Tongue Anatomy Questions With Answers
Question 1: Why genioglossus is called ‘safety muscle’?
Table of Contents
Answer: 1. Genioglossus is a protractor of the tongue. It prevents the falling back of the tongue and prevents the choking of the air passage. Hence, it is called the “safety muscle of the tongue”.
Question 2: Name the muscles required for changing the shape of the tongue.
Answer: Intrinsic muscles of the tongue change the shape of the tongue. They are
1. Longitudinal
- Superior
- Inferior
2. Transverse
3. Verticals
Read And Learn More: Neck Anatomy Notes And Important Questions With Answers
Question 3: What is the effect of bilateral paralysis of genioglossus?
Answer: If both genioglossi are paralyzed, the tongue may fall backward. It obstructs the airway (oropharynx) which may lead to the death of an individual due to suffocation.
Question 4: Why jugular-omohyoid node is called the ‘lymph node of the tongue’?
Answer: The jugular-omohyoid node is situated close to the omohyoid muscle. It is mainly associated with drainage of the tongue.
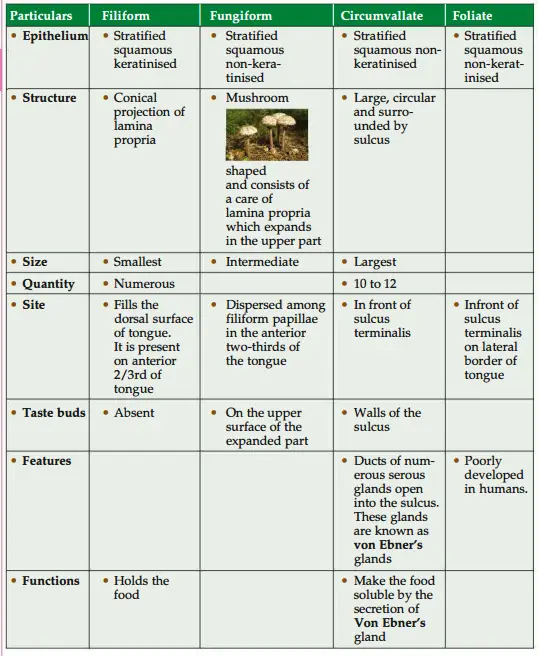
Question 5: Name different types of papillae present on the dorsum of the tongue and give their functions
Answer:
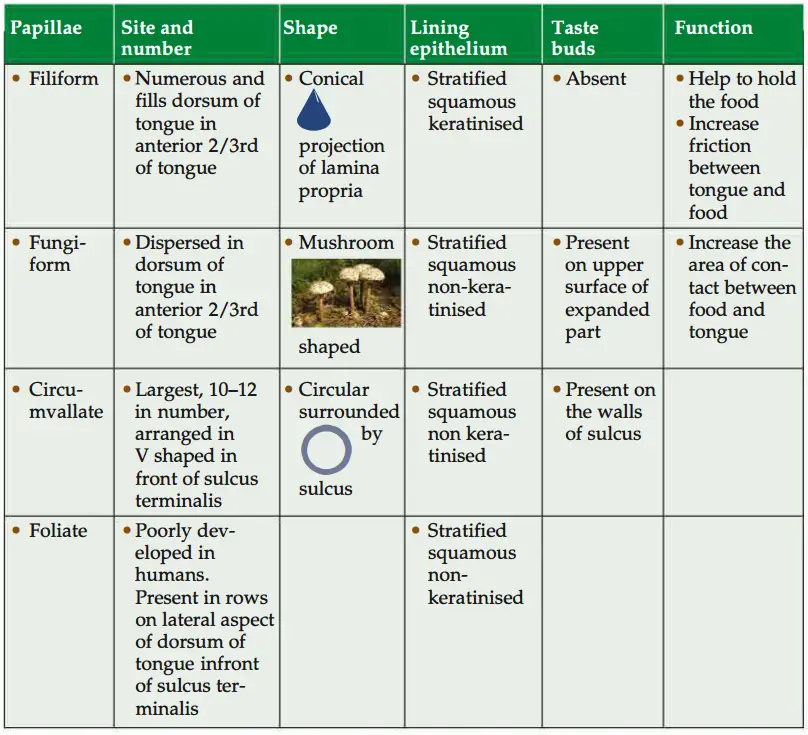
Define a lingual papilla. State its four types, salient features, differences, and functions of each
Question 6: Which lingual papilla does not contain taste buds?
Answer: Filiform papilla.
Question 7: What are Von Ebner’s, and Nuhn’s glands?
Answer: These are serous glands. The ducts of these glands open into the sulcus present around each circumvallate papilla.
Question 8: State the two types of epithelia found in lip and explain why these epithelia are found there.
Answer:
1. Outer surface lined by stratified squamous keratinised epithelium.
The outer surface of the lip is dry.
The cells on the surface loose nuclei and become dead and the
epithelium is called stratified squamous keratinised epithelium.
2. Inner surface is lined by stratified squamous non-keratinised epithelium. Inner surface of the lip remains moist.
The most superficial cells are living and nuclei can be seen in them.
This kind of epithelium is described as stratified squamous non keratinised epithelium. ”
Question 9: What is vermilion zone, border?
Answer: 1. In between the outer and inner surfaces, there is a zone of transition called vermilion zone.
2. It is lined by modified skin which does not have glands and hairs.
3. It has highly vascular dermis and because of this, it appears pink.
4. It lacks glands, so it remains dry and cracks in the dry weather.
5. It is kept moist by saliva to prevent cracking.
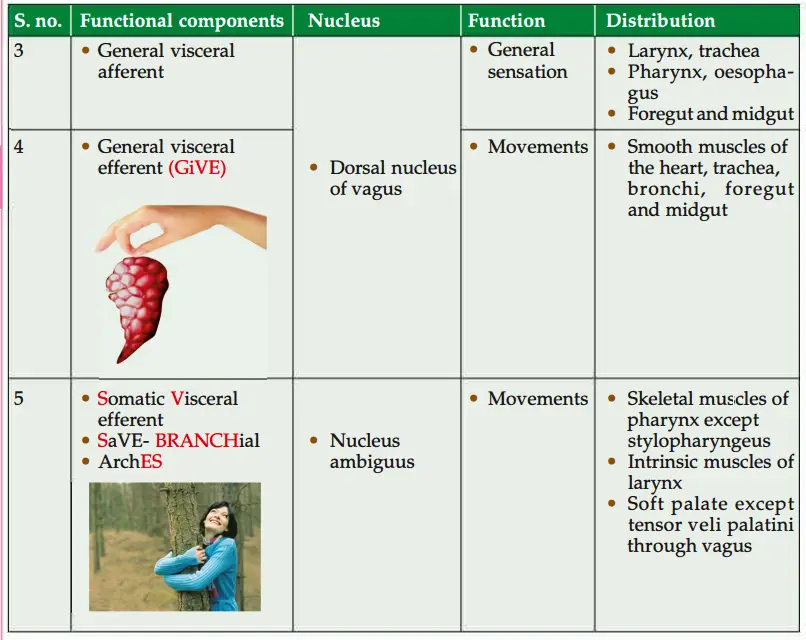
Vagus nerve (Alderman’s nerve) in neck
Introduction: It is Xth cranial nerve supplying mainly the muscles of larynx and
sensations to most posterior part of tongue.
1. Functional components:
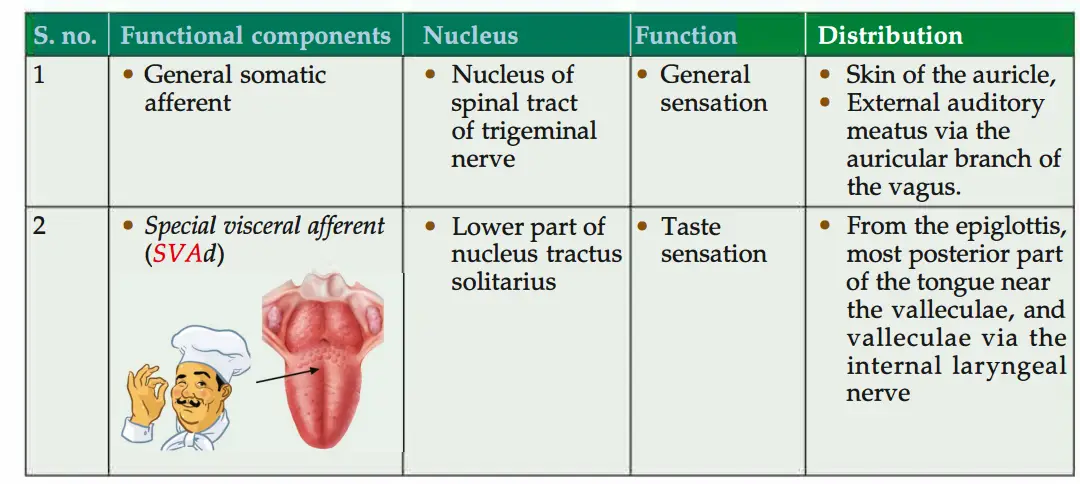
2. Exit from
- Brainstem: Post-olive sulcus.
- Cranium: Through the jugular foramen but separated from the glossopharyngeal nerve by a fibrous septum.
3. Ganglions
1. Superior (jgular): It lies in jugular foramen. It is connected with
- Inferior ganglion of the IXth (glossopharyngeal nerve),
- Cranial root of the Xlth (accessory nerve),
- Sympathetic trunk. It sends auricular branch which joins with the facial nerve by a twig. This ganglion is concerned with general somatic sensations via its auricular branch.
2. Inferior ganglion (ganglion nodosum): It lies just below the jugular foramen. It is connected with
- Hypoglossal.
- Superior cervical ganglion of the sympathetic.
Loop between Cl and C2 nerves.
This ganglion is concerned with special sense (taste) from the epiglottis, valleculae and general visceral sensory from the larynx, pharynx, heart, lungs, oesophagus, stomach and intestine.
4. Course
1. In the neck: The nerve descends vertically lying within the carotid sheath.
- Up to the level of the upper border of the thyroid cartilage, the nerve lies in between and behind the internal jugular vein and internal carotid artery.
- Below the level of the upper border of the thyroid cartilage, the nerve lies in between and behind the internal jugular vein and common carotid artery.
2. Entrance in the thorax:
1. Right vagus crosses
- Right subclavian, and
- Right common carotid arteries from front and enters the thorax.
2. Left vagus enters the thorax and lies between left common carotid and left subclavian arteries. It lies behind the left brachiocephalic vein.
5. Branches
1. From superior cervical ganglion
- Auricular,
- Meningeal,
2. From inferior ganglion
- Pharyngeal,
- Superior laryngeal,
- Internal laryngeal
- External laryngeal
3. Sinus branch
- Carotid body
- Carotid sinus
4. Superior and inferior cardiac branch.
5. Riht vagus gives right recurrent laryngeal nerve, only on the right side in the neck.
6. Left vagus gives left recurrent laryngeal nerve, in the thorax.
6. Development: It is the nerve of 6th branchial arch.
7. Applied anatomy
- Isolated lesions of the vagus nerve are uncommon but they may be involved in
injuries or disease of related structures. - Damage or compression of the vagus and/or recurrent laryngeal nerves during
surgical dissection of the carotid triangle may produce an alteration in the voice. - Ramsay-Hunt syndrome: It is due to herpes zoster infection of the geniculate ganglion of the facial nerve.
It is associated with ipsilateral facial paralysis.
It is usually transient.
There are vesicles on the external ear or tympanic membrane.
If the nerve is irritated, there is spasm and irritation of the muscles of the pharynx.
It causes cough. - Auricular branch of vagus nerve is stimulated by
Impacted wax, or - By syringing the external ear. It can give rise to reflex cough.
If the nerves of both sides are cut, both the vocal folds are paralysed and take the paramedian position. - If left nerve is cut, the left vocal fold will be paralysed and become motionless.
- The right vocal fold will cross the midline of the rima glottidis as a compensatory phenomenon.
As a result, the voice is possible but very weak.
8. Testing of the nerves
- The pharyngeal reflex may be tested by touching the lateral wall of the pharynx with a spatula.
- The innervation or the soft palate can be tested by asking the patient to say “ah”.
Normally, the soft palate rises and the uvula moves backward in the midline. - Hoarseness or absence of the voice may occur. Laryngoscopic examination may reveal abductor paralysis.
- The lesions of the vagus nerve will produce following effects:
- Nasal regurgitation of the swallowed liquids.
- Nasal twang of the voice.
- Flattening of the palatal arch.
- Hoarseness of the voice.
- Cadaveric position of the vocal cords and dysphasia.
Question 10: Describe tongue under the following heads:
1. Muscles of tongue,
2. Tongue Blood supply,
3. Lymphatic drainage,
4. Applied anatomy of lymphatic drainage,
5. Tongue Nerve supply,
6. The 4 varieties of papillae,
7. Tongue Development, and
8. Tongue Applied anatomy
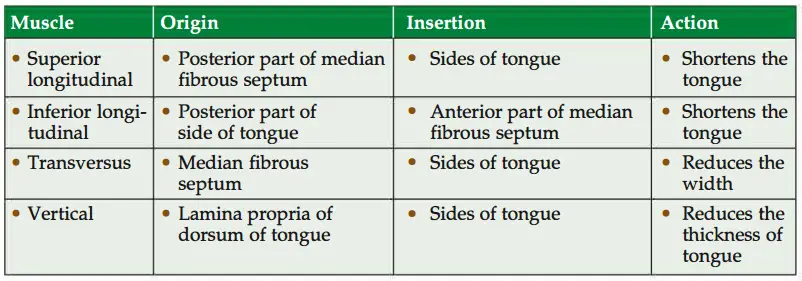
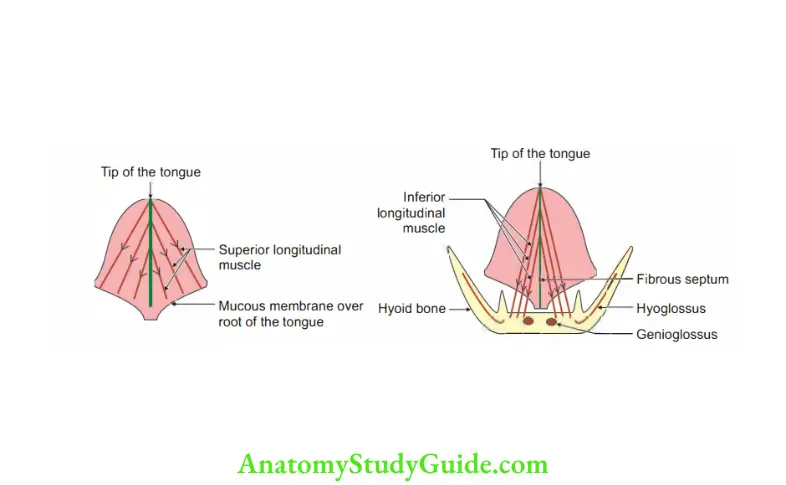
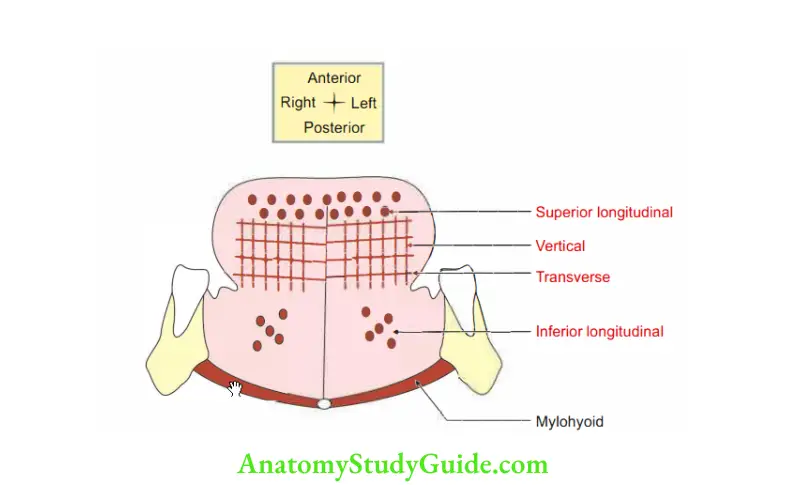
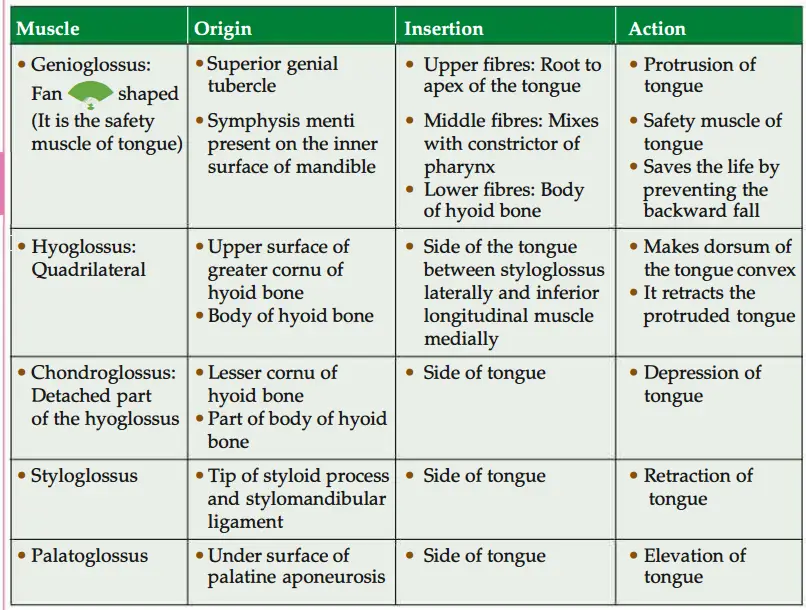
Answer: 1. Muscles of tongue: These are grouped into intrinsic and extrinsic muscles.
- Intrinsic muscles: The muscles having origin and insertions in the tongue.
They alter the shape and size of tongue. - Extrinsic muscles of tongue
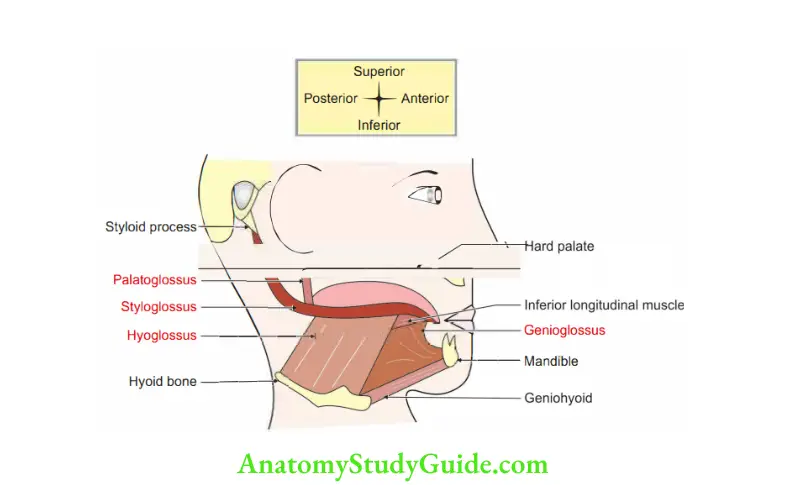
2. Tongue Blood supply
1. Arterial supply
The lingual artery (chief artery of the tongue), a branch of the external carotid artery supplies the tongue through
- Profunda lingual artery: It supplies the oral part of the tongue.
- Dorsal lingual artery: It supplies the pharyngeal part of the tongue.
Facial artery through
- Ascending palatine.
- Tonsillar branch.
2. Ascending pharyngeal branch of the external carotid artery.
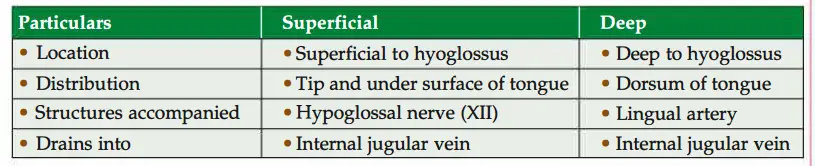
lingual vein.
Venous drainage: Veins are arranged in two sets. Mainly drain into profunda lingual vein.
3. Tongue Lymphatic drainage
1. Peculiarities
- Do not accompany the blood vessels.
- The tip of the tongue has the richest lymphatic plexus.
- Lymphatics in the posterior one-third of the tongue drain bilaterally.
- Lymphatics of the tongue ultimately drain into Jugulo-OmoHyoid Nodes.
Hence, they are called lymph nodes of the tongue. JOHN has TONGUE.
Lymphatic drainage of the tongue consists of the following sets.
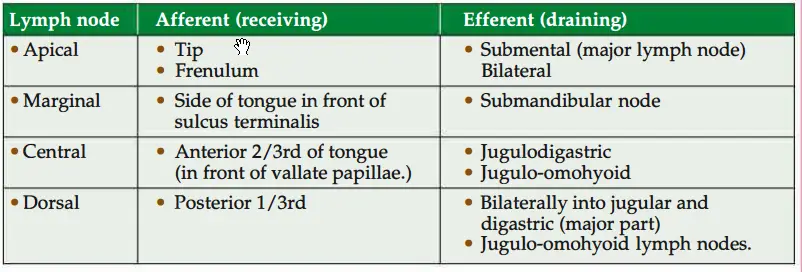
4. Applied anatomy of lymphatic drainage
- Malignancy in the tip and posterior one-third of the tongue is more dangerous since it drains bilaterally.
- Lymph vessels piercing the mylohyoid are often closely related to the periosteum of the mandible accounting for early spread to the bone.
5. Nerve supply of tongues: It is divided into motor and sensory.
1. Motor
- Somatomotor: All the extrinsic and intrinsic muscles of the tongue are supplied by the hypoglossal nerve (nerve of occipital myotome) except the palatoglossus which is supplied by the pharyngeal plexus.
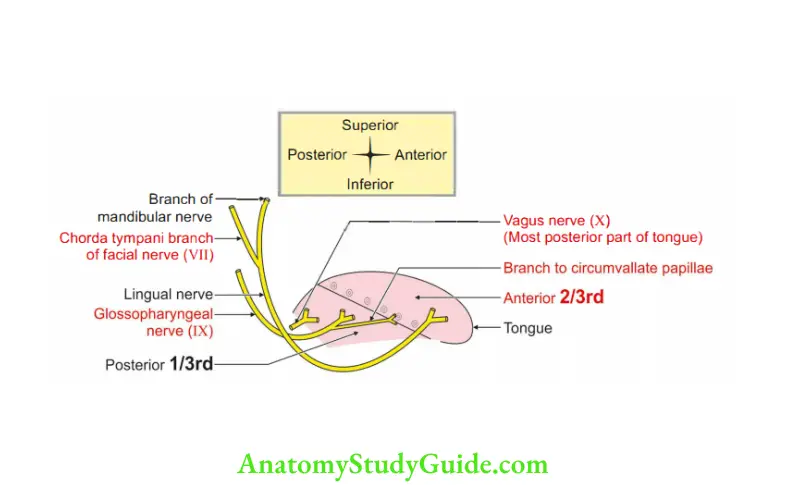
- Secretomotor fibers are derived from superior salivatory nucleus-facial nerve chords tympani-lingual nerve-submandibular ganglion-lingual glands.
- The vasomotor nerve arises from the spinal cord-superior sympathetic ganglion plexus around the external carotid artery (plexus around the lingual artery).
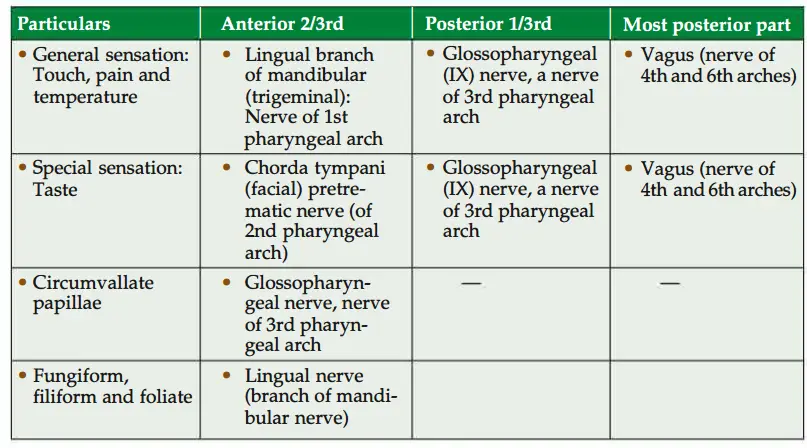
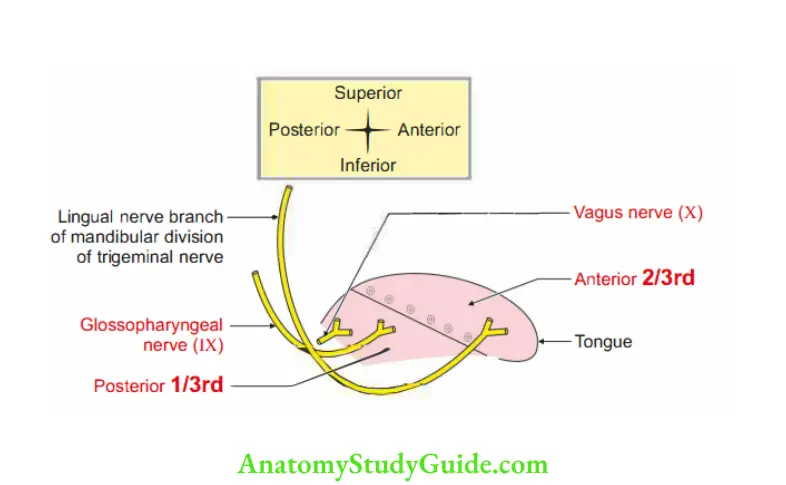
2. Sensory
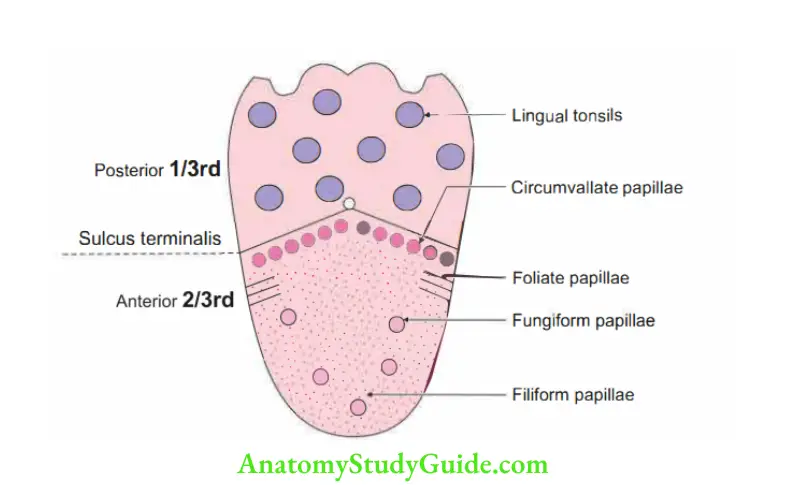
6. The papillae are of four varieties
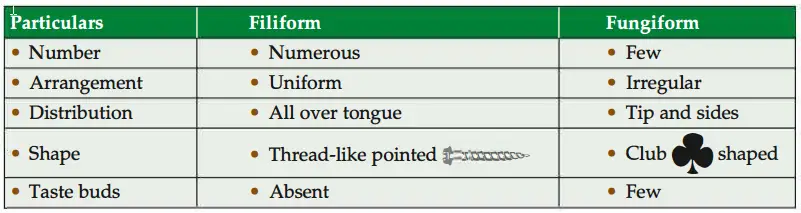
1. Filiform
2. Fungiform
3. Vallate, and
4. Foliate.
They consist of a fibrous core derived from the tunica propria, covered with
stratified squamous epithelium.
1. The filiform papillae are tapering and thread-like.
They are arranged in V-shaped rows present over the dorsum of the oral part of the tongue.
They contain touch corpuscles.
Their epithelium is scaly.
In some animals (For Example. cats, and cows), it is cornified and is used as a rasp (grating noise) to grasp food.
2. Thefugifrm papillae have globular heads and are red.
The core is more vascular and the epithelium is not scaly.
They lie scattered singly among the filiform papillae.
They are present at the tip and margin of the tongue. They do not rise above them.
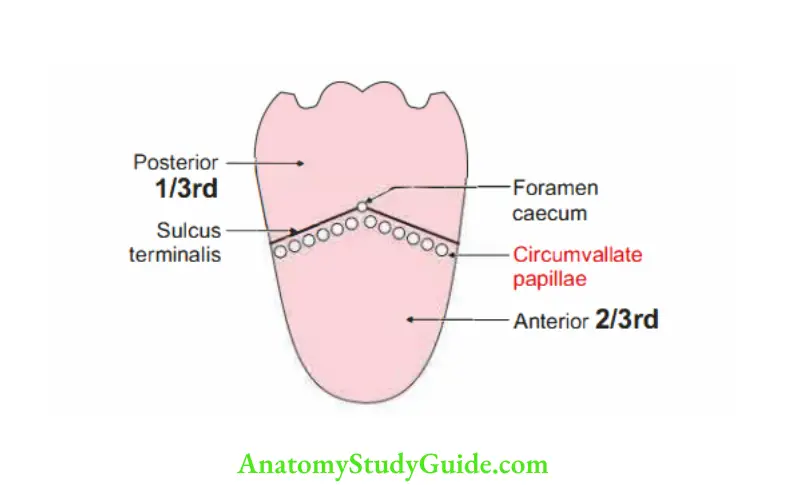
3. The vallate papillae are circular, about 2 mm in diameter.
They are a dozen in number.
They are also arranged in a V-shaped row just in front of the sulcus terminalis. Their fiat tops hardly rise above the general surface.
4. The foliate papillae, rudimentary in man, are 3 4ertical folds at the hinder part of the sides of the tongue.
Taste buds occur on most fungiform papillae, on the opposite sides of the foliate, and on both walls of the vallate.
They also occur sparsely on the soft palate, epiglottis, and posterior wall of the pharynx.
7. Development of the tongue
1. Chronological age: It develops in the 4th week of intrauterine life.
2. Germ layer
- Tip of tongue-surface ectoderm
- Base of tongue-endoderm
- Muscles-mesoderm
3. Site: Floor of the pharynx just cranial to median thyroid diverticulum.
4. Sources
1. Muscles:
- All the muscles of the tongue are developed from the occipital myotome except the palatoglossus.
The nerve of the occipital myotome is hypoglossal (12th cranial nerve).
Hence, all the muscles are supplied by the hypoglossal nerve. - Palatoglossus developed from pharyngeal arches which develop from r neural crest cells.
2. Mucous membrane: It is developed from the endoderm of the floor of the pharynx and is subdivided into
1. Anterior 2/3rd is developed from:
- Fusion of a pair of lingual swelling arising from the pouch of the 1st branchial I arch, and
- Tuberculum impar (impar unpaired) a midline swelling arises from 1st pouch and gives a very little contribution.
The post-trematic nerve of 1st arch is the lingual nerve and the pre-trematic nerve of 2nd arch is chorda tympani nerve.
2. Posterior 1 /3rd is developed from the cranial part of hypobranchial eminence, which is formed by the fusion of the 3rd and 4th branchial arches only.
The eminence is divided by a transverse groove into cranial and caudal parts.
The nerve of the 3rd arch is the glossopharyngeal nerve, the nerve of the 4th arch is the superior laryngeal nerve and the nerve of the 6th arch is the recurrent laryngeal nerve.
3. Fibrous stroma: Blood vessels and lymphatics are developed from the mesoderm of the adjacent arches.
4. Papillae:
- Formed by thickening of epithelium of the dorsum of the tongue.
- Fungiform and filiform papillae develop in the anterior two-thirds of the tongue.
- Circumvallate papillae develop in the posterior one-third of the tongue which is developed from the 3rd pharyngeal arch.
The nerve of the posterior one-third of the tongue is the glossopharyngeal nerve.
It gets submerged by the overgrowth of the 3rd arch and these papillae occupy the anterior wall of the sulcus terminalis.
Hence, they are supplied by the glossopharyngeal nerve (9th nerve).
5. Anomalies
1. Ankyloglossia: Restricted movements of tongue. It may be
- Ankyloglossia superior: The tongue is adherent to the palate.
- Ankyloglossia inferior or tongue-tie: The tongue is adherent to the floor of the mouth.
2. Microglossia: Too small tongue.
3. Aglossia: Absence of tongue. This is due to complete agenesis of the tongue.
4. Hemiglossia: Suppression of one of the lingual swellings.
5. Macroglossia: Too large tongue.
6. Tongue Applied anatomy
- Injury to the hypoglossal nerve produces paralysis of the muscles of the tongue on the side of the lesion.
Infranuclear lesion shows ipsilateral hemiatrophy of the tongue. Supranuclear lesion produces paralysis without wasting. - In an unconscious patient, the tongue may fall back and obstruct the air passage.
This can be prevented by keeping the tongue on one side or pulling the tongue
anteriorly. - Carcinoma of the tongue is quite common. It is better treated by radiotherapy than by surgery.
Occipital myotome
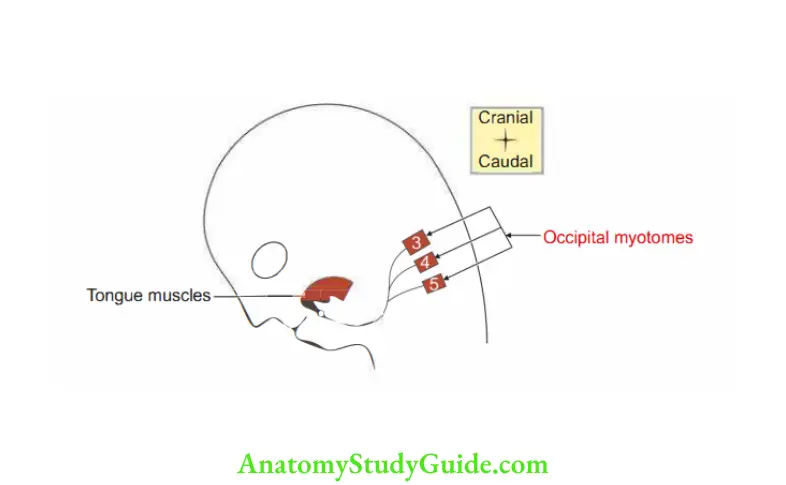
Occipital Myotome Introduction: The muscles of the tongue are developed from occipital myotomes.
1. Occipital Myotome Formation: They are formed by occipital or precervical somites.
2. Occipital Myotome Number: They are four in number. The 1st somite disappears.
3. Occipital Myotome Innervation: Pre-cervical nerves. These nerves unite and form the hypoglossal nerve.
4. Occipital Myotome Course: As the tongue develops in the floor of the pharynx, the occipital myotome migrates and invades the substance of the tongue.
Circumvallate papillae
1. Papillae surrounded by trench.
2. Circumvallate Papillae Size: 2 mm, pinhead size.
3. Circumvallate Papillae Number: About 10 to 12.
4. Circumvallate Papillae Situation: They are present in front of the sulcus terminalis as a single row.
5. Circumvallate Papillae Contains taste buds, present on the lateral wall of papillae.
6. Circumvallate Papillae Taste buds: They contain three types of cells.
- Gustatory cells or bipolar cells.
- Sustentacular or supporting cells.
- Basal cells.
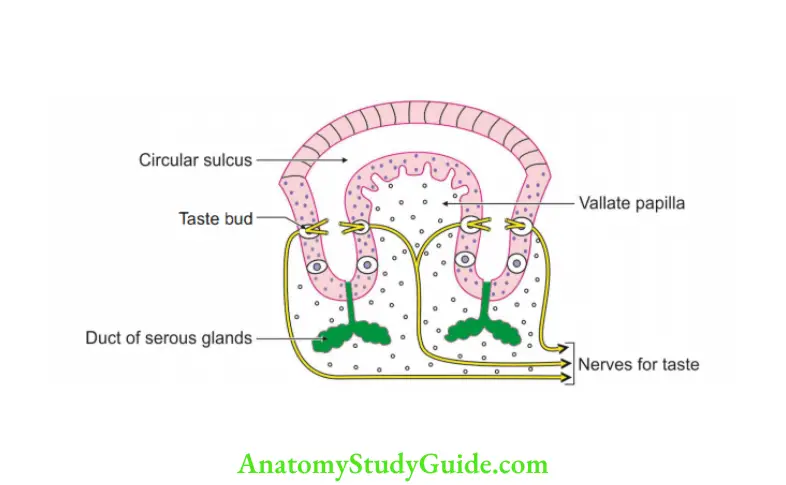
7. Nerve supply: Glossopharyngeal nerve (IXth cranial nerve).
8. Development: It develops in the posterior one-third of the tongue, migrates, and settles in the anterior two-thirds of the tongue in front of the sulcus terminalis.
Histological Features Of Taste Buds
1. These are end organs for taste sensations.
2. Each is barrel-shaped and stands on the corium but extends through the whole thickness of the epithelium. It opens on the surface through a minute gustatory pore. They are formed of two types of cells.
1. The gustatory cells are
- Slender, fusiform.
- Situated in the central part of the taste bud.
- The central part of each cell contains the nucleus.
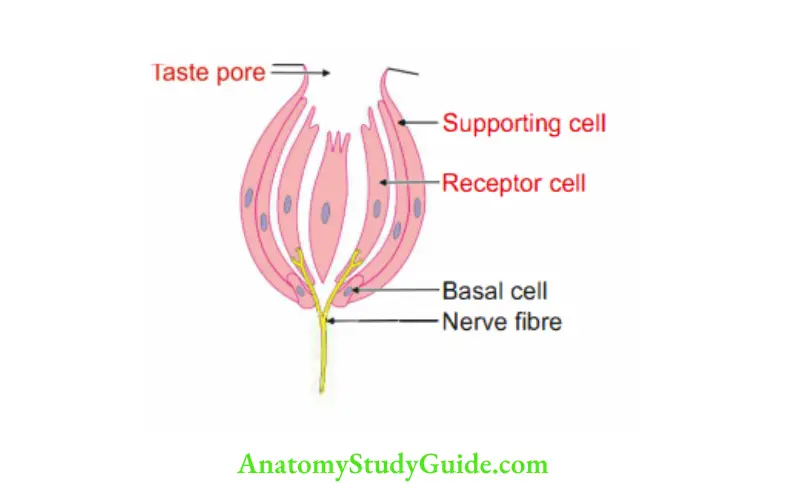
The ends are tapering.
- At one end, it has a hair-like process that projects through the gustatory pore.
- The other end is branched and sensory nerve fibers end around these processes as well as between the cells.
2. Sustentacular cells form a lining for the taste buds and, therefore, surround the gustatory cells. They are also long and slender.
Foliate papillae of the tongue
Foliate Papillae Of Tongue Introduction: They are vertical mucous folds occasionally noted on the side of the tongue.
1. Foliate Papillae Of Tongue Site: They are present close to the palatoglossal arch. Found in the anterior two-thirds of the tongue in front of the lateral end of the sulcus terminalis.
2. Foliate Papillae Of Tongue Number: 3 to 4.
3. Foliate Papillae Of Tongue Content: Taste buds.
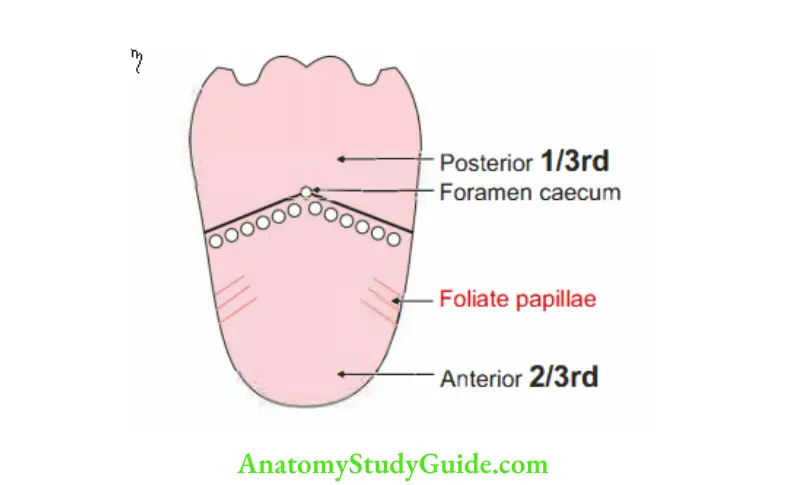
Note: They are present in rabbits. They are not prominent in man.
Question 11: Describe the lingual nerve under the following heads:
1. Lingual Nerve Origin,
2. Lingual Nerve Course,
3. Lingual Nerve Branches,
4. Lingual Nerve Distribution, and
5. Lingual Nerve Applied anatomy
Answer: Lingual Nerve Introduction: It is the sensory nerve of the anterior two-thirds of the tongue.
1. Lingual Nerve Origin: It is one of the two terminal branches of the mandibular nerve.
2. Lingual Nerve Course
1. It begins 1 cm below the base of the skull.
2. It runs between
- Tensor palatine and pterygoid, and then
- Lateral and medial pterygoids.
3. It joins at an acute angle with chorda tympani nerve.
4. At the lower border of the lateral pterygoid, it runs downwards between the medial pterygoid and mandible.
5. It lies anterior to the inferior alveolar nerve.
6. It lies in direct contact with the mandible.
It is medial to the third molar tooth.
It is covered only by a mucous membrane.
Hence, it is palpated from within the mouth.
7. It runs forward across the floor of the mouth and supplies the mucous membrane.
8. It lies on the hyoglossus muscle.
Here, it has connections with the submandibular ganglion.
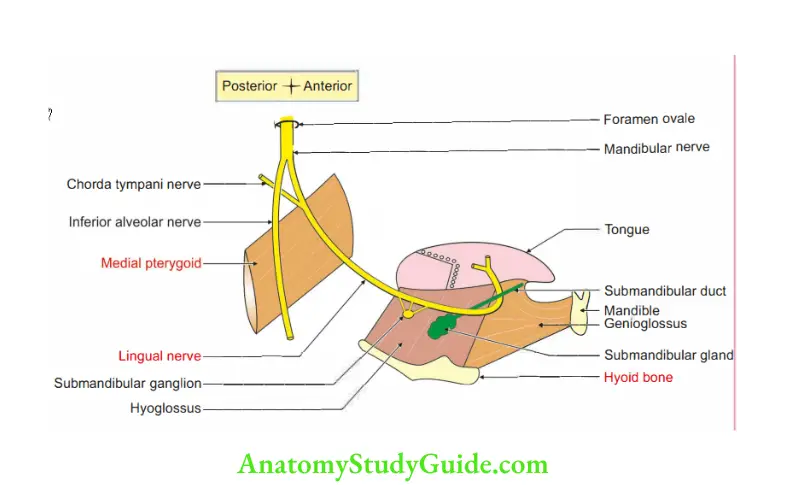
9. It lies deep in the submandibular duct. It runs forward and upwards between sublingual and genioglossus. It then divides into terminal branches.
3. Lingual Nerve Branches
- The gingival branch supplies all the lingual gum and mucous membrane.
- Communicating branches to
- Submandibular ganglion, and
- Hypoglossal nerve
4. Lingual Nerve Distribution
- It carries general sensations (of touch, pain, and temperature) and special sensations (of taste through chorda tympani) from the anterior two-thirds of the tongue.
- It carries pre- and post-ganglionic secretomotor fibers to salivary glands in the floor of the mouth.
- It has sensory fibers in the
- The mucous membrane lining the floor of the mouth, and
- Lingual surface of the mandibular alveolar process.
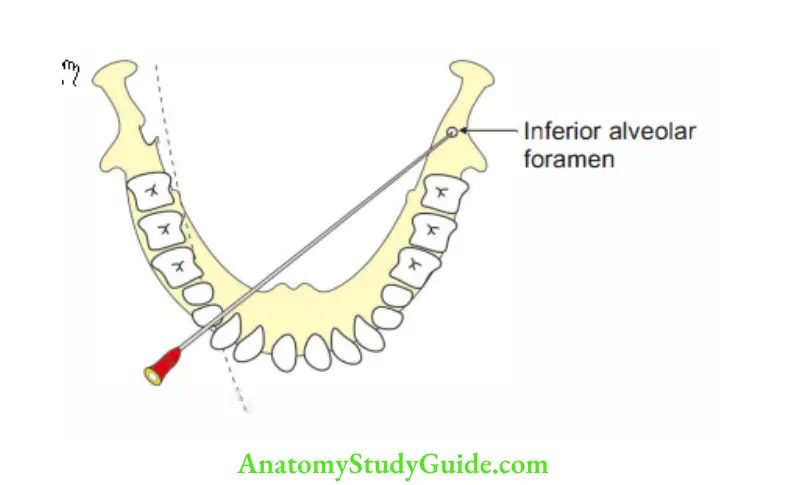
5. Lingual Nerve Applied anatomy
- The lingual nerve is closely related to 3rd molar tooth.
Care is taken while extracting a misplaced wisdom tooth to avoid injury to the lingual nerve. - Lingual nerve block: It is approached from premolar teeth of the opposite side, a small injection is made 0.5 cm from the mucosal surface when the needle is above the lingual nerve.
Leave a Reply