Gangrene
Gangrene is necrosis of tissue associated with superadded putrefaction, most often following coagulative necrosis due to ischaemia (for example , In gangrene of the bowel, gangrene of limb). On the other hand, gangrenous or necrotising inflammation is characterised primarily by inflammation provoked by virulent bacteria resulting in massive tissue necrosis.
Read And Learn More: General Pathology Notes
Thus, the end-result of necrotising inflammation and gangrene is the same but the sequence in which the two are produced, is different. ”
The examples of necrotising inflammation are: gangrenous appendicitis, gangrenous stomatitis (noma, cancrum oris).
There are 2 main types of gangren dry and wet, and a variant of wet gangrene called gas gangrene. In all types of gangrene, necrosis undergoes liquefaction by the action of putrefactive bacteria.
1. Dry Gangrene:
This form of gangrene begins in the distal part of a limb due to ischaemia. The typical example is dry gangrene in the toes and feet of an old patient due to severe atherosclerosis of arteries supplying blood to the lower limb. Other causes of dry gangrene foot include thromboangiitis obliterans (Buerger’s disease), Raynaud’s disease, trauma, ergot poisoning.
It is usually initiated in one of the toes which is farthest from the blood supply, containing so little blood that even the invading bacteria find it hard to grow in the necrosed tissue.
The gangrene spreads slowly upwards to the point where the blood supply is adequate to keep the tissue viable. A line of separation is formed at this point between the gangrenous part and the viable part.

Morphologic Features of Dry Gangrene:
- Grossly, the affected part is dry, shrunken and dark black, resembling the mummified foot.
- It is black due to liberation of haemoglobin from haemolysed red blood cells which is acted upon by hydrogen disulfide (H2S) produced by bacteria resulting in formation of black iron sulfide.
- The line of separation usually brings about complete separation with eventual falling off of the gangrenous tissue if it is not removed surgically (i.e. spontaneous amputation)
- Histologically, there is necrosis with smudging of the tissue. The line of separation consists of inflammatory granulation tissue.
2. Wet Gangrene:
Wet gangrene occurs in naturally moist tissues and organs such as the bowel, lung, mouth, cervix, vulva etc.
Two other examples of wet gangrene having clinical significance are as follows:
- Diabetic foot which is due to high glucose content in the necrosed tissue which favours growth of bacteria.
- Bed sores occurring in a bed-ridden patient due to pressure on sites like the sacrum, buttocks and heel.
Wet gangrene is more rapid and develops more often from blockage of venous drainage, but may also occur from blockage of both venous and arterial blood flow. The affected part is stuffed with blood which favours the rapid growth of putrefactive bacteria.
The toxic products formed by bacteria are absorbed in the circulation causing profound systemic manifestations of septicaemia, and finally death. Wet gangrene generally lacks clear-cut line of demarcation and may spread to peritoneal cavity causing peritonitis.



Morphologic Features:
- Grossly, the affected part is soft, swollen, putrid, rotten and dark. The classic example is gangrene of the bowel, commonly due to strangulated hernia, volvulus or intussusception. The part is stained dark black due to the same mechanism as in dry gangrene.
- Histologically, there is coagulative necrosis with stuffing of affected part with blood. The mucosa is ulcerated and sloughed. Lumen of the bowel contains mucus and blood. Affected tissue area intense acute inflammatory exudates and thrombosed vessels. The line of demarcation between gangrenous segment and viable bowel is generally not clear-cut.
Gas Gangrene:
It is a special form of wet gangrene caused by gas-forming clostridia (grampositive anaerobic bacteria) which gain entry into the tissues through open contaminated wounds, especially in the muscles following roadside injury, or as a complication of operation on colon which normally contains clostridia.
Clostridia produce various toxins which produce necrosis and oedema locally and are also absorbed producing profound systemic manifestations.


Morphologic Features of Gas Gangrene:
Grossly, the affected area is swollen, oedematous, painful and crepitant due to accumulation of gas bubbles of carbon dioxide within the tissues formed by fermentation of sugars by bacterial toxins. Subsequently, the affected tissue becomes dark black and is foul-smelling.
Microscopically, the muscle fibres undergo coagulative necrosis with liquefaction. Large number of gram-positive bacilli can be identified. At the periphery, a zone of leucocytic infiltration, oedema and congestion are found. Capillary and venous thrombi are common.
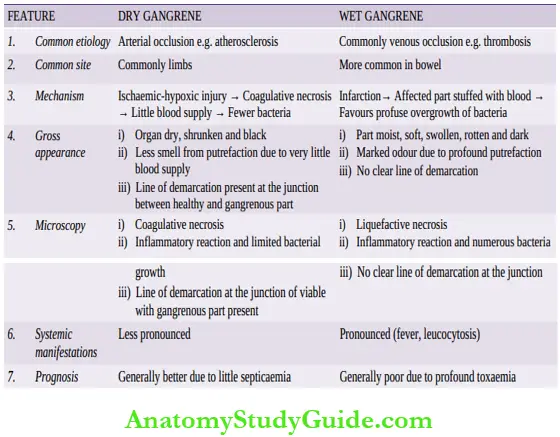
Contrasting features of dry and wet gangrene:
Gangrene:
- Gangrene is necrosis of tissue associated with superadded putrefaction, most often following coagulative necrosis due to ischaemia.
- There are 2 main types of gangrene — dry and wet.
- Dry gangrene begins in the distal part of a limb due to ischaemia for example,Due to severe atherosclerosis, Buerger’s disease etc.
- A line of separation generally marks the junction of viable and gangrenous tissue e.g. gangrene foot.
- Affected part is dry and shrunken with little blood supply; hence bacterial growth is much less. Wet gangrene occurs in naturally moist tissues and organs for example,Gangrene bowel, lungs.
- A line of separation between viable and non-viable tissue is not distinct.
- Venous stuffing of blood in the affected part causes profuse bacterial overgrowth, and hence septicaemic manifestations are common.
- Diabetic foot and bed sores are also examples of wet gangrene.
- Gas gangrene is a special form of wet gangrene caused by gas-forming clostridia.
Leave a Reply