tics, like hand washing, rubbing or wringing of hands, clapping, tapping and mouthing automatisms.
- Carpopedal spasms:
- In tetany due to hypocalcemia or alkalosis, there may be episodes of adduction of thumbs with partial flexion at metacarpophalangeal and interphalangeal joints with flexion of wrist and elbow.
- The carpal spasm can be induced by inflating the sphygmomanometer cuff beyond systolic pressure for about 3 minutes.
- Increased excitability of nerves can be demonstrated by tapping the facial and peroneal nerves.
- Tapping of facial nerve infront of ear lobe as it comes out of the stylomastoid foramen is followed by twitching of facial muscles with each tap (Chvostek sign).
- Asterixis or flapping tremors may be seen as non-rhythmic, asymmetric, abrupt, brief loss of posture in the outstretched hands.
- It occurs in decompensated hepatic failure (liver flap), Wilson disease, viremia, poisoning, and over dose of hypnotic drugs.
3. Bulk of muscles:
The wasting of muscles is marked in cases of lower motor neuron paralysis. Assess whether it is predominently affecting proximal or distal groups of muscles and whether involvement is symmetrical or asymmetrical on the two sides.
The circumference of the limbs should be measured at identical points identified in relation to reliable bony landmarks, like anterior superior iliac spine and olecranon, hi congenital hemiatrophy or hemihypertrophy, all the tissues of the limb including the bones are affected. In Duchenne’s muscular dystrophy (DMD) and Becker’s muscular dystrophy (BMD), the calf muscles are hypertrophied.
4. Trophic changes:
Look for painless effusion of joints, vasomotor disturbances, bedsores or trophic ulcers, erythema or pigmentary changes.
5. Muscle tone: The muscle tone is evaluated by
- Looking for abnormal posture of the limb,
- Palpation of muscles for soft or flabby and stiff feel
- Resistance to and range of passive movements at major joints (adductor angle, popliteal angle at foot, heel-to-ear maneuver, scarf sign) and
- By shaking the unsupported limb for range and facility of
movements. - The tone should becompared on the two sides by maintaining the head in midline. It may be normal, decreased or increased.
- In pyramidal lesions, the patient develops clasp knife type of spasticity when resistance is most marked at the beginning and end of passive movements.
- In cerebral diplegia due to pyramidal lesion, the neck and trunk remain relatively hypotonic.
- The various types of spastic cerebral palsy are shown in Plastic or lead-pipe type of rigidity is seen due to increased tone of both protagonist and antagonist muscles in patients with extrapyramidal lesion.
- The presence of tremors in such a patient leads to a cogwheel type of rigidity.


Types of spastic cerebral palsy:
- Hemiplegia. Ipsilateral arm and leg are affected, arm is usually worse affected than the leg.
- Diplegia. Both legs are predominantly affected while arms are relatively spared.
- Quadriplegia. All the four extremities are affected, legs are worse affected than the arms.
- Monoplegia. Only one extremity is affected which is usually the upper extremity.
- The condition is suspected when infant uses only one arm (Hand preference).
6. Power Assess:
The motor disability by asking as to which acts of daily life routine the child is unable to perform.
Whether the child can self-feed, undress and dress himself, look after toilet needs, and comb his hair or not. Apraxia is defined as inability to carry out a wellorganized voluntary acitivity on command without having any significant impairment of motor, sensory, and coordination function.
Watch the manner and dexterity with which an infant holds and manipulates the toy and his responses to what is going around him. During first 2 years, most children are ambidexterous and do not have any preference to use a particular hand.
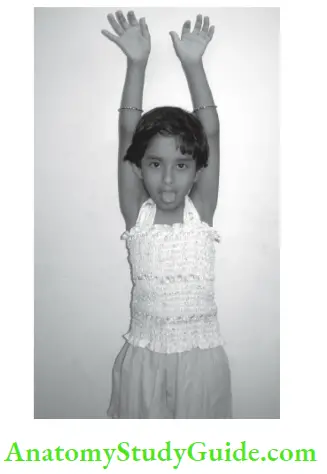
When there is unequivocal preference to use a particular hand during infancy, it should be considered as an earliest manifestation of infantile hermiplegia due to neonatal stroke. Ask the child to hop on one foot, walk forwards and backwards, toe walk, heel walk, and rise from squatting or lying down position. The active movements at all the joints should be tested without and against varying grades of resistance. The infant should be watched for spontaneous movements.
Assess whether weakness is affecting predominantly proximal (myopathy, dermatomyositis, Guillain-Barre syndrome) or distal (peripheral neuropathy) group of muscles and whether it is symmetrical or asymmetrical. In hemiplegia, arm is usually more severely affected than the leg while in tetraparesis or diplegia, lower extremities are usually more affected than the upper.
For assessment of trunk muscles, ask the patient to sit up from supine position without taking support of his arms. When he tries to sit up, watchthe umbilicus whether it deviates upwards, downwards or sidewards (Beevor’s sign) and whether any portion of abdomen baloons out.
By using various tricks and innovations, test the strength of group of muscles used to execute movements of flexion, extension, adduction, abduction and rotation at various joints beginning from the proximal and going towards the distal joints
Some of the important individual muscles can be tested as follows:
- Ask the child to elevate or shrug the shoulders (trapezius).
- Ask the patient to abduct the arms to horizontal position (deltoid C5, C6).
- Movements at different joints:
- Neck: Flexion, extension, side ways, and rotation
- Shoulder: Abduction, adduction, flexion, and extension
- Elbow: Flexion, and extension
- Wrist: Flexion and extension of the wrist, pronation and supination of the forearm
- Fingers: Abduction, adduction of the fingers, apposition of thumb and little finger, and hand grip
- Trunk muscles: Flexion, extension, lateral bending
- Hips: Flexion, extension, abduction, and adduction
- Knees: Flexion, and extension
- Ankle: Dorsiflexion and plantar flexion, inversion, and eversion
- Toes: Flexion and extension
- Ask the patient to flex the elbow with forearm supinated and palm facing upwards (biceps C5, C6).
- Ask the child to extend the arm against resistance (triceps C7, C8).
- With the patient sitting at the edge of the table, ask him to raise the leg to extend the knee (quadriceps L2, L3, L4).
- The patient lies in lateral decubitus and is asked to flex the knee and abduct the hip of superior leg (gluteus medius L4, L5, S1).
- The patient lies prone with both the knees flexed and is asked to lift the hips off the bed (gluteus maximus L5, S1, S2).
- The patient lies supine and is asked to push down examiner’s palm with sole of the foot (gastrocnemius and soleus L5, S1, S2).
- The patient lies supine and is asked to dorsi-flex the foot against resistance (tibialis anterior L4, L5, S1).
- Paralysis of respiratory muscles is characterized by rapid shallow breathing, weak voice or cry, inability to count beyond 10 with a single breath, anxious look and cyanosis.
- Paradoxical breathing, i.e. retraction of abdomen with each inspiration is suggestive of diaphragmatic paralysis which is often associated with paralysis of deltoid muscles because of identical spinal innervation (C5, C6).
- In phrenic nerve injury, paradoxical inward movement of ipsilateral abdominal wall occurs with inspiration due to paralysis of diaphragm.
- The umbilicus moves upwards towards the involved side which is called as “belly dancer’s sign”. The muscle power is graded as shown in.
Grading of muscle power:
- Muscle power → Grade
- No flicker → 0
- Flicker + → 1
- Movement possible with gravity eliminated → 2
- Movement possible against gravity → 3
- Movement possible against gravity → 4
- Normal power → 5
In hysterical paralysis, child makes little effort to execute a movement as evidenced by positive Hoover’s sign. The patient lies on his back and examiner puts one hand under the heel of the normal side.
The child is asked to elevate the apparently paralyzed leg keeping the knee extended. In genuine hemiplegia, while patient is attempting to raise the paralyzed limb, there is counterpressure from the normal limb. There is no counter-pressure or any muscle wasting in hysterical paralysis.
7. Coordination:
Incoordination is pathognomonic of cerebellar dysfunction.
The coordination cannot be tested unless child has fair degree of muscle power. Infant’s coordination can be tested by offering him small objects or toys by playful interaction.
- Finger-nose test: with eyes open and closed. Each arm in turn is drawn out to full abduction and child is asked to alternately touch the tip of his nose and examiner’s finger (which is moved to different positions) with the help of tip of his index finger. Look for intention tremors and past pointing (dysmetria).
- Dysdiadochokinesia: Inability to perform alternating movements with speed and precision, for example, Supination-pronation movements, clapping, slapping the thigh with the palm and back of the hand alternately, rapid touching of thumb and little fingers on both sides, etc. Normally children above 5 years of age are able to execute rapid alternate movements with ease and speed

- Handwriting: Record is useful for followup to assess the improvement. Ask the patient to draw a line between two converging lines, thread a needle or bead, draw a person, tieshoe laces, etc.
- Rebound phenomenon: Try to extend the patient’s elbow against his biceps contraction and resistance. When wrist is suddenly released the hand would jerk back suddenly and may hit his face. Positive rebound test is suggestive of cerebellar lesion.
- Heel-knee test: for lower limbs is equivalent of finger-nose test in the upper limbs. In addition, ask the patient to lie in a prone position and maintain his both legs flexed at
right angle at the knees. Observe how long the legs can be kept without fatigue and tremors. - Romberg’s sign: It is not a cerebellar sign but is used to assess loss of position sense (sensory ataxia) in the legs. The patient is asked to stand with feet close together. He is then asked to close the eyes.
- If Romberg’s sign: Is positive, as soonas the eyes are closed, the patient becomes unsteady and begins to sway and may even fall. The sign is positive in patients with tabes dorsalis and sensory neuropathy.
- Gait: Ask the patient to “tandem walk” along a straight line with the heel of one foot touching the toes of the other. Make the child walk around a chair, observe his balance on sudden bending of trunk or while taking sudden turn on walking.
8. Deep tendon reflexes:
There are involuntary contractions of muscles when their tendon is tapped with a reflex hammer which causes brisk stretch of the muscles. Tendon reflexes are exaggerated in patients with pyramidal lesion while they are sluggish or absent if lower motor neurons or muscles are diseased.
In muscle disease, tendon reflexes are diminished or absent in accordance with severity of muscle weakness. The patient should be relaxed and free from anxiety or tension when deep jerks are elicited.
The attention of the infant should be diverted by offering him a toy or key ring. Look for movements of the limb and visible contraction of the muscle. The spinal segments involved in various deep tendon jerks are given in.
Jaw jerk is elicited by asking the child to relax and open his mouth slightly. The examiner places his index finger on the midpoint of the child’s chin and taps it gently with a reflex hammer. Easily elicitable jaw jerk is indicative of pyramidal involvement above the level of pons.
Exaggerated jaw jerk in a child with evidences of pyramidal involvement in all the limbs indicates that lesion must be higher than the cervical spine. It is commonly seen in patients with pseudobulbar palsy, motor neuron disease, and disseminated sclerosis.
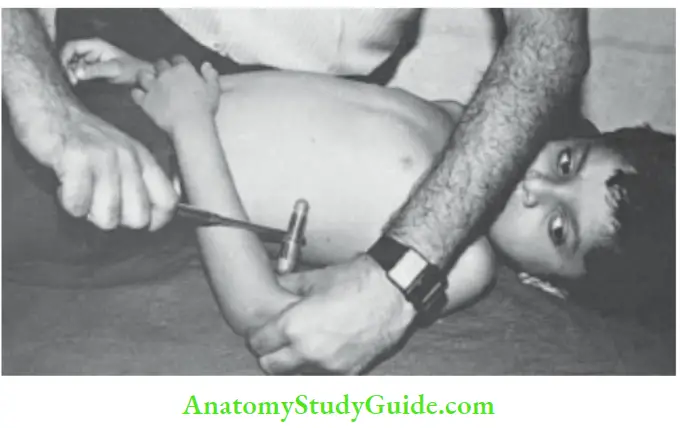
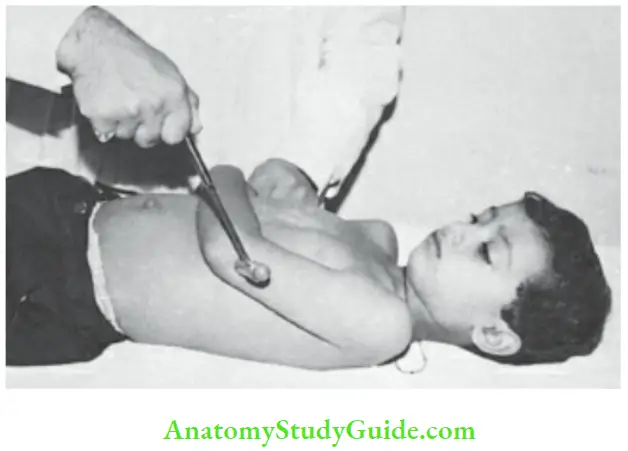
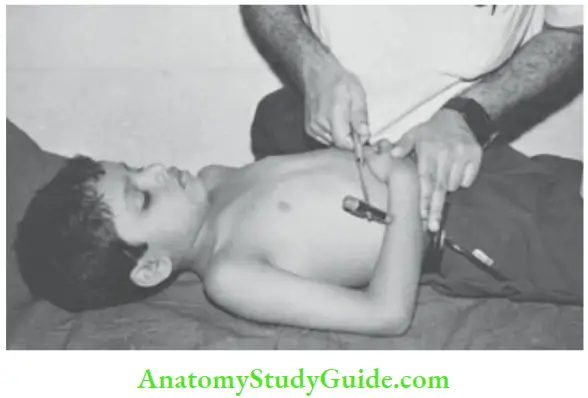
The techniques for elicitation of other deep tendon jerks are illustrated in. In newborn babies and infants, middle finger can be used (instead of reflex hammer) to elicit the deep tendon jerks.
Deep tendon jerks are rather brisk during infancy. When knee jerk is elicited on one side, crossed adductor response may be obtained in normal infants. The reacting muscle should be palpated as well as observed for the movement produced.
Toe jerks can be elicited in infants by tapping the base of the toes or dorsum of the foot. Brisk flexion of toes may be seen in infants with cerebral palsy and progressive degenerative brain disease.
Spinal root location of deep tendon jerks:
- Reflex – Segmental level
- Jaw jerk – Pons
- Biceps jerk – C5, C6
- Triceps jerk – C7, C8
- Supinator or radial jerk – C5, C6
- Knee jerk – L3, L4
- Ankle jerk – L5, S1, S2
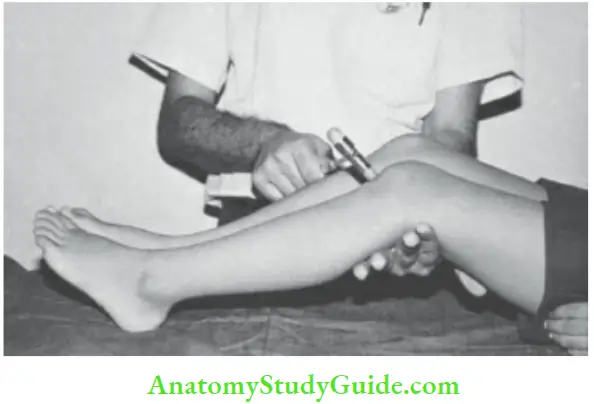
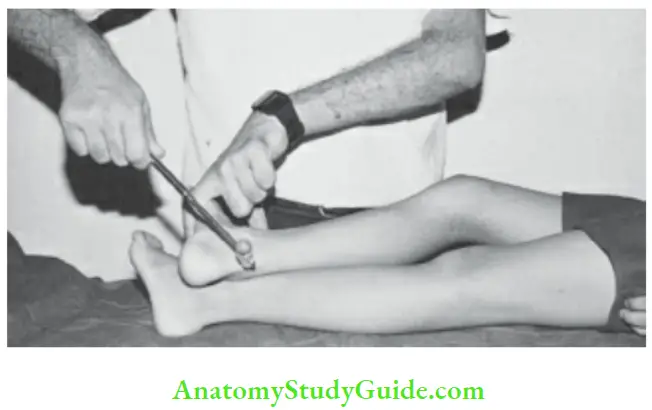
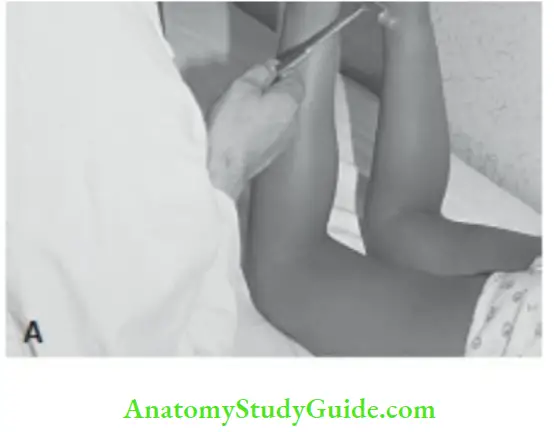
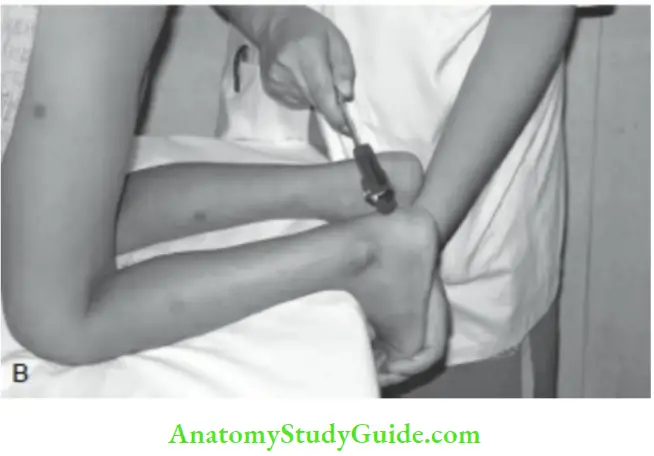
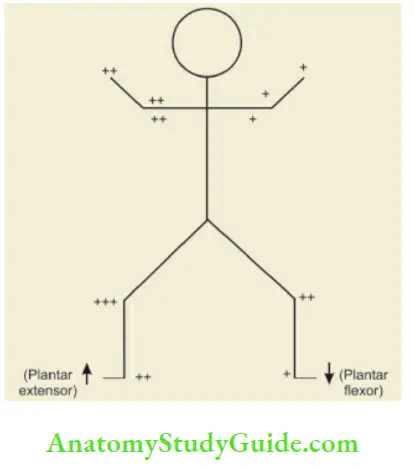
When deep tendon jerks are sluggish, try to elicit them after diverting child’s attention or reenforcement by using Jendrassik maneuver . When deep tendon jerks are exaggerated, look for sustained (at least 8–10 jerks) knee jerks and ankle clonus which are elicited by sudden jerky stretching of tendons .
Jendrassik maneuver. The child is asked to lock the hands and pull them apart to divert his attention, while deep tendon jerks are being elicited. Alternatively, the child can be asked to clench his teeth.
Grading of tendon reflexes
Absent even with reinforcement – 0
Sluggish – +
Normal – ++
Brisk – +++
Exaggerated and associated with clonus – ++++
Brisk or hyperactive tendon jerks may be associated with or without response in the muscles of adjacent joints or crossed response to the other side.
Sensations
There are two groups of sensory nerve fibers in tire spinal cord. Posterior column carries the information from the same side of the body for stereognosis, i.e. sense of position, weight, shape, size, and vibration.
The anterior and lateral columns carry the sensory information for touch, pain, and temperature from the opposite side of the body through anterior and lateral spinothalamic tracts.
A unilateral lesion of the spinal cord, therefore, results in loss of pain and thermal sensibility below the level of lesion on the opposite side of the body, while on the side of the lesion, in addition to spastic paralysis, there is loss of sense of position, size and vibration. (Brown-Sequard syndrome).
Look for anesthesia and ask for subjective features of hyperesthesia, i.e. excessive perception of pain and burning sensations wherein child may not tolerate touch or even the weight of the bed sheet.
Paresthesias, i.e. sensation of numbness, tingling, and crawling of ants is a recognized feature of Guillain-Barre syndrome, systemic lupus erythematosus, transverse myelopathy, tick paralysis, Refsum disease, and peripheral neuropathy.
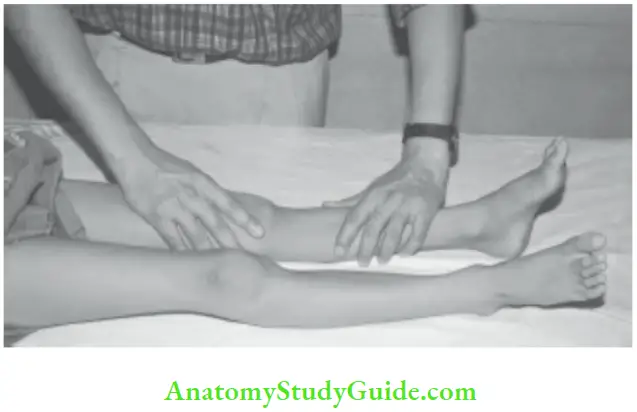
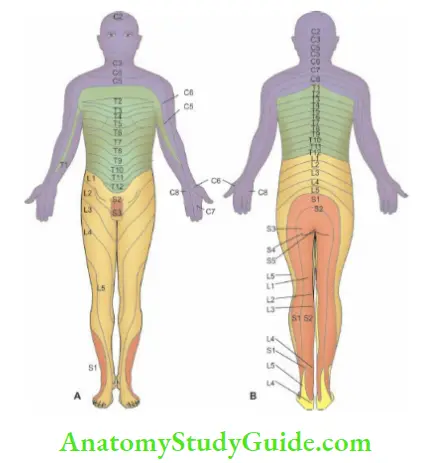
The precise evaluation of sensations is difficult in young children. shows sensory innervation of tire skin (dermatomes) over fire anterior and posterior aspects of fire body.
1. Superficial sensations:
Assess cotton touch, pain, (broken wooden spatula or toothpick), and temperature (hot and cold water in metal tubes). Avoid use of sharp pins and needles.
Congenital analgia is a recognized feature of congenital indifference to pain, congenital sensory neuropathy, Lesch-Nyhan syndrome, familial dysautonomia, autism, and Prader-Willi syndrome. These children do not cry when vaccine shots are given and may cause self-mutilation of their fingers or toes.
2. Deep sensations: Sense of pressure, sense of position, sense of movements, and vibration sense (128 Hz) are tested. They are impaired in the lower extremities in children with Friedreich ataxia.
3. Cortical sensations: The following signs are useful to assess the loss of cortical sensations.
- Two-point discrimination: Two pin pricks up to 1 cm apart can be normally appreciated. A pair of compass having two sharp pin ends can be used to assess two-point discrimination.
- Sensory inattention: Two mirror spots on the two sides are simultaneously pricked. The patient may not feel tire prick on tire affected side. When proximal and distal (cheek and hand) parts of tire body are touched simultaneously, the patient with parietal lobe lesion may not recognise the distal stimulus due to extinction.
- Astereognosis: The child is unable to identify an object by touch (with eyes closed), due to inability to appreciate shape, texture and weight.
- Graphesthesia: There is inability to appreciate the figures, and shapes drawn with a pen on the palms and soles of affected side.
Superficial Reflexes
1. Corneal or conjunctival reflex (5th and 7th cranial nerves):
Touching of cornea or bulbar conjunctiva with a cotton wick is followed by prompt closure of the eye. Ask the child to look in one direction and approach the bulbar conjunctiva from the other side.
When sensory reflex arc is disrupted (5th nerve damage), there will be no response from either lid when tire affected side is stimulated, and a normal response from both sides when the normal side is stimulated.
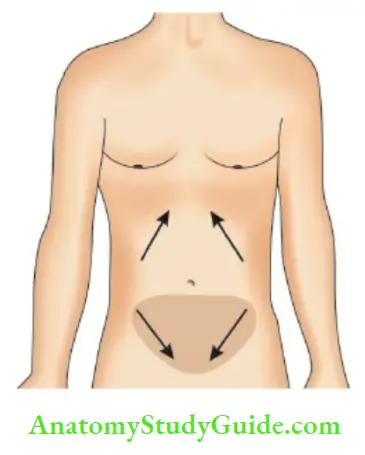
2. Abdominal reflexes (D6 – D12):
Stroke gently with a blunt pencil or a key four quadrants of the abdomen from periphery towards the midline . The underlying muscles in the quadrants would contract and the umbilicus moves in that direction. Abdominal fat of infants may interfere with the response.
Avoid too firm pressure which will elicit deep abdominal reflexes instead. The loss of abdominal reflexes (along with exaggerated deep tendon jerks in the lower limbs) is suggestive of pyramidal lesion above D6 level.
3. Cremasteric reflex (L1, L2):
Stroke the medial aspect of upper thigh and watch for ipsilateral contraction of cremaster muscle. It is usually lost in patients with pyramidal lesion above the level of L1.
It is normally exaggerated in infants and may remain intact even when there is a pyramidal lesion. The cremasteric reflex may be absent, if testes are undescended or already retracted and in a case of torsion of testis.
4. Anal reflex (S3, S4):
Perianal area is stroked and anal response observed. Anal tone can be assessed by inserting a finger into the anal canal.
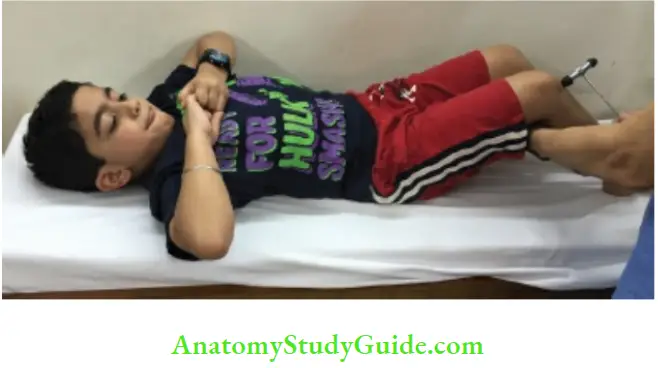
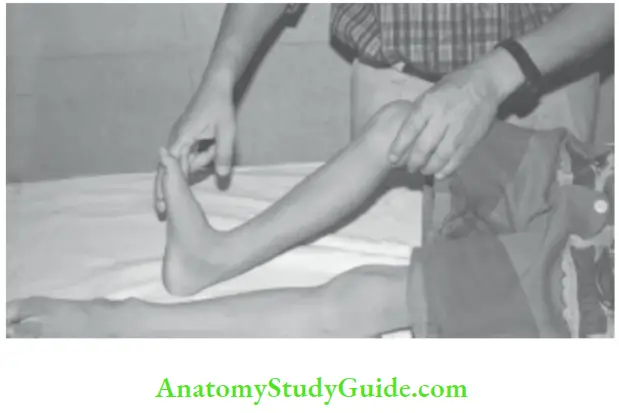
5. Plantar reflex orBabinski response (S1, S2):
The plantar surface of the foot is scratched with thumb’s nail, match stick, key, or any semi-sharp object along the lateral border of the sole, from heel forwards crossing over the distal ends of the metatarsals towards the base of great toe.
Younger is the child, lighter should be the stimulus. The response may be extensor (positive Babinski) with dorsiflexion of great toe and fanning of small toes, flexor (normal), equivocal, or withdrawal .
Infants up to two years of age, plantar response may be normally extensor on both sides and is associated with eversion of foot and dorsiflexion of ankle. Unilateral extensor plantar response is pathological even during infancy and is suggestive of pyramidal lesion. Extensor plantar response is diagnostic of pyramidal lesion above the level of S1.
In addition to conventional technique of elicting plantar response The following additional techniques may be used to elicit plantar reflex:
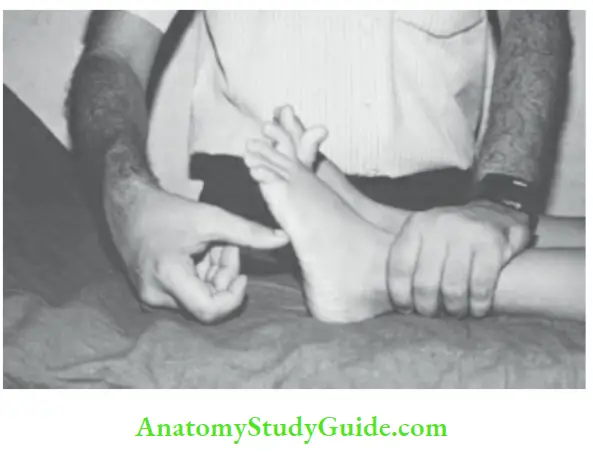
- Oppenheim’s sign: Apply firm pressure over the tibia from above downwards to elicit plantar response.
- Chaddock’s sign: Scratch around the lateral malleolus.
- Gordon’s sign: Firm squeeze of tendo-Achilles or muscles of calf is followed by plantar response.
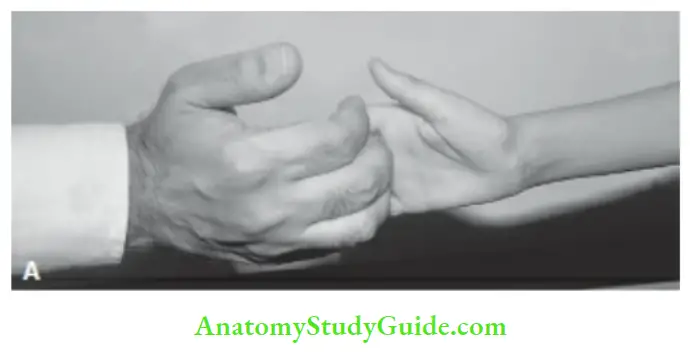
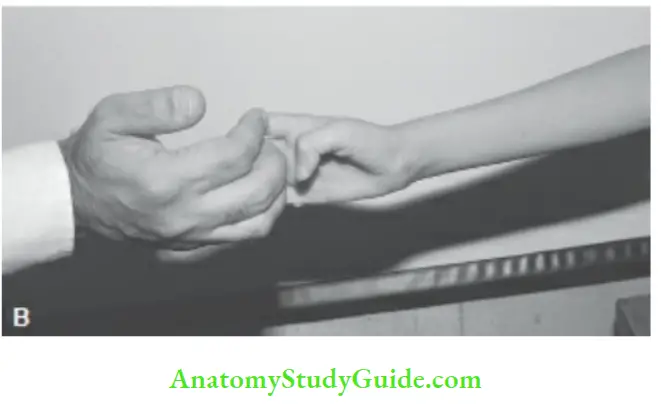
- Hoffmann’s sign: Is equivalent of Babinski in tire upper limbs. The patient is asked to stretch his hand towards the examiner with palm facing downwards.
The middle phalanxof the middle finger of the patient is grasped with the index finger and thumb of examiner’s hand . A sharp snap or flick is given to the terminal phalanx and nail of patient’s middle finger with the thumb of examiner’s right hand. Sudden adduction of patient’s thumb and flexion of other fingers is indicative of pyramidal lesion above C7. - Wartenberg’s sign: The child is asked to supinate his hand and flex the fingers like a claw. The examiner locks his flexed fingers with the patient and exerts resistance. Normally, the thumb extends but its terminal phalanx may flex slightly. In pyramidal tract lesion, thumb adducts and flexes strongly towards the palm


6. Glabellar tap reflex: Tapping of nasion is followed by blink response. The response normally disappears after 3 to 4 taps due to habituation. Persistent uninhibited glabellar tap response is suggestive of diffuse degenerative disorder of CNS.
7. Palmomental reflex: Scratch or tap tire thenar eminence of hand There is no response normally Contraction of the mentalis or orbicularis oris muscle on tire ipsilateral side is indicative of bilateral frontal lobe lesion.
8. Grasp reflex: The presence of unilateral grasp reflex in a child with CNS disorder is suggestive of a lesion of frontal lobe on tire opposite side.
9. Ciliospinal reflex: When skin of tire neck is pinched, pupil dilates due to stimulation of reflexspinal arc through sympathetic trunk. The absence of ciliospinal reflex is suggestive of deep coma and is used as one of tire criteria for brain death
Spine And Sphincters
They must be checked in every patient. The spinal cord ends at the level of lower border of body of first lumbar vertebra (lower border of L3 in the newborn) but meninges are carried as far down as second sacral vertebra. The spinal segments do not correspond numerically with overlying vertebrae as shown in
The 10th dorsal arch overlies L1 and L2, eleventh dorsal arch overlies L3 and L4 and twelfth dorsal arch overlies L5 and S1. All the sacral and coccygeal segments are located against the first lumbar vertebra. It should also be remembered that the spine corresponds to the next vertebral body below.
The urinary bladder has three neural mechanisms; sacral parasympathetic (S2, S3) which is excitatory or motor, inhibitory sympathetic supply ending at L1, L2 and a voluntary excitatory corticospinal pathway.
Cord lesions at the sacral level are associated with urinary retention. After a few weeks, reflex bladder evacuations occur in response to bladder distension. Lesions of the cauda equina usually result in persistent incontinence.
Higher cord lesions may lead to precipitancy or urgency of micturition and at times even hesitancy of micturition and retention of urine due to involvement of voluntary excitatory corticospinal fibers.
Bowel involvement is usually characterized by constipation and retention of feces irrespective of the level of lesion. The lesion at sacral level, however, is usually associated with relaxation of external rectal sphincter leading to fecal incontinence.
In diastemato-myelia, a bony or fibrocartilaginous septum produces a sagittal division and transfixation of the spinal cord or cauda equina. The clinical features include delay or difficulty in walking, an abnormal gait, weakness, and atrophy of muscles of lower extremity, deformities of feet, and urinary incontinence.
The caudal regression syndrome is characterized by sacral agenesis with associated abnormalities like a neurogenic bladder, weakness of lower extremities, equinovarus deformities of feet, and a froglike posture. The developmental defect is more common in infants born to diabetic mothers.
Identification of spinal segment in relation to vertebral body:
Vertebral body – Spinal segment
Cervical – Add 1
1st–6th Dorsal – Add 2
7th–9th Dorsal – Add 3
10th Dorsal – L1, L2
11th Dorsal – L3, L4
12th Dorsal – L5 and sacral segments
The salient clinical differences between extramedullary and intramedullary spinal tumors are shown in.
GAIT
Gait of the child should be closely observed to identify any abnormalities. The child should be asked to squat on the floor and watched as he gets up to the standing posture.
Gower’s sign, wherein child “climbs up his legs” to stand due to weakness of glutei maximi muscles is classically seen in children with Duchenne’s muscular dystrophy.
Difficulty in getting up from the squatting posture is also seen in children with polymyositis, poliomyelitis, and Guillain-Barre syndrome. Ask the child to walk on heels and toes, skip on one foot, and climb upstairs.
Children over 5 years of age are able to walk on their toes and hop. The ability to skip occurs by 7 years of age and tandem walking is achieved by 9 years. Gait is best evaluated when the child is unaware of being watched.
1. Spastic gait (pyramidal lesion):
There is circumduction and lifting of the leg in the form of an arc at the hip. Hip is elevated on the affected side with slight dragging of the foot and scraping of toes
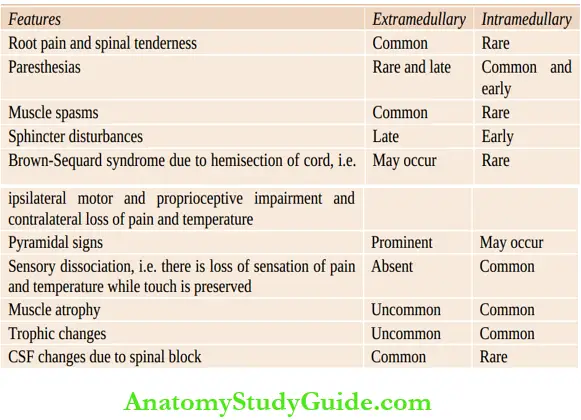
2. Stamping gait (posterior column lesion):
The foot is placed on tire ground with a thud due to loss of sense of position.
3. High stepping gait:
High steps are taken due to foot drop to avoid tripping of toes. The patient walks cautiously while watching tire floor intently. It is seen in children with peripheral neuropathy, poliomyelitis, and progressive muscular atrophy
4. Ataxic gait or staggering gait or reeling gait (cerebellar lesion):
Patient walks like a drunkard man. The gait is unsteady and uncoordinated and child cannot walk in a straight line or around a chair. Friedreich’s ataxia produces combined sensory and cerebellar ataxia.
5. Festinentgait (Parkinsonism):
The patient walks with short, stiff, and shuffling steps. The arms do not swing during walking.
6. Waddling gait:
The waddling gait is like the gait of a duck. The trunk is tilted backwards, with an increase in lumbar lordosis, tire feet are planted rather widely apart and the body sways from side to side as each step is taken.
It is seen in patients with Duchenne’s muscular dystrophy, bilateral congenital dislocation of hips, bilateral coxa vara (reduction of angle between the shaft and neck of the femur), achondroplasia, Morquio’s disease, exstrophy of bladder (pelvic bones are widely separated), bilateral slipped femoral epiphyses, polymyositis, Engelmann’s disease (progressive diaphyseal dysplasia) and myelodysplasia.
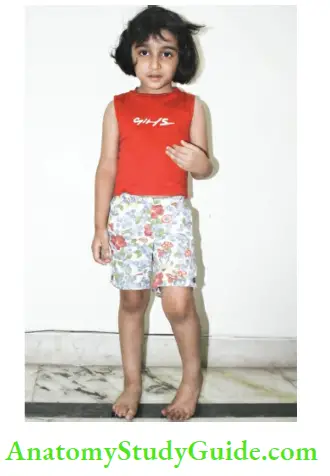
7. Scissor gait: It is seen in children with cerebral diplegia due to bilateral adduction and contractures.
8. Limping gait: This may occur due to a variety of neuromuscular and orthopedic disorders of the lower limbs.
9. Astasia abasia: Occurs due to hysterical inability to stand and walk. The patient is ataxic and sways from the hips rather than ankles. The ataxia decreases when patient is not watched or attention is diverted by asking him to execute the finger-nose test.
The hysterical patient does not injure himself. He is not benefitted by holding the wall or furniture, unlike a patient with organic ataxia.
Cerebellar Signs
1. Tone is decreased. Power is normal but there is easy fatiguability.
2. Nystagmus It is characterized by involuntary conjugate movements of the eyes which may be rhythmic (pendular) or non-rhythmic, with a fast and slow component. Nystagmus is defined by the direction of quick phase.
- It may occur spontaneously (vestibular) or induced by movements of the eyes.
- Ask the child to follow the movements of the examiner’s index finger or a toy, which is quickly moved horizontally or up and down.
- Keep the finger or toy at the extreme position for a few seconds to see the direction of quick movement and whether nystagmus is transitory or persistent.
- Nystagmus may be horizontal, vertical, rotary, or mixed.
- Coarse, slow, searching, pendular nystagmus movements are seen in blind children. In cerebellar nystagmus, the fast component is towards the side of lesion.
- The nystagmoid movements become slow and coarse when eyes are turned towards the side of lesion.
- In contrast, the fast component of the nystagmus is towards the normal side in vestibular dysfunction and the nystagmus is enhanced when the patient looks in the direction of fast component.
3. Skew deviation of eyes may occur in acute cerebellar lesions. The eye towards the side of lesion is turned downwards and inwards.
4. Incoordination. Its presence is assessed by following tests:
- Finger-nose test
- Dysdiadochokinesia
- Ankle-knee test
- Handwriting
- Rebound phenomenon
- Romberg’s sign is negative
5. Deep tendon jerks are pendular.
6. Speech is explosive and jerky with scanning of syllables.
7. Gait is ataxic or reeling in character. The patient has a tendency to fall towards the side of lesion. The minimal ataxia can be brought out by asking the patient to walk around a chair in both directions, taking sudden turn, sudden flexion of the trunk, and by doing sits-stands.
Trunkal ataxia is common among children due to involvement of vermis. Heel-to-toe walking and walking along a straight line are particularly difficult in these children, hi midline posterior fossa or cerebellar vermis lesion (tonsillar herniation due to Arnold-Chiari malformation), no abnormalities of coordination in upper limbs may be detected when patient is lying in bed. However, there will be gross ataxia on walking which should not be misdiagnosed as hysteria.
Autonomic Functions:
The autonomic nervous system comprises of central (cortical region, amygdala, hypothalamic and brainstem nuclei) and peripheral (sympathetic thoracolumbar outflow and parasympathetic craniosacral outflow) components.
Autonomic dysfunction is evidenced by instability and excessive fluctuations of vital signs, excessive or reduced sweating, areas of skin with blanching or blotchyness, inadequate or absent salivation or lacrimation, and sphincteric disturbances. Record the pulse rate at rest and following 6 maximal deep breaths.
In normal subjects, the pulse rate should fall by greater than 15 beats/min; while in autonomic dysfunction, pulse rate slows by less than 10 beats/min. In a patient with autonomic dysfunction, the systolic blood pressure may fall greater than 20 mm Hg on standing from recumbent position (orthostatic hypotension).
Diagnosis And Localization Of Cns Disorder
Imaging technology (CT scan, MRI) has provided most reliable and non-invasive means for exact localization of the space-occupying lesion and other disorders of the CNS.
Nevertheless, attempt should be made to identify the following characteristics of the CNS disorder, hi order to enhance clinical acumen, the diagnosis based on clinical evaluation of CNS should be correlated with CT/MRI findings to augment the learning process and improve clinical skills.
The following clinical parameters are useful to identify the site and nature of CNS disorder:
- Is disease acute or dramatic in onset, subacute or insidious?
- Is the disorder stationary, progressive or showing slow or fast recovery?
- Is it upper motor neuron or lower motor neuron disorder?
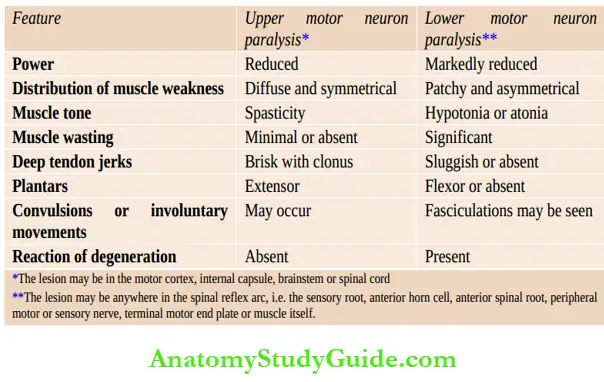
- Is patient having spinal shock? Sudden and complete transaction of spinal cord (traumatic or transverse myelitis) may produce transitory lower motor neuron features due to sudden loss of descending control of the lower motor neurons.
- There is dramatic onset of flaccid paralysis, areflexia, loss of sensations below the level of lesion, autonomic dysfunction, and loss of bowel and bladder control.
- The state of spinal shock is gradually followed by classical features of upper motor neuron paralysis over a period of a few days.
- Are there any associated clinical features of raised intracranial tension?
- Is the disease diffuse and generalized or localized to the specific area/s of the central nervous system?
- Is it primarily a white matter disease, gray matter disease, or combined?
- Summarize the positive CNS findings and their probable localization in the CNS.
- Provides useful guidelines for localization of the probable site of lesion in the CNS on the basis of abnormal neurological findings and basic knowledge of neuroanatomy.
- What is the probable nature of the disease and likely diagnostic possibilities?
- Is it a space occupying lesion, infective, metabolic or degenerative CNS disorder, vascular phenomenon, anoxic insult, toxic, traumatic, psychotic, functional disorder or conduct disorder?
- Advanced magnetic imaging techniques, like diffusion tensor imaging (DTI), functional MRI (fMRI), MR perfusion (MRP), and MR spectroscopy (MRS) are available for localization and definitive diagnosis of a variety of CNS disorders.
During the presentation of the case, the student is asked to summarize important findings of the history and physical examination, localize neurologic findings, formulate a differential diagnosis, provide the most likely diagnosis, discuss a diagnostic evaluation plan, and provide a management protocol.
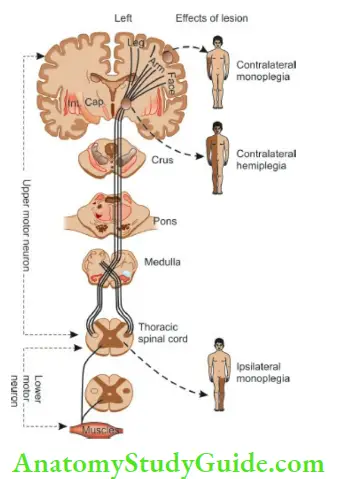
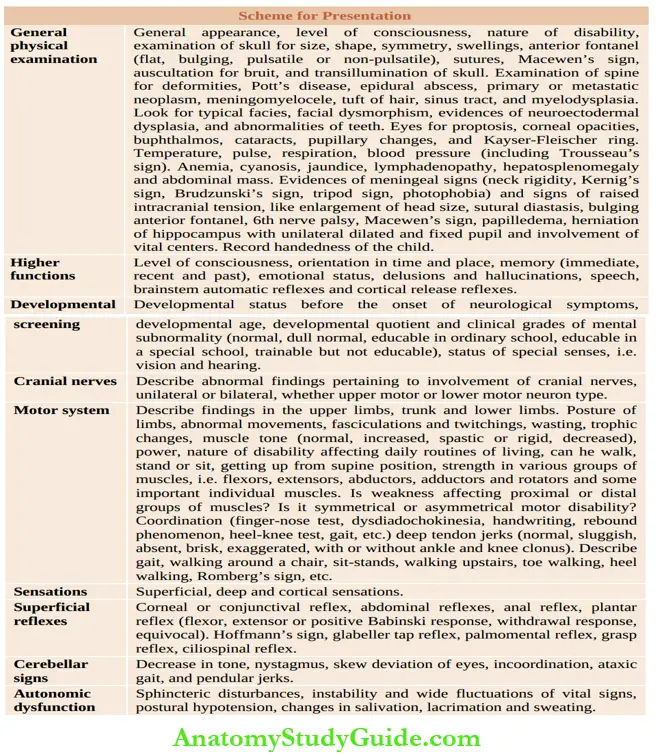
Leave a Reply