Chronic Infectious Disease Introduction
Actinomycosis, leprosy, syphilis, and AIDS are chronic diseases.
Table of Contents
- Actinomycosis is a rare disease, leprosy and syphilis are of more interest to dermatologists, and AIDS is an interesting topic to all clinicians.
- Hence, only relevant aspects of each of these diseases, as far as general surgeons are concerned, will be discussed here.
Read And Learn More: General Surgery Notes
Actinomycosis
Mycetomas are of two types. Eumycetoma is caused by fungi and actinomycosis is caused by bacteria. It predominantly occurs in the mycetoma belt that lies between the latitudes 15°S and 30°N, comprising countries such as Sudan, Somalia, India, Argentina, Mexico, etc.
- Actinomycosis is caused by Actinomyces is raelii, an anaerobic, gram-positive, branching, filamentous organism (ray fungus). It is normally present in the oral cavity, tonsillar crypts, and dental cavities.
- They become pathogenic in the presence of trauma. Other species include A. neuri and A. neyeri. Three types of actinomycosis which are of interest to general surgeons are discussed here.
Actinomycosis Faciocervical Actinomycosis (50%)
- It is the most common manifestation of actinomycosis.
- It is common in patients with poor oral hygiene, bad caries teeth, etc.
- Diabetes mellitus, immunosuppression, local tissue damage secondary to radiation and neoplasia may precipitate actinomycosis.
- There is subacute or chronic inflammation for many months to years and a lumpy jaw.
- Differential Diagnosis
- Jaw tumour
- Osteomyelitis of jaw
- Malignancy of oral cavity
Eventually, the cheek, mandible, jaws, and salivary glands are involved, resulting in suppuration. The most common site is the mandible.
Actinomycosis Faciocervical Actinomycosis Clinical Features
Two patterns are identified:
1. Chronic slowly progressive inflammation resulting in an indurated mass.
- Extensive (marked) induration of the lower jaw (mandible) and gums give the consistency of bone.
- Multiple subcutaneous nodules over bluish skin covering the jaw.
- The nodules rupture, resulting in multiple discharging sinuses.
- The discharge contains sulphur granules which contain gram-positive mycelia surrounded by gram-negative clubs.
2. Less commonly, it may present as an acute suppurative infection with rapid progression to abscess formation. This causes pain, trismus, dyspnoea, and dysphagia.
- Lymph nodes are not involved. It spreads mainly by direct extension.
- Triad of actinomycosis: Subcutaneous mass, multiple sinuses, and seropurulent discharge.
Actinomycosis Actinomycosis Of The Thorax And Lung (30%)
- It is common in children and is caused by inhalation of ray fungus.
- Over a period of years, it produces actinomycosis of the lung with involvement of the pleura. Later, it also involves the chest wall, resulting in multiple discharging sinuses.
- There may be associated empyema and it may easily spread to the liver.
Actinomycosis Actinomycosis Of The Right Iliac Fossa And Liver (Abdominal Actinomycosis—20%)
It commonly occurs after surgery when there is mucosal injury or discontinuity (for example. after appendicectomy, after perforation of a hollow viscus, or neoplasia).
- The organisms which are normally present in the gut slowly migrate into the periapical tissue, then into the soft tissue and subcutaneous tissue, and produce subacute or chronic low-grade inflammation.
- No compromise of the bowel lumen.
- Once the portal venous radical gets involved, it spreads to the liver.
Actinomycosis Of The Right Iliac Fossa And Liver Clinical Features
- The history of appendicectomy is present in almost all cases.
- 3–6 months later, fever and swelling in the right iliac fossa appear.
- On examination, there is an indurated, nodular, and fixed mass in the right iliac fossa.
- Late stages produce multiple discharging sinuses, sometimes discharging faecal matter and sulphur, granules. Unlike tuberculosis, the lymph nodes are not enlarged.
Differential Diagnosis
Carcinoma caecum, Crohn’s ileocolitis, pericolic abscess, etc.
Actinomycosis Of The Right Iliac Fossa And Liver Management Of Actinomycosis In General
- It is a low-grade chronic disease and is difficult to eradicate.
- Inj. crystalline penicillin 10 lakh units once a day for 6 months–1 year. Tetracycline and lincomycin are alternatives. Amoxycillin 500 mg thrice daily may have to be given for 2–6 months.
- Sinuses in the jaw may have to be excised.
- Osteomyelitis has to be cured.
- Actinomycosis of the right iliac fossa may require a right hemicolectomy. Surgery is not easy. Often, there is extensive necrosis and abscess formation. Malignancy cannot be ruled out. If possible, resect. Otherwise, excise the fistulae, drain the abscesses, and administer IV antibiotics.
Leprosy (Hansens Disease)
- Leprosy is caused by Mycobacterium leprae, an acid-fast bacillus. Poverty, poor hygiene, and population (overcrowding) facilitate its spread.
- The disease is contracted in childhood or adolescence but manifests after a latent period of 2–5 years.
- Nasal secretions are the main source of infection but active ulcers and sweat also contain lepra bacilli.
- Leprosy predominantly affects the skin, upper respiratory tract (nasal cavity), and nerves. Thus, characteristic lesions of leprosy include an anaesthetic patch of skin, or hypopigmented macule, thickened nerves, a deformed leonine face, and a collapsed nasal bridge.
Leprosy Types
- Tuberculoid leprosy: It occurs in patients with good immunity or strong tissue response.
- Lepromatous leprosy: It occurs in patients with poor immunity or poor tissue response.
- Borderline leprosy: It may be borderline lepromatous or borderline tuberculoid leprosy, depending on the immune response.
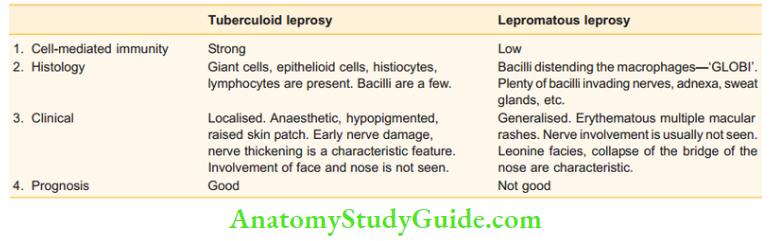
Comparison of tuberculoid leprosy with Lromatous leprosy
Diagnosis Of Leprosy
- Skin biopsy: A full-thickness biopsy is taken from the most active margin of the most active lesion and subjected to acid-fast staining. Skin smears may be taken from ears, elbows, and knees.
- PCR: Polymerase chain reaction is used to detect M. leprae DNA.
Note: No other blood test is available.
Leprosy Treatment
1. Lepromatous and borderline lepromatous leprosy (multibacillary disease)
- A 3-drug regimen is the most ideal treatment.
- For a minimum period of 2 years. Skin smear should be negative.
- Dapsone 100 mg/day
- Clofazimine 50 mg/day
- Rifampicin 600 mg once
- monthly, supervised.
- Clofazimine 300 mg once
- monthly, supervised.
2. Tuberculoid and borderline tuberculoid leprosy (paucibacillary disease)
- For a period of 6 months.
- Dapsone 100 mg daily
- Rifampicin 600 mg once a month, supervised.
Deformities In Leprosy
1. Primary Deformity
They occur directly due to the disease.
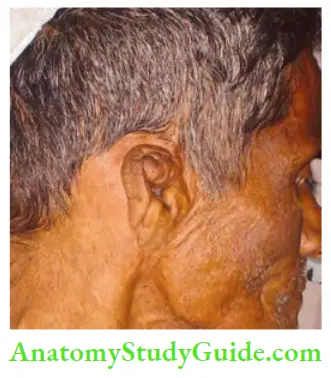
- Face: It is involved in lepromatous leprosy and is described as ‘leonine facies’ with multiple nodules over the face, pigmentation, loss of the lateral portion of the eyebrows (madarosis), the collapse of the nasal bridge due to the destruction of nasal cartilages (warm and moist area), and paralysis of the facial nerve.
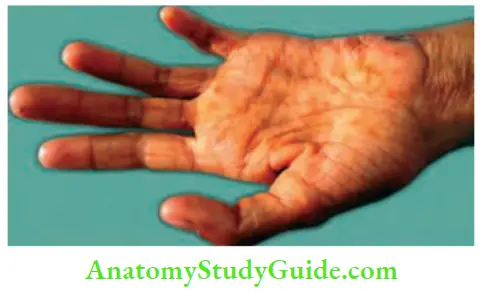
- Hands: Involvement of the ulnar nerve at the elbow and median nerve at the wrist gives rise to claw hand.
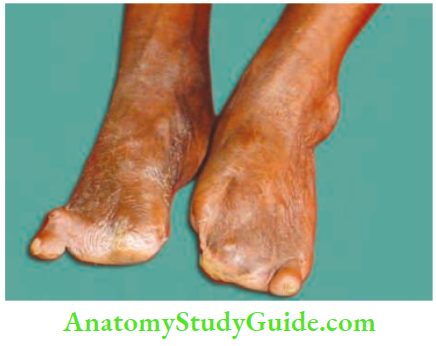
- Foot: The posterior tibial nerve is involved at the ankle leading to clawing of the toes. Foot drop occurs when the lateral popliteal nerve below the knee joint is involved.

Clinical notes MS exam case, KMC, Manipal (2004)
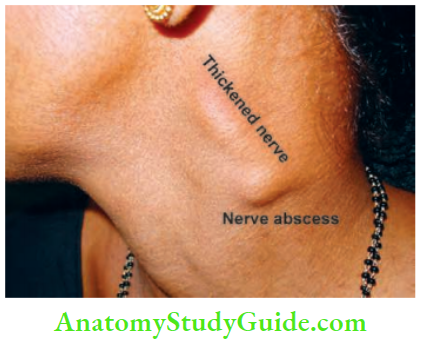
- A 28-year-old lady complained of swelling in the posterior triangle of 8 months duration. The swelling was tender, a bit irregular, and had restricted mobility.
- 3 candidates offered nonspecific lymphadenitis as a diagnosis. Only one candidate thought of a nerve abscess. The clue was a thickened nerve above. It was a case of Hansen’s disease.
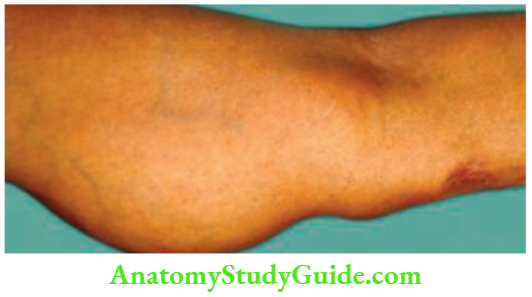
Deformities In Leprosy Ulnar Nerve Abscess And Small Muscle Atrophy In The Hand
Ulnar Nerve Abscess
- May be a part of pure neuritic leprosy.
- Presents as oval fluctuant swelling on the medial side of the arm.
- Granuloma is common. Progression to abscess occurs in tuberculoid leprosy.
- Schwann’s cell is affected. Slowly whole endoneurial zone is occupied by endothelial cells.
- High-resolution ultrasound can demonstrate the echotexture of masses.
- MRI—with the post-gadolinium T1 W sequence—peripheral rim enhancement with central necrosis.
- Treatment: Incision, drainage, excision of granulomatous mass followed by treatment for leprosy.
clinical notes
- A 33-year-old male presented to the outpatient department with the inability to use his right hand for the last 6 months. He said he could not work or hold objects. Examination revealed small muscle atrophy, especially of the hypothenar and interossei muscles.
- A 2 cm ‘skin ulcer’ was also noticed. On careful questioning, he said he also had a loss of sensation. Further examination revealed a 4-cm × 3-cm, firm, oval swelling on the medial side of his right arm, with some amount of fluctuation.
Deformities In Leprosy What is the diagnosis?
Ulnar nerve abscess (cold) secondary to leprosy. This is a case of pure neuritic leprosy with nerve abscess, an uncommon manifestation of M. leprae. No other peripheral nerve was involved.
Correction of Facial Deformities by Plastic Reconstruction
- A prosthesis to correct the nose.
- Lateral tarsorrhaphy to prevent exposure to keratitis.
- Temporalis muscle flap for the upper eyelid to prevent exposure to keratitis.
Deformities In Leprosy Correction of Hand and Foot Deformities
- The claw hand may be corrected using the extensor carpiradialis brevis (Paul Brand’s procedure). Otherwise, the flexor digitorum superficialis may be used (Bunnell’s procedure).
- Foot drop may be corrected by using a tibialis posterior tendon transfer (Ober’s and Barr’s procedure).
2. Secondary Deformities
Because of nerve involvement, sensations are impaired or lost. As a result, ulcers on the fingers, a deep, penetrating, perforating ulcer over the sole of the foot, or even autoamputation of the toes may occur.
Treatment Of Secondary Deformities
- Nonhealing ulcer over the sole of the foot is corrected with the application of a POP (plaster of Paris) posterior slab offloading or non-weight-bearing cast. It takes off the pressure to help the ulcer heal.
- If the calcaneus is involved due to osteomyelitis, the bone has to be cured, followed by the application of regular dressings.
Syphilis French Disease Great Pox
- This is a sexually transmitted disease caused by Treponema pallidum. It is a delicate spiral organism (spirochaete).
- Syphilis is infective only in its early stages. Early lesions are predominantly situated in moist areas, such as the genitalia and oral cavity.
Syphilis French Disease Great Pox Clinical Presentation
Describes congenital syphilis
- Early syphilis
- Late syphilis
Congenital Syphilis
- Early
- Snuffles (rhinitis), epiphysitis, periostitis, osteochondritis.
- Late
- Hutchinson’s triad
- Interstitial keratitis
- 8th nerve deafness
- Hutchinson’s teeth
1. Early Syphilis
- Primary syphilis: Classically, a genital chancre occurs in the penis or vulva after 3–4 weeks of sexual exposure.
- The chancre is a shallow, indurated, painless ulcer called Hunterian chancre. Associated inguinal nodes, which are shotty, multiple, and nontender clinch the diagnosis.
- Extragenital chancres may occur over the lips, tongue, nipple, etc. They produce large enlargement of the corresponding lymph nodes. Chancres in the rectum and perianal region are common in homosexuals. They are painful and resemble anal fissures.

Early Syphilis Investigations
Serological tests for syphilis
- Nonspecific: VDRL, Kahn, Meinicke, Wasserman
- Specific treponemal antigen tests
- CFT—complement fixation test
- TPHA—TP haemagglutination test
- TPI—TP immobilisation test
- FTA-Abs—fluorescent treponema antibody absorption test
- Demonstration of Treponema pallidum in the clear exudate of the lesion by dark field microscopy confirms the diagnosis.
Secondary syphilis: It appears after 6–12 weeks of spirochaetaemia.
- It is characterised by bilateral, symmetrical, coppery red rashes which are generalised. The rash is macular or papular, but never vesicular. Papules on moist sites such as the vulva and perineum enlarge to form condylomata lata—fleshy wart-like growths.
- Small superficial ulcers in the mouth join to form snail-track ulcers.
- Generalised lymphadenopathy involving the epitrochlear and occipital nodes may occur.
- Moth-eaten alopecia, iritis, bone and joint pains.
Latent syphilis: If secondary syphilis is not treated, it will develop into latent syphilis. There are no signs, but serum tests are positive.
2. Late Syphilis
- It is also called tertiary syphilis. It basically affects vessels causing inflammatory reactions and the end result is as follows: ‘Endarteritis obliterans’! tissue necrosis! ulcers or fibrosis.
- This stage develops after 5–15 years of primary syphilis. It causes neurosyphilis and cardiovascular syphilis (aortitis).
- Neurosyphilis includes general paresis and tabes dorsalis involving the posterior column and dorsal roots. It presents with sensory atonia, lancinating pain, and Argyll Robertson pupils.
- A lesser form is a benign lesion called gumma. Gumma is a syphilitic hypersensitivity reaction comprising a granuloma with central necrosis and sloughing.
Clinical Features Of Gumma
- Typically, it is a subcutaneous swelling.
- Affects the midline of the body (for example. the posterior one-third of the tongue, sternum, and sternoclavicular joint).
- Edges are punched out if the gumma ulcerates.
- The floor contains washed leather slough.
- On healing, it leaves a silvery, tissue paper scar (thin scar).
- Gumma may also involve the bone, testis, and liver (ovary is not involved).
Late Syphilis Treatment
- Primary and secondary syphilis are treated by Inj. procaine penicillin 2.4 MU in 1 ml stat. Doxycycline 100 mg BID is given for 21 days. Tetracycline 500 mg QID is also given. In tertiary or latent syphilis: Inj. procaine penicillin
- 4 MU IM once a week for 3 weeks.
- In late syphilis: Treatment is continued for 21 days. With the current effective treatment of syphilis, it is highly unusual to find late cases now.
Aids And The General Surgeon
Acquired Immunodeficiency Syndrome (AIDS) is the end stage of a progressive state of immunodeficiency.
- Causative organism: Human immunodeficiency virus(HIV)
- The details regarding the aetiopathogenesis and immunology of AIDS are discussed in medicine books. Topics of surgical interest are discussed below.
Prophylactic Measures To Be Adopted By Surgeons (Healthcare Workers) While Treating Aids Patients (Universal Precautions)
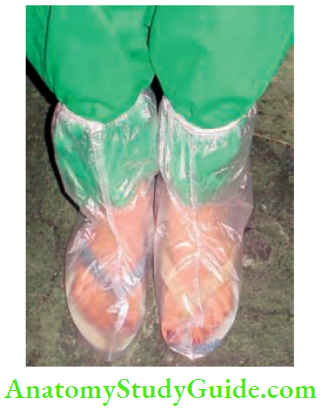
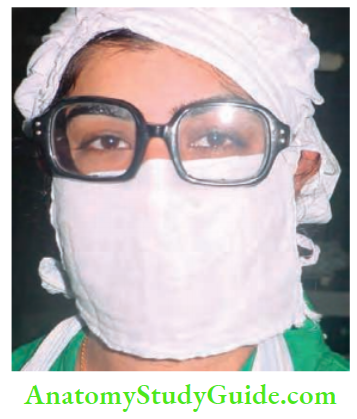
Summary of Universal Precautions to be Taken in OT
- Face mask to be worn
- Avoid splashing on the body: Be slow
- Cover feet and legs: Shoe covers, boot
- Extra glove: Double glove
- Meticulous technique: Haemostasis, gentleness
- Allow only required people
- Spectacles: Protects from splash
- Kidney tray: Use it to transfer sharps
- Remember as FACE MASK
1. In the Outpatient Department (OPD)
- Wear gloves1 when examining any patient with an open wound.
- Wear gloves during proctoscopy or sigmoidoscopy.
- Use hand gloves and eye protection during flexible endoscopy.
- Use disposable instruments.
- Clean reusable instruments such as endoscopes with soap and water, and immerse them in glutaraldehyde.
- Do not perform any surgical procedure involving sharp instruments in the OPD.
2. In the Operation Theatre
- The operating table is covered with a single sheet of polythene.
- The number of theatre personnel is reduced to a minimum.
- Staff with abrasions or lacerations on their hands are not allowed inside the theatre.
- Staff who enter the theatre must wear shoe covers, gloves, disposable and water-resistant gowns, and eye protection.
- Double gloves and eye protection by staff directly involved in the operation (surgeon, assistant, scrub nurse).

Surgical technique:
-
- Avoid ‘sharps’ and needlestick injuries
- Preferably use scissors or diathermy instead of a scalpel
- Use skin clips rather than skin sutures
- Proper autoclaving after the surgery
- In the event of a needlestick injury, allow the part to bleed and wash thoroughly under tap water.
- AZT—zidovudine, lamivudine and indinavir should be given to health workers following exposure of susceptible areas to infected material from AIDS patients.
Range Of Surgery In Hiv Positive Patients
1. Anorectal disease is the most frequent reason for surgical treatment in HIV-positive patients. This is common in homosexuals, in whom AIDS is also common. They have been grouped together as “AIDS anus syndrome.” Anorectal disease may be classified into:
- Anal warts, diarrhoea
- Perianal sepsis—abscesses
- Anal ulceration, fissures
- Reduced sphincter tone and anal incontinence in homosexuals
2. Abdominal pain: This is due to a gastrointestinal opportunistic infection, usually caused by cytomegalovirus (CMV). It is a type of colitis and produces abdominal pain, cramps, loose stools, and blood and mucus in the stools, resulting in emaciation.
- Flexible sigmoidoscopy may reveal severe proctitis. Severe colitis may lead to acute toxic dilatation of the colon.
- Biliary tract infection by cryptosporidium may cause acute cholecystitis. AIDS-related sclerosing cholangitis may occur, resulting in right upper quadrant pain.
- Abdominal lymphoma with involvement of the liver and spleen may also cause abdominal pain.
- Severe abdominal pain may be due to perforation of the small or large bowel and should be treated as an emergency.
- Appendicitis is also common due to CMV infection.
3. Lymphoma, Kaposi’s sarcoma, etc. They occur due to reduced cellular immunity because of:
- Immunosuppression used in organ transplantation
- Severe malnourishment
- HIV infection
- Lymphoproliferative disease
- Kaposi’s sarcoma may affect the skin surface, gastrointestinal tract, lungs, etc. It presents as pigmented multifocal skin lesions.
- HIV-associated Lymphomas
- Lymphomas in HIV patients—‘B’ symptoms and intraabdominal and extranodal involvement including lung, bone marrow and liver are common.
- HIV-associated lymphomas are Diffuse Large Cell (DLC) or Burkitt’s lymphoma.
- HIV-associated lymphomas present as ascites or pleural effusion, etc.
- Treatment should be HAART (highly active antiretroviral therapy) with standard chemotherapy and granulocyte-colony stimulating factor.
4. Oesophageal ulcers may present as dysphagia and odynophagia. Endoscopy should be done using a glove and the scope should be washed thoroughly with soap and water and immersed in cetrimide solution for 15 minutes.
5. Lymphadenopathy: Very often, surgeons are called for lymph node biopsy to evaluate fever or generalised lymphadenopathy. All universal precautions must be observed in all patients.
- A 23-year-old lady, carrying a 6-month-old child, presented to us with severe dysphagia and odynophagia. Endoscopy revealed extensive, unusual, oesophageal ulcers which prompted us to conduct an HIV test. It was positive.
- We called her husband and wanted to convey the message to him, but before we could, he said, ‘I am HIV-positive, my wife is HIV-positive, and even my child is HIV-positive!!!’
Risk of HIV Transmission
- The risk of HIV transmission from patient to surgeon is very low but dangerous.
- Routine use of barriers (gloves and goggles), washing hands before and after examination of the patient, and careful handling of sharps and needles greatly reduce transmission of the disease.
- Post-exposure prophylaxis should begin immediately.
- Routes of exposure and incidence of HIV transmission:
- Percutaneous—0.3%
- Cutaneous— 0.09%
- Mucus membrane—0.09%.
Post-Exposure Prophylaxis (Occupational Exposure)
- Immediate decontamination of the injured area— washing the area with soap and water for cutaneous and percutaneous exposure. For punctured wounds, clean them with alcohol-based agents. For infected eyes, irrigate with a copious amount of sterile water or saline.
- Early reporting of exposure: Blood tests have to be done.
- As soon as possible or within 2 hours, post-exposure prophylaxis should be done using the 3-drug regimen given below.
- Raltegravir 400 mg 3 times/day, tenofovir 300 mg/day and emtricitabine 200 mg/day.
Leave a Reply